Abstract
Purpose: To investigate the therapeutic effect of maintenance hemodialysis in patients with chronic renal failure and summarize the analysis of inflammatory factors in serum, and the risk factors in patients with chronic renal failure undergoing maintenance hemodialysis. Methods: A total of 50 patients with chronic renal failure undergoing maintenance hemodialysis who were admitted to our hospital from January 2017 to January 2019 were selected as the research subjects to analyze the therapeutic effects and complications of maintenance hemodialysis of these patients, compare the changes of inflammatory factor levels in serum such as interleukin-2 (IL-2), interleukin-6 (IL-6), and high-sensitivity C-reactive protein (hs-CRP) and renal function indicators such as creatinine, urea nitrogen, and urinary albumin clearance, and analyze the risk factors of maintenance hemodialysis in patients with chronic renal failure by multivariate logistic factor analysis. Results: The effective rate of maintenance hemodialysis in patients with chronic renal failure was 64% (32 cases). After dialysis, urea nitrogen, urinary albumin and creatinine clearance were significantly decreased (P < 0.05). As for the complications, 10 patients died, and 8 patients had infection. The levels of inflammatory factors in serum, such as IL-2, hs CRP were significantly decreased after maintenance hemodialysis (P < 0.05), and the difference was statistically significant. The results of multivariate logistic factor analysis showed that high capacity load and anemia were independent risk factors for death in patients with chronic renal failure undergoing maintenance hemodialysis. Simultaneously, diabetes mellitus, central venous catheterization, and hypoalbuminemia were independent risk factors for infection in patients with chronic renal failure undergoing maintenance hemodialysis. Conclusion: The level of inflammatory factors in the serum of patients with chronic renal failure after maintenance hemodialysis was significantly reduced. The risk factors of death and infection include hypertension, anemia, diabetes, etc. In contrast, the independent risk factors of death were anemia and high capacity load, and the independent risk factors of infection were diabetes, hypoalbuminemia, and central venous catheterization.
Keywords: Chronic renal failure, maintenance hemodialysis, inflammatory factors in serum, risk factors
Introduction
Chronic renal failure is a disease which seriously affects the health of many people. Currently, hemodialysis is widely used in treating patients with chronic renal failure in China, to alleviate the suffering of patients and prolong their lives [1-3].
The levels of IL-2, hs-CRP, and other inflammatory factors in the serum of patients with chronic renal failure will increase, leading to a micro-inflammatory state. Chronic inflammation easily occurs when patients are in a micro-inflammatory state over a long period, resulting in metabolic disorders, the decrease of immune function, and other phenomena, which are extremely unfavorable for the recovery of patients. It has been reported that maintenance hemodialysis can alleviate the micro-inflammatory state in patients and reduce the expression level of inflammatory factors in serum [4-6].
In addition, death, infection and other complications may occur during maintenance hemodialysis. Therefore this study was conducted to investigate the therapeutic effect of maintenance hemodialysis in patients with chronic renal failure, analyze the changes of serum inflammatory factors in patients before and after hemodialysis, and clarify the risk factors of maintenance hemodialysis. The specific research reports are as follows:
Materials and methods
General information
A total of 50 patients with chronic renal failure undergoing maintenance hemodialysis who were admitted to our hospital from January 2017 to January 2019 were selected as the research subjects. The patients were 30 to 70 years old, including 25 males and 25 females. Among them, 10 people had diabetic nephropathy, 5 people had gouty nephropathy, 7 people had hypertensive nephropathy, 24 people had chronic nephritis, and 4 people had obstructive nephropathy.
Inclusion criteria
① Symptoms were consistent with the typical clinical manifestations of chronic renal failure; ② The patient had been undergoing hemodialysis in our hospital for more than 3 months; ③ The patients had normal cognitive function and no history of drug allergy and drug abuse; ④ The study was approved by the ethics committee of the hospital. All patients participated in the study voluntarily and signed an informed consent.
Exclusion criteria
① Patients with chronic renal failure associated with other organic diseases were excluded from the study; ② Patients with chronic renal failure were excluded except hemodialysis; ③ Patients with unstable control of blood pressure, blood sugar and other biological indicators were excluded.
Methods
Preparation before dialysis
① Because of the different effects of primary diseases in patients with chronic renal failure, it is necessary to control the primary diseases before hemodialysis. The fasting blood glucose of patients with diabetic nephropathy should be controlled in the range of 3.9-6.1 mmol/l. The systolic blood pressure and diastolic blood pressure should be maintained between 90-140 mmhg and 60-90 mmhg in patients with hypertensive nephropathy to avoid the risk during hemodialysis. ② Before dialysis, psychological counseling should be given to patients and their families to popularize the basic principles of hemodialysis so as to relieve the tension of patients. ③ Preparation of tools for hemodialysis and inspection of the dialyzer (specification: BLS812SD; batch number: SFDA (I) No. 20123452513 (A)).
Methods of measuring serum inflammatory factors
We collected blood and urine from the patient’s intravenous fistula before and after hemodialysis, using the serum inflammatory factor level test paper to determine the levels of serum IL-2, IL-6, hs-CRP, and other inflammatory factors, then we compared the results before and after hemodialysis. We recorded renal function indexes, such as creatinine, urea nitrogen and, albumin clearance before and after treatment.
Methods of dialysis
The 50 patients with chronic renal failure were treated with hemodialysis. Bicarbonate dialysate (specification: SXG-Y-A; SFDA approval No. (2013): 3450779) was selected for dialysis with reverse osmosis water, and the flow rate was maintained at 500 ml/min.
Blood access was established and heparin (specification: 5000 IU; batch number: SFDA approval No. H10980166; manufacturer: Zhaoke Pharmaceutical (Hefei) Co., Ltd.) was used as an anticoagulant. The first injection of heparin was 10 minutes before the start of dialysis, the dose was 0.5 mg/kg, and heparin was injected at a rate of 8 ml/h after the start of dialysis. The injection of heparin was stopped 50 min before the end of dialysis to ensure that the blood clotting time in the patient was within 45-60 min [7-9].
To ascertain the possible risk factors of patients in real time and adjust the dialysis plan according to the recorded results, the patient’s body temperature, respiration, pulse, blood pressure, and other indicators were closely monitored and recorded every 30~60 min during dialysis.
Nursing staff carried out appropriate treatment to the patient when the patient had symptoms such as bleeding, heart failure, myocardial infarction, and other symptoms during dialysis. If blood stratification and coagulation occurred during dialysis, the dosage of heparin was increased in real time, and if the color of dialysate changed, they dialysis was stopped immediately and replacement of the dialysis device was performed.
Monitoring after dialysis
Basic information such as the patient’s temperature, respiration, pulse, and blood pressure were measured after dialysis. To clarify the effect factors of hemodialysis and determine the next-stage dialysis plan, blood samples were taken to check creatinine, urea nitrogen, K+, Na+, Cl- [10-13].
During the whole dialysis treatment process, it was necessary to strictly monitor the amount of fluid in and out of the patient’s body to prevent heart failure due to excessive increase of fluid. Therefore, the amount of water patients had to drink was controlled within a safe range. The diet of patients strictly followed the recommended diet, with low salt, low potassium, a moderate amount of protein, and ensure the intake of high vitamins.
Detection methods of risk factors
Patient’s general data, hemodialysis time, primary disease, number of infections and deaths, time of death, infection site, catheterization status, routine blood indices, routine urine indices, blood sugar, blood lipids, hormones, blood pressure, heart rate, dialysis indicators, volume load and other indicators were analyzed by multivariate logistic factor analysis to explore the correlation between the above indicators and death and infection in patients to obtain the risk factors of death and infection of patients.
Evaluation index
The therapeutic effect and complications of maintenance hemodialysis in patients with chronic renal failure were analyzed. The clinical data of patients and the changes of serum IL-2, IL-6, hs-CRP, and other inflammatory factors before and after dialysis were compared. The related complications of patients with chronic renal failure during maintenance hemodialysis, and the correlation of risk factors were analyzed by multivariate logistic factor analysis.
Statistical analysis
Data were analyzed with GraphPad Prism (GraphPad Software, La Jolla, CA) and SPSS 20 (SPSS Inc., Chicago, IL). The measurement data was expressed as (x̅ ± sd)and tested by t-test, and enumeration data were tested by chi-squared test and expressed by [n (%)]. When P < 0.05, the difference between the two groups had statistical significance.
Results
The therapeutic effect, cure rate, and complications of maintenance hemodialysis
In this study, the effective rate of maintenance hemodialysis treatment in 50 patients with chronic renal failure was 64%, that is, there were 32 patients with no complications in hemodialysis and 18 patients (36%) with complications, including 10 patients who died and 8 patients with infection.
Comparison of serum inflammatory factor levels in patients
Comparison of interleukin levels and renal function
The levels of interleukins (IL-1β, IL-2, IL-6, IL-8) after dialysis were lower than those before dialysis (P < 0.05), as shown in Figure 1. After dialysis, urea nitrogen, urinary albumin, and clearance of creatinine were significantly decreased (P < 0.05), as shown in Table 1.
Figure 1.
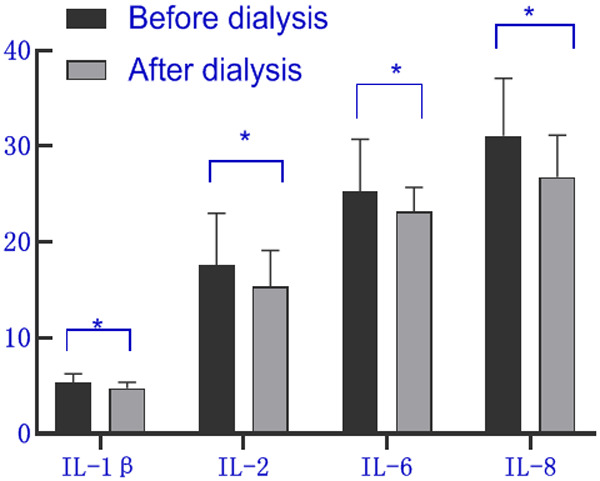
Comparison of interleukin levels before and after dialysis. Note: The abscissa represents IL-1β, IL-2, IL-6, IL-8 from left to right, and the ordinate represents the expression level of IL-1β, IL-2, IL-6, and IL-8 (ng/L). Comparison of expression levels of IL-1β before and after dialysis [(5.39±0.86) ng/L vs (4.76±0.61) ng/L] was statistically significant (t=4.23, *P=0.0001); Comparison of expression levels of IL-2 before and after dialysis [(17.56±5.44) ng/L vs (15.35±3.78) ng/L] was statistically significant (t=2.36, *P=0.02); Comparison of expression levels of IL-6 before and after dialysis [(25.33±5.37) ng/L vs (23.21±2.50) ng/L] was statistically significant (t=2.53, *P=0.01). Comparison of expression levels of IL-8 before and after dialysis [(31.09±6.00) ng/L vs (26.78±4.37) ng/L] was statistically significant (t=4.11, *P=0.0001).
Table 1.
Comparison of renal function
| Time | Creatinine (umol/L) | Urea Nitrogen (mmol/L) | Creatinine Clearance (ug/min) |
|---|---|---|---|
| Before treatment | 115.13±21.13 | 8.99±0.91 | 120.74±22.74 |
| After treatment | 89.14±11.70 | 4.10±0.77 | 82.11±13.45 |
| T | 1.235 | 2.567 | 5.886 |
| P | 0.001 | 0.002 | 0.004 |
Comparison of the level of other inflammatory factors
The expression levels of hs-CRP, TNF-α, and PCT after dialysis were obviously lower than those before dialysis (P < 0.05). This showed that hemodialysis can reduce the expression of serum inflammatory factors and alleviate the inflammatory state in patients. The effect of hemodialysis can be judged by detecting the expression level of inflammatory factors in patients, as shown in Figure 2.
Figure 2.
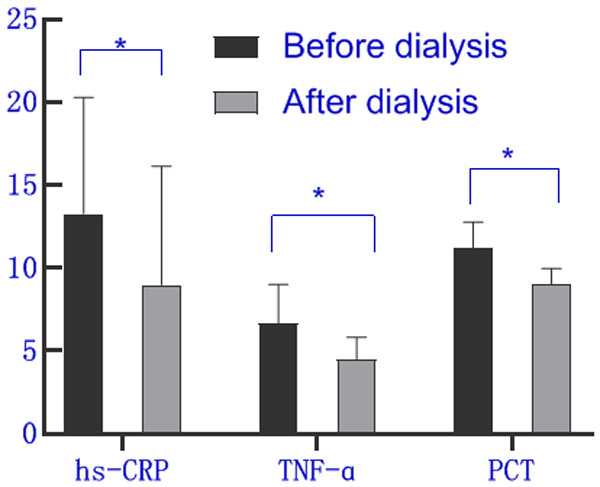
Comparison of the expression levels of hs CRP, TNF-α and PCT before and after dialysis. Note: The abscissa represents hs-CRP, TNF-α, PCT from left to right, and the ordinate represents the expression level of hs-CRP (mg/L), TNF-α (ng/mL), and PCT (ng/mL). Comparison of expression levels of hs-CRP (mg/L) before and after dialysis [(13.28±7.00) mg/L vs (8.99±7.15) mg/L] was statistically significant (t=3.03, *P=0.003); Comparison of expression levels of TNF-α (ng/mL) before and after dialysis [(6.67±2.34) ng/mL vs (4.49±1.33) ng/mL] was statistically significant (t=5.73, *P < 0.05); Comparison of expression levels of PCT (ng/mL) before and after dialysis [(11.22±1.57) ng/mL vs (9.00±0.97) ng/mL] was statistically significant (t=8.51, *P < 0.05).
Analysis of risk factors for death
The patient’s general data, hemodialysis time, primary disease, number of infections and deaths, time of death, infection site, catheterization status, blood indices, urine indices, blood sugar, blood lipids, hormone, blood pressure, heart rate, adequate dialysis, volume load, and other indicators were taken as independent variables, and whether the patient died was taken as the dependent variable.
Univariate regression analysis showed that hypertension, anemia, age ≥ 65 years, high volume load, high plasma homocysteine level, and high serum parathyroid hormone levels were the risk factors for death in patients with chronic renal failure undergoing maintenance hemodialysis, and adequate dialysis was the protective factor.
We took the above 6 risk factors as independent variables and patient death as the dependent variable. According to the multivariate analysis, high volume load and anemia were independent risk factors for death in patients with chronic renal failure undergoing maintenance hemodialysis (Table 2).
Table 2.
Logistics single factor regression analysis
| Influencing factors | Regression coefficients | Standard error | Wald X2 | P | OR (95% Cl) |
|---|---|---|---|---|---|
| Hypertension | 1.649 | 0.303 | 21.591 | < 0.001 | 4.301 |
| Anemia | 2.113 | 0.286 | 54.592 | < 0.001 | 7.540 |
| Age ≥ 65 | 1.136 | 0.259 | 7.348 | 0.007 | 2.710 |
| High capacity load | 2.341 | 0.360 | 39.001 | < 0.001 | 11.038 |
| High plasma homocysteine | 1.754 | 0.331 | 27.021 | < 0.001 | 5.369 |
| High serum parathyroid hormone levels | 1.776 | 0.319 | 28.557 | < 0.001 | 6.008 |
| Adequate dialysis | -2.864 | 0.669 | 17.895 | < 0.001 | 0.059 |
Analysis of infection factors
The patient’s general data, hemodialysis time, primary disease, number of infections and deaths, time of death, infection site, catheterization status, blood indices, urine indices, blood sugar, blood lipids, hormone, blood pressure, heart rate, adequate dialysis, volume load, and other indicators were taken as independent variables, and infection was the dependent variable. According to univariate regression analysis, hemodialysis duration of more than half a year, diabetes mellitus, low serum albumin, and central venous catheterization were the risk factors of hemodialysis infection (Tables 3, 5).
Table 3.
Logistics multivariate regression analysis
| Influencing factors | Regression coefficients | Standard error | Wald X2 | P | OR (95% Cl) |
|---|---|---|---|---|---|
| High capacity load | 2.559 | 0.427 | 38.167 | < 0.001 | 13.339 |
| Anemia | 1.814 | 0.463 | 14.968 | < 0.001 | 5.461 |
Table 5.
Logistics multivariate regression analysis
| Influencing factors | Regression coefficients | Standard error | Wald X2 | P | OR (95% Cl) |
|---|---|---|---|---|---|
| Diabetes | 0.604 | 0.299 | 12.463 | < 0.001 | 1.914 |
| Low serum albumin | 0.507 | 0.241 | 9.379 | 0.002 | 1.804 |
| Central venous catheterization | 0.613 | 0.134 | 10.262 | 0.001 | 1.795 |
We took the above 4 risk factors as independent variables and infection as the dependent variable. According to the multivariate regression analysis, diabetes, low serum albumin, and central venous catheterization were the independent factors for infection in patients with chronic renal failure undergoing maintenance hemodialysis, as presented in Table 4.
Table 4.
Logistics single factor regression analysis
| Influencing factors | Regression coefficients | Standard error | Wald X2 | P | OR (95% Cl) |
|---|---|---|---|---|---|
| Dialysis for more than half a year | 0.568 | 0.128 | 5.377 | 0.020 | 1.446 |
| Diabetes | 0.673 | 0.296 | 11.460 | 0.001 | 1.960 |
| Low serum albumin | 0.681 | 0.300 | 9.392 | 0.002 | 1.773 |
| Central venous catheter | 0.637 | 0.196 | 11.002 | 0.001 | 1.835 |
Discussion
Chronic renal failure is a common urinary system disease, especially in middle-aged and elderly patients. There are many causes of chronic renal failure such as diabetes, hypertension, primary nephropathy etc. With the development of modern medicine, the level of medical technology has improved. Hemodialysis is a crucial treatment approach to maintain the health and lives of patients with chronic renal failure and alleviate their suffering. However, hemodialysis is a treatment with both risks and benefits. Due to the fluctuation of serum inflammatory factors, patients with chronic renal failure easily suffer from chronic inflammation, resulting in decreased immunity. In addition, because dialysis can affect the function of some organs, organic lesions are also common complications of hemodialysis patients [17,18].
Among the 50 patients with chronic renal failure on maintenance hemodialysis in this study, the levels of IL-2, hs-CRP, and other serum inflammatory factors before and after dialysis were evidently different. After dialysis, urea nitrogen, urinary albumin, and creatinine clearance were significantly decreased (P < 0.05). The reason why the level of inflammatory factors is higher than the normal range before dialysis was that the renal function of patients with chronic renal failure decreases and the function of filtering toxins decreases, which causes the accumulation of toxins in the body and stimulates the release of inflammatory transmitters in the body. In the long run, the level of inflammatory factors in the serum increased slowly and stably, and a micro-inflammatory state appeared. Khaloo Pegah et al. [19] put forward that the change of HS-CRP level could predict the possibility of retinopathy in diabetic patients, which is in conformity with our study wherein the expression level of HS-CRP in patients after dialysis was significantly decreased, and the effect of hemodialysis could be determined by monitoring the expression level of serum inflammatory factors.
Among the 50 patients, 18 patients had complications, of which 10 patients died and 8 patients had infection. Analyzing the risk factors of complications in maintenance hemodialysis patients with chronic renal failure by Logistic regression analysis method, the results showed that hypertension, anemia, age ≥ 65 years, high volume load, high plasma homocysteine level and high serum parathyroid hormone level were the risk factors for death in patients with chronic renal failure undergoing maintenance hemodialysis, and adequate dialysis was the protective factor.
Among the above six risk factors for death, anemia and high-volume load are independent risk factors for the death of patients with chronic renal failure on maintenance hemodialysis. The analysis of risk factors for infection showed that diabetes, dialysis duration over half a year, low serum albumin and central venous catheterization were risk factors for infection, among which diabetes, low serum albumin, and central venous catheterization were independent risk factors for infection. This result was in conformity with the conclusion proposed by Zhang Ning et al. [20] that decreased hemoglobin, and serum albumin are independent risk factors for peritoneal dialysis infection. The limitation of this study is that in the analysis of serum inflammatory factor levels and risk factors in chronic renal failure maintenance hemodialysis patients, with the independent risk factors of chronic renal failure maintenance hemodialysis patients were analyzed, but serum IL-2 and hs-CRP were not detected. In the future, the number of patients will be expanded, and the diagnostic efficacy of inflammatory factors for chronic renal failure in maintenance hemodialysis patients will be further tested to provide rapid detection and strong theoretical basis.
In conclusion, the level of serum inflammatory factors in maintenance hemodialysis patients with chronic renal failure was significantly lower than that before dialysis. Complications during hemodialysis included death and infection. The independent risk factors for death were anemia and high volume load. In contrast, the independent risk factors for infection were diabetes, low serum albumin, and central venous catheterization.
Disclosure of conflict of interest
None.
References
- 1.Guler HS, Tulunay Kaya C, Kumru G, Kosku H, Ozyuncu N, Sengul S, Kutlay S. Acute stunning effect of hemodialysis on myocardial performance: a three-dimensional speckle tracking echocardiographic study. Artif Organs. 2020;12:1081–1089. doi: 10.1111/aor.13698. [DOI] [PubMed] [Google Scholar]
- 2.Smyth B, Zuo L, Gray NA, Chan CT, de Zoysa JR, Hong D, Rogers K, Wang J, Cass A, Gallagher M, Perkovic V, Jardine M ACTIVE Dialysis Study Investigators. No evidence of a legacy effect on survival following randomization to extended hours dialysis in the ACTIVE Dialysis trial. Nephrology (Carlton) 2020;25:792–800. doi: 10.1111/nep.13737. [DOI] [PubMed] [Google Scholar]
- 3.Egeland EJ, Witczak BJ, Zaré HK, Christensen H, Åsberg A, Robertsen I. Chronic inhibition of CYP3A is temporarily reduced by each hemodialysis session in patients with end-stage renal disease. Clin Pharmacol Ther. 2020;108:866–873. doi: 10.1002/cpt.1875. [DOI] [PubMed] [Google Scholar]
- 4.Wang Z, Liu R, Yang H, Wang Y. Nanoporous polysulfones with in situ PEGylated surfaces by a simple swelling strategy using paired solvents. Chem Commun (Camb) 2017;53:9105–9108. doi: 10.1039/c7cc04091a. [DOI] [PubMed] [Google Scholar]
- 5.Ferrey AJ, Choi G, Hanna RM, Chang Y, Tantisattamo E, Ivaturi K, Park E, Nguyen L, Wang B, Tonthat S, Rhee CM, Reddy U, Lau WL, Huang SS, Gohil S, Amin AN, Hsieh L, Cheng TT, Lee RA, Kalantar-Zadeh K. A case of novel coronavirus disease 19 in a chronic hemodialysis patient presenting with gastroenteritis and developing severe pulmonary disease. Am J Nephrol. 2020;51:337–342. doi: 10.1159/000507417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shang W, Li Y, Li H, Li W, Li C, Cai Y, Dong J. Correlation between laboratory parameters on admission and outcome of COVID-19 in maintenance hemodialysis patients. Int Urol Nephrol. 2021;53:165–169. doi: 10.1007/s11255-020-02646-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murasawa M, Uehara A, Suzuki T, Shimizu S, Kojima S, Uchida D, Okamoto T, Naganuma T, Sasaki S, Imai N, Chikaraishi A, Matsukawa S, Kawarazaki H, Sakurada T, Shibagaki Y. Association between pill burden and interdialytic weight gain in patients with hemodialysis: a multi-center cross-sectional study. Ther Apher Dial. 2021;25:475–482. doi: 10.1111/1744-9987.13585. [DOI] [PubMed] [Google Scholar]
- 8.Yamamoto S, Matsuzawa R, Hoshi K, Suzuki Y, Harada M, Watanabe T, Isobe Y, Imamura K, Osada S, Yoshida A, Kamiya K, Matsunaga A. Modified creatinine index and clinical outcomes of hemodialysis patients: an indicator of sarcopenia? J Ren Nutr. 2020;S1051-2276:30211–30219. doi: 10.1053/j.jrn.2020.08.006. [DOI] [PubMed] [Google Scholar]
- 9.Ogawa C, Tsuchiya K, Maeda K. High serum magnesium levels are associated with favorable prognoses in diabetic hemodialysis patients, retrospective observational study. PLoS One. 2020;15:e0238763. doi: 10.1371/journal.pone.0238763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koshi E, Saito S, Okazaki M, Toyama Y, Ishimoto T, Kosugi T, Hiraiwa H, Jingushi N, Yamamoto T, Ozaki M, Goto Y, Numaguchi A, Miyagawa Y, Kato I, Tetsuka N, Yagi T, Maruyama S. Efficacy of favipiravir for an end stage renal disease patient on maintenance hemodialysis infected with novel coronavirus disease 2019. CEN Case Rep. 2021;10:126–131. doi: 10.1007/s13730-020-00534-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu Y, Zheng Y, Wang L, Zhong X, Qin D, Chen W, Tan R, Liu Y. Lower levels of blood zinc associated with intradialytic hypertension in maintenance hemodialysis patients. Biol Trace Elem Res. 2021;199:2514–2522. doi: 10.1007/s12011-020-02385-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zheng Y, Tang Z, You L, Wu Y, Liu J, Xue J. Trimethylamine-N-oxide is an independent risk factor for hospitalization events in patients receiving maintenance hemodialysis. Ren Fail. 2020;42:580–586. doi: 10.1080/0886022X.2020.1781170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang C, Lin Y, Yang Y, Zeng F, Jiang H, Lin T, Zheng L. Effectiveness and safety of warm needle acupuncture on chronic renal failure: protocol for a systematic review and meta-analysis. Medicine (Baltimore) 2020;99:e18706. doi: 10.1097/MD.0000000000018706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saliba F, Dharancy S, Salamé E, Conti F, Eyraud D, Radenne S, Antonini T, Guillaud O, Guguenheim J, Neau-Cransac M, Demartin E, Lasailly G, Duvoux C, Sobesky R, Coilly A, Tresson S, Cailliez V, Boillot O, Pageaux GP, Samuel D, Calmus Y, Dumortier J. Time to conversion to an everolimus-based regimen: renal outcomes in liver transplant recipients from the EVEROLIVER registry. Liver Transpl. 2020;26:1465–1476. doi: 10.1002/lt.25879. [DOI] [PubMed] [Google Scholar]
- 15.Jiang M, Zheng H, Xu C, Wang Y, Wan T. Meta-analysis treatment hyperphosphatemia chronic renal failure based on nano lanthanum hydroxide. J Nanosci Nanotechnol. 2020;20:6555–6560. doi: 10.1166/jnn.2020.18576. [DOI] [PubMed] [Google Scholar]
- 16.Guler HS, Tulunay Kaya C, Kumru G, Kosku H, Ozyuncu N, Sengul S, Kutlay S. Acute stunning effect of hemodialysis on myocardial performance: a three-dimensional speckle tracking echocardiographic study. Artif Organs. 2020;44:1081–1089. doi: 10.1111/aor.13698. [DOI] [PubMed] [Google Scholar]
- 17.Smolarek D, Gruchała M, Sobiczewski W. Echocardiographic evaluation of right ventricular systolic function: the traditional and innovative approach. Cardiol J. 2017;24:563–572. doi: 10.5603/CJ.a2017.0051. [DOI] [PubMed] [Google Scholar]
- 18.Abe T, Aoyama T, Sano K, Miyasaka R, Yamazaki T, Honma Y, Tominaga H, Ida M, Arao A, Sakakibara M, Hashimoto K, Takahashi H, Sakai T, Naito S, Koitabashi T, Sano T, Takeuchi Y. Initiation of peritoneal dialysis in a patient with chronic renal failure associated with tetralogy of Fallot: a case report. BMC Nephrol. 2020;21:277. doi: 10.1186/s12882-020-01939-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khaloo P, Qahremani R, Rabizadeh S, Omidi M, Rajab A, Heidari F, Farahmand G, Bitaraf M, Mirmiranpour H, Esteghamati A, Nakhjavani M. Nitric oxide and TNF-α are correlates of diabetic retinopathy independent of hs-CRP and HbA1c. Endocrine. 2020;69:536–541. doi: 10.1007/s12020-020-02353-x. [DOI] [PubMed] [Google Scholar]
- 20.Barraclough K, Hawley CM, McDonald SP, Brown FG, Rosman JB, Wiggins KJ, Bannister KM, Johnson DW. Polymicrobial peritonitis in peritoneal dialysis patients in Australia: predictors, treatment, and outcomes. Am J Kidney Dis. 2010;55:121–131. doi: 10.1053/j.ajkd.2009.08.020. [DOI] [PubMed] [Google Scholar]


