Abstract
Objective: To explore the effect of multidisciplinary collaborative continuous nursing on the psychological state and quality of life of cervical cancer patients. Methods: A total of 132 patients with cervical cancer who were hospitalized in our hospital were selected as the research subjects, and they were randomized into the observation group (n=66) and the control group (n=66). The control group was given regular continuous nursing, while the observation group was given three-month multidisciplinary collaborative continuous nursing. It was conducted through WeChat, telephone follow-up, face-to-face consultation and lectures, giving guidance on diet, medication, pain control, psychological health, self-care, review time, recognition and processing of postoperative complications, daily activities, social behaviors and so on. Patients’ anxiety, depression, quality of life, cancer-related fatigue, complication incidence, and sleep quality were compared between the two groups. Results: Self-rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS) were applied for evaluation. The anxiety and depression scores of patients in the observation group were significantly lower than those in the control group (both P<0.001). The scores on physical functioning, general health, social role functioning, emotional role functioning, and mental health, in the observation group were higher than those in the control group (all P<0.01). Compared with patients in the control group, those in the observation group had higher scores on behavioral/severity, affective meaning, sensory and cognition/mood (all P<0.001). Patients in the observation group had lower complication incidence of postoperative nausea, abdominal pain, wound infection and intestinal obstruction (P<0.05). Besides, the sleep quality scores of patients in the observation group were also lower than those in the control group (all P<0.001). Conclusion: The application of multidisciplinary collaborative continuous nursing for patients with cervical cancer is effective. It can improve patients’ depression, anxiety, quality of life, cancer-related fatigue, sleep quality, and reduce the incidence of complications. Therefore, it is worthy of clinical application and promotion.
Keywords: Cervical cancer, multidisciplinary collaboration, continuous nursing, quality of life, psychological state
Introduction
Cervical cancer is a common gynecological malignant tumor in the female reproductive tract which originates from the cervix [1,2]. The cause is complicated, and it is closely related to factors such as HPV virus infection, sexual behaviors, times of childbirths, infections of pathogens such as Chlamydia trachomatis and trichomoniasis, smoking, malnutrition, and bad sanitation [3]. Some research has revealed that there are about 500,000 cases of cervical cancer, each year around the world, and more than 260,000 women die of cervical cancer annually, mainly in developing countries. It ranks second among female malignancies and those affected tend to be younger females [4]. The onset of the disease is insidious, and in most cases, it doesn’t cause any noticeable symptoms in the early stages. As the disease progresses, its manifestation can be noticed as contact bleeding and abnormal bleeding and discharge from the vagina. When the disease develops to an advanced stage, the prognosis is bad, which can threaten life [5]. At present, the main treatment for cervical cancer include surgery, radiation therapy, chemotherapy, and drug therapy [6]. However, there many complications after surgery such as postoperative bleeding, vaginal stump dehiscence, vaginal stump bleeding, vesicovaginal fistula, rectovaginal fistula, urinary fistula, pulmonary infection, stress-induced gastric ulcer, lower extremities deep vein thrombosis are extremely likely to occur. What’s worse, the severe physical and mental trauma caused by the decline of the physical functioning brought on by the disease makes patients highly vulnerable to negative emotions such as anxiety, fear and sense of loss. It enormously affects their recovery, psychological health and quality of life [7]. Therefore, alleviating depression and anxiety and improving the quality of life and mental health of patients has become the focus of postoperative nursing.
Continuous nursing can meet patients’ needs on health care and psychological support after discharge and promote recovery, since it provides systemic services such as medical treatment, nursing, rehabilitation promotion, and health guidance for patients after discharge [8,9]. Multidisciplinary collaborative continuous nursing is the application of multidisciplinary collaboration concept to continuous nursing, complementing each other for the limitations of the professional skills of nursing staff. It aims to provide patients with a comprehensive and high-quality nursing service [10]. Although there are some reports on the application of multidisciplinary collaborative continuous nursing for patients with cervical cancer, they have not focused on the patients’ psychological state, sleep quality and cancer-related fatigue [11]. This study mainly explores the application effect of multidisciplinary collaborative continuous nursing on improving the psychological state and quality of life of patients after cervical cancer surgery.
Materials and methods
Generation information
A total of 132 patients with cervical cancer hospitalized and operated on in our hospital from May 12, 2019 to June 30, 2020 were selected as the research subjects, and they were randomized into the observation group (n=66) and control group (n=66). This study was approved by the Medical Ethics Committee of our hospital.
Inclusion criteria were as follows: patients who met the diagnostic criteria for cervical cancer [12]. Patients aged >18 years old; Patients who needed surgery; Patients who agreed to participate in this study and signed an informed consent.
Exclusion criteria were as follows: patients with cancer metastasis; patients with dysfunction of important organs or systemic infectious diseases; patients with a history of mental illness or cognitive impairment; patients with metastatic cervical cancer that can only be treated with palliative treatment and cannot tolerate operation; patients with other malignant tumors.
Methods
During hospitalization, the two groups of patients received the same nursing, including postoperative complication prevention, diet guidance, and condition monitoring. However, after being discharged from the hospital, the two groups of patients were treated with different continuous nursing.
Patients in the control group were given regular discharge guidance and continuous nursing including telephone follow-up once every week to acquire the existing problems and providing guidance.
Patients in the observation group received a multidisciplinary collaborative continuous nursing in addition to the nursing measures taken in the control group. The specific measures include: (1) Establishing a multidisciplinary collaborative continuous nursing team consisting of 10 medical staff, including 3 doctors (1 chief physician, 2 attending physicians), 1 dietitian, 1 pharmacist, 1 psychological counselor, 1 sex counselor, 1 head nurse and 2 nurses in charge. (2) Collecting basic data of patients and making continuous nursing files. (3) Responsibility of team members: doctors were responsible for answering questions about patients’ postoperative wounds, such as redness and swelling, and other surgical and disease-related problems; pharmacists were responsible for formulating medication plans for patients; psychological counselors were responsible for patients’ psychological problems; dieticians were responsible for formulating dietary prescriptions; the head nurse was responsible for coordinating and arranging the work of the team members to ensure the progress and its quality; the nurse in charge was responsible for guiding patients and their families in home self-care, health education, and making of follow-up files. (4) Formulating a multidisciplinary collaborative continuous nursing plan and implementing nursing work in accordance with the plan (the content of the telephone follow-up was determined three days after the team was formed; messages needing to be sent in the WeChat group were discussed one day in advance; the main content of the family visit was determined 5 days before the family visit; a special lecture was arranged 10 days after the establishment of the team). (5) Establishing a WeChat group of multidisciplinary collaborative continuous nursing. Group members share knowledge about cervical cancer-related rehabilitation, diet, and self-care in the group every day, and give professional advice to patient consultations. (6) Telephone follow-up. According to the plan, a telephone follow-up and record was done every 5 days, with follow-up questions about postoperative recovery, mental state, review time, medication, etc. (7) Family visit. A professional team was established including 5 members, a doctor, a nurse, a psychological counselor, a dietician and a pharmacist. Family visit was implemented once every 2 weeks. They would communicate with patients face to face according to WeChat conversations, telephone follow-up and personal situations. The family visit conversations focused on dietary guidance, medication guidance, pain control, mental health, self-care knowledge, review time, discernment and treatment of postoperative complications, daily behaviors, social behavior etc. (8) Special lectures. Special lectures on health education were held in the hospital every month. (9) Nursing effect evaluation. Nursing intervention was evaluated every 2 weeks and the nursing plan was adjusted if necessary.
Outcome measures
Main outcome measures
(1) The anxiety status of patients in the two groups was compared three months after discharge. Self-rating Anxiety Scale (SAS) was used to assess the anxiety of patients [13]. SAS score ≥50 points indicated existence of anxiety symptoms, and the scores were positively corelated with the anxiety degree. (2) The depression status of patients in the two groups was compared three months after discharge. Self-rating Depression Scale (SDS) was applied to evaluate the depression status of patients (scores from 53 to 62 points indicating mild depression; 63 to 72 representing moderate depression; scores over 73 points falling on severe depression). The scores were positively corelated with the degree of depression [14]. (3) The quality of life of patients in the two groups was compared three months after discharge. MOS SF-36 was used to measure the quality of life of the patients. It included 5 sections: physical functioning, general health, social role functioning, emotional role functioning, and mental health. The full score of all sections is 100 points. A higher score represented better quality of life in each relevant section [15].
Secondary outcome measures
(1) Cancer-related fatigue of patients in the two groups was compared. Piper Fatigue Scale (PFS) was used to measure the four dimensions of patients’ cancer-related fatigue, which included behavioral/severity, affective meaning, sensory and cognition/mood. Scores were positively corelated with the degree of cancer-related fatigue [16]. (2) Incidence of complication of patients between two groups was compared one month after discharge, with complications including nausea, abdominal pain, wound infection, intestinal obstruction and others. If multiple complications occurred in the same patient, they were all counted in total cases of complications. Total incidence equals number of complication cases/total number of cases ×100%. (3) Sleep quality of patients between two groups was compared by the Pittsburgh Sleep Quality Index (PSQI). Higher scores represented worse sleep quality [17,18].
Statistical analysis
SPSS 20.0 was chosen for statistical analysis. Count data was expressed as n/%, and performed by χ2 test; Measurement data conforming to a normal distribution were expressed as mean ± standard deviation (x̅ ± sd). Independent t test was applied to comparison between groups. Data which did not conform to a normal distribution was expressed as the median. Rank sum test was implemented for comparison between groups. The difference was statistically significant at P<0.05.
Results
Comparison of general information of patients between the two groups
During the time of this study, there were no patients lost to follow-up or who dropped out in either group.
There was no statistically significant difference between patients of the two groups in age, pathological type, FIGO 2009 stage, comorbidities, and surgical methods (P>0.05). Therefor the two groups were comparable. See Table 1 in detail.
Table 1.
Comparison of general information of patients between the two groups (n, x̅ ± sd)
| Indexes | Observation group (n=66) | Control group (n=66) | χ2/t | P |
|---|---|---|---|---|
| Age (years) | 44.4±8.2 | 45.5±7.9 | 0.808 | 0.420 |
| Pathological type | 0.214 | 0.898 | ||
| Squamous cell carcinomas | 55 | 53 | ||
| Adenocarcinoma | 7 | 8 | ||
| Squamous adenocarcinoma | 4 | 5 | ||
| FIGO 2009 stages | 0.461 | 0.927 | ||
| Ia | 13 | 12 | ||
| Ib | 6 | 7 | ||
| IIa | 46 | 45 | ||
| IIb | 1 | 2 | ||
| Comorbidities | ||||
| Hypertension | 8 | 10 | 0.257 | 0.612 |
| Uterine fibroids | 7 | 6 | 0.085 | 0.770 |
| Surgical methods | 0.527 | 0.912 | ||
| Lower cervical coning and cervical annulus | 11 | 12 | ||
| Hysterectomy | 12 | 13 | ||
| Hysterectomy and adnexectomy | 1 | 2 | ||
| Extensive hysterectomy | 42 | 39 |
Note: FIGO: International Federation of Gynecology and Obstetrics.
Comparison of anxiety of patients between the two groups
SAS score of the observation group was lower than that of the control group (47.16±5.41 vs. 51.15±5.12; t=4.352, P<0.001). See Figure 1.
Figure 1.
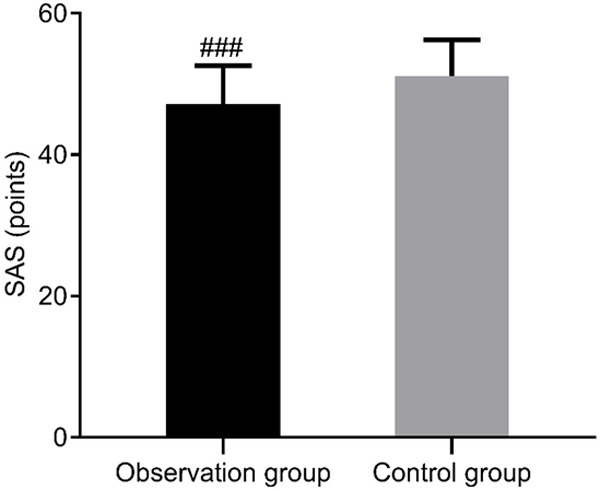
Comparison of SAS scores of patients between two groups. Compared with the control group, ###P<0.001. SAS: Self-rating Anxiety Scale.
Comparison of depression in patients between the two groups
SDS score of the observation group was lower than that of the control group (47.89±5.60 vs. 53.87±5.87; t=5.988, P<0.001). See Figure 2.
Figure 2.
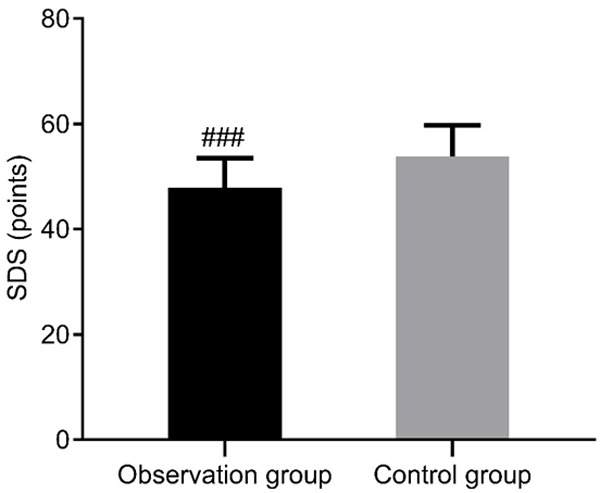
Comparison of SDS scores of patients between two groups. Compared with the control group, ###P<0.001. SDS: Self-rating Depression Scale.
Comparison of the quality of life between patients in the two groups
Compared with patients in the control group, the scores of physical functioning, general health, social role functioning, emotional role functioning and mental health of those in the observation group were higher (all P<0.01). See Table 2.
Table 2.
Comparison of MOS SF-36 for the quality of life score between the two groups (score, x̅ ± sd)
| Indexes | Observation group (n=66) | Control group (n=66) | t | P |
|---|---|---|---|---|
| Physical functioning | 78.17±10.23 | 65.88±9.21 | 7.253 | 0.000 |
| General health | 91.62±10.23 | 85.05±12.11 | 3.367 | 0.001 |
| Social role functioning | 72.31±11.20 | 65.83±10.22 | 3.472 | 0.001 |
| Emotional role functioning | 63.76±9.18 | 55.52±7.21 | 5.735 | 0.000 |
| Mental health | 68.23±10.20 | 57.34±7.21 | 7.083 | 0.000 |
Comparison of cancer-related fatigue of patients between the two groups
Compared with patients in the control group, those in the observation group had lower scores on behavioral/severity, affective meaning, sensory and cognition/mood (all P<0.001). See Table 3.
Table 3.
Comparison of cancer-related fatigue of patients between the two groups (score, x̅ ± sd)
| Cancer-related fatigue | Observation group (n=66) | Control group (n=66) | t | P |
|---|---|---|---|---|
| Behavioral/severity | 2.16±0.32 | 5.10±0.95 | 23.826 | 0.000 |
| Affective meaning | 1.95±0.22 | 5.10±0.81 | 30.489 | 0.000 |
| Sensory | 1.80±0.23 | 4.83±0.74 | 31.766 | 0.000 |
| Cognition/mood | 2.15±0.21 | 5.50±0.90 | 29.448 | 0.000 |
Comparison of postoperative adverse reactions of patients between the two groups
In the observation group, there were 3 cases of nausea and 2 cases of abdominal pain. The total incidence of complications was 7.58%. In the control group, there were 7 cases of nausea, 3 cases of abdominal pain, 3 cases of wound infection, and 1 case of intestinal obstruction. The total incidence of complications was 21.21%. The total incidence of complications in the observation group was significantly lower than that in the control group (P<0.05). See Table 4.
Table 4.
Comparison of postoperative adverse reactions of patients between the two groups (n, %)
| Groups | Nausea | Abdominal pain | Wound infection | Intestinal obstruction | Incidence of complications |
|---|---|---|---|---|---|
| Observation group (n=66) | 3 | 2 | 0 | 0 | 7.58 |
| Control group (n=66) | 7 | 3 | 3 | 1 | 21.21 |
| χ2 | 1.730 | 0.210 | 3.072 | 1.011 | 4.980 |
| P | 0.188 | 0.648 | 0.079 | 0.315 | 0.025 |
Comparison of sleep quality of patients between the two groups
Compared with patients in the control group, patients in the observation group had lower score on PSQI (10.95±2.11 vs. 14.70±3.41; t=7.597, P<0.001). See Figure 3.
Figure 3.
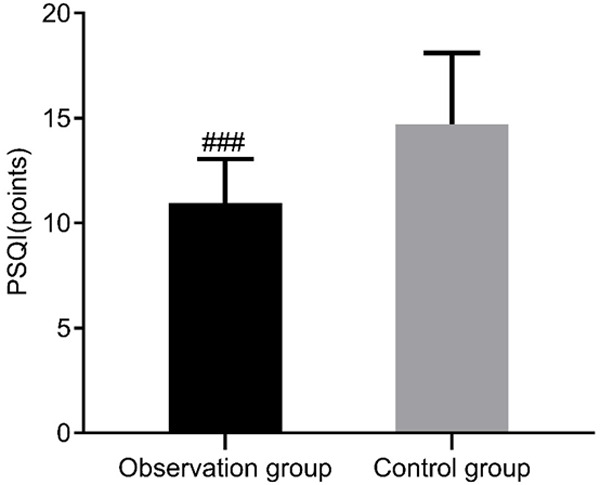
Comparison of PSQI scores of patients between two groups. Compared with the control group, ###P<0.001. PSQI: Pittsburgh Sleep Quality Index.
Discussion
Since 2007, scholars in China have applied continuous nursing to out-of-hospital care for patients with chronic and surgical diseases, which has achieved good results. It can reduce the recurrence rate and improve the prognosis of patients as well as the quality of care [19,20]. Multidisciplinary collaborative continuous nursing refers to a series of standardized, individualized, and comprehensive continuous nursing services formulated from a multidisciplinary perspective to improve the prognosis of patients. The concept of multidisciplinary collaboration, combined with continuous nursing has been widely applied to clinical nursing and has achieved positive effects [21,22].
Anxiety and depression are the most common psychological states of patients with cervical cancer after surgery. The inability to deal with negative emotions may affect the patient’s rehabilitation. Zhao et al. took 80 patients undergoing radical mastectomy as research subjects [23]. In their study, patients in the control group received regular postoperative intervention, while those in the observation group underwent a multidisciplinary collaborative model to continuous nursing. It found that the SAS score and SDS score of patients in the observation group were significantly lower than those in the control group. In this study, the observation group was given multidisciplinary collaborative continuous nursing and it was compared with the regular continuous nursing in the control group. The results showed that the SAS and SDS scores of the observation group were lower than those of the control group, indicating that multidisciplinary collaborative continuous nursing can reduce patient’s anxiety which may be due to the supportive psychotherapy, behavioral therapy, family therapy and other methods for psychological consultation and psychotherapy carried out by the professional psychologists from our multidisciplinary team. Those nursing measures improved the patient’s negative emotions and psychological state.
Besides, multidisciplinary collaborative continuous nursing is of great significance for improving the quality of life of patients. He et al. took 100 patients with cervical cancer as the research subjects and randomized them into an observation group and a control group [11]. The control group was given regular nursing after discharge. The observation group received an intervention of multidisciplinary team care based on the nursing measures performed in control group. This demonstrated that multidisciplinary collaborative continuous nursing is beneficial to improve the quality of life of patients. In this study, the scores of all aspects of the quality of life of patients in the observation group were higher than those of the control group, suggesting that the quality of life of patients in the observation group was better than that in the control group. It once again proved the advantages of multidisciplinary collaborative to continuous nursing, which is consistent with the abovementioned research results.
Cancer-related fatigue is one of the common symptoms of cervical cancer. It is a disturbing, persistent physical, emotional and/or cognitive subjective feeling of fatigue and energy exhaustion caused by tumors or anti-tumor treatments, which influence patients’ daily life activities. The symptoms are non-specific weakness, general weakness, decline of physical functioning, lethargy, fatigue, and its incidence reaches from 50% to 95%, which can lead to negative coping strategies, emotions and affect the enthusiasm of patients to cooperate with treatment [24,25]. In this study, PFS was used to evaluate the cancer-related fatigue of the two groups of patients. We found that the scores of behavioral/severity, affective meaning, sensory and cognitive/mood of patients in the observation group were significantly lower than those of the control group. This suggests that multidisciplinary collaborative continuous nursing can alleviate patients’ cancer-related fatigue and enable patients to actively face the disease. In addition, the sleep quality scores of the observation group were lower than those of the control group, showing that the sleep quality of patients in the observation group was better than that in the control group, which proves that multidisciplinary collaborative continuous nursing can improve the sleep quality of patients.
Apart from the cancer-related fatigue, complications are inevitable after surgery and will have a greater negative impact on the prognosis. In this study, the total incidence of complications in the observation group is lower than that in the control group, displaying that multidisciplinary collaborative continuous nursing can reduce the incidence of adverse reactions such as nausea, abdominal pain, wound infection, and intestinal obstruction after cervical cancer surgery, which is of positive significance for early recovery of patients. However, this study did not observe the negative emotions and quality of life of the patients’ family members. Research with large samples of long-term care effect should be carried out in the future to confirm the feasibility and importance of the multidisciplinary collaborative continuous nursing in cervical cancer patients.
To sum up, multidisciplinary collaborative continuous nursing applied to patients with cervical cancer has a good effect. It can improve patients’ depression, anxiety, quality of life, cancer-related fatigue, patients’ sleep quality, and reduce the incidence of complications. Therefore, it is worthy of clinical application and promotion.
Acknowledgements
This work was supported by the Research and Development Fund of The First Affiliated Hospital of Xi’an Jiaotong University (2018HL02).
Disclosure of conflict of interest
None.
References
- 1.Zhang QJ, Di CX, Yan JF, Wang F, Qu T, Wang YP, Chen YH, Zhang XT, Liu Y, Yang HY, Zhang H. Inhibition of SF3b1 by pladienolide B evokes cycle arrest, apoptosis induction and p73 splicing in human cervical carcinoma cells. Artif Cells Nanomed Biotechnol. 2019;47:1273–1280. doi: 10.1080/21691401.2019.1596922. [DOI] [PubMed] [Google Scholar]
- 2.Horn LC, Höhn AK, Hentschel B, Fischer U, Bilek K, Brambs CE. Prognostic relevance of low-grade versus high-grade FIGO IB1 squamous cell uterine cervical carcinomas. J Cancer Res Clin Oncol. 2019;145:457–462. doi: 10.1007/s00432-018-2793-3. [DOI] [PubMed] [Google Scholar]
- 3.Li XS, Wu SD, Li DC, Yu T, Zhu HX, Song YL, Meng LM, Fan HX, Xie LZ. Intravoxel incoherent motion combined with dynamic contrast-enhanced perfusion MRI of early cervical carcinoma: correlations between multimodal parameters and HIF-1α expression. J Magn Reson Imaging. 2019;50:918–929. doi: 10.1002/jmri.26604. [DOI] [PubMed] [Google Scholar]
- 4.da Silva VTM, Fortuna Diniz AP, Martins J, Cursino K, Esteves SCB, Teixeira JC. Use of interstitial brachytherapy in pelvic recurrence of cervical carcinoma: clinical response, survival, and toxicity. Brachytherapy. 2019;18:146–153. doi: 10.1016/j.brachy.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Zheng M, Zhou Q, Liu XG, Wang CZ, Liu GL. CTHRC1 overexpression promotes cervical carcinoma progression by activating the Wnt/PCP signaling pathway. Oncol Rep. 2019;41:1531–1538. doi: 10.3892/or.2019.6963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lund KV, Simonsen TG, Kristensen GB, Rofstad EK. Pharmacokinetic analysis of DCE-MRI data of locally advanced cervical carcinoma with the brix model. Acta Oncol. 2019;58:828–837. doi: 10.1080/0284186X.2019.1580386. [DOI] [PubMed] [Google Scholar]
- 7.Düzgüne N, Cheung J, Konopka K. Suicide gene therapy of oral squamous cell carcinoma and cervical carcinoma in vitro: methods and protocols. Methods Mol Biol. 2019;1895:177–184. doi: 10.1007/978-1-4939-8922-5_14. [DOI] [PubMed] [Google Scholar]
- 8.Tang YF, Gu ZJ, Yin XG, Xing SS, Zhao J. Meta analysis of the effect of continuous nursing on chronic wound treatment. J Nurs Manag. 2018;18:538–542. [Google Scholar]
- 9.Fu MY, Lu L, Zhang YX, Zhou J. The influence of continuous nursing intervention on the compliance, quality of life and complications of patients with acute myocardial infarction after PCI. J Guangxi Med Univ. 2018;35:415–418. [Google Scholar]
- 10.Yan XM, Sun W, Han Y, Su JP. Application of multidisciplinary cooperative continuous nursing guided by nursing outcomes in patients after radical resection of esophageal cancer. Nurs Res. 2018;32:122–126. [Google Scholar]
- 11.He XL, Yang SP, Min LH, Chen YW, Li F. The effect of group health management in the continuous nursing of cervical cancer patients under multi-disciplinary cooperation. J Clinl Pract Hosp. 2020;17:166–169. [Google Scholar]
- 12.Kong BH. Standardizing the diagnostic procedure and defining the diagnostic standard of diagnosis of cervical cancer. Chin Health Stand Manag. 2012;4:64–67. [Google Scholar]
- 13.Dunstan DA, Scott N, Todd AK. Screening for anxiety and depression: reassessing the utility of the zung scales. BMC Psychiatry. 2017;17:329. doi: 10.1186/s12888-017-1489-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sepehry AA. Zung self-rating depression scale. In: Sepehry AA, editor. New York: Springer; 2011. [Google Scholar]
- 15.Vitorino D, Martins F, Souza A, Galdino D, Prado G. Utilizao do SF-36 em ensaios clínicos envolvendo pacientes fibromiálgicos: determinao de critérios mínimos de melhora clínica. Rev Neurociências. 2004;12:147–151. [Google Scholar]
- 16.Gledhill JA, Rodary C, Mahé C, Laizet C. French validation of the revised piper fatigue scale. Rech Soins Infirm. 2002;68:50–65. [PubMed] [Google Scholar]
- 17.Zhou R, Chen YX, Su X, Wu YM. Application effect of psychological nursing combined with pain nursing in improving perioperative anxiety and sleep quality of patients with cervical cancer. Int J Respir. 2016;35:967–969. [Google Scholar]
- 18.Sun DL. Evaluation of the efficacy of endoscopic sinus surgery with sinusitis specific quality of life scale. World Clin Med. 2017;11:81–83. [Google Scholar]
- 19.Tian JL, Gongzhi HJ, Liu Y, Zhang S. Research status of continuous care for patients with chronic diseases. China Nurs Manag. 2017;17:108–111. [Google Scholar]
- 20.Ji CH, Guo HL, Xu XY. Investigation of current requirement of transitional care model on surgical patient% needs for continuous nursing mode. Chin J Mod Nurs. 2017;23:2346–2349. [Google Scholar]
- 21.Zhang LY, Ni H, Yu GH, Ding WN, Wang XZ. Application effect of multidisciplinary team cooperation on patients with acute coronary syndrome after PCI. Prev Treat Cardiovasc Cerebrovasc Dis. 2018;18:436–438. [Google Scholar]
- 22.Pei JQ, Jiang JF, Zhang ZJ, Xu YF, Yu JP, Yao HZ. Effect of multidisciplinary cooperative extended nursing on self-care ability and quality of life of patients with depression and diabetes. Nurs Res. 2018;32:3447–3450. [Google Scholar]
- 23.Zhao LJ, Zhang F, Fang CL. Influence of continuity management of multidisciplinary cooperation mode on postoperative recovery and adverse emotions of breast cancer patients. Cancer Prog. 2020;18:852–856. [Google Scholar]
- 24.Zhang YY, Jin LL, Cui T. Effect of liujunzi decoction on immune function, cancer-related fatigue and quality of life in patients with cervical cancer undergoing adjuvant radiotherapy and chemotherapy. Chin J Tradit Chin Med. 2018;36:1721–1723. [Google Scholar]
- 25.Song XS, Yang YJ, Wang WB, Chu HY, Wang M, Zhang W, Liu NN, Qiu XH. The relationship between self-efficacy and cancer-related fatigue in patients with cervical cancer: a study on the mediating role of disease uncertainty. J Harbin Med Univ. 2018;52:156–159. [Google Scholar]


