Abstract
Objective: To ivestigate the effect of stored autotransfusion on the electrolytes and postoperative complications in patients undergoing elective orthopedic surgery. Methods: A total of 76 cases of patients undergoing elective orthopedic surgery were randomly divided into an observation group (38 cases, taking stored autotransfusion) and a control group (38 cases, taking allogeneic blood transfusion) according to a random number table method. The intraoperative-related indexes (intraoperative blood loss, autologous or allogeneic blood transfusion volume, urine volume, and length of hospital stay), electrolyte levels before and 48 hours after the operation, routine blood and coagulation function were compared between the two groups, and the postoperative complications related to blood transfusion were recorded. Results: The length of hospital stay of the observation group was significantly lower than that of the control group (P<0.05). The concentrations of K+ and Na+ in the control group 48 h after the operation were higher than those before the operation and than those in the observation group, while the concentration of Ca2+ was lower than that before the operation and that in the observation group (all P<0.05). The levels of Hb, RBC, and HCT in the control group 48 h after the operation were lower than those before the operation and those in the observation group (all P<0.05). The levels of WBC in the two groups 48 h after the operation were significantly higher, but those in the observation group were lower than those in the control group (all P<0.05). There were no significant changes in Pt, APTT, D-D, and FIB levels between the two groups. There were no significant changes in Pt, APTT, D-D, and FIB levels 48 hours after the operation compared with those before the operation (P>0.05). The incidence of postoperative complications caused by blood transfusion in the observation group was lower than that in the control group (P<0.05). Conclusion: Storage autotransfusion can effectively balance the electrolyte level and reduce the incidence of complications in patients undergoing elective orthopedic surgery. This is worthy of clinical application.
Keywords: Stored autotransfusion, elective orthopedic surgery, electrolytes, complications
Introduction
In recent years, with frequent traffic accidents and aerial work accidents, more and more patients need a blood transfusion. Although a blood donation policy has been implemented, the increasing blood demand still can not be met [1]. There are many ways of clinical blood transfusion. Storage autotransfusion is a relatively safe, effective, economical and straightforward way of blood transfusion, and is widely used in patients undergoing elective surgery [2]. Its essence is to use patients’ blood, which can save the lives of patients and reduce the burden of an insufficient blood supply [3].
Orthopedic surgery generally takes a long time. The muscles and the surrounding tissues need to be stripped during the operation, so the operation time is prolonged and the amount of intraoperative blood loss is increased. Most patients need a blood transfusion during the operation to maintain stability of vital signs [4]. Storage autotransfusion was first used in orthopedic patients undergoing elective surgery. However, this autotransfusion mode’s effect on electrolyte and coagulation function of patients has not been uniformly reported. Some studies pointed out that autotransfusion had no noticeable effect on coagulation function, but Harrison et al. found the opposite result [5,6]. Therefore, this study mainly discusses the influence of storage autotransfusion on electrolyte levels and coagulation function of patients undergoing elective orthopedic surgery and analyzes the influence of different blood transfusion modes on postoperative complications.
Materials and methods
General information
A total of 76 patients with elective surgery in the Department of Orthopedics of our hospital from December 2018 to January 2020 were randomly divided into an observation group (n=38, storage autotransfusion) and the control group (n=38, allogeneic blood transfusion) according to the random number table method. Inclusion criteria: Patients aged 20-55 years old; patients who met the indications of stored autotransfusion in the technical specification for clinical blood transfusion formulated by the Ministry of the health of the People’s Republic of China [7]; patients who are hospitalized in the orthopedics department of our hospital and scheduled for elective orthopedic surgery; patients who had a fracture or needed a hip replacement; patients whose blood routine test indicated hemoglobin (Hb) >110 g/L on admission; patients who signed informed consent. Exclusion criteria: Patients with contraindications of stored autotransfusion; patients with coagulation dysfunction; patients with obvious acute or chronic bacterial or viral infection on admission; patients with Hb <110 g/L on admission; patients with severe heart disease or pacemakers; patients with other severe cerebrovascular diseases, such as cerebral infarction, cerebral hemorrhage, etc.; patients with malignant tumor; patients who participated in other research at the same time; patients who are pregnant or lactating. This study was approved by the Ethics Committee of our hospital.
Method
In the control group, allogeneic blood transfusion was used. Before the blood transfusion, the basic information such as the patient’s name and gender, and the hospitalization information such as blood type, ward, bed number and hospitalization number were routinely checked. After the appropriate blood type was provided, normal saline was first used for flushing the blood transfusion pathway, and the blood bag was checked for damage, precipitation, and other abnormalities. After ensuring no errors, the appropriate blood was infused into patients according to the intraoperative blood loss. For patients who need a large amount of blood transfusion, the blood bag should be put into 37°C warm water for 10-15 min before the blood transfusion. In the process of blood transfusion, the aseptic operation should be strictly carried out, and the reaction of patients should be closely observed. In case of any abnormality, the blood transfusion should be stopped first, and timely treatment should be given when the cause is found. Storage autotransfusion was adopted in the observation group: (1) Collection of autologous blood: First, according to the “Technical specifications for clinical blood transfusion”, autologous blood of patients was collected by the doctors of the blood transfusion department a week before the operation (the amount of blood collected was determined according to the patient’s situation) [7,8]. The collected blood samples were placed in the blood collection bag with citrate in advance. The blood samples were then stored in the special blood storage refrigerator for standby after the name, bed number and other marks were noted. The blood collection certificate was issued. (2) Autologous blood transfusion: The spare autogenous blood was found referring to the blood certificate. The transfusion volume, and transfusion speed were adjusted according to the changes in intraoperative blood loss, transfusion volume, blood pressure, and central venous pressure. Timely symptomatic treatment was given if adverse reactions caused by blood transfusion occurred during the operation.
Outcome measures
Main outcome measures
(1) The related clinical indexes of the two groups were compared, and the intraoperative blood loss, autologous or allogeneic blood transfusion, urine volume, and the length of hospital stay were recorded. (2) About 6 mL of venous blood was collected before and 48 hours after the operation and placed in the blood collection vessel filled with citrate anticoagulant in advance. Among them, 2 mL were detected by an automatic electrolyte analyzer (manufacturer: Nanjing Beden Medical Co., Ltd., model: AC9800, origin: China) to analyze K+, Na+, and Ca2+ in the whole blood. About 2 mL of blood was detected by an automatic blood analyzer (manufacturer: Hizen Meikang (Japan) Company, model: XN9000, country of origin: Japan) to have blood routine test and record the levels of Hb, RBC, WBC, and HCT. (3) The remaining 2 mL of blood was centrifuged to separate plasma and four coagulation parameters, including prothrombin time (PT), activated partial thromboplastin time (APTT), D-Dimer (D-D), and fibrinogen (FIB) were detected by automatic coagulation analyzer (manufacturer: Megtron company, model: Coatron 3000, origin: Germany).
Secondary outcome measures
The postoperative complications caused by blood transfusion were compared between the two groups, such as fever, allergy, hyperkalemia, and Hb urine.
Statistical analysis
SPSS 20.0 was used for statistical analysis. The count data were expressed as n (%) and the chi-square test was used for comparison. The data consistent with normal measurement data were expressed as x̅ ± sd. Paired t-test was used for comparison before and after the operation in the same group and an independent t-test was used for comparison between the two groups. P<0.05 was considered significant.
Results
General information
There was no significant difference in general information between the two groups (all P>0.05), which were comparable. See Table 1.
Table 1.
General information of patients in two groups (n, x̅ ± sd)
| Indicator | Observation group (n=38) | Control group (n=38) | χ2/t | P |
|---|---|---|---|---|
| Gender (n) | 0.474 | 0.491 | ||
| Male | 20 | 17 | ||
| Female | 18 | 21 | ||
| Age (years) | 40.5±5.3 | 41.1±6.6 | 0.437 | 0.663 |
| BMI (kg/m2) | 23.37±3.05 | 23.18±3.22 | 0.264 | 0.792 |
| Hb (g/L) | 130.03±10.99 | 128.87±11.84 | 0.443 | 0.659 |
| Hct (%) | 40.09±2.22 | 40.76±2.38 | 1.269 | 0.208 |
| Blood type (n) | 1.641 | 0.650 | ||
| A | 10 | 8 | ||
| B | 12 | 13 | ||
| O | 8 | 7 | ||
| AB | 8 | 10 | ||
| Types of disease (n) | 0.561 | 0.454 | ||
| Hip replacement | 10 | 13 | ||
| Fracture | 28 | 25 |
Note: BMI: body mass index; HB: hemoglobin; Hct: hematocrit.
Clinically relevant indicators
There were no significant differences in intraoperative blood loss, blood transfusion and urine volume between the two groups (all P>0.05). The length of stay in the hospital of the observation group was significantly lower than that of the control group (P<0.05), as shown in Table 2.
Table 2.
Clinically relevant indexes of the two groups (x̅ ± sd)
| Group | Intraoperative blood loss (mL) | Blood transfusion volume (mL) | Urine output (mL) | Length of hospital stay (d) |
|---|---|---|---|---|
| Observation group (n=38) | 540.59±40.95 | 510.04±43.33 | 180.09±25.50 | 6.1±1.2 |
| Control group (n=38) | 542.28±38.70 | 507.50±48.89 | 183.33±30.08 | 9.2±1.3 |
| t | 0.185 | 0.240 | 0.506 | 10.801 |
| P | 0.854 | 0.811 | 0.614 | <0.001 |
Electrolytes
The concentration of K+, Na+, and Ca2+ in the observation group had no significant changes before and after the operation (all P>0.05). The concentration of K+ and Na+ in the control group 48 hours after the operation was higher than that before the operation, and the concentration of Ca2+ was lower than that before the operation (all P<0.05). The differences between the two groups were significant (all P<0.05), as shown in Table 3.
Table 3.
Electrolyte level of two groups before and after the operation (x̅ ± sd, mmol/L)
| Groups | Observation group (n=38) | Control group (n=38) | t | P |
|---|---|---|---|---|
| K+ | ||||
| Before the operation | 4.40±0.47 | 4.56±0.50 | 1.437 | 0.155 |
| 48 h after the operation | 4.44±0.52 | 5.03±0.46* | 5.239 | <0.001 |
| Na+ | ||||
| Before the operation | 142.20±5.44 | 142.54±4.08 | 0.308 | 0.759 |
| 48 h after the operation | 142.04±4.95 | 144.75±4.83* | 2.415 | 0.018 |
| Ca2+ | ||||
| Before the operation | 2.33±0.30 | 2.28±0.32 | 0.703 | 0.484 |
| 48 h after the operation | 2.30±0.34 | 1.77±0.37* | 6.502 | <0.001 |
Note: K+: potassium ion; Na+: sodium ion; Ca2+: calcium ion.
Compared with the same group before the operation;
P<0.05.
Blood routine
Compared with those before the operation, the Hb levels, RBC, and HCT in the control group decreased 48 hours after the operation and were lower than those in the observation group (all P<0.05). The level of WBC in the two groups increased significantly 48 hours after the operation, but that in the observation group was lower than that in the control group (all P<0.05), as shown in Table 4.
Table 4.
Blood routine before and after the operation (x̅ ± sd)
| Group | Observation group (n=38) | Control group (n=38) | t | P |
|---|---|---|---|---|
| Hb (g/L) | ||||
| Before the operation | 130.03±10.99 | 128.87±11.84 | 0.443 | 0.659 |
| 48 h after the operation | 128.99±12.48 | 101.49±15.55* | 8.502 | <0.001 |
| RBC (×1012/L) | ||||
| Before the operation | 4.40±0.40 | 4.44±0.39 | 0.390 | 0.698 |
| 48 h after the operation | 4.38±0.43 | 3.89±0.30* | 5.761 | <0.001 |
| WBC (×109/L) | ||||
| Before the operation | 5.96±0.94 | 5.89±1.03 | 0.309 | 0.758 |
| 48 h after the operation | 8.89±1.22* | 10.94±1.30* | 7.088 | <0.001 |
| Hct (%) | ||||
| Before the operation | 40.09±2.22 | 40.76±2.38 | 1.269 | 0.208 |
| 48 h after the operation | 39.33±3.94 | 34.40±3.75* | 5.587 | <0.001 |
Note: Hb: hemoglobin; RBC: red blood cell count; WBC: white blood cell count; Hct: hematocrit.
Compared with the same group before the operation;
P<0.05.
Coagulation function
PT, APTT, D-D, and FIB levels of the two groups had no significant changes before and 48 hours after the operation (all P>0.05), as shown in Table 5.
Table 5.
Coagulation function before and after the operation in two groups (x̅ ± sd)
| Group | Observation group (n=38) | Control group (n=38) | t | P |
|---|---|---|---|---|
| PT (s) | ||||
| Before the operation | 12.88±1.10 | 12.95±1.23 | 0.262 | 0.794 |
| 48 h after the operation | 13.03±1.29 | 13.22±1.37 | 0.622 | 0.536 |
| APTT (s) | ||||
| Before the operation | 35.59±2.88 | 35.96±3.04 | 0.545 | 0.588 |
| 48 h after the operation | 36.02±3.30 | 35.89±2.85 | 0.184 | 0.855 |
| D-D (mg/L) | ||||
| Before the operation | 0.39±0.11 | 0.37±0.10 | 0.829 | 0.410 |
| 48 h after the operation | 0.37±0.16 | 0.36±0.12 | 0.308 | 0.759 |
| FIB (g/L) | ||||
| Before the operation | 3.24±0.83 | 3.20±0.78 | 0.216 | 0.829 |
| 48 h after the operation | 3.03±0.91 | 2.93±0.86 | 0.492 | 0.624 |
Note: PT: prothrombin time; APTT: activated partial thromboplastin time; D-D: D-dimer; FIB: fibrinogen.
Postoperative complications
The incidence of postoperative complications caused by blood transfusion in the observation group was lower than that in the control group (P<0.05), as shown in Table 6 and Figure 1.
Table 6.
Comparison of the incidence of postoperative transfusion-related complications between the two groups (n, %)
| Group | Fever | Allergy | Hyperkalemia | Hemoglobinuria | The total incidence |
|---|---|---|---|---|---|
| Observation group (n=38) | 0 (0.00) | 0 (0.00) | 1 (2.63) | 1 (2.63) | 2 (5.26) |
| Control group (n=38) | 3 (7.89) | 2 (5.26) | 1 (2.63) | 2 (5.26) | 8 (21.05) |
| χ2 | 1.388 | 0.514 | 0.514 | 0.000 | 4.145 |
| P | 0.239 | 0.474 | 0.474 | 1.000 | 0.042 |
Figure 1.
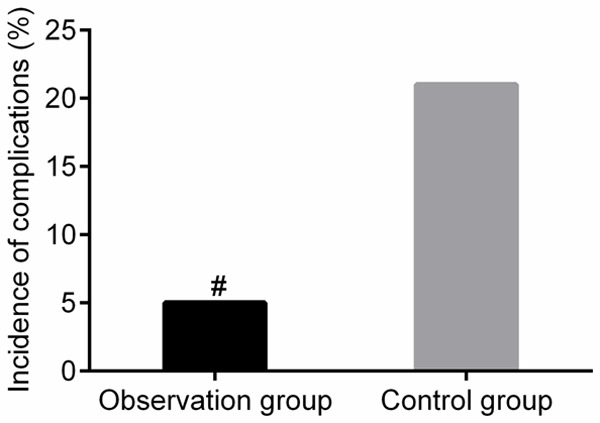
Comparison of the incidence of blood transfusion related complications between the two groups. Compared with the control group, #P<0.05.
Discussion
Allogeneic blood transfusion is a common and conventional way of blood transfusion in the clinic. However, allergic reactions, electrolyte disorders or infections will inevitably occur [9,10]. Compared with allogeneic blood transfusion, storage autotransfusion is a safe, effective, economical, and straightforward way of blood transfusion, which can greatly reduce the risk of transfusion-related complications [11,12].
In this study, there was no significant difference in intraoperative blood loss, blood transfusion, and urine volume between the two groups, but the length of stay in f the observation group was significantly lower than that of the control group (P<0.05). It has been proven that there was no significant relationship between the changes of various indicators before and after the operation and intraoperative blood loss and blood transfusion, and this would not increase the economic difficulties of patients. After a comparative analysis of the electrolyte concentration, it was found that the concentration of K+ and Na+ in the control group 48 h after the operation was higher than that before the operation and that in the observation group. In comparison, the concentration of Ca2+ was lower than that before the operation and that in the observation group. However, the concentration of K+, Na+ and Ca2+ in the observation group had no significant change before and after the operation, which indicated that the two blood transfusion modes (allogeneic blood transfusion and storage autotransfusion) adopted in this study had significant differences in the effects on electrolytes in patients undergoing elective orthopedic surgery. Compared with allogeneic blood transfusion, the effect of storage autotransfusion mode on body electrolyte was smaller, effectively reducing the occurrence of postoperative hyperkalemia and hypercalcemia. Tomimaru et al. studied the effects of storage autotransfusion mode and conventional allogeneic blood transfusion mode on electrolytes before, and 1 d and 3 d after the operation [13]. The results showed that the conventional allogeneic blood transfusion mode had a greater impact on the fluctuation of body electrolytes. At the same time, there were no significant changes in the body electrolytes before, one day and three days after the operation under the stored autologous blood transfusion mode, which was consistent with this study. It is speculated that the transfusion of allogeneic blood is the stock red blood cell suspension, and the stock red blood cell suspension can be slightly acidic due to glycolysis after a period of time, which can induce metabolic acidosis and break the acid-base balance of the body after a large amount of infusion in patients [14]. Besides, after storage for a while, K+ can be released from the red blood cells, resulting in an increase of free potassium concentration in the red blood cell suspension. Hyperkalemia can be caused by massive transfusion in patients, while storage autotransfusion can effectively avoid the above problems [15-17].
In this study, Hb, RBC, and HCT in the control group 48 hours after the operation were lower than those before the operation and those in the observation group. The level of WBC of the two groups increased significantly after the operation, but that in the observation group was lower than that of the control group, suggesting that the effect of storage autotransfusion on the blood indexes of patients undergoing elective orthopedic surgery is small. Sakai et al. also had a similar conclusion. Their study compared the effect of storage autotransfusion mode and conventional allogeneic blood transfusion mode on the blood routine of patients [18]. The results showed that Hb and HCT decreased significantly and WBC increased significantly after the conventional allogeneic blood transfusion. It is speculated that allogeneic blood transfusion is, after all, the blood of different individuals. The recipient can be considered a foreign substance, which is different from their blood components to different degrees. Therefore, a massive infusion can cause changes in many blood indexes [19,20]. In terms of blood coagulation, this study found that the levels of PT, APTT, D-D, and FIB levels had no significant changes in the two groups before and 48 hours after the operation, suggesting that both allogeneic blood transfusion and storage autotransfusion had no significant effect on blood coagulation function, which is consistent with the results reported by Donati et al. but some scholars hold the opposite opinion [21]. For example, Salamin et al. think that allogeneic blood transfusion has a greater impact on the coagulation function than storage autotransfusion, which may be related to the sample size and the amount of infusion [22]. Finally, this study found that the total incidence of complications caused by blood transfusion in the observation group was lower than that in the control group, suggesting that storage autotransfusion can reduce the incidence of transfusion-related complications. However, this study is a single-center clinical study. The sample size is limited and there is no follow-up after discharge. The effects of two different blood transfusion methods on long-term electrolytes and coagulation function of patients still need more in-depth research to confirm.
To sum up, for patients undergoing elective orthopedic surgery, the effect of storage autotransfusion mode on postoperative blood indexes and body electrolytes is smaller, which can effectively reduce postoperative transfusion-related complications and has no significant impact on the body’s coagulation function. Therefore, storage autotransfusion can be given priority to patients who meet the indications for storage autotransfusion.
Disclosure of conflict of interest
None.
References
- 1.Yu X, Wang Z, Shen Y, Liu Z, Wang H, Zhang S, Gan J, Xue F, Han W, Shi X, Hu Y, Wang L, Li N, Wu P, Yang C, Jiang J. Population-based projections of blood supply and demand, China, 2017-2036. Bull World Health Organ. 2020;98:10–18. doi: 10.2471/BLT.19.233361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iwata S, Hirasaki Y, Nomura M, Ozaki M. Thromboelastometric evaluation of coagulation profiles of cold-stored autologous whole blood: a prospective observational study. Medicine (Baltimore) 2019;98:e17357. doi: 10.1097/MD.0000000000017357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hulsebos H, Bernard J. Consider autotransfusion in the field. Mil Med. 2016;181:e945–7. doi: 10.7205/MILMED-D-15-00046. [DOI] [PubMed] [Google Scholar]
- 4.Chou MY, Wang YC, Peng LN, Liang CK, Chu CS, Liao MC, Lin YT, Hsu CJ, Chen LK. Intraoperative blood transfusion predicts postoperative delirium among older patients undergoing elective orthopedic surgery: a prospective cohort study. Int J Geriatr Psychiatry. 2019;34:881–888. doi: 10.1002/gps.5086. [DOI] [PubMed] [Google Scholar]
- 5.Karafin MS, Francis RO. Impact of G6PD status on red cell storage and transfusion outcomes. Blood Transfus. 2019;17:289–295. doi: 10.2450/2019.0092-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harrison HB, Smith WZ, Salhanick MA, Higgins RA, Ortiz A, Olson JD, Schwacha MG, Harrison CR, Aydelotte JD, Stewart RM, Dent DL. An experimental model of hemothorax autotransfusion: impact on coagulation. Am J Surg. 2014;208:1078–1082. doi: 10.1016/j.amjsurg.2014.09.012. [DOI] [PubMed] [Google Scholar]
- 7.Ministry of Health. Technical specification for clinical blood transfusion. China Hospital. 2000;11:1–11. [Google Scholar]
- 8.Tamai K, Terai H, Toyoda H, Suzuki A, Yasuda H, Dozono S, Nakamura H. Which is the best schedule of autologous blood storage for preoperative adolescent idiopathic scoliosis patients? Scoliosis. 2015;10(Suppl 2):S11. doi: 10.1186/1748-7161-10-S2-S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang X, Hu Q, Liu Z, Huang H, Zhang Q, Dai H. Comparison between nitroglycerin and remifentanil in acute hypervolemic hemodilution combined with controlled hypotension during intracranial aneurysm surgery. Int J Clin Exp Med. 2015;8:19353–19359. [PMC free article] [PubMed] [Google Scholar]
- 10.Yu T, Xu G, Xu X, Yang J, Ding L. Myeloid sarcoma derived from the gastrointestinal tract: a case report and review of the literature. Oncol Lett. 2016;11:4155–4159. doi: 10.3892/ol.2016.4517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jin J, Zhou J, Zhang QL, Chen Z, Wu GL. Application of component apheresis in pre-deposited autotransfusion. Ann Clin Lab Sci. 2018;48:634–638. [PubMed] [Google Scholar]
- 12.Seyfried TF, Streithoff F, Gruber M, Unterbuchner C, Zech N, Kieninger M, Hansen E. Platelet sequestration with a new-generation autotransfusion device. Transfusion. 2018;58:989–997. doi: 10.1111/trf.14491. [DOI] [PubMed] [Google Scholar]
- 13.Tomimaru Y, Noguchi K, Dono K. Necessity for autologous blood storage and transfusion in patients undergoing pancreatoduodenectomy. Surg Today. 2017;47:568–574. doi: 10.1007/s00595-016-1407-4. [DOI] [PubMed] [Google Scholar]
- 14.Chen J, Biller E, Losos M, Li J, Hamad D, Blower L, Grevenow M, Oakley J. Irradiation and prolonged storage of red cells are associated with increased adverse events. Vox Sang. 2018;113:468–475. doi: 10.1111/vox.12660. [DOI] [PubMed] [Google Scholar]
- 15.Jani VP, Mailo S, Athar A, Lucas A, Williams AT, Cabrales P. Blood quality diagnostic device detects storage differences between donors. IEEE Trans Biomed Circuits Syst. 2017;11:1400–1405. doi: 10.1109/TBCAS.2017.2749304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bal SH, Heper Y, Kumaş LT, Guvenc F, Budak F, Göral G, Oral HB. Effect of storage period of red blood cell suspensions on helper T-cell subpopulations. Blood Transfus. 2018;16:262–272. doi: 10.2450/2017.0238-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Frank SM, Sikorski RA, Konig G, Tsilimigras DI, Hartmann J, Popovsky MA, Pawlik TM, Waters JH. Clinical utility of autologous salvaged blood: a review. J Gastrointest Surg. 2020;24:464–472. doi: 10.1007/s11605-019-04374-y. [DOI] [PubMed] [Google Scholar]
- 18.Sakai A, Matsunaga S, Nakamura E, Samejima K, Ono Y, Yamamoto K, Takai Y, Maeda H, Seki H. Optimal preoperative autologous blood storage volume required in surgeries for placenta previas and low-lying placentas. J Obstet Gynaecol Res. 2019;45:1843–1850. doi: 10.1111/jog.14044. [DOI] [PubMed] [Google Scholar]
- 19.Pawaskar A, Salunke AA, Kekatpure A, Chen Y, Nambi GI, Tan J, Sonawane D, Pathak S. Do autologous blood transfusion systems reduce allogeneic blood transfusion in total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc. 2017;25:2957–2966. doi: 10.1007/s00167-016-4116-z. [DOI] [PubMed] [Google Scholar]
- 20.Ma M, Yu XR, Wang Y, Huang YG, Lu SF, Tian Y, Bai B. Irrationality of allogeneic red blood cell transfusion in intraoperative cell salvage patients: a retrospective analysis. Chin Med Sci J. 2018;33:77–83. doi: 10.24920/11807. [DOI] [PubMed] [Google Scholar]
- 21.Donati F, Acciarini R, De Benedittis I, de la Torre X, Pirri D, Prete M, Stampella A, Vernucci E, Botre F. Detecting autologous blood transfusion in doping control: biomarkers of blood aging and storage measured by flow cytofluorimetry. Curr Pharm Biotechnol. 2018;19:124–135. doi: 10.2174/1389201019666180405165118. [DOI] [PubMed] [Google Scholar]
- 22.Salamin O, De Angelis S, Tissot JD, Saugy M, Leuenberger N. Autologous blood transfusion in sports: emerging biomarkers. Transfus Med Rev. 2016;30:109–15. doi: 10.1016/j.tmrv.2016.05.007. [DOI] [PubMed] [Google Scholar]


