Abstract
Purpose: To explore the significance of psychological interventions in the nursing care of rectal cancer patients undergoing ostomy surgery. Methods: We recruited 120 rectal cancer patients undergoing ostomy surgery in our hospital from March 2017 to March 2018 as the study cohort, and they were equally and randomly divided into a control group and an observation group. The control group was administered routine nursing, and the observation group was administered routine nursing combined with psychological nursing. The patients’ conditions were evaluated using the self-rating anxiety scale (SAS), the self-rating depression scale (SDS), the MOS item short form health survey (SF-36), and their defecation. The two groups’ satisfaction levels with the nursing were also compared. Results: The SAS, SDS, HAMA, and HAMD scores in the two groups after the treatment were lower than they were before the treatment, and the observation group was much lower. The SF-36 scores, the patients’ defecation, the nursing satisfaction levels, and the sleep durations in the observation group were higher than they were in the control group, and there were fewer incidences of postoperative complications in the observation group than there were in the control group (P < 0.05). Conclusion: The effects of psychological interventions in the nursing of rectal cancer patients undergoing ostomy surgery are significant. The interventions can relieve the patients’ bad moods, stabilize the patients’ conditions, and improve the patients’ defecation, so it is superior to routine nursing.
Keywords: Rectal cancer ostomy surgery, nursing, psychological interventions, applied research
Introduction
Rectal cancer is a malignant tumor that occurs from the dental line to the junction of the sigmoid colorectal. The main carcinogenic factors include diet, rectal polyps, genetics, etc. [1]. In China, about 70% of rectal cancer patients have low rectal cancer, which requires a colostomy after the radical resection of the low rectal cancer, that is, a permanent artificial anus is made in the left lower abdomen [2]. The rectal cancer stoma takes a great toll on patients, such as their physical, mental, and social functions, and their quality of life. Therefore, due importance should be given to rectal cancer postoperative nursing [3]. After rectal cancer stoma surgery, negative emotions such as anxiety and depression are prone to occur. Appropriate psychological interventions are known to help alleviate psychological problems [4]. In view of this, this study examined psychological nursing interventions for rectal cancer stoma patients, and the clinical outcomes were satisfactory. The report is as follows.
Materials and methods
General information
We recruited 120 patients with rectal cancer stomas who were admitted to our hospital from January 2017 to January 2018 and randomly divided them into a control group and an observation group according to the different nursing method each patient underwent, with 60 cases in each group. The control group ranged in age from 20-70 years old, and the observation group ranged in age from 23-69 years old.
Inclusion criteria: Patients with a clear diagnosis and an ostomy, male or female, patients with a diagnosis in line with International Classification of Diseases for Oncology, third edition, and patients who underwent neoadjuvant chemoradiation followed by resection surgery.
Exclusion criteria: Patients with mental disorders or a cognitive dysfunction, patients with severe infectious diseases, and patients with other malignant tumors.
Informed consent forms were signed by the patients or their family members. The study was approved by the hospital ethics committee.
Nursing methods
The patients in the control group underwent routine nursing care, including vital sign testing, medication guidance, education, etc.
The patients in the observation group underwent targeted psychological nursing interventions in addition to the nursing the control group underwent. 1. Preoperative psychological care. Preoperative psychological counseling for the patients was performed, with the purpose of enabling the patients to actively cooperate with the medical staff in their treatment. Before the surgery, most patients develop negative emotions such as depression, fear, anxiety, etc., and they cannot accept the fact that they need to use an ostomy bag for life after the surgery. The nursing staff explained the importance of the surgical treatment to the patients prior to operation, showed the patients a stoma model, and appropriately alleviated their fear of the operation. The nursing staff invited an experienced stoma expert to provide on-site guidance to increase each patient’s stoma awareness, and the nursing staff taught each patient’s family about rectal cancer so that each patient’s family fully understood the importance of surgery and actively assisted in nursing the patient. 2. According to each patient’s condition, surgical method, etc., the appropriate stoma position was determined during the operation. After the operation, the nursing staff made sure the area around the stoma was clean and provided regular cleaning. 3. The nursing staff guided the patients to master the correct cleaning method after their operations, so that patients could manage their stomas independently. 4. The nursing staff carried out diet and nutrition education for the patients. Foods that are easy to digest and high in nutrition were chosen after eating was allowed, and multiple small meals were encouraged. Foods with high protein content and low fiber were advised when semi-liquid food is consumed. Spicy, irritating, and gas-producing foods were avoided, and smoking and alcohol were prohibited. Regular bowel habits were developed. 5. Individualized psychological intervention and guidance were provided to each patient after the operations to rebuild the patients’ confidence in life. If necessary, a psychologist was asked to assist with the treatment. 6. Before the discharge, home care was taught, follow-up visit lists formulated, and ward mate groups formed to promptly communicate stoma information and stoma complications via the Internet.
Outcome measures
(1) The self-rating anxiety scale (SAS) scores were used to evaluate the patients’ anxiety. (2) The self-rating depression scale (SDS) scores were used to evaluate the patients’ anxiety and depression. (3) The MOS item short form health survey (SF-36) scores were used to evaluate the two groups’ quality of life before and after the intervention, including social function, mental health, emotional function, and physical function. Higher scores indicate a high quality of life, and vice versa. (4) The number of patients with defecation discomfort and defecation regularity was determined. (5) The Nurses’ Observation Scale for Inpatient Evaluation (NOSIE) was used to evaluate the satisfaction with the nursing. The higher the score, the higher the level of satisfaction, and vice versa. According to the criteria, t ≥90 points indicates very satisfied, 60-90 points indicates satisfied, 30-60 points indicates general, and less than 30 points indicates unsatisfied. (6) The patients’ sleep durations within 2 weeks before and after undergoing the care were determined, and the average value was calculated. The patients’ quality of sleep was evaluated using the Pittsburgh Sleep Quality Index (PSQI) [11], which has 24 questions that can be divided into 7 categories. The scores in each category range from 0 to 3 points, of which 0 represents no problem, and 3 indicates very difficult. And the total score is the sum of each category, which range from 0 to 21 points, and the higher the score, the worse the quality of sleep. (7) The anxiety and depression levels in the two groups before and after the intervention were compared, and the Hamilton Anxiety Scale (HAMA) was used to assess the anxiety. The scale has 14 items and uses the 5-likert scale method from 0 to 4 points. The total score ranges from 0 to 56 points. The higher the score, the more serious the anxiety. The Hamilton Depression Scale (HAMD) was used to assess the depression. The scale has a total of 17 items and uses a 5-likert scale method from 0 to 4 points. The total score ranges from 0 to 68 points, with a higher score representing more serious depression. (8) The MOS item short from health survey (SF-36) was used to assess the patients’ quality of life. The domain includes general health (GH), physical functioning (PF) and social functioning (SF), bodily pain (BP), role-physical (RP), mental health (MH), role-emotional (RE), and vitality (VT). The higher the score, the better the quality of life. (9) The complications of the two groups were observed. (10) The patients’ employment was measured using the Productivity Cost Questionnaire from the institute for Medical Technology Assessment (iMTA PCQ), which contains 12 items [5]. The patient Empowerment was measured using two elements of empowerment, i.e. self-efficacy and mastery. The self-efficacy was measured using the General Self-Efficacy Scale (GSE), a questionnaire with 10-hypotheses to assess optimistic self-beliefs to cope with a variety of difficult demands in life [6].
Statistical methods
The statistical analyses were performed using the Statistical Package for the Social Sciences for Windows 15.0 (SPSS Inc.; Chicago, IL, USA).
The categorical data were compared using the chi-square tests; however, the continual variables were compared using ANOVA. A p value of < 0.05 was considered significant for all the statistical tests. GraphPad Prism 8 software was used to plot the graphics.
Results
Baseline information
The baseline data of the two groups were comparable, as shown in Table 1.
Table 1.
Baseline information
| Index | observation group (n=60) | control group (n=60) | t/X2 | P |
|---|---|---|---|---|
| Gender | 1.745 | 0.863 | ||
| male | 32 | 35 | ||
| female | 28 | 25 | ||
| Age (years) | 41.25±6.01 | 40.47±5.28 | 1.452 | 0.635 |
SAS and SDS scores
The SAS and SDS scores in the observation group were found to be lower when compared with the control group (P < 0.05), as shown in Figure 1A, 1B.
Figure 1.
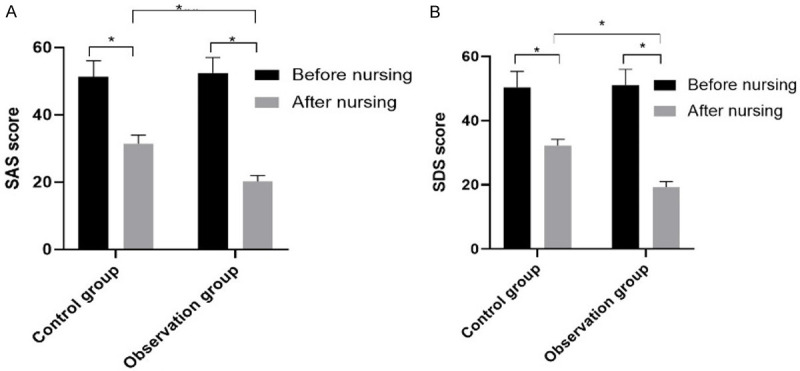
The patients’ SAS and SDS scores in the two groups. Note: A. The SAS scores in the two groups (*mean P < 0.05); B. The SDS scores in the two groups (*mean P < 0.05).
The HAMA and HAMD scores
The results compiled in Table 2 show that the comparisons of the HAMA and HAMD scores before and after the intervention in the two groups were significant and were in favor of the observation group (P < 0.05).
Table 2.
Comparison of the HAMA and HAMD scores before and after the intervention in the two groups
| Group | n | HAMA score | HAMD score | |
|---|---|---|---|---|
| Control group | before intervention | 60 | 14.88±3.47 | 19.33±3.75 |
| after intervention | 60 | 12.24±2.07* | 13.66±3.67* | |
| Observation group | before intervention | 60 | 14.94±3.76 | 19.69±3.91 |
| after intervention | 60 | 9.91±1.76*,# | 10.55±2.63*,# |
Note: Compared with the same group before the intervention;
P < 0.05.
Compared with the control group;
P < 0.05.
SF-36 score
The SF-36 quality of life scores in the observation group were higher than they were in the control group (P < 0.05), as shown in Table 3.
Table 3.
The SF-36 scores (quality of life) in the two groups
| Group | n | role-physical | bodily pain | mental health | physical functioning | |
|
| ||||||
| Control group | before intervention | 60 | 14.88±3.47 | 19.33±3.75 | 51.35±8.04 | 48.28±6.22 |
| after intervention | 60 | 12.24±2.07* | 13.66±3.67* | 61.13±7.74* | 61.32±6.97* | |
| Observation group | before intervention | 60 | 14.94±3.76 | 19.69±3.91 | 52.82±8.04 | 49.04±5.78 |
| after intervention | 60 | 9.91±1.76*,# | 10.55±2.63*,# | 72.56±7.54*,# | 72.48±5.46*,# | |
|
| ||||||
| n | role-emotional | social functioning | general health | vitality | ||
|
| ||||||
| Control group | before intervention | 60 | 55.88±7.47 | 37.33±4.75 | 38.32±8.24 | 36.28±6.27 |
| after intervention | 60 | 62.24±9.07* | 60.66±5.67* | 60.13±7.24* | 60.37±5.97* | |
| Observation group | before intervention | 60 | 54.94±7.76 | 37.69±5.91 | 37.82±9.04 | 37.04±5.28 |
| after intervention | 60 | 7.91±8.76*,# | 68.55±5.63*,# | 75.53±8.24*,# | 75.08±4.86*,# | |
Note: Compared with the same group before the intervention;
P < 0.05.
Compared with the control group;
P < 0.05.
Defecation conditions and complications
Table 4 shows that the comparison of the defecation conditions and complications of patients was significant, and the observation group outperformed the control group.
Table 4.
The defecation situations of the patients in the two groups and a comparison of the complications in the two groups
| Groups | n | Defecation discomfort | Regular defecation | stoma damage | stoma infection | stoma prolapse | stoma stenosis | Totaling |
|---|---|---|---|---|---|---|---|---|
| Control group | 60 | 30 (50%) | 6 (10%) | 3 | 6 | 3 | 7 | 19 |
| Observation group | 60 | 10 (16%) | 21 (35%) | 1 | 3 | 1 | 2 | 7 |
| X2 | 4.50 | 4.50 | 7.07 | |||||
| P | < 0.05 | < 0.05 | 0.007 |
Nursing satisfaction
The observation group had a higher level of satisfaction with the nursing (Table 5).
Table 5.
The nursing satisfaction levels in the two groups
| Group | n | Nursing satisfaction | |||
|---|---|---|---|---|---|
|
| |||||
| Very satisfied | Generally satisfied | Satisfied | Unsatisfied | ||
| Control group | 60 | 21 | 12 | 22 | 5 |
| Observation group | 60 | 33 | 22 | 4 | 1 |
| X2 | 4.125 | ||||
| P | P < 0.05 | ||||
Sleep durations and PSQI scores
With respect to the sleep durations and PSQI scores, the observation group was better, as shown in Table 6.
Table 6.
A comparison of the sleep conditions in the two groups before and after the intervention
| Group | n | PSQI score | Sleep length per night | |
|---|---|---|---|---|
| Control group | before intervention | 60 | 14.28±3.57 | 5.43±2.05 |
| after intervention | 60 | 8.04±2.17* | 6.76±1.97* | |
| Observation group | before intervention | 60 | 14.24±3.78 | 5.59±1.96 |
| after intervention | 60 | 5.01±1.66*,# | 7.91±1.23*,# |
Note: Compared with the same group before the intervention;
P < 0.05.
Compared with the control group;
P < 0.05.
Employment and empowerment
The employment and empowerment levels in the two groups were statistically distinguishable (P < 0.05).
Discussion
Rectal cancer is a common malignant tumor seen in gastrointestinal surgery, and surgery remains the mainstay for the treatment [7]. One major drawback of this approach is that it can result in defecation function disorder, despite the general treatment effect achieved [8-11]. Rectal cancer stomas are a key component of rectal cancer treatment. In addition to good surgical outcomes, nursing work is considerably important, especially in the psychological intervention of patients [12,13]. Due to the double blow of disease and stoma in the patients, most patients will have an inferiority complex, anxiety, fear and other adverse psychological reactions, which will lower the patient’s treatment compliance and seriously affect the treatment outcome and prognosis [14-16]. Studies have found that active psychological interventions can effectively improve the patients’ bad moods, help patients restore confidence in the treatment, boost patient compliance, and significantly improve their clinical prognoses [17,18]. Stoma nursing care is thus considered extremely critical in the treatment of rectal cancer. Effective stoma nursing care can avoid or reduce the occurrence of infections, and it can help patients return to a normal social life. Taking psychology as the core of nursing, advocating the principles of people-oriented, active initiative, role transition, problem orientation, etc., is a new nursing model [19]. We provided psychological interventions for patients with rectal cancer stomas in our study, focusing on being people-oriented, fully respecting the will of the patients, questioning the patients in detail, formulating nursing plans, and improving patient cooperation. To quickly find and solve each patient’s problems and to mobilize their proactiveness, each patient’s confidence in returning to society and family was boosted; to instruct scientific health education and increase each patient’s awareness of the disease, while taking into account gaps in different cultures and social roles, individualized care was realized [20,21]. We found that the SAS, SDS, HAMA, and HAMD scores in the two groups of patients after the treatment were lower than they were before the treatment, and the observation group was much lower, while the SF-36 scores, the defecation conditions, the satisfaction with the nursing, and the sleep durations were much higher, and the postoperative complication rate in the observation group was much lower. Taken together, all these findings indicate that psychological nursing intervention applied to colostomy patients after rectal cancer surgery can relieve their depression, improve their quality of life, and increase their nursing satisfaction. Our study has limitations. The use of a retrospective database limited our ability to investigate other sources of potential bias. On the other hand, the generalizability of our study findings needs to be considered.
In conclusion, the application of psychological nursing interventions for patients with rectal cancer stomas can relieve their unhealthy moods, improve their quality of life, and increase their level of satisfaction with the nursing care. It is worthy of widespread clinical application.
Disclosure of conflict of interest
None.
References
- 1.Shussman N, Wexner SD. Current status of laparoscopy for the treatment of rectal cancer. World J Gastroenterol. 2014;20:15125–15134. doi: 10.3748/wjg.v20.i41.15125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li GD, Dong XS, Liu M. Progress in surgical treatment of rectal cancer. Chin J Cancer Prevent Treat. 2015;5:402–406. [Google Scholar]
- 3.Zeng CY, Tang D, Zhang LF. Observation on the application effect of individualized nursing intervention in postoperative nursing of rectal cancer. Chin Contempor Med. 2017;15:176–178. [Google Scholar]
- 4.Sun XM, Guan QY, Xiao MY, Wang QX, Li YF. Application of case management model in the care of patients with permanent colostomy. Chin Electr J Colorect Dis. 2017;6:525–528. [Google Scholar]
- 5.Cai L, Ahlström G, Tang P, Ma K, Edvardsson D, Behm L, Fu H, Zhang J, Yang J. Psychometric evaluation of the Chinese version of the person-centred climate questionnaire - staff version (PCQ-S) BMJ Open. 2017;7:e017250. doi: 10.1136/bmjopen-2017-017250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Molero Jurado MDM, Pérez-Fuentes MDC, Oropesa Ruiz NF, Simón Márquez MDM, Gázquez Linares JJ. Self-efficacy and emotional intelligence as predictors of perceived stress in nursing professionals. Medicina (Kaunas) 2019;55:237. doi: 10.3390/medicina55060237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Biffi R, Luca F, Bianchi PP, Cenciarelli S, Petz W, Monsellato I, Valvo M, Cossu ML, Ghezzi TL, Shmaissany K. Dealing with robot-assisted surgery for rectal cancer: current status and perspectives. World J Gastroenterol. 2016;22:546–556. doi: 10.3748/wjg.v22.i2.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wei JL, Zhang S. Progress in clinical treatment of colorectal cancer. Chin J New Clin Med. 2018;2:202–208. [Google Scholar]
- 9.Xu WQ, Zhang YF, Liang R. The effect of comprehensive nursing intervention on the marital quality of patients with rectal cancer after stoma. Chin Gener Pract. 2013;7:1143, 1152. [Google Scholar]
- 10.Seibert RG, Hanchate AD, Berz JP, Schroy PC 3rd. National disparities in colorectal cancer screening among obese adults. Am J Prev Med. 2017;53:e41–e49. doi: 10.1016/j.amepre.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 11.Siantz E, Wu B, Shiroishi M, Vora H, Idos G. Mental illness is not associated with adherence to colorectal cancer screening: results from the California health interview survey. Dig Dis Sci. 2017;62:224–234. doi: 10.1007/s10620-016-4366-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Manderbacka K, Arffman M, Lumme S, Suvisaari J, Keskimäki I, Ahlgren-Rimpiläinen A, Malila N, Pukkala E. The effect of history of severe mental illness on mortality in colorectal cancer cases: a register-based cohort study. Acta Oncol. 2018;57:759–764. doi: 10.1080/0284186X.2018.1429649. [DOI] [PubMed] [Google Scholar]
- 13.Yarborough BJH, Hanson GC, Perrin NA, Stumbo SP, Green CA. Colorectal cancer screening completion among individuals with and without mental illnesses: a comparison of 2 screening methods. Am J Health Promot. 2018;32:925–931. doi: 10.1177/0890117116686573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.May FP, Yano EM, Provenzale D, Steers WN, Washington DL. Race, poverty, and mental health drive colorectal cancer screening disparities in the veterans health administration. Med Care. 2019;57:773–780. doi: 10.1097/MLR.0000000000001186. [DOI] [PubMed] [Google Scholar]
- 15.Lloyd S, Baraghoshi D, Tao R, Garrido-Laguna I, Gilcrease GW 3rd, Whisenant J, Weis JR, Scaife C, Pickron TB, Huang LC, Monroe MM, Abdelaziz S, Fraser AM, Smith KR, Deshmukh V, Newman M, Rowe KG, Snyder J, Samadder NJ, Hashibe M. Mental health disorders are more common in colorectal cancer survivors and associated with decreased overall survival. Am J Clin Oncol. 2019;42:355–362. doi: 10.1097/COC.0000000000000529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tuesley KM, Jordan SJ, Siskind DJ, Kendall BJ, Kisely S. Colorectal, cervical and prostate cancer screening in Australians with severe mental illness: retrospective nation-wide cohort study. Aust N Z J Psychiatry. 2019;53:550–558. doi: 10.1177/0004867418814945. [DOI] [PubMed] [Google Scholar]
- 17.Wang AH, Luo N, Zhao HB. The impact of stoma special care on the quality of life of patients with rectal cancer after stoma. Chin J Clin Oncol Rehabilitat. 2017;12:1509–1512. [Google Scholar]
- 18.Wang M, Zhu XL, Wang CY, Li YZ, Xiao GH. The source of control, quality of life and coping styles of patients with rectal cancer stoma. Chin Mental Health J. 2013;10:750–753. [Google Scholar]
- 19.Feng JL. The effect of continuous nursing on the mental state and self-care ability of patients with rectal cancer stoma. Electron J Pract Clin Nur. 2017;47:125, 134. [Google Scholar]
- 20.Mosher CE, Winger JG, Given BA, Helft PR, O’Neil BH. Mental health outcomes during colorectal cancer survivorship: a review of the literature. Psychooncology. 2016;25:1261–1270. doi: 10.1002/pon.3954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brown JC, Damjanov N, Courneya KS, Troxel AB, Zemel BS, Rickels MR, Ky B, Rhim AD, Rustgi AK, Schmitz KH. A randomized dose-response trial of aerobic exercise and health-related quality of life in colon cancer survivors. Psychooncology. 2018;27:1221–1228. doi: 10.1002/pon.4655. [DOI] [PMC free article] [PubMed] [Google Scholar]


