Abstract
Objective: To explore the value of human papillomavirus (HPV) E6/E7 mRNA detection in the diagnosis of cervical cancer and its precancerous lesions after kidney transplantation. Methods: One hundred and sixty-six women who underwent cervical cancer screening after kidney transplantation were selected and received thinprep cytology test (TCT), HPV DNA and HPV E6/E7 mRNA tests. A biopsy under colposcopy was performed for those with suspicious test results. The positive rates of TCT, HPV DNA and HPV E6/E7 mRNA expressions in patients with different biopsy pathological grades, the positive rates of HPV E6/E7 mRNA in TCT and HPV DNA positive patients were compared. Besides, the relationship between the results of the three detections and the pathological results of cervical biopsy as well as the diagnostic efficacy of cervical cancer and its precancerous lesions were compared. Results: Among the 166 women undergoing cervical cancer screening, 87 cases received histopathological biopsy, of which, the positive expression rates of HPV E6/E7 mRNA in the negative, cervical intraepithelial neoplasia (CIN) I, CIN II, CIN III and invasive carcinoma (ICC) patients were 51.43%, 54.55%, 66.67%, 81.82% and 100.00%, respectively. The positive expression rates of HPV E6/E7 mRNA in TCT and HPV DNA-positive patients were 47.50% and 51.96%, respectively; those rates for diagnosis of ≥CIN II were significantly greater than that of ≤CIN I (both P<0.01). Receiver operating characteristic curve revealed that the areas under the concentration-time curve of TCT, HPV DNA and HPV E6/E7 mRNA detection for cervical cancer and precancerous lesions were 0.723, 0.833, 0.929, respectively. Their sensibilities were 76.89%, 83.30% and 92.38%, and their specificities were 77.04%, 88.47% and 94.47%, respectively. Conclusion: HPV E6/E7 mRNA detection effectively improves the diagnostic sensitivity and specificity of cervical cancer and precancerous lesions, thereby avoiding over-examination and over-treatment.
Keywords: Kidney transplantation, human papillomavirus, E6/E7 mRNA, cervical cancer, precancerous lesions, diagnostic value
Introduction
Cervical cancer is a high incidence malignant tumor type in the female reproductive system. The incidence in China is about two out of 100,000. In 2017, there were about 500,000 new cases of cervical cancer in the world, and China accounted for about 20% [1]. Human papillomavirus (HPV) infection is the main cause of cervical cancer. It has strong epithelial and tissue specificity. There are more than 150 types of HPV, among which, HPV 16, and HPV 18 are the high-risk types [2-4]. Studies have confirmed that overexpression of E6 and E7 in the early reading frame of HPV results in malignant proliferation of cells, which in turn leads to the occurrence of cancer [5,6].
Kidney transplantation is the main treatment for end-stage renal disease. The female patients receiving kidney transplantation were more likely to have HPV than normal women and it takes a long time to recover after surgery due to their poor health [7]. However, some Chinese women do not pay enough attention to HPV opportunistic screening, which was reflected by low detection rates of HPV infections and even cervical cancer [8]. For female patients confronted with cervical cancer without effective treatment in the early stage, their lives were cut short, leaving the costly and hard-won kidney transplantation of little significance. During this period, effective screening of cervical cancer and precancerous lesions for female patients becomes a significant prerequisite for giving early regular treatment optiolns, improving the prognosis, and prolonging their lives [9,10].
At present, there are many studies on HPV E6/E7 in the diagnosis of cervical cancer in normal women, and the results show that HPV E6/E7 mRNA detection is better than TCT detection in the diagnosis of cervical cancer [11]. However, there is no research focusing solely on the diagnostic efficacy of HPV E6/E7 mRNA detection in women with cervical cancer after kidney transplantation. Therefore, this study mainly explores the application value of HPV E6/E7 mRNA detection in the diagnosis of cervical cancer and its precancerous lesions after kidney transplantation.
Materials and methods
Data collection
We selected 166 women who were screened for cervical cancer in our hospital from July 2017 to October 2020 after kidney transplantation. All of them underwent thinprep cytology test (TCT), HPV DNA and HPV E6/E7 mRNA tests. A biopsy under colposcopy was performed for those with suspicious test results. This study was approved by the Ethics Committee of our hospital.
Inclusion criteria: (1) Patients aged from 20 to 70 years old. (2) Patients who received a kidney transplant. (3) Patients who sought medical treatment due to cervical inflammation, abnormal vaginal discharge, and abnormal leukorrhea, and those who volunteered for cervical cancer screening. (4) Patients understood the purpose of this research and signed the informed consent.
Exclusion criteria: (1) Patients who had been previously diagnosed with cervical cancer. (2) Patients who received organ transplants other than kidneys. (3) Patients that could not cooperate to complete TCT, HPV DNA and HPV E6/E7 mRNA tests. (4) Patients who were diagnosed with malignant tumors. (5) Patients that could not accept long-term follow-up. (6) Patients who participated in other research projects at the same time.
Methods
The cervical exfoliated cells at the junction of the squamous column epithelium and the cervical canal were scraped with a special TCT brush to make a thin layer smear, which was Pap stained and examined under an optical microscope. Among them, atypical squamous cells that could not be clearly defined were judged as positive, and vice versa [12].
The HPV special brush was used to scrape the cervical exfoliated cells at the junction of the squamous column epithelium and the cervical canal. HPV DNA detection was performed by fluorescent PCR [13]. All kits were purchased from Shanghai Toujing Life Technology Co., Ltd, China.
The cervical exfoliated cells at the junction of the squamous column epithelium and the cervical canal were scraped with a special TCT brush. A cold light meter (EnSURE™ Touch, Beijing Chuqi Instrument Co., Ltd., China) was adopted for HPV E6/E7 mRNA detection. HPV E6/E7 mRNA ≥1 copy/mL was defined as positive; otherwise, it was negative [14].
Histopathological biopsy was done by an experienced physician. According to the WHO classification criteria, the test results were divided into normal or inflammation (negative), cervical intraepithelial neoplasia (CIN, including CIN I, CIN I, CIN III), and invasive carcinoma (ICC). If there were different levels of diagnosis, the type with the highest pathological level would be the final diagnosis result [15].
Statistical analysis
SPSS 20.0 was used for statistical analysis. Counting data was expressed as n (%) and analyzed by chi-square test. Measurement data was expressed as mean ± standard deviation. P<0.05 was regarded as statistical significance. GraphPad Prism software was adopted for receiver operating characteristic curve (ROC) to analyze the diagnostic efficiency of the TCT, HPV DNA and HPV E6/E7 mRNA detections on cervical cancer and its precancerous lesions.
Results
General data
One hundred and sixty-six enrolled patients, aged 22-63 years old, with an average of (35.4±6.5) years old. The primary diseases leading to end-stage renal failure included chronic glomerulonephritis, diabetic nephropathy, hypertensive nephropathy, polycystic kidney disease, and IgA nephropathy. Some patients had hypertension, diabetes, hyperlipidemia, coronary disease, hepatitis B and tuberculosis. One hundred and forty-four cases of women had a history of childbirth, and 155 cases had sexual activity. See Table 1.
Table 1.
General data
| General data | Details |
|---|---|
| Age (year) | 35.4±6.5 |
| Body mass index (kg/m2) | 22.20±1.74 |
| Primary disease of end-stage renal failure (n) | |
| Chronic glomerulonephritis | 49 |
| Diabetic nephropathy | 37 |
| Hypertensive nephropathy | 34 |
| Polycystic kidney disease | 23 |
| IgA nephropathy | 14 |
| Others | 9 |
| Operation time of kidney transplant (min) | 184.48±25.58 |
| History of childbirth (n) | |
| Yes | 144 |
| No | 22 |
| Sexual activity (n) | |
| Yes | 155 |
| No | 11 |
| Complications (n) | |
| Hypertension | 45 |
| Diabetes | 13 |
| Hyperlipidemia | 8 |
| Coronary disease | 3 |
| Infectious disease (n) | |
| Hepatitis B | 10 |
| Tuberculosis | 3 |
| Monthly income (yuan) | 4,887.78±174.49 |
HPV E6/E7 mRNA expression in patients with different grades of cervical lesions
Among the 166 women undergoing cervical cancer screening, 87 cases received histopathological biopsy, of which, 35 were negative, accounting for 40.23%; 22 were CIN I, accounting for 25.29%; 15 were CIN II, accounting for 17.24%; 11 were CIN III, accounting for 12.64%; 4 were ICC, accounting for 4.60%. The positive expression rates of HPV E6/E7 mRNA in the negative, CIN I, CIN II, CIN II and ICC patients were 51.43%, 54.55%, 66.67%, 81.82% and 100.00%, respectively. See Table 2.
Table 2.
HPV E6/E7 mRNA expression in patients with different grades of cervical lesions (n, %)
| Pathological biopsy outcomes | Case (n) | Rate (%) | Number of HPV E6/E7 mRNA positive cases (n) | Positive rate of HPV E6/E7 mRNA (%) |
|---|---|---|---|---|
| Negative | 35 | 40.23 | 18 | 51.43 |
| CIN I | 22 | 25.29 | 12 | 54.55 |
| CIN II | 15 | 17.24 | 10 | 66.67 |
| CIN III | 11 | 12.64 | 9 | 81.82 |
| ICC | 4 | 4.60 | 4 | 100.00 |
| Total | 87 | 100.00 | 53 | 60.92 |
Note: HPV: human papillomavirus; CIN: cervical intraepithelial neoplasia; ICC: invasive carcinoma.
Expression of HPV E6/E7 mRNA in TCT and HPV DNA-positive patients
Among the 166 women undergoing cervical cancer screening, 80 cases (48.19%) were positive TCT, 38 cases (47.50%) were positive HPV E6/E7 mRNA, 102 cases (61.45%) were positive HPV DNA, and 53 cases (51.96%) were positive HPV E6/E7 mRNA. There were no significant differences in the positive rates of HPV E6/E7 mRNA among TCT and HPV DNA-positive patients (both P>0.05). See Figure 1.
Figure 1.
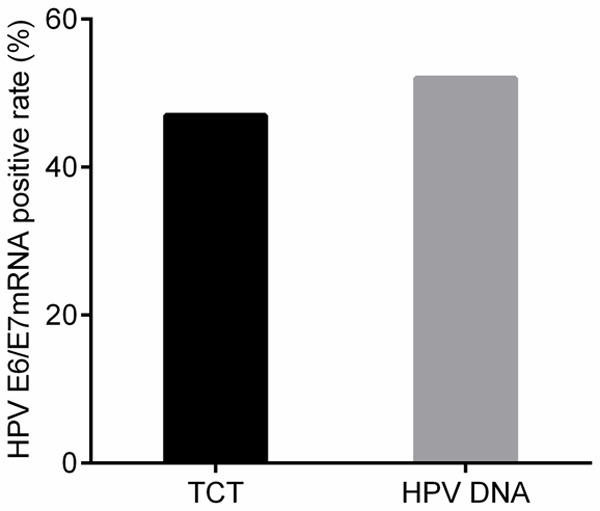
Expression of HPV E6/E7 mRNA in TCT and HPV DNA-positive patients. TCT: thinprep cytology test; HPV: human papillomavirus.
Relationship between the results of the 3 detections and histopathological biopsy
The histopathological biopsy outcomes were divided into ≤CIN I (negative, CIN I) and ≥CIN II (CIN II, CIN III, ICC). Compared with the positive rate of diagnosis of the above two by the three detections of TCT, HPV DNA and HPV E6/E7 mRNA, TCT, HPV DNA had no statistically significant difference in the diagnostic positive rate of ≤CIN I and ≥CIN II (P>0.05), while the positive rate of HPV E6/E7 mRNA for ≥CIN II was significantly greater than ≤CIN I (P<0.01). See Table 3.
Table 3.
Relationship between the results of 3 methods and the results of histopathological biopsy (n, %)
| Histopathological biopsy | χ2 | P | ||
|---|---|---|---|---|
|
| ||||
| ≤CIN I | ≥CIN II | |||
| TCT | 0.036 | 0.850 | ||
| Positive | 24 (27.59) | 12 (13.79) | ||
| Negative | 33 (37.93) | 18 (20.69) | ||
| HPV DNA | 0.431 | 0.511 | ||
| Positive | 30 (34.48) | 18 (20.69) | ||
| Negative | 27 (31.03) | 12 (13.79) | ||
| HPV E6/E7 mRNA | 10.827 | 0.001 | ||
| Positive | 29 (33.33) | 26 (29.89) | ||
| Negative | 28 (32.18) | 4 (4.60) | ||
Note: HPV: human papillomavirus; TCT: thinprep cytology test; CIN: cervical intraepithelial neoplasia.
Diagnostic efficacy of the 3 detections for cervical cancer and precancerous lesions
ROC curve revealed that the areas under the concentration-time curve of TCT, HPV DNA and HPV E6/E7 mRNA detections for cervical cancer and precancerous lesions were 0.723, 0.833, 0.929, respectively. Their sensibilities were 76.89%, 83.30% and 92.38%, and their specificities were 77.04%, 88.47% and 94.47%, respectively. See Table 4.
Table 4.
Diagnostic efficacy of 3 methods for cervical cancer and precancerous lesions
| Items | TCT | HPV DNA | HPV E6/E7 mRNA |
|---|---|---|---|
| AUC | 0.723 | 0.833 | 0.929 |
| 95% confidence interval | 0.602-0.864 | 0.723-0.926 | 0.836-0.977 |
| Sensibility (%) | 76.89 | 83.30 | 92.38 |
| Specificity (%) | 77.04 | 88.47 | 94.47 |
Note: AUC: area under the concentration-time curve; TCT: thinprep cytology test; HPV: human papillomavirus.
Discussion
In China, cervical cancer is a malignant tumor of the female reproductive system with a high incidence, which is mainly caused by persistent HPV infection [13,14]. The female patients receiving kidney transplantation were more likely to be infected with HPV than normal women due to their poor overall health. There has been HPV opportunistic screening in China, but some women do not pay enough attention to it, resulting in low detection rate of HPV infections and even cervical cancer [15]. The use of appropriate test methods to improve the detection rate of cervical cancer and precancerous lesions plays an important role in improving the quality of life of women after kidney transplantation.
The main purpose of this study is to explore the diagnostic value of TCT, HPV DNA and HPV E6/E7 mRNA in the diagnosis of cervical cancer and precancerous lesions in women after kidney transplantation. Histopathological biopsy was considered as the gold standard, to analyze HPV E6/E7 mRNA expression in patients with different grades of cervical lesions. It was found that among 87 cases that received histopathological biopsy, the positive expression rates of HPV E6/E7 mRNA in the CIN I, CIN II, CIN III and ICC patients were 54.55%, 66.67%, 81.82% and 100.00%, suggesting the higher the level of cervical lesions, the higher the positive expression rate of HPV E6/E7 mRNA, which was consistent with the results reported by Liu et al. [16,17]. HPV is the general term for human papillomavirus. In more than 150 types, different types of HPV viruses cause different diseases. Among them, HPV 16 and HPV 18 are the main HPV types that induce cervical cancer and cervical intraepithelial lesions [16]. TCT and HPV DNA are the main screening methods for early cervical cancer and precancerous lesions. However, the limited diagnostic efficacy of TCT easily leads to missed diagnosis or misdiagnosis situation [18,19]. HPV DNA detection has significantly increased the detection rate of cervical cancer and precancerous lesions but it has less specificity. Because only a small part of HPV infection will eventually lead to the occurrence of cervical cancer and precancerous lesions; HPV DNA detection fails to reflect the carcinogenic activity of the virus which is to blame for overtreatment [20]. E6 and E7 genes are the main types of genes that induce cervical cancer. After the body is infected with high-risk HPV types, E6 and E7 are expressed wildly as the main oncogenes, producing E6 and E7 early oncoproteins, which affects the normal regulation of the body’s cell cycle and eventually lead to cancer [21]. The genetic information of DNA needs to be transcribed to mRNA and then translated into protein through mRNA. Therefore, the expression of HPV mRNA can be detected to reflect oncogene activity.
In this study, the positive expression rates of HPV E6/E7 mRNA in TCT and HPV DNA-positive patients were 47.50% and 51.96%, demonstrating that HPV E6/E7 mRNA was not necessarily positive for TCT and HPV DNA-positive patients. This laid the foundation for the next step in the diagnosis of the three detection methods. Subsequently, it was found that the diagnostic positive rate of HPV E6/E7 mRNA for ≥CIN II was significantly greater than ≤CIN I, which proved that HPV E6/E7 mRNA had a higher diagnostic value for cervical cancer and precancerous lesions again.
In order to further analyze the value of HPV E6/E7 mRNA in the diagnosis of early cervical cancer and precancerous lesions in women undergoing kidney transplantation, this study analyzed the ROC curve. It revealed that the areas under the concentration-time curve of TCT, HPV DNA and HPV E6/E7 mRNA in the diagnosis of cervical cancer and precancerous lesions were 0.723, 0.833, and 0.929, indicating that TCT, HPV DNA and HPV E6/E7 mRNA tests had diagnostic value on cervical cancer and precancerous lesions. What was more, the sensitivity and specificity of HPV E6/E7 mRNA in the diagnosis of cervical cancer and precancerous lesions were 92.38% and 94.47%, respectively, which were significantly higher than the detection of TCT and HPV DNA. It demonstrated that HPV E6/E7 mRNA detection has higher diagnostic value for cervical cancer and precancerous lesions in women after kidney transplantation, and its diagnostic efficiency was better than TCT and HPV DNA detections, which was consistent with the report from Dupin et al. This may be because HPV mRNA detection is a genetic level detection [22].
However, this study is only an analysis of the diagnostic effect of cervical cancer screening in 166 women after kidney transplantation, and it has not been compared with the screening of normal women for cervical cancer. This will be the focus of the later research to determine whether kidney transplantation will affect HPV E6/E7 mRNA screening for cervical cancer.
In summary, the higher the level of cervical lesions was, the higher the positive expression rate of HPV E6/E7 mRNA. HPV E6/E7 mRNA detection has higher diagnostic value for cervical cancer and precancerous lesions in women after kidney transplantation. Therefore, HPV E6/E7 mRNA detection can be used to diagnose cervical cancer and precancerous lesions to avoid excessive examination and treatment.
Acknowledgements
This work was supported by the Science and Technology Project of Yinzhou District Social and Agricultural Development (2019AS0023).
Disclosure of conflict of interest
None.
References
- 1.Tsikouras P, Zervoudis S, Manav B, Tomara E, Iatrakis G, Romanidis C, Bothou A, Galazios G. Cervical cancer: screening, diagnosis and staging. J BUON. 2016;21:320–325. [PubMed] [Google Scholar]
- 2.Olusola P, Banerjee HN, Philley JV, Dasgupta S. Human papilloma virus-associated cervical cancer and health disparities. Cells. 2019;8:622–625. doi: 10.3390/cells8060622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hu Z, Ma D. The precision prevention and therapy of HPV-related cervical cancer: new concepts and clinical implications. Cancer Med. 2018;7:5217–5236. doi: 10.1002/cam4.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johnson CA, James D, Marzan A, Armaos M. Cervical cancer: an overview of pathophysiology and management. Semin Oncol Nurs. 2019;35:166–174. doi: 10.1016/j.soncn.2019.02.003. [DOI] [PubMed] [Google Scholar]
- 5.Wang R, Pan W, Jin L, Huang W, Li Y, Wu D, Gao C, Ma D, Liao S. Human papillomavirus vaccine against cervical cancer: opportunity and challenge. Cancer Lett. 2020;471:88–102. doi: 10.1016/j.canlet.2019.11.039. [DOI] [PubMed] [Google Scholar]
- 6.Argyri E, Tsimplaki E, Daskalopoulou D, Stravopodis DJ, Kouikoglou O, Terzakis E, Panotopoulou E. E6/E7 mRNA expression of high-risk HPV types in 849 Greek women. Anticancer Res. 2013;33:4007–4011. [PubMed] [Google Scholar]
- 7.Angell J, Dodds N, Darweish-Mednuik AM, Lewis S, Pyke M, Mitchell DC, Hamilton K, White P, Tolchard S. Characterising recovery from renal transplantation and live-related donation using cardiopulmonary exercise testing. Disabil Rehabil. 2019 doi: 10.1080/09638288.2019.1674387. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 8.Maver PJ, Poljak M. Primary HPV-based cervical cancer screening in Europe: implementation status, challenges, and future plans. Clin Microbiol Infect. 2020;26:579–583. doi: 10.1016/j.cmi.2019.09.006. [DOI] [PubMed] [Google Scholar]
- 9.Keeling E, Murray SL, Williams Y, Sexton DJ, O’Kelly P, Deady S, O’Leary E, Dorman A, Roche M, Ni Raghallaigh S, McCormick A, Moloney FJ, O’Neill JP, Conlon PJ. Merkel cell carcinoma in kidney transplant recipients in Ireland 1964-2018. Br J Dermatol. 2019;181:1314–1315. doi: 10.1111/bjd.18218. [DOI] [PubMed] [Google Scholar]
- 10.Klitzke S, Wender IO, Salcedo MP, Pessini SA. Cervical cancer screening abnormalities in immunosuppressed renal transplant women: case-control study in Southern Brazil. Arch Gynecol Obstet. 2020;302:649–655. doi: 10.1007/s00404-020-05621-3. [DOI] [PubMed] [Google Scholar]
- 11.Hoppe-Seyler K, Bossler F, Braun JA, Herrmann AL, Hoppe-Seyler F. The HPV E6/E7 oncogenes: key factors for viral carcinogenesis and therapeutic targets. Trends Microbiol. 2018;26:158–168. doi: 10.1016/j.tim.2017.07.007. [DOI] [PubMed] [Google Scholar]
- 12.Liu Y, Zhang L, Zhao G, Che L, Zhang H, Fang J. The clinical research of thinprep cytology test (TCT) combined with HPV-DNA detection in screening cervical cancer. Cell Mol Biol (Noisy-le-grand) 2017;63:92–95. doi: 10.14715/cmb/2017.63.2.14. [DOI] [PubMed] [Google Scholar]
- 13.Chera BS, Kumar S, Shen C, Amdur R, Dagan R, Green R, Goldman E, Weiss J, Grilley-Olson J, Patel S, Zanation A, Hackman T, Blumberg J, Patel S, Thorp B, Weissler M, Yarbrough W, Sheets N, Mendenhall W, Tan XM, Gupta GP. Plasma circulating tumor HPV DNA for the surveillance of cancer recurrence in HPV-associated oropharyngeal cancer. J. Clin. Oncol. 2020;38:1050–1058. doi: 10.1200/JCO.19.02444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gustinucci D, Giorgi Rossi P, Cesarini E, Broccolini M, Bulletti S, Carlani A, D’angelo V, D’amico MR, Di Dato E, Galeazzi P, Malaspina M, Martinelli N, Spita N, Tintori B, Giaimo MD, Passamonti B. Use of cytology, E6/E7 mRNA, and p16INK4a-Ki-67 to define the management of human papillomavirus (HPV)-positive women in cervical cancer screening. Am J Clin Pathol. 2016;145:35–45. doi: 10.1093/ajcp/aqv019. [DOI] [PubMed] [Google Scholar]
- 15.Motaparthi K, Kapil JP, Velazquez EF. Cutaneous squamous cell carcinoma: review of the eighth edition of the american joint committee on cancer staging guidelines, prognostic factors, and histopathologic variants. Adv Anat Pathol. 2017;24:171–194. doi: 10.1097/PAP.0000000000000157. [DOI] [PubMed] [Google Scholar]
- 16.Clifford GM, Tully S, Franceschi S. Carcinogenicity of human papillomavirus (HPV) types in HIV-positive women: a meta-analysis from hpv infection to cervical cancer. Clin Infect Dis. 2017;64:1228–1235. doi: 10.1093/cid/cix135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu TY, Xie R, Luo L, Reilly KH, He C, Lin YZ, Chen G, Zheng XW, Zhang LL, Wang HB. Diagnostic validity of human papillomavirus E6/E7 mRNA test in cervical cytological samples. J Virol Methods. 2014;196:120–125. doi: 10.1016/j.jviromet.2013.10.032. [DOI] [PubMed] [Google Scholar]
- 18.Liang H, Fu M, Zhou J, Song L. Evaluation of 3D-CPA, HR-HPV, and TCT joint detection on cervical disease screening. Oncol Lett. 2016;12:887–892. doi: 10.3892/ol.2016.4677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen JY, Wang ZL, Wang ZY, Yang XS. The risk factors of residual lesions and recurrence of the high-grade cervical intraepithelial lesions (HSIL) patients with positive-margin after conization. Medicine (Baltimore) 2018;97:127–129. doi: 10.1097/MD.0000000000012792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saeed M, Alshammari FD, Alam MJ, Sarim KM, Ahmad K, Hussain T, Khan M, Kamal MA, Kausar MA, Alkreathy HM, Faisal SM, Ashraf GM. A synopsis on the role of human papilloma virus infection in cervical cancer. Curr Drug Metab. 2018;19:798–805. doi: 10.2174/1389200219666180302160317. [DOI] [PubMed] [Google Scholar]
- 21.Pan D, Zhang CQ, Liang QL, Hong XC. An efficient method that combines the ThinPrep cytologic test with E6/E7 mRNA testing for cervical cancer screening. Cancer Manag Res. 2019;11:4773–4780. doi: 10.2147/CMAR.S197749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dupin C, Siproudhis L, Henno S, Minjolle S, Arvieux C, Tattevin P. Use of human papillomavirus genotyping and biomarkers for targeted screening of anal dysplasia in human immunodeficiency virus-infected patients. Dig Liver Dis. 2015;47:423–428. doi: 10.1016/j.dld.2015.01.150. [DOI] [PubMed] [Google Scholar]


