Abstract
Objective: To investigate the balance function and subjective quality of life in elderly female knee osteoarthritis patients KOAKOA treated with Wuqinxi exercises. Methods: A total of 284 elderly female patients with knee osteoarthritis (KOA) were randomly divided into an experimental group, which did Wuqinxi exercises for 24-weeks (n=132), and a control group, which didn’t do any regular physical exercises (n=134). The experimental group did Wuqinxi exercises for 24 weeks, and the control group didn’t engage in any regular physical exercise. We performed limits of stability (LOS) tests, static posture stability (SPS) tests, and dynamic fall index (DFI) tests to assess the patients’ balance, and we administered the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) questionnaire to evaluate the physical functioning of the patients’ knees. Results: The limits of stability (LOS) test, the static posture stability (SPS) test, and the dynamic fall index (DFI) test results were improved in the experimental group compared with the control group (P < 0.05). From baseline to the week 24 follow-up, the WOMAC tests, and the pain, joint stiffness, and lower limb muscle strength showed significant differences between the two groups (P < 0.05). Conclusions: Wuqinxi exercises are an effective treatment for elderly female patients with knee osteoarthritis, and can improve their balance and subjective quality of life. The therapy effectively alleviates the clinical symptoms of the elderly female knee osteoarthritis patients.
Keywords: Wuqinxi exercise, balance function, quality of life, knee osteoarthritis
Introduction
Knee osteoarthritis (KOA) is a common, chronic joint disease, and its clinical symptoms include pain, joint stiffness, and dysfunction which seriously affect the quality of life [1]. Its worldwide prevalence rate is 10-30% [2,3]. In prior studies, KOA has been associated with increased pain, the disruption of daily activities, altered gait patterns, and falling down [4,5]. The current therapeutic methods for treating KOA patients include surgery, non-operative management, and rehabilitation. Surgery isn’t a better choice for KOA patients. Nowadays, exercise therapy is recommended as a primary non-operative treatment for KOA, as it can ameliorate quality of life [6,7]. Wuqinxi exercises, a type of exercise therapy for KOA patients, are generated through muscle activity primarily around the hip and ankles to dredge the systemic blood circulation. Additionally, Wuqinxi exercises have many advantages: attractiveness, uncomplication, diversity, feasibility, and small space requirements. A study showed that exercise has a significant effect on relieving KOA symptoms and improving knee function [1].
This study aimed to evaluate the effect of the balance function and quality of life Wuqinxi exercises on elderly female patients with KOA.
Materials and methods
Study design
The study was a randomized controlled trial. This study was performed at Hubei Provincial Hospital of Traditional Chinese Medicine from July 2017 to July 2020. The KOA diagnoses were based on the revised 2006 American College of Rheumatology diagnostic criteria [8]. Inclusion criteria (At least three of the following 1-6 items were met): 1) Age < 75 years, 2) The duration of the morning stiffness is less than 30 minutes, 3) The joints bounce when they move, 4) Bone tenderness, 5) The knee joint has bone hypertrophy, 6) Osteophyte formation, 7) The course of KOA has lasted for more than 6 months, 8) The subjects were willing to cooperate and participate in the experiment, and 9) Each participant had a medical clearance to do physical exercises. Exclusion criteria: 1) Previous hip, knee, or ankle surgery, 2) Rheumatoid arthritis, 3) Patients with a previous cardiovascular, kidney, or liver failure, 4) Infectious arthritis, and 5) Patients who did not undergo the treatment after their enrollment according to the established regimen or who gave up during the treatment. The study was approved by the hospital Research Ethics Committee, and all the participants provided an informed consent before their inclusion in the trial. Furthermore, this study was conducted in accordance with the Declaration of Helsinki.
Participants and subgroup
A total of 354 KOA patients were treated at the Hubei Provincial Hospital of Traditional Chinese Medicine, including 284 patients who met the inclusion and exclusion criteria. The 284 eligible patients enrolled in this study were randomly allocated into one of two groups: the experimental group (EG) (n=142) or the control group (CG) (n=142).
Interventions
EG: The patients underwent a 24-week course of Wuqinxi exercises. Every participant was trained with professional guidance. The KOA patients practiced 6 times a week, with 3 groups of exercises each time, and with 5 minutes’ rest between each group of exercises. The whole process was completed within 60 minutes. The exercises included: 1) Tiger play, 2) Deer play, 3) Bear play, 4) Ape play, and 5) Bird play. The patients had follow-up visits on the final treatment (day 28), and follow up visits at 12 weeks and 24 weeks.
CG: The participants didn’t take any regular physical exercise. Patients had follow-up with visits at the end of the treatment (day 28), 12 weeks follow-up and 24 weeks follow-up.
Primary outcome measures
The balance function was determined using the Biodex Balance System (BBS) (American BBS Co., Ltd.). The device can be used to conduct limits of stability (LOS) tests, static posture stability (SPS) tests, and dynamic fall index (DFI) tests. Each test was performed three times, and the average value was taken. The quality of life was evaluated using the Short-Form Health Survey 36 (SF-36).
Secondary outcomes
The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) was used to evaluate the functional outcomes after the exercise course in the KOA patients, and the Chinese version of the WOMAC questionnaire was applied in our research [9].
Statistical analysis
All the data were analyzed using SPSS 22.0. The results are presented as the means ± standard deviation (means ± SD) or percentages. Two groups were compared using analyses of variance, and the intergroup comparisons were performed using Shapiro-Wilk tests. For the normally distributed data, t-tests were used (paired samples t-tests for the comparisons of the before/after parameters, independent samples t-tests for the comparisons between the arms). For the non-normally distributed data, Mann-Whitney U tests and Wilcoxon signed rank tests were used. A P value of ≤ 0.05 was considered statistically significant.
Result
Clinical characteristics
Table 1 shows the characteristics of the participants. The study included 266 patients after the follow-up and involved 132 patients in the experimental group, with a mean age of (71±2.92) years old, while in the control group, the mean age was (69±3.72) years old. The BMI in the experimental group was (29.8±7.07) kg/m2, and in the control group it was (28.4±3.7) kg/m2, and there was no statistically significance difference between the two groups (P=0.07, > 0.05). The number of smokers in experimental group was 69 (52.3%), and in the control group it was 79 (58.9%). The number of participants who took analgesics occasionally was 79 (59.8%) in experimental group, and in control group it was 60 (44.8%). The two groups were similar in terms of their demographics, clinical characteristics, and the occurrences of of chronic diseases like diabetes, hypertension, or coronary heart disease, so there were no significant statistical differences between the two groups.
Table 1.
Comparison of clinical characteristics of the KOA patients between the two groups
| Experimental group (n=132) | Control group (n=134) | t/X2 | P | |
|---|---|---|---|---|
| Age (years) | 71±2.92 | 69±3.72 | 0.45 | 0.75 |
| Height (cm) | 154.5±3.75 | 150.5±4.26 | 1.29 | 0.31 |
| Weight (Kg) | 80.25±3.4 | 78.2±10.8 | 3.39 | 0.38 |
| BMI | 29.8±7.07 | 28.4±3.7 | 2.25 | 0.07 |
| Smokers (n%) | 69 (52.3%) | 79 (58.9%) | 4.96 | 0.48 |
| Diabetes | 83 (62.9%) | 90 (67.2%) | 7.63 | 0.96 |
| Hypertension | 68 (51.5%) | 65 (48.5%) | 12.13 | 0.81 |
| Coronary Heart Disease | 49 (37.1%) | 41 (30.6%) | 11.67 | 0.68 |
| KOA duration | 28.3±18.1 | 27.9±17.98 | 5.59 | 0.54 |
| Take Medicine | ||||
| Analgesics | 79 (59.8%) | 60 (44.8%) | 10.32 | 0.23 |
| Cartilage protection drugs | 97 (73.5%) | 104 (77.6%) | 4.48 | 0.16 |
| physicotherapeutics | 49 (37.1%) | 58 (43.3%) | 2.23 | 0.49 |
Note: Significant difference as P < 0.05. EG: Experimental group; CG: Control group.
The static posture stability (SPS) indexes in the two groups
As shown in Figure 1 and Table 2, in the experimental group, the Static Posture Stability (SPS) Index was significantly decreased at the 12 week follow-up and the 24 week follow-up compared with the baseline. At the 12 week follow-up and 24 week follow-ups, the Static Posture Stability (SPS) Index showed statistically significant differences between the two groups (at the 12 week follow-up, (1.58±0.26) vs. (1.75±0.18), P=0.04. At the 24 week follow-up, (1.44±0.18) vs. (1.63±0.16), P=0.02).
Figure 1.
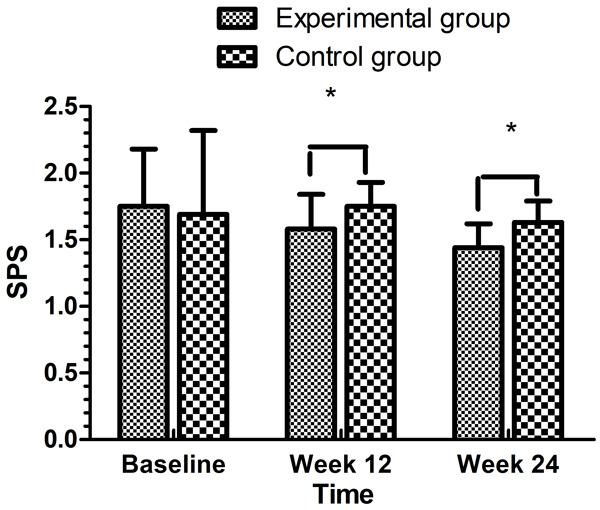
Comparison of the SPS indexes between the two groups. *P < 0.05.
Table 2.
Comparison of the Static Posture Stability (SPS) index scores between the two groups (points, x̅ ± s)
| group | Number of cases | Baseline | Week 12 | Week 24 |
|---|---|---|---|---|
| Experimental group | 132 | 1.75±0.43 | 1.58±0.26 | 1.44±0.18 |
| Control group | 134 | 1.69±0.63 | 1.75±0.18 | 1.63±0.16 |
| t | - | 3.76 | 5.38 | 5.93 |
| P | - | 0.27 | 0.04 | 0.02 |
Note: Significant difference as P < 0.05.
The dynamic fall index (DFI) tests in the two groups
In the EG, the patients had a significant decrease in their DFI scores compared to the CG, with statistically significant differences at the 12 week follow-up and the 24 week follow-up (P < 0.05) (Table 3). And the DFI tests in the follow-up period were decreased compared with the baseline in the experimental group (Table 3 and Figure 2).
Table 3.
Comparison of the Dynamic Fall Index (DFI) scores between the two groups (points, x̅ ± s)
| Group | Number of cases | Baseline | Week 12 | Week 24 |
|---|---|---|---|---|
| Experimental group | 132 | 1.26±0.51 | 0.94±0.32 | 0.93±0.28 |
| Control group | 134 | 1.20±0.43 | 1.02±0.38 | 1.17±0.24 |
| t | - | 3.168 | 6.636 | 8.954 |
| P | - | 0.48 | 0.003 | 0.0001 |
Note: Significant difference as P < 0.05.
Figure 2.
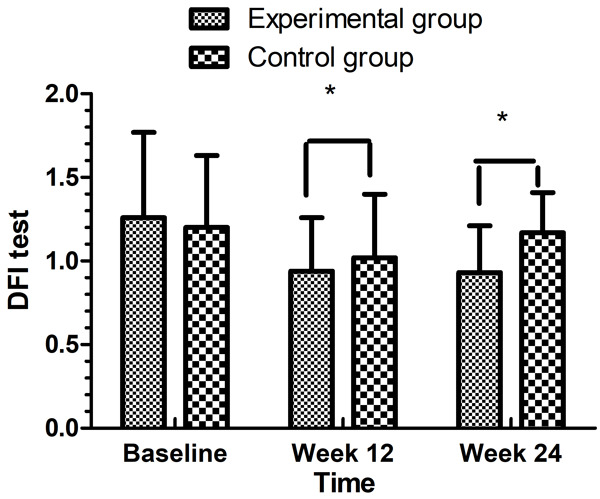
Comparison of the DFI test results between the two groups. *P < 0.05.
The limits of stability (LOS) tests in the two groups
Limits of stability (LOS) test results were significantly decreased in the EG. The Limits of Stability (LOS) test results were significantly decreased with the Wuqinxi exercise therapy. And the LOS test results were significantly decreased with the Wuqinxi exercise therapy at the 24 weeks follow-up compared between the two groups ((0.83±0.28) VS. (0.94±0.22)) (Table 4 and Figure 3).
Table 4.
Comparison of the Limits of Stability (LOS) index between the two groups (points, x̅ ± s)
| Group | Number of cases | Baseline | Week 12 | Week 24 |
|---|---|---|---|---|
| Experimental group | 132 | 1.08±0.44 | 0.92±0.22 | 0.83±0.28 |
| Control group | 134 | 1.04±0.54 | 0.93±0.41 | 0.94±0.22 |
| t | - | 1.168 | 3.636 | 5.934 |
| P | - | 0.75 | 0.68 | 0.04 |
Note: Significant difference as P < 0.05.
Figure 3.
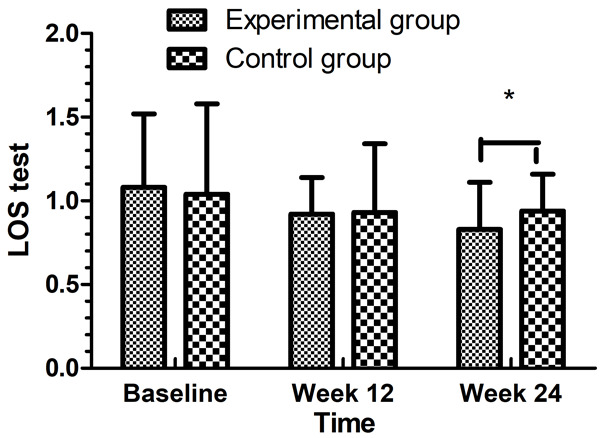
Comparison of the LOS test results between the two groups. *P < 0.05.
The WOMAC test scores in the two groups
From baseline to the week 24 follow-up, the WOMAC test scores, the pain intensity, the joint stiffness and lower limb muscle strength were significantly different between the two groups. The pain intensity in the experimental group decreased, and the decline in the experimental group was significantly different compared with the control group at the 12 week follow-up and the 24 week follow-up ((81.25±25.53) vs. (77.35±24.45), P=0.003; (75.7±20.19) vs. (94.25±27.73), P=0.001). The joint stiffness improved in both groups, but the exercises in the experimental group were more effective than they were in the control group at the 12 week follow-up and the 24 week follow-up ((27.20±8.74) vs. (29.35±9.17), P=0.042; (23.65±8.93) vs. (27.10±10.11), P=0.009). As to the lower limb muscle strength, it increased in the two groups, and the exercises in the experimental group were more effective than they were in the control group at the 12 week follow-up and the 24 week follow-up ((256±84.22) vs. (265.70±75.37), P=0.03; (245.5±94.77) vs. (285.35±94.22), P=0.002) (Table 5).
Table 5.
Scores for WOMAC test of two groups before and after intervention (points, x̅ ± s)
| Experimental group (n=132) | Control group (n=134) | t/X2 | P | |
|---|---|---|---|---|
| Pain intensity | ||||
| Baseline | 98.45±36.01 | 97.95±25.61 | 3.78 | 0.86 |
| Week 12 | 81.25±25.53 | 77.35±24.45 | 11.37 | 0.000 |
| Week 24 | 75.7±20.19 | 94.25±27.73 | 16.83 | 0.000 |
| Joint Stiffness | ||||
| Baseline | 32.25±5.3 | 30.9±8.93 | 5.21 | 0.57 |
| Week 12 | 27.20±8.74 | 29.35±9.17 | 6.91 | 0.042 |
| Week 24 | 23.65±8.93 | 27.10±10.11 | 16.73 | 0.000 |
| Lower limb muscle strength | ||||
| Baseline | 208.65±88.44 | 304.45±123.49 | 25.67 | 0.65 |
| Week 12 | 256±84.22 | 265.70±75.37 | 17.79 | 0.003 |
| Week 24 | 245.5±94.77 | 285.35±94.22 | 19.93 | 0.000 |
Note: Significant difference as P < 0.05.
The SF-36 tests in the two groups
The quality of life was assessed using the SF-36 questionnaire. As shown in Table 6, from the baseline to the 12 and 24 week follow-ups, there was a significant improvement in quality of life at the 24 week follow-up compared with the baseline between two groups (P < 0.05). In addition, the two groups’ SF-36 scores at week 12 and week 24 were significantly improved compared to the baseline scores, and the difference between the EG and CG at the 24 week follow-up point was statistically significant ((17.83±5.28) vs. (13.94±4.22), P=0.001).
Table 6.
Comparison of SF-36 test between the two groups (points, x̅± s)
| Group | Number of cases | Baseline | Week 12 | Week 24 |
|---|---|---|---|---|
| Experimental group | 132 | 10.6±8.44 | 12.92±6.22 | 17.83±5.28 |
| Control group | 134 | 10.4±6.54 | 12.53±3.41 | 13.94±4.22 |
| t | - | 2.71 | 1.27 | 6.793 |
| P | - | 0.35 | 0.28 | 0.000 |
Note: Significant difference as P < 0.05.
Discussion
As shown in our research, Wuqinxi exercises can significantly improve the balance function and subjective quality of life among elderly female patients with KOA. From the baseline to the week 24 follow-up, the limits of stability (LOS) tests, the static posture stability (SPS) tests, and the dynamic fall index (DFI) tests in the EG were improved compared with the same tests in the CG. Furthermore, the WOMAC scores were significantly different between the two groups (P < 0.05), and the experimental patients’ clinical symptoms and QOL were improved.
It is said that Wuqinxi exercises are a health preserving and healthy exercise; furthermore, they are based on the theory of traditional Chinese medicine and imitate the movements of tigers, bears, deer, apes, and birds (cranes) [10]. The exercises combine body and spirit, integrating guidance and breathing [11]. The Wuqinxi exercises described in this study embody the concept of “stretching the limbs and moving the joints” in the process of creating the skills. In theory, Wuqinxi exercises can improve patients’ balance abilities, core strength, and the proprioception of patients with KOA [12]. As we all know, Wuqinxi exercises improve the stability and flexibility of the body and limbs and the motility of the muscles and bones [12-14]. Consistent with the results of our study, Wuqinxi exercises can significantly improve the balance function and subjective quality of life among the elderly female patients with KOA.
The results show that a 24-week course of Wuqinxi exercises can effectively improve the muscle strength and muscle endurance of the quadriceps femoris and the myxocrine muscle. It can significantly relieve the clinical symptoms such as pain, stiffness, and limited movement. Furthermore, it can improve patients’ functional status and quality of life as a whole. The above experimental results show that Wuqinxi exercises improve the muscle strength of KOA patients and improve their clinical symptoms. Wuqinxi exercises can relieve pain and reduce functional limitations. The muscles around the knee joint include the quadriceps femoris, the myxocyprinus and gastrocnemius. Wuqinxi exercises can stabilize the knee joints and improve muscle strength. Our findings are consistent with those of other studies [15-17].
We assessed the quality of life using SF-36 questionnaires, which evaluates physical function and mental health [18]. Our research indicated that the SF-36 scores of the EG and CG were improved at 12 weeks follow-up and 24 weeks follow-up compared with the baseline. Furthermore, the experimental group had a statistically significant difference at the 24 week follow-up (P < 0.05). This indicates that long-term Wuqinxi exercises can improve quality of life.
One clear weakness of our current study is the fact that it was a small, single center study. In particular, the difficulties in enrolling patients were related to the limits on the number of KOA patients. On the other hand, although our results are promising, the explanation is limited by the self-control designed study. These interpretations indicate the need for a larger, placebo-controlled, prospective study to evaluate the efficacy and safety of Wuqinxi exercise treatment for elderly female patients with knee osteoarthritis.
At present, the therapeutic mechanisms of Wuqinxi exercises in treating KOA patients includes two aspects: First, Wuqinxi exercises can produce changes in muscle tension and stimulate the mechanical receptors through the continuous flexion and extension of the joints, muscle contractions, and relaxation [19]. Wuqinxi exercises improve the excitability of the action neurons, regulate the muscle spindle fibers positively, enhance the muscle strength, and improve the stability of the knee joint. Second, Wuqinxi exercises can increase the muscle strength of the lower limbs, improving the balance ability and proprioception of the human body [20]. We plan to carry out an in-depth investigation of the mechanism underlying the therapy of Wuqinxi exercises for KOA patients.
In summary, this study provides preliminary evidence that Wuqinxi exercises result in greater improvements in balance function and subjective quality of life among elderly female patients with KOA. Large, blinded, randomized clinical trials of longer duration are needed to assess the long-term efficacy and safety of Wuqinxi exercises in elderly female patients with KOA.
Disclosure of conflict of interest
None.
References
- 1.Li D, Li S, Chen Q, Xie X. The prevalence of symptomatic knee osteoarthritis in relation to age, sex, area, region, and body mass index in China: a systematic review and meta-analysis. Front Med (Lausanne) 2020;7:304–309. doi: 10.3389/fmed.2020.00304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cho HJ, Morey V, Kang JY, Kim KW, Kim TK. Prevalence and risk factors of spine, shoulder, hand, hip, and knee osteoarthritis in community-dwelling Koreans older than age 65 years. Clin Orthop Relat Res. 2015;473:3307–14. doi: 10.1007/s11999-015-4450-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Postler A, Ramos AL, Goronzy J, Günther KP, Lange T, Schmitt J, Zink A, Hoffmann F. Prevalence and treatment of hip and knee osteoarthritis in people aged 60 years or older in Germany: an analysis based on health insurance claims data. Clin Interv Aging. 2018;13:2339–2349. doi: 10.2147/CIA.S174741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knoop J, van der Leeden M, van der Esch M, Thorstensson CA, Gerritsen M, Voorneman RE, Lems WF, Roorda LD, Dekker J, Steultjens MP. Association of lower muscle strength with self-reported knee instability in osteoarthritis of the knee: results from the Amsterdam Osteoarthritis cohort. Arthritis Care Res (Hoboken) 2012;64:38–45. doi: 10.1002/acr.20597. [DOI] [PubMed] [Google Scholar]
- 5.Skou ST, Wrigley TV, Metcalf BR, Hinman RS, Bennell KL. Association of knee confidence with pain, knee instability, muscle strength, and dynamic varus-valgus joint motion in knee osteoarthritis. Arthritis Care Res (Hoboken) 2014;66:695–701. doi: 10.1002/acr.22208. [DOI] [PubMed] [Google Scholar]
- 6.Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SMA, Kraus VB, Lohmander LS, Abbott JH, Bhandari M, Blanco FJ, Espinosa R, Haugen IK, Lin J, Mandl LA, Moilanen E, Nakamura N, Snyder-Mackler L, Trojian T, Underwood M, McAlindon TE. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019;27:1578–1589. doi: 10.1016/j.joca.2019.06.011. [DOI] [PubMed] [Google Scholar]
- 7.Wang L, Chen H, Lu H, Wang Y, Liu C, Dong X, Chen J, Liu N, Yu F, Wan Q, Shang S. The effect of transtheoretical model-lead intervention for knee osteoarthritis in older adults: a cluster randomized trial. Arthritis Res Ther. 2020;22:134–148. doi: 10.1186/s13075-020-02222-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peat G, Thomas E, Duncan R, Wood L, Hay E, Croft P. Clinical classification criteria for knee osteoarthritis: performance in the general population and primary care. Ann Rheum Dis. 2006;65:1363–7. doi: 10.1136/ard.2006.051482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim MJ, Kang BH, Park SH, Kim B, Lee GY, Seo YM, Park KS, Yoo JI. Association of the Western Ontario and Mcmaster Universities Osteoarthritis Index (WOMAC) with muscle strength in community-dwelling elderly with knee osteoarthritis. Int J Environ Res Public Health. 2020;17:2260. doi: 10.3390/ijerph17072260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang T, Xiao G, Li Z, Jie K, Shen M, Jiang Y, Wang Z, Shi X, Zhuang J. Wuqinxi exercise improves hand dexterity in patients with Parkinson’s disease. Evid Based Complement Alternat Med. 2020;2020:835–841. doi: 10.1155/2020/8352176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xiao CM, Li JJ, Kang Y, Zhuang YC. Follow-up of a Wuqinxi exercise at home programme to reduce pain and improve function for knee osteoarthritis in older people: a randomised controlled trial. Age Ageing. 2021;50:570–575. doi: 10.1093/ageing/afaa179. [DOI] [PubMed] [Google Scholar]
- 12.Yao C, Li Z, Zhang S, Wu Z, Zhu Q, Fang L. Effects of Wuqinxi in the patients with chronic low back pain: a randomized controlled trial. Evid Based Complement Alternat Med. 2020;14:1–12. doi: 10.1155/2020/1428246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang B, Cheng CS, Ye MG, Han CZ, Peng DY. A preliminary study of the effects of medical exercise Wuqinxi on indicators of skin temperature, muscle coordination, and physical quality. Medicine (Baltimore) 2018;97:e12003. doi: 10.1097/MD.0000000000012003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bennell KL, Nelligan RK, Kimp AJ, Wrigley TV, Metcalf B, Kasza J, Hodges PW, Hinman RS. Comparison of weight bearing functional exercise and non-weight bearing quadriceps strengthening exercise on pain and function for people with knee osteoarthritis and obesity: protocol for the TARGET randomised controlled trial. BMC Musculoskelet Disord. 2019;20:291–299. doi: 10.1186/s12891-019-2662-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu F, Cui J, Liu X, Chen KW, Chen X, Li R. The effect of Tai Chi and Qigong exercise on depression and anxiety of individuals with substance use disorders: a systematic review and meta-analysis. BMC Complement Med Ther. 2020;20:161–172. doi: 10.1186/s12906-020-02967-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wayne PM, Lee MS, Novakowski J, Osypiuk K, Ligibel J, Carlson LE, Song R. Tai Chi and Qigong for cancer-related symptoms and quality of life: a systematic review and meta-analysis. J Cancer Surviv. 2018;12:256–267. doi: 10.1007/s11764-017-0665-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chang PS, Knobf T, Oh B, Funk M. Physical and psychological health outcomes of Qigong exercise in older adults: a systematic review and meta-analysis. Am J Chin Med. 2019;47:301–322. doi: 10.1142/S0192415X19500149. [DOI] [PubMed] [Google Scholar]
- 18.Dworkin RH, Turk DC, Trudeau JJ, Benson C, Biondi DM, Katz NP, Kim M. “Validation of the short-form McGill pain questionnaire-2 (SF-MPQ-2) in acute low back pain”. J Pain. 2015;16:357–366. doi: 10.1016/j.jpain.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 19.Tsuji T, Yoon J, Aiba T, Kanamori A, Okura T, Tanaka K. Effects of whole-body vibration exercise on muscular strength and power, functional mobility and self-reported knee function in middle-aged and older Japanese women with knee pain. Knee. 2014;21:1088–95. doi: 10.1016/j.knee.2014.07.015. [DOI] [PubMed] [Google Scholar]
- 20.Rausch Osthoff AK, Juhl CB, Knittle K, Dagfinrud H, Hurkmans E, Braun J, Schoones J, Vliet Vlieland TPM, Niedermann K. Effects of exercise and physical activity promotion: meta-analysis informing the 2018 EULAR recommendations for physical activity in people with rheumatoid arthritis, spondyloarthritis and hip/knee osteoarthritis. RMD Open. 2018;4:e000713. doi: 10.1136/rmdopen-2018-000713. [DOI] [PMC free article] [PubMed] [Google Scholar]


