Abstract
Background/Objectives
Trauma survivors with chronic post-traumatic stress disorder (PTSD) have been found to have cognitive impairment. But little is known about these outcomes among Latino and Asians who comprise more than 80% of the U.S. immigrant population. They also experience disparities in PTSD and dementia care albeit increased exposure to trauma. This study aimed to (1) examine the association between trauma exposures and PTSD with cognitive impairment in a sample of Latino and Asian older adults; and (2) assess whether sleep quality attenuated the PTSD-cognitive impairment association.
Design
Cross-sectional secondary analysis of baseline data from the Positive Minds-Strong Bodies (PMSB) randomized controlled trial (RCT) on disability prevention.
Setting
Community-based organizations serving minority or immigrant elders in Massachusetts, New York, Florida or Puerto Rico.
Participants
Hispanic/Latino and Asian/Pacific Islander adults age 60+ eligible per RCT screening for elevated mood symptoms and minor-to-moderate physical dysfunction (n=134 and n=86, respectively).
Measurements
Neuropsychiatric measures were cognitive impairment (MoCA), PTSD (PCL-5), trauma exposure (BTQ), depression (PHQ-9), generalized anxiety (GAD-7), and daytime sleepiness (ESS).
Results
Mean age was 72.8 years and 77.5 years for the Latino and Asian groups, respectively. The Asian group was 100% immigrant, whereas 70.2% (n=92) of the Latino group was foreign-born. In unadjusted models, higher PCL-5 scores were associated with decreased odds of normal cognitive functioning (MoCA ≥ 25) in the Asian group (OR [95% CI] = .93 [.87, .99]), but not the Latino group (OR [95% CI] = .99 [.95, 1.05]). This association remained significant after adjusting for covariates. Daytime sleepiness did not moderate the association between PTSD and cognitive functioning in the Asian group.
Conclusions
Higher PTSD symptoms was associated with cognitive impairment in Asian, but not Latino, older adults. Clinicians serving older Asians should integrate trauma and cognitive screening to ensure this growing, underserved population receives appropriate evidence-based treatments.
Keywords: older adults, trauma, sleep, cognitive impairment, minority health
INTRODUCTION
Previous studies indicate that post-traumatic stress disorder (PTSD) is associated with increased risk of neurocognitive disorders of aging, like Alzheimer’s disaease1, but the causal link of this association remains unclear. One possibility is that chronic stress from PTSD may be causally related to the development of cognitive impairment. Neuroimaging studies have reported that trauma survivors with chronic PTSD have more rapid hippocampal volume loss, reduced cortical thickness, increased β-amyloid deposition, and changes to plasma β-amyloid burden.2–4 Acute stress and PTSD also produce higher levels of cortisol and inflammatory markers associated with greater cognitive decline and dementia risk.5,6 Conversely, PTSD may simply be comorbid with dementia, or dementia may trigger a relapse of symptoms in individuals with a history of PTSD suggesting a bidirectional relationship.7 It is also possible that PTSD predisposes people to developing dementia due to greater vulnerability from social or environmental factors. Sleep problems, which can be precipitated by PTSD, lead to cellular damage in brain structures critical for learning and memory and have been proposed as another potential link explaining the PTSD-dementia connection.8,9
Much of the current understanding of PTSD and dementia has been derived from studies of veterans. In one systematic review of a predominantly male veteran cohort, those diagnosed as having PTSD were at a nearly 2-fold-higher risk of developing dementia compared with those without PTSD.10 The knowledge base is limited, however, regarding how diverse older adults with PTSD across ethnic and racial groups fare in terms of cognitive impairment. This is despite evidence of increased exposure to trauma in this population11, existing disparities in both PTSD and dementia care in ethnic and racial minority groups12,13, and the focus on specific patient cohorts (e.g. veterans) limiting generalizability of the data to other populations. Furthermore, the majority of projected U.S. population growth over the next few decades is linked to Latino and Asian immigration.14 Together, Latinos and Asians make up more than 80% of the U.S. immigrant population.15 By 2060, nearly half of older adults in the U.S. are projected to be racial/ethnic minorities.16
The objectives of this study were therefore to (1) examine the association between trauma exposures and PTSD with prevalence of cognitive impairment in a sample of Latino and Asian minority older adults, and (2) assess whether sleep attenuated the association between PTSD and cognitive impairment.
METHODS
Design
This is a cross-sectional secondary analysis of baseline data from the Positive Minds-Strong Bodies (PMSB) program, a randomized controlled trial (RCT) of a disability prevention intervention offered by community health workers to mostly immigrant older adults in four languages.17 The PMSB program consisted of 10 sessions of individual cognitive behavioral therapy and psychoeducation, and 36 sessions of group exercise training over 6 months. Primary aims of the intervention were to improve mood symptoms and physical functioning (additional details on the intervention development and trial outcomes are available elsewhere.)17,18 Although the PMSB program was not designed specifically for treating trauma, assessment of trauma exposure and PTSD symptoms was included in the research assessments for two reasons. First, previous studies have documented high rates of trauma exposure among racial/ethnic minority older adults living in the U.S.11 Second, two main outcomes of the PMSB program, depression and anxiety, commonly co-occur with PTSD, in part due to overlapping symptom criteria and because exposure to trauma can be an underlying contributor to the disorders.19 Trauma exposure and PTSD symptoms assessment was thus warranted as part of the intervention’s development and CBT treatment. The Massachusetts General Hospital/Partners HealthCare IRB approved the study protocol.
Participants, Setting, and Data Collection
The PMSB study recruited and enrolled community-dwelling older adults from partner community-based organizations (CBOs) and community clinics serving low-income minorities or immigrants in Massachusetts, New York, Florida, or Puerto Rico. To be eligible, participants had to be 60+ years old, speak either English, Spanish, Mandarin or Cantonese, and their screening measures indicated mild to severe anxiety or depressive symptoms—scored five or more on either the Patient Health Questionnaire (PHQ-9)20, the Generalized Anxiety Disorder 7-item Scale (GAD-7)21, or the Geriatric Depression Scale (GDS-15)22—and some degree of mobility limitations—scored between three and 11 in the Short Physical Performance Battery (SPPB).17 Interviews were conducted in English or the primary language spoken by the participant (Spanish, Mandarin, or Cantonese). All measures were validated in these languages in previous studies, or translated and back translated by the research team, with a multinational panel of experts resolving any ambiguities raised during back translation.17 Exclusion criteria included either cognitive impairment as assessed by the Mini-Cog screening instrument23; disclosure of substance use disorders; having received mental health treatment in the last three months or an appointment within the next month; lacking capacity to consent; being homebound; having a neuromusculoskeletal impairment; or not having medical clearance for exercise. Participants disclosing serious suicide plans or attempts were referred to emergency health services per protocol.
In total, 307 out of 1,057 screened participants were eligible and agreed to participate in the trial, 66 of whom self-identified as White/Caucasian, 24 as Black/African/African American, one as American Indian, 102 as Asian/Pacific Islander, 136 as Hispanic/Latino, and nine as other. Participants were assessed at baseline (and then randomized into intervention and control conditions), with follow-ups at two-months, six-months and 12-months. Due to our research question focus on immigrant populations, the present study restricted analysis to Hispanic/Latino and Asian/Pacific Islander respondents with non-missing data in any of the study variables (n=134 and n=86, respectively). In both groups, the source of missing data (n=2 and n=16, respectively) was nonresponse in the outcome variable (the Mini Montreal Cognitive Assessment, MoCA). Since approximately 15% of the observations were missing in the Asian/Pacific Islander group, we tested for differential attrition in all variables included in the present study and found no significant differences between those with missing and non-missing data in the MoCA (Supplementary Table S1). The African American/Afro-Caribbean group was not included due to small sample size (n=24).
Measures
Neuropsychiatric Measures
Mini Montreal Cognitive Assessment (MoCA).
The MoCA is a screening tool for mild cognitive impairment (MCI)24, shown to be sensitive to MCI and predict future cognitive decline. The MoCA five-minute protocol evaluates five cognitive domains (attention, orientation, language, verbal learning and memory, and executive function) and has a maximum score of 30. MoCA scores above 25 are indicative of normal cognitive functioning.24 In the present study, cognitive ability was measured as a binary variable to reflect normal versus abnormal cognitive function (0: MoCA < 25 indicating cognitive impairment; 1: MoCA ≥ 25 indicating normal cognitive functioning).24
Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5).
The PCL-5 is a 20-item screening measure of DSM-5 post-traumatic stress disorder (PTSD) symptoms.25 Using a 5-point Likert scale (1=Not at all, 5=Extremely), participants rated how much they are bothered by PTSD symptoms in the past month to generate a total score ranging from 17 to 85, with higher scores indicating greater symptom severity.25 Since trauma exposure was measured using the Brief Trauma Questionnaire that assesses Criterion A of PTSD per the Diagnostic and statistical Manual (DSM)26, the PCL-5 was administered using the format without Criterion A for PTSD. In the present study, the PCL-5 was included as a continuous scale. We used a continuous variable as the study was not sufficiently powered to use a provisional PTSD cut-off and there are differing cut-offs proposed for different racial-ethnic minority groups.27
Brief Trauma Questionnaire (BTQ).
The BTQ is a 10-item self-report questionnaire designed to assess traumatic exposure according to PTSD Criterion A as outlined in the DSM-5 DSM-IV.26 Respondents are asked about trauma exposures (0=No, 1=Yes) and, if the traumatic event ever happened, whether they thought their life was endangered (0=No, 1=Yes). In the present study, traumatic exposure was measured through a binary variable equal to one if the respondent met DSM-IV A.1 criteria for PTSD and equal to zero otherwise. This indicator of traumatic exposure (measured via the BTQ) and the PCL-5 were positively correlated in our sample (r = .660), consistent with both the difference in time frames of the two instruments (e.g. lifetime versus last month) and an understanding that other risk factors beyond exposure to traumatic events (e.g. coping style, sociocultural context) contribute to the generation of PTSD symptoms.
Patient Health Questionnaire-9 (PHQ-9).
The PHQ-9 is a validated 9-item self-administered measure for depression screening.20 Items are rated on a 4-point Likert-type scale, ranging from 0 (not at all) to 3 (nearly every day). Total score ranges from 0 to 27, with higher scores meaning higher likelihood of depression. In the present study, the PHQ-9 was included as a continuous scale.
Generalized Anxiety Disorder Scale-7 (GAD-7).
The GAD-7 is a 7-item self-rated scale developed as a screening tool and severity indicator for generalized anxiety disorder.21 Each item is scored on a 4-point Likert-type scale (0=not at all, 3=nearly every day), with higher scores reflecting higher severity of symptom. Scores range from 0 to 21. In the present study, the GAD-7 was included as a continuous scale.
Epworth Sleepiness Scale (ESS).
The ESS is a validated 8-item self-administered measure of excessive daytime sleepiness.28 Respondents are asked about their chances of dozing off in different situations on a 4-point Likert scale (0=No chance, 3=High chance), with higher scores indicating increased daytime sleepiness. Total scores range from 0 to 24, with 0–9 considered to be normal while a number > 0 indicates excessive daytime sleepiness requiring medical evaluation. In the present study, daytime sleepiness was included as a binary variable to reflect normal versus excessive daytime sleepiness (0: ESS score between zero and nine, 1: ESS score between ten and 24).
Covariates
Participant self-reported age (continuous), gender (male versus female), educational attainment (below high school versus above high school, including vocational school and higher) and physical health (excellent/very good/good versus fair/poor) were included as additional covariates linked to cognitive impairment.
Data Analysis
We began by comparing all the variables included in the present study between Latinos and Asians, using paired t-tests for continuous variables and chi-square tests for categorical variables (Table 1). We then tested the association between PTSD (PCL-5 scores) and normal cognitive functioning (MoCA scores ≥ 25), calculating crude odds ratio (Figure 1: Model 1) and then adjusted odds ratio (Figure 1: Model 2) controlling for the confounding variables of age, gender, educational attainment, and self-reported physical health. We tested afterwards whether sleep difficulty moderated the association between PTSD and normal cognitive functioning by adding to Model 2 the daytime sleepiness indicator and its two-way interaction with the PCL-5 score (Figure 1: Model 3). In exploratory post-hoc analyses, we repeated the same strategy to examine the association between the binary indicator of traumatic exposure (measured via BTQ) and normal cognitive functioning, the association between depressive symptoms (PHQ-9 scores) and normal cognitive functioning, and the association between anxiety symptoms (GAD-7 scores) and normal cognitive functioning. The estimated odd ratios and their 95% confidence intervals were calculated using logistic regression models in STATA version 15.1, and used two-sided tests at α = .05 for statistical significance. Missing data was handled using listwise deletion. All models were estimated separately for Latinos and Asians.
Table 1.
Baseline demographic and clinical characteristics
| Latino (n=134) | Asian (n=86) | χ2(df) or t(df); p | |
|---|---|---|---|
| Baseline demographics | |||
| Age, mean (SD) [range] | 72.8 (7.0) [62–91] | 77.5 (7.3) [62–95] | t(218) = −4.77; p < .01 |
| Gender, n (%) | |||
| Male | 28 (20.9%) | 19 (22.1%) | χ2(1) = .05; p = .83 |
| Female | 106 (79.1%) | 67 (77.9%) | |
| Education, n(%) | |||
| Less than high school | 54 (40.3%) | 31 (36.1%) | χ2(1) = .40; p = .53 |
| High school or more | 80 (59.7%) | 55 (63.9%) | |
| Place of birth, n(%) | |||
| Outside of U.S. | 92 (70.2%) | 86 (100.0%) | χ2(1) = 31.21; p < .01 |
| U.S. | 39 (29.8%) | 0 (.0%) | |
| Self-rated physical health, n(%) | |||
| Good/Very Good/Excellent | 67 (50.0%) | 20 (23.3%) | χ2(1) = 15.67; p < .01 |
| Fair/Poor | 67 (50.0%) | 66 (76.7%) | |
| Language, n(%) | |||
| English | 6 (4.5%) | 1 (1.2%) | χ2(2) = 216.40; p < .01 |
| Spanish | 128 (95.5%) | 0 (.0%) | |
| Mandarin/Cantonese | 0 (.0%) | 85 (98.8%) | |
| Any chronic conditions, n (%) | |||
| No | 21 (15.7%) | 7 (8.1%) | χ2(1) = 2.68; p = .10 |
| Yes | 113 (84.3%) | 79 (91.9%) | |
| Baseline clinical characteristics | |||
| PTSD (PCL-5), mean (SD) [range] | 15.8 (14.0) [0–62] | 9.5 (11.2) [0–61] | t(218) = 3.53; p < .01 |
| Traumatic exposurea (BTQ), n (%) | |||
| No | 34 (25.4%) | 56 (66.7%) | χ2(1) = 36.32; p < .01 |
| Yes | 100 (74.6%) | 28 (33.3%) | |
| Psychotropic medication useb, n (%) | |||
| No | 108 (80.6%) | 73 (84.9%) | χ2(1) = .66; p = .42 |
| Yes | 26 (19.4%) | 13 (15.1%) | |
| Depression (PHQ-9), mean (SD) [range] | 8.7 (4.7) [0–22] | 6.9 (5.14) [0–24] | t(217) = 2.64; p < .01 |
| Anxiety (GAD-7), mean (SD) [range] | 6.6 (4.4) [0–20] | 4.5 (4.5) [0–21] | t(216) = 3.50; p < .01 |
| ESS scorec, mean (SD) [range] | 8.3 (5.4) [0–24] | 8.3 (4.9) [0–21] | t(218) = −.02; p = .98 |
| 0–9 n (%) | 88 (65.7%) | 58 (67.4%) | χ2(1) = .07; p = .79 |
| 10–24 n (%) | 46 (34.3%) | 28 (32.6%) | |
| MoCA scored, mean (SD) [range] | 19.7 (3.5) [11–29] | 22.1 (3.8) [13–29] | t(218) = −4.84; p <.01 |
| 0–24 n (%) | 125 (93.3%) | 60 (69.8%) | χ2(1) = 21.65; p < .01 |
| 25–30 n (%) | 9 (6.7%) | 26 (30.2%) |
Notes:
Traumatic exposure was defined as meeting DSM-IV A.1 criteria for post-traumatic stress disorder: respondents experienced, witnessed or was confronted with an event or events that involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others.
Psychotropic medication use was assessed through the question “Have you gotten a prescription or medicine for your emotions, nerves or mental health from a psychiatrist, psychiatrist nurse practitioner, or PCP in the last 12-months?”.
ESS scores between 0 and 9 are indicative of a respondent being unlikely to have abnormal sleepiness or an average amount of daytime sleepiness; ESS scores between 10 and 24 are indicative that a respondent may be excessively sleepy and may need medical attention or that a respondent is excessively sleepy and should consider seeking medical attention.
MoCA scores between 0 and 24 are indicative of cognitive impairment; MoCA scores between 25 and 30 are indicative of normal cognitive functioning.
Figure 1. Association between PTSD (PCL-5 scores) and normal cognitive functioning (MoCA scores ≥ 25) among Latino and Asian older adults.
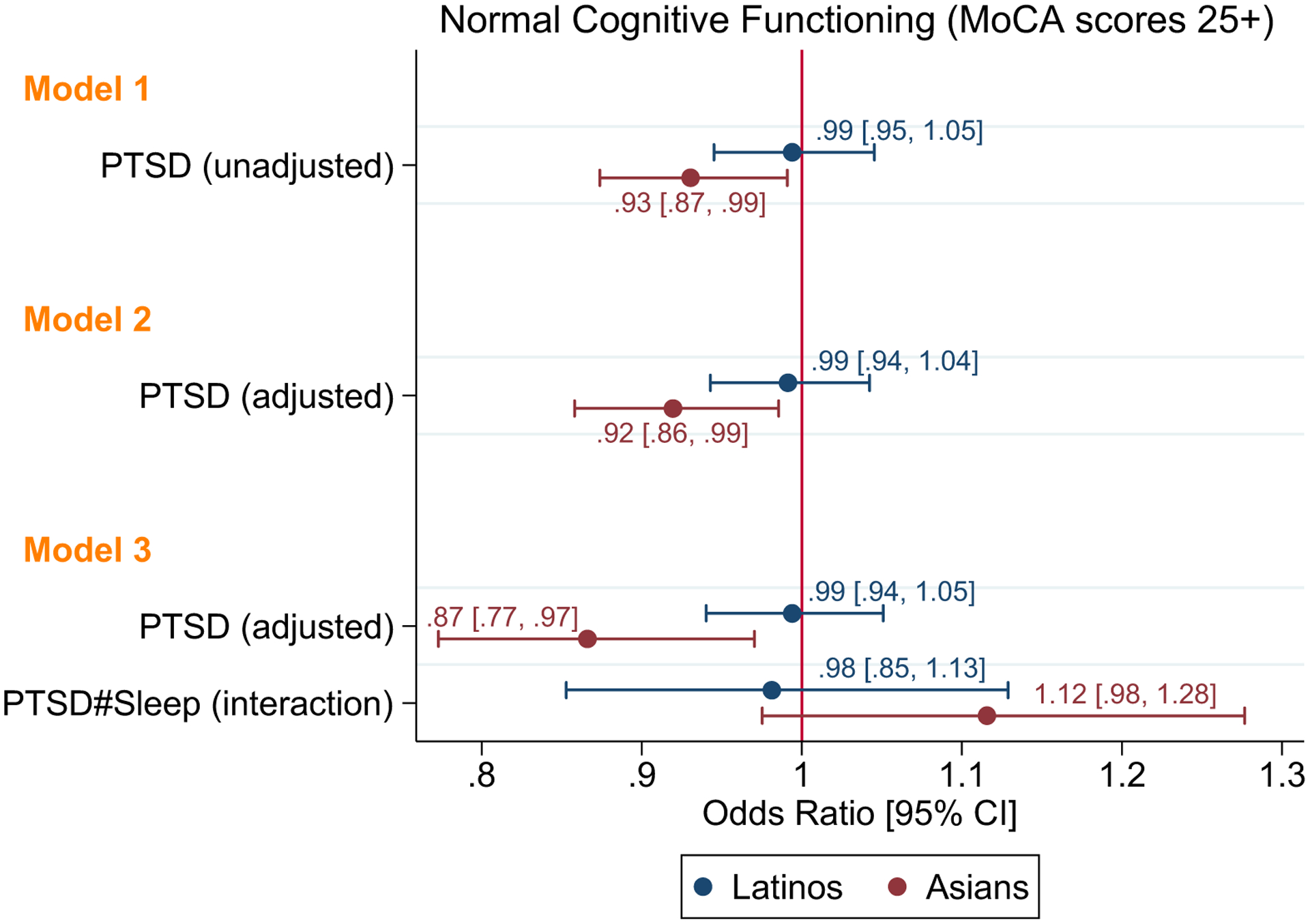
Unadjusted and adjusted odds ratios for the association between PCL-5 and MoCA scores. Two-sided tests at α = .05 were used for statistical significance.
Notes:
Model 1 presents the unadjusted association (crude odds ratio) between PTSD (PCL-5 scores) and normal cognitive functioning (MoCA scores ≥ 25).
Model 2 presents the adjusted association between PTSD and normal cognitive functioning controlling for age, gender, educational attainment and self-reported physical health.
Model 3 tested whether sleep difficulty moderated the association between PTSD and normal cognitive functioning by adding to Model 2 daytime sleepiness and its two-way interaction with PTSD.
RESULTS
Table 1 presents the characteristics of the study sample. Most participants were female, representing 79.1% (n=106) of the Latino sample and 77.9% (n=67) of the Asian sample. The mean age of the Latino group was 72.8 years (SD 7.0) and 77.5 years (SD 7.3) for the Asian group. Around 60% of both groups had at least a high school diploma. The Asian group was 100% immigrant, whereas 70.2% (n=92) of the Latino group was not born in the U.S. Less than 5% of either group selected English as their primary language. The mean scores on measures of PTSD (PCL-5), trauma (BTQ), depression (PHQ-9) and anxiety (GAD-7) were all higher in the Latino group than in the Asian group (Table 1).
Figure 1 presents model estimates of the association between PTSD (PCL-5 scores) and normal cognitive functioning (MoCA scores ≥ 25). In unadjusted models (Model 1), PCL-5 scores were not associated with cognitive functioning in the Latino group (OR [95% CI] = .99 [.95, 1.05]). However, higher PCL-5 scores were associated with decreased odds of normal cognitive functioning in the Asian group (OR [95% CI] = .93 [.87, .99]). This significant association among the Asian group remained after adjusting for confounding variables (Model 2). There was also no evidence that daytime sleepiness (ESS scores) moderated the association between PTSD and normal cognitive functioning in the Asian group (Model 3). No other variable was significantly associated with normal cognitive functioning (Supplementary Table S2).
As previous studies have found the optimal cut-off for cognitive impairment using the MoCA to be 24 for Hispanics29, we conducted sensitivity analyses examining whether our results were different using a cut-off of 24 instead of a cut-off of 25 among the Latino group. Our results remained the same, with no significant association between PTSD (PCL-5 scores) and normal cognitive functioning (MoCA scores ≥ 24) among Latino participants in our sample (Supplementary Table S3). We conducted three additional sets of sensitivity analyses. Since chronic conditions can impair cognition30 and were highly prevalent in our sample (84.3% of Latinos and 91.9% of Asians had at least one chronic condition), we examined whether including chronic conditions in our model impacted our results (Supplementary Table S4: Model 1). We also examined whether adding past-year use of psychotropic medications, which can also affect cognitive function31, affected the observed associations (Supplementary Table S4: Model 2). Finally, within the Latino group, we investigated whether including country of origin (U.S. born versus foreign born) as a proxy for acculturation impacted our findings given potential associations of acculturation with our primary outcome32 (Supplementary Table S4: Model 3). Our results all remained the same in that higher PCL-5 scores were associated with decreased odds of normal cognitive functioning in the Asian group but not in the Latino group, and neither chronic conditions, psychotropic medication use, or country of origin were significantly associated with normal cognitive functioning.
Results from exploratory post-hoc analyses (data not shown) found that neither trauma exposure alone (measured via BTQ) nor depressive (PHQ-9 scores) or anxiety symptoms (GAD-7 scores) were significantly associated with normal cognitive functioning among either Asian or Latinos in both unadjusted and adjusted models. Results suggested then that PTSD, but not trauma exposure, depression or anxiety, was associated with decreased odds of normal cognitive function in Asian but not Latino older adults, and that sleep difficulty did not moderate this association.
DISCUSSION
The current study involved a sample of Latino and Asian mostly immigrant seniors across three states and one U.S. territory (Massachusetts, New York, Florida, and Puerto Rico) participating in a randomized controlled trial. PTSD (PCL-5 scores) were higher in the Latino group as contrasted to Asians, which is consistent with high prevalence rates in the Latino population.33 The literature identifies differences in symptom-reporting among Latinos with a propensity to over-report symptoms during the experience or subsequent to the experience.12,34 A possible explanation for elevated prevalence of PTSD in Latinos could be discrimination, acculturative stress and pre-migration political violence.35
PTSD was associated with cognitive impairment in only the Asian, but not Latino group in multivariate analysis. Several possible explanations could account for the above-mentioned differences. Although we adjusted for age, we did not have information about time with the PTSD symptoms. It might be that because the Asian sample tended to be older, they had longer time with the PTSD symptoms. A study using three nationally representative surveys found that people with PTSD that persists into later life were more likely to have cognitive decline.36
There might also be cultural differences in how PTSD is managed by Asian older adults as compared to Latino older adults. Cultural conflict across generations can harm the mental health of both Latino and Asian older adults37,38, but intergenerational conflict might be managed more by avoidance in Asian older adults and become more severe, particularly among older immigrants.39 Chinese conflict management can be based on one’s status in terms of power, defined by seniority and authority, and the established hierarchy within a social structure or social group.40 But this seniority and authority of the older adult Asian might not be acknowledged by the younger generations living in the U.S., due to acculturation differences, and lead to greater emotional burden among Asians than among Latino older adults.41
The association between PTSD and cognitive impairment that we observe in this study could also be due to variations in acculturation, with previous studies suggesting variations in mental health outcomes among immigrants based on acculturation.42 Previous literature has also found that Asian Americans, compared to white Americans, perceive social support as less helpful when faced with stressful situations.43 As our sample contains a foreign-born Chinese Asian population, there could be contributing roles for immigration-related factors such as acculturation not accounted for in this study. Further, there exists large within-population heterogeneity within Asian American groups, including in the prevalence of cognitive impairment and dementia13. While this study focuses on Mandarin and Cantonese-speaking Chinese older adults, identifying similarities or differences among other Asian American communities to tailor outreach remains an important direction for future research. Overall, this study highlights the importance of clinician screening for trauma-based symptoms alongside cognition to best serve this population. Chinese Americans in particular have been shown to be at high risk for delayed diagnosis and suboptimal treatment of dementia.44,45
Yet screening for cognitive impairment and dementia may be challenging in minority and immigrant communities. Although one-size-fits-all cutoffs are commonly used to define impaired performance on the MoCA, conventional single cutoff scores have been associated with substantially high rates of misclassification in less-educated patients and those identifying as racial/ethnic minorities.46 Various studies have suggested lower cutoff scores to lower the false-positive rate and improve diagnostic accuracy47, particularly in minority communities and among people with lower educational attainment.29 While our sensitivity analyses using a lower cut-off did not alter the study results, further studies are needed to determine most appropriate cutoffs for accurately identifying cognitive impairment in ethnic/racial minority populations. Any screening should consequently be interpreted in conjunction with clinical history, collateral information, and behavioral observations in a clinical encounter.
Clinicians not routinely recognizing or screening for trauma and related distress in older individuals might confront negative downstream implications such as incomplete treatment plans without appropriate psychotherapy48, or interruption of services to address PTSD, above and beyond cognitive decline. Other studies have even identified an increased likelihood of cardiovascular events for those with a PTSD diagnosis.49 In addition to clinicians’ increasing integration of trauma and cognitive screens among Asian American immigrant older adults, there is also a need for increased awareness among minority communities themselves, encouraging receipt of appropriate evidence-based treatment. Health system impacts of neglecting this issue include increased suicide risk and healthcare utilization among older adults, both for those with PTSD and those with cognitive impairment.50,51
We did not find that exposure to traumatic events alone was associated with cognitive impairment, and depression or anxiety did not confer the same risk of cognitive impairment as PTSD. This is consistent with a prior study that also found PTSD conferring greater risk on cognitive impairment than depression symptoms52; in this study, however, the strongest associations were among individuals with comorbid PTSD and depression. How cognitive impairment, mood symptoms, trauma exposure and PTSD are inter-related requires further study.
We did not find support for sleep quality attenuating the relationship between PTSD and cognitive impairment in our sample of Asian immigrant older adults. Recent findings from population-based surveys have revealed disparities in sleep quality and sleep deficiency by race/ethnicity and socioeconomic indicators like income.53 Future research will need to continue to fill this research gap pertaining to immigrants, cognitive impairment, PTSD, and sleep quality.
There are several limitations to this study. First, this cross-sectional study does not establish a causal link between PTSD and cognitive impairment in this population of Latino and Asian older adults. In fact, previous data has suggested a bidirectional relationship7, and these underlying mechanisms need to be further elucidated in prospective studies. Second, there may also be additional confounding variables not included in this study, such as acculturation, discrimination, or traumatic brain injury that have been shown to affect the measures and outcomes used in this study.54–57 Third, there may be concerns about the use of self-reported data. For example, reports of remote traumatic life exposures may be diminished in older adults for whom the events are less salient. Fourth, the small sample size reduces the power of the study to detect differences that may exist between the groups. Fifth, other differences between the groups such as their age and gender distributions impact how generalizable our results are. For example, although we adjust for gender in our models, the samples included more women who do experience more affective disorders. That said, the strength of our study remains the inclusion of a sizeable cohort of diverse older adults under-represented in randomized clinical trials in psychology and psychiatry. An understanding of the connections between immigrant status, race/ethnicity, post-traumatic stress disorder, and cognitive impairment may provide help in explaining outcomes where there are documented health disparities.
Supplementary Material
Supplementary Table S1: Differential attrition comparing Asians with MoCA score and Asians without MoCA scores.
Supplementary Table S2: Additional variables associated with cognitive functioning.
Supplementary Table S3: Model estimates among Latino participants using a MoCA cutoff score of 24.
Supplementary Table S4: Sensitivity analyses with additional controls.
Key Points:
Higher post-traumatic stress disorder (PTSD) symptoms are associated with increased odds of cognitive impairment among Asian, but not Latino, older adults.
Depression or anxiety do not confer the same risk of cognitive impairment as PTSD.
Sleep quality does not attenuate the association between PTSD and cognitive functioning in the Asian older adult group.
Why does this paper matter?
Elucidating the relationship between PTSD and cognition among immigrant Latino and Asian older adults is a critical first step to explaining and addressing mental health and cognitive outcomes where there are documented health disparities.
ACKNOWLEDGEMENTS
Sponsor’s Role:
The funders (NIA, NIMH) had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Funding Statement:
Research reported in this publication was supported by the National Institute on Aging and the National Institute of Mental Health under grant number R01AG046149. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest: The authors have no conflicts to disclose.
REFERENCES
- 1.Song H, Sieurin J, Wirdefeldt K, et al. Association of Stress-Related Disorders With Subsequent Neurodegenerative Diseases. JAMA Neurol 2020; published online March 9. DOI: 10.1001/jamaneurol.2020.0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mohamed AZ, Cumming P, Srour H, et al. Amyloid pathology fingerprint differentiates post-traumatic stress disorder and traumatic brain injury. Neuroimage Clin 2018; 19: 716–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lindemer ER, Salat DH, Leritz EC, McGlinchey RE, Milberg WP. Reduced cortical thickness with increased lifetime burden of PTSD in OEF/OIF Veterans and the impact of comorbid TBI. Neuroimage Clin 2013; 2: 601–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Felmingham K, Williams LM, Whitford TJ, et al. Duration of posttraumatic stress disorder predicts hippocampal grey matter loss. Neuroreport 2009; 20: 1402–6. [DOI] [PubMed] [Google Scholar]
- 5.Yaffe K, Lindquist K, Penninx BW, et al. Inflammatory markers and cognition in well-functioning African-American and white elders. Neurology 2003; 61: 76–80. [DOI] [PubMed] [Google Scholar]
- 6.Swaab DF, Raadsheer FC, Endert E, Hofman MA, Kamphorst W, Ravid R. Increased cortisol levels in aging and Alzheimer’s disease in postmortem cerebrospinal fluid. J Neuroendocrinol 1994; 6: 681–7. [DOI] [PubMed] [Google Scholar]
- 7.Desmarais P, Weidman D, Wassef A, et al. The Interplay Between Post-traumatic Stress Disorder and Dementia: A Systematic Review. Am J Geriatr Psychiatry 2020; 28: 48–60. [DOI] [PubMed] [Google Scholar]
- 8.Mohlenhoff BS, O’Donovan A, Weiner MW, Neylan TC. Dementia Risk in Posttraumatic Stress Disorder: the Relevance of Sleep-Related Abnormalities in Brain Structure, Amyloid, and Inflammation. Curr Psychiatry Rep 2017; 19: 89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mohlenhoff BS, Chao LL, Buckley ST, Weiner MW, Neylan TC. Are hippocampal size differences in posttraumatic stress disorder mediated by sleep pathology? Alzheimers Dement 2014; 10: S146–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yaffe K, Vittinghoff E, Lindquist K, et al. Posttraumatic Stress Disorder and Risk of Dementia Among US Veterans. Arch Gen Psychiatry 2010; 67: 608–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Asnaani A, Hall-Clark B. Recent developments in understanding ethnocultural and race differences in trauma exposure and PTSD. Curr Opin Psychol 2017; 14: 96–101. [DOI] [PubMed] [Google Scholar]
- 12.Alcántara C, Casement MD, Lewis-Fernández R. Conditional risk for PTSD among Latinos: a systematic review of racial/ethnic differences and sociocultural explanations. Clin Psychol Rev 2013; 33: 107–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mehta KM, Yeo GW. Systematic review of dementia prevalence and incidence in United States race/ethnic populations. Alzheimers Dement 2017; 13: 72–83. [DOI] [PubMed] [Google Scholar]
- 14.Lopez MH, Passel JS, Rohal M. Modern Immigration Wave Brings 59 Million to U.S., Driving Population Growth and Change Through 2065. Pew Research Center’s Hispanic Trends Project. 2015; published online September 28. https://www.pewresearch.org/hispanic/2015/09/28/chapter-2-immigrations-impact-on-past-and-future-u-s-population-change/ (accessed June 19, 2020). [Google Scholar]
- 15.Greenstone M, Looney A. Ten Economic Facts about Immigration. Brookings Institute. 1AD; published online November 30. https://www.brookings.edu/research/ten-economic-facts-about-immigration/ (accessed June 19, 2020).
- 16.Mather M, Jacobsen LA, Pollard K. Aging in the United States. Population Reference Bureau 2015; 70. https://www.prb.org/wp-content/uploads/2016/01/aging-us-population-bulletin-1.pdf. [Google Scholar]
- 17.Alegría M, Frontera W, Cruz-Gonzalez M, et al. Effectiveness of a Disability Preventive Intervention for Minority and Immigrant Elders: The Positive Minds-Strong Bodies Randomized Clinical Trial. Am J Geriatr Psychiatry 2019; 27: 1299–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Falgas-Bague I, Ramos Z, del Cueto P, et al. Adaptation of an Evidence-Based Intervention for Disability Prevention, Implemented by Community Health Workers Serving Ethnic Minority Elders. Am J Geriatr Psychiatry 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brady KT, Killeen TK, Brewerton T, Lucerini S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J Clin Psychiatry 2000; 61 Suppl 7: 22–32. [PubMed] [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16: 606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006; 166: 1092–7. [DOI] [PubMed] [Google Scholar]
- 22.Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 1982; 17: 37–49. [DOI] [PubMed] [Google Scholar]
- 23.Borson S, Scanlan JM, Watanabe J, Tu S-P, Lessig M. Simplifying detection of cognitive impairment: comparison of the Mini-Cog and Mini-Mental State Examination in a multiethnic sample. J Am Geriatr Soc 2005; 53: 871–4. [DOI] [PubMed] [Google Scholar]
- 24.Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005; 53: 695–9. [DOI] [PubMed] [Google Scholar]
- 25.Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. J Trauma Stress 2015; 28: 489–98. [DOI] [PubMed] [Google Scholar]
- 26.Schnurr P, Vielhauer M, Weathers F, Findler M. Brief Trauma Questionnaire. 1999. DOI: 10.1037/t07488-000. [DOI]
- 27.Fung HW, Chan C, Lee CY, Ross CA. Using the Post-traumatic Stress Disorder (PTSD) Checklist for DSM-5 to Screen for PTSD in the Chinese Context: A Pilot Study in a Psychiatric Sample. Journal of Evidence-Based Social Work 2019; 16: 643–51. [DOI] [PubMed] [Google Scholar]
- 28.Johns MW. A New Method for Measuring Daytime Sleepiness: The Epworth Sleepiness Scale. Sleep 1991; 14: 540–5. [DOI] [PubMed] [Google Scholar]
- 29.Milani SA, Marsiske M, Cottler LB, Chen X, Striley CW. Optimal cutoffs for the Montreal Cognitive Assessment vary by race and ethnicity. Alzheimers Dement (Amst) 2018; 10: 773–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taylor CA, Bouldin ED, Greenlund KJ, McGuire LC. Comorbid Chronic Conditions Among Older Adults with Subjective Cognitive Decline, United States, 2015–2017. Innovation in Aging 2020; 4: igz045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brooks JO, Hoblyn JC. Neurocognitive Costs and Benefits of Psychotropic Medications in Older Adults. J Geriatr Psychiatry Neurol 2007; 20: 199–214. [DOI] [PubMed] [Google Scholar]
- 32.Martinez-Miller EE, Robinson WR, Avery CL, et al. Longitudinal Associations of US Acculturation With Cognitive Performance, Cognitive Impairment, and Dementia. American Journal of Epidemiology 2020; 189: 1292–1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Roberts AL, Gilman SE, Breslau J, Breslau N, Koenen KC. Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychol Med 2011; 41: 71–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ortega AN, Rosenheck R. Posttraumatic stress disorder among Hispanic Vietnam veterans. Am J Psychiatry 2000; 157: 615–9. [DOI] [PubMed] [Google Scholar]
- 35.Keller A, Joscelyne A, Granski M, Rosenfeld B. Pre-Migration Trauma Exposure and Mental Health Functioning among Central American Migrants Arriving at the US Border. PLoS One 2017; 12. DOI: 10.1371/journal.pone.0168692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Byers AL, Covinsky KE, Neylan TC, Yaffe K. Chronicity of Posttraumatic Stress Disorder and Risk of Disability in Older Persons. JAMA Psychiatry 2014; 71: 540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu J, Dong X, Nguyen D, Lai DWL. Family Relationships and Depressive Symptoms Among Chinese Older Immigrants in the United States. J Gerontol A Biol Sci Med Sci 2017; 72: S113–8. [DOI] [PubMed] [Google Scholar]
- 38.Mulvaney-Day NE, Alegría M, Sribney W. Social cohesion, social support, and health among Latinos in the United States. Soc Sci Med 2007; 64: 477–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Glick JE. Connecting Complex Processes: A Decade of Research on Immigrant Families. Journal of Marriage and Family 2010; 72: 498–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen G-M, Starosta WJ. Chinese Conflict Management and Resolution: Overview and Implications.;: 14.
- 41.Hwang W-C, Myers HF. Major depression in Chinese Americans: the roles of stress, vulnerability, and acculturation. Soc Psychiatry Psychiatr Epidemiol 2007; 42: 189–97. [DOI] [PubMed] [Google Scholar]
- 42.Saadi A, Ponce NA. Worse Mental Health Among More-Acculturated and Younger Immigrants Experiencing Discrimination: California Health Interview Survey, 2015–2016. J Gen Intern Med 2019; published online November 1. DOI: 10.1007/s11606-019-05412-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang S, Shih JH, Hu AW, Louie JY, Lau AS. Cultural differences in daily support experiences. Cultur Divers Ethnic Minor Psychol 2010; 16: 413–20. [DOI] [PubMed] [Google Scholar]
- 44.Chow TW, Liu CK, Fuh JL, et al. Neuropsychiatric symptoms of Alzheimer’s disease differ in Chinese and American patients. Int J Geriatr Psychiatry 2002; 17: 22–8. [DOI] [PubMed] [Google Scholar]
- 45.Mehta KM, Yin M, Resendez C, Yaffe K. Ethnic differences in acetylcholinesterase inhibitor use for Alzheimer disease. Neurology 2005; 65: 159–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wong A, Law LSN, Liu W, et al. Montreal Cognitive Assessment: One Cutoff Never Fits All. Stroke 2015; 46: 3547–50. [DOI] [PubMed] [Google Scholar]
- 47.Davis DH, Creavin ST, Yip JL, Noel‐Storr AH, Brayne C, Cullum S. Montreal Cognitive Assessment for the diagnosis of Alzheimer’s disease and other dementias. Cochrane Database Syst Rev 2015; 2015. DOI: 10.1002/14651858.CD010775.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Clapp JD, Beck JG. Treatment of PTSD in Older Adults: Do Cognitive-Behavioral Interventions Remain Viable? Cognitive and Behavioral Practice 2012; 19: 126–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vidal C, Polo R, Alvarez K, et al. Co-Occurrence of Posttraumatic Stress Disorder and Cardiovascular Disease Among Ethnic/Racial Groups in the United States. Psychosom Med 2018; 80: 680–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Haviland MG, Banta JE, Sonne JL, Przekop P. Posttraumatic Stress Disorder-Related Hospitalizations in the United States (2002–2011): Rates, Co-Occurring Illnesses, Suicidal Ideation/Self-Harm, and Hospital Charges. J Nerv Ment Dis 2016; 204: 78–86. [DOI] [PubMed] [Google Scholar]
- 51.Lin P-J, Zhong Y, Fillit HM, Chen E, Neumann PJ. Medicare Expenditures of Individuals with Alzheimer’s Disease and Related Dementias or Mild Cognitive Impairment Before and After Diagnosis. J Am Geriatr Soc 2016; 64: 1549–57. [DOI] [PubMed] [Google Scholar]
- 52.Sumner JA, Hagan K, Grodstein F, Roberts AL, Harel B, Koenen KC. Posttraumatic stress disorder symptoms and cognitive function in a large cohort of middle-aged women. Depress Anxiety 2017; 34: 356–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Whinnery J, Jackson N, Rattanaumpawan P, Grandner MA. Short and Long Sleep Duration Associated with Race/Ethnicity, Sociodemographics, and Socioeconomic Position. Sleep 2014; 37: 601–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Parkerson HA, Thibodeau MA, Brandt CP, Zvolensky MJ, Asmundson GJG. Cultural-based biases of the GAD-7. J Anxiety Disord 2015; 31: 38–42. [DOI] [PubMed] [Google Scholar]
- 55.O’Driscoll C, Shaikh M. Cross-Cultural Applicability of the Montreal Cognitive Assessment (MoCA): A Systematic Review. J Alzheimers Dis 2017; 58: 789–801. [DOI] [PubMed] [Google Scholar]
- 56.Starck A, Gutermann J, Schouler-Ocak M, Jesuthasan J, Bongard S, Stangier U. The Relationship of Acculturation, Traumatic Events and Depression in Female Refugees. Front Psychol 2020; 11. DOI: 10.3389/fpsyg.2020.00906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Li Y, Li Y, Li X, et al. Head Injury as a Risk Factor for Dementia and Alzheimer’s Disease: A Systematic Review and Meta-Analysis of 32 Observational Studies. PLoS ONE 2017; 12: e0169650. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1: Differential attrition comparing Asians with MoCA score and Asians without MoCA scores.
Supplementary Table S2: Additional variables associated with cognitive functioning.
Supplementary Table S3: Model estimates among Latino participants using a MoCA cutoff score of 24.
Supplementary Table S4: Sensitivity analyses with additional controls.


