Abstract
Burn units have historically used paper diagrams to estimate percent burn; however, unintentional errors can occur. The use of a computer program that incorporates wound mapping from photographs onto a three-dimensional (3D) human diagram could decrease subjectivity in preparing burn diagrams and subsequent calculations of TBSA burned. Analyses were done on 19 burned patients who had an estimated TBSA burned of ≥20%. The patients were admitted to Shriners Hospitals for Children or the University of Texas Medical Branch in Galveston, Texas, from July 2012 to September 2013 for treatment. Digital photographs were collected before the patient’s first surgery. Using BurnCase 3D (RISC Software GmbH, Hagenberg, Austria), a burn mapping software, the user traced partial- and full-thickness burns from photographs. The program then superimposed tracings onto a 3D model and calculated percent burned. The results were compared with the Lund and Browder diagrams completed after the first operation. A two-tailed t-test was used to calculate statistical differences. For partial-thickness burns, burn sizes calculated using Lund and Browder diagrams were significantly larger than those calculated using BurnCase 3D (15% difference, P < .01). The opposite was found for full-thickness burns, with burn sizes being smaller when calculated using Lund and Browder diagrams (11% difference, P < .05). In conclusion, substantial differences exist in percent burn estimations derived from BurnCase 3D and paper diagrams. In our studied cohort, paper diagrams were associated with overestimation of partial-thickness burn size and underestimation of full-thickness burn size. Additional studies comparing BurnCase 3D with other commonly used methods are warranted.
In burn victims, an accurate calculation of TBSA burned is paramount to guiding burn care. The percent TBSA burned is used to determine whether the patient needs to be transferred to a burn center and to calculate both initial fluid resuscitation and nutritional requirements.1–4 Both overresuscitation and underresuscitation of the burn patient can increase morbidity and mortality.5–7 Problems with burn assessment and resuscitation are particularly apparent in obese burn patients8 and children. Thus, a model capable of adjusting for different body types is needed. Gender-specific models would also increase the accuracy of burn size estimations, as the current 2D paper burn diagrams are gender-neutral.9
Traditionally, 2D paper diagrams have been used to estimate TBSA burned. Many diagrams are available, each assigning varying percentages to different parts of the body.6,10,11 The most commonly used methods to calculate TBSA burn include using the size of a patient’s hand to represent 1% TBSA in small burns, the rule of nines, and the Lund and Browder diagram.11–13 The Lund and Browder diagram has been widely used and accepted as standard since 1944.13 This is considered the most precise 2D diagram in terms of adjusting for age and different body segments; however, even when these diagrams are used, overestimation is possible.2,6,10,11,13
Berry et al6 noted that physicians will often adjust for the known error in TBSA burned estimations by arbitrarily increasing the TBSA burned. In addition, an error inherent to estimating burn size using diagrams is the human factor of transferring burns from what is observed on the patient to a diagram. This is known as the “look then draw” technique. The subjective nature of this assessment leads to inaccurate estimations, especially in burns covering a large amount of disjointed and scattered areas and in burns that occur over larger sections of the body such as the torso.5,6,10,11,14 Therefore, human error is difficult to avoid in burn size estimation.
To date, no studies have been undertaken to compare burn size estimations obtained with three-dimensional (3D) computer-aided software with those obtained with standard-of-care methods. The present study was conducted to compare currently used paper Lund and Browder diagrams with a computer-aided program, BurnCase 3D (RISC Software GmbH, Hagenberg, Austria), which relies on clinical patient photographs.
METHODS
Burned Subjects
Nineteen burned patients with an estimated TBSA burned of more than 20% were analyzed. Children were admitted to Shriners Hospital for Children and adults were admitted to the University of Texas Medical Branch in Galveston, Texas, from July 2012 to September 2013 for treatment. This research project was performed under a University of Texas Medical Branch Institutional Review Board–approved protocol.
Subjects and Clinical Care
All subjects were admitted to their respective burn units directly from the scene of injury or from a referring hospital, and they were treated in a similar manner by a team of three burn surgeons. Standard treatment included early excision of third-degree burn wounds, receipt of systemic antibiotics, and continuous enteral feeding. Full-thickness burns were excised and covered with grafts within 48 hours of admission. Full-thickness burns were estimated based on color, presence of hair follicles, blanching, and surrounding skin color. The final estimations of percent TBSA full-thickness burns were determined during surgery, when the burn could be completely excised down to healthy tissue and burn depth could be determined. Patients returned to the operating room as donor sites healed and for reharvesting of homografts (between 6 and 10 days). Additional surgical procedures for excision and grafting were performed until all wounds were covered and healed.
Study Design
At admission, a Lund and Browder diagram was completed by a resident or clinical fellow based on visual assessment of the wound, color of the wound and surrounding tissue, presence of hair follicles, and blanching. This preoperative burn diagram was used to estimate size of the burn wound. During the patient’s first surgery, a resident or clinical fellow examined the extent of the thermal injury and then completed a paper Lund and Browder postoperative diagram, with areas of partial-thickness and full-thickness burns being documented. The diagrams became a part of the patient’s medical record.
Estimation of burn size and depth with BurnCase 3D (RISC Software GmbH, Hagenberg, Austria) was performed by a nonmedical person, who collected digital photographs before the patient’s first surgery and imported these photographs into BurnCase 3D. This nonmedical person, a Research Associate I, had a bachelor’s degree in biological sciences and had no computer background. BurnCase 3D was first developed in 2001 with the help of burn surgeons and has been used clinically in Europe since 2005. The 3D model consists of more than 100,000 triangles that, when summed, equal 100% of the BSA. The burned area marked by the user is the sum of the marked triangles, which is expressed as a percentage of the TBSA.
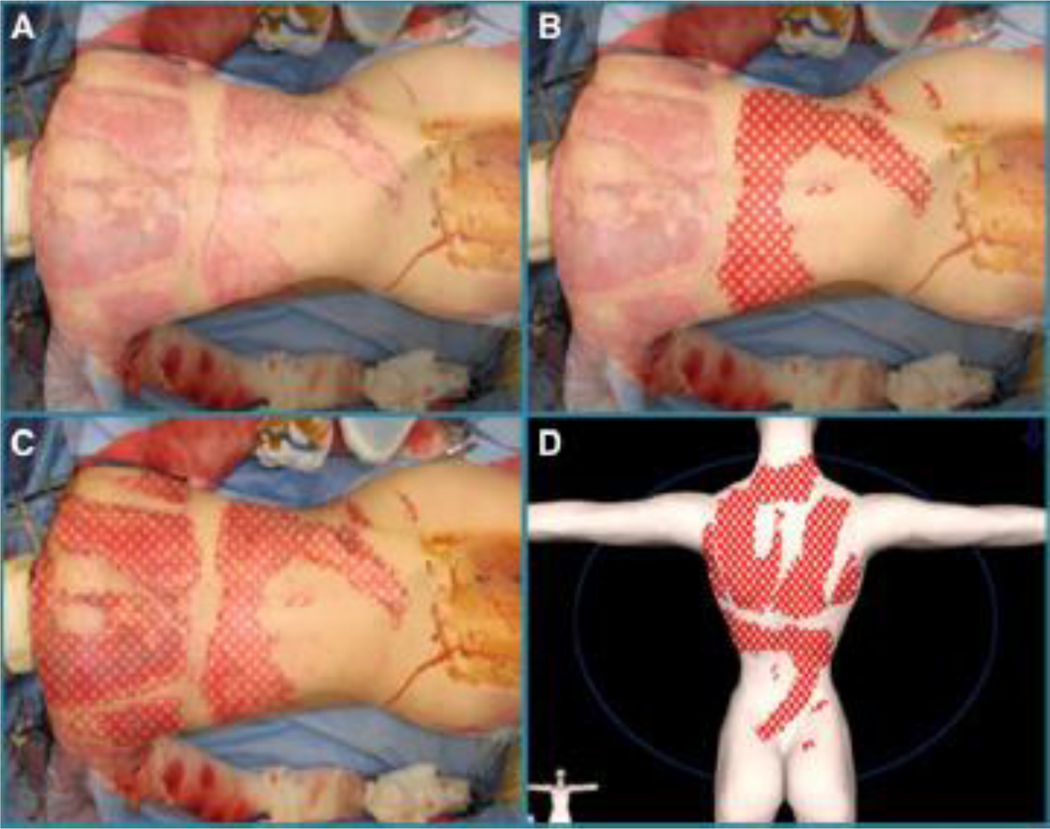
Photographs were superimposed over a 3D diagram matching the patient’s characteristics including height, weight, gender, age, and overall build (normal or corpulent) as demonstrated in Figure 1. The burns were then traced from the picture onto the 3D diagram. Each diagnosis type was made with a distinguishing color and pattern (i.e., a partial-thickness flame burn was designated by light blue diagonal lines while a full-thickness flame burn was noted by red hatch markings). It should be noted that the distinction between partial- and full-thickness burns was made by the user. The computer program calculated the percent partial-thickness, full-thickness, and total burn size based on the tracing. A clinical fellow approved each 3D diagram, which was completed by an individual with no medical training.
Figure 1.
Representative photograph-assisted tracing in BurnCase 3D. A. The posterior torso of a 14-year-old female is shown, superimposed onto a properly fitted and positioned 3D model. B. Partially complete tracing of the burn injury using the photograph as a reference. C. Completed tracing of the burn injury. D. Final depiction of the burn injury to the posterior torso shown on the 3D model alone.
To address possible concerns regarding the accuracy of residents and clinical fellows (more than 5 years of clinical surgical experience) in estimating the percent burn, we conducted a substudy to compare their ratings with those of faculty burn physicians. Blank Lund and Browder diagrams were given to three faculty burn physicians. Each faculty physician was given the age and photographs of the patients. No other names or identifying information were provided. The faculty physicians completed the burn diagrams for each patient based on the photographs.
Data Analysis
Data sets from postoperative Lund and Browder diagrams and BurnCase 3D were entered into Microsoft Excel 2010 (Microsoft, Richmond, VA) for each of the 19 patients. A two-tailed t-test was performed to compare ratings obtained using postoperative Lund and Browder diagrams and BurnCase 3D for each patient’s partial-thickness burn, full-thickness burn, and TBSA burned. P < .05 was considered significant.
The difference between the percent partial-thickness burn estimated using the Lund and Browder diagram and BurnCase 3D was determined for each patient. As we wanted to demonstrate a more accurate difference in the percent burn marked using these two methods, we took the absolute value of the differences. The absolute differences were averaged, and SDs were calculated. This was repeated for both percent full-thickness burned and percent TBSA burned.
The estimates of partial-thickness, full-thickness, and TBSA burned given by the three faculty physicians were averaged for each patient. A two-tailed t-test was performed on these averaged estimations provided by faculty and those calculated by BurnCase 3D. These methods were repeated to compare estimations made by residents/clinical fellows and faculty.
RESULTS
This study included 19 burned patients who were predominately Hispanic men (Table 1). The average patient age was 23 years (range, 16 months to 49 years). Most subjects sustained a flame burn. According to resident- and clinical fellow–completed Lund and Browder diagrams, the average TBSA burned was 55% and the average area with full-thickness burns was 32% (Table 2). According to BurnCase 3D, the average TBSA burned was 50%, with full-thickness burns covering 43% of the TBSA (Table 2). Significant differences in estimations derived from diagrams and BurnCase 3D were noted for TBSA burned (P = .012), partial-thickness burns (P = .006), and full-thickness burns (P = .044).
Table 1.
Demographics and burn injury characteristics
| Characteristic | Value | Minimum | Maximum |
|---|---|---|---|
| N | 19 | - | - |
| Age (yr) | 22.5 ± 14.9 | 1.3 | 49 |
| Gender, males (%) | 15 (79) | - | - |
| BMI (kg/m2) | 24.7 ± 5.6 | 16.5 | 37.8 |
| Ethnicity, N (%) | - | - | |
| African American | 1 (5) | - | - |
| Hispanic | 15 (79) | - | - |
| Caucasian | 3 (16) | - | - |
| Burn type, N (%) | - | - | |
| Flame | 14 (74) | - | - |
| Scald | 1 (5) | - | - |
| Chemical | 1 (5) | - | - |
| Electrical/flame | 3 (16) | - | - |
BMI, body mass index.
Data presented as mean ± SD or counts (%). Double dash represents not applicable.
Table 2.
Burn classifications per diagram
| Burn | Lund and Browder | BurnCase 3D |
|---|---|---|
| Partial thickness, % | 22 ± 20 | 7 ± 10 |
| Full thickness, % | 32 ± 30 | 43 ± 27 |
| TBSA, % | 55 ± 21 | 50 ± 23 |
Data presented as mean ± SD.
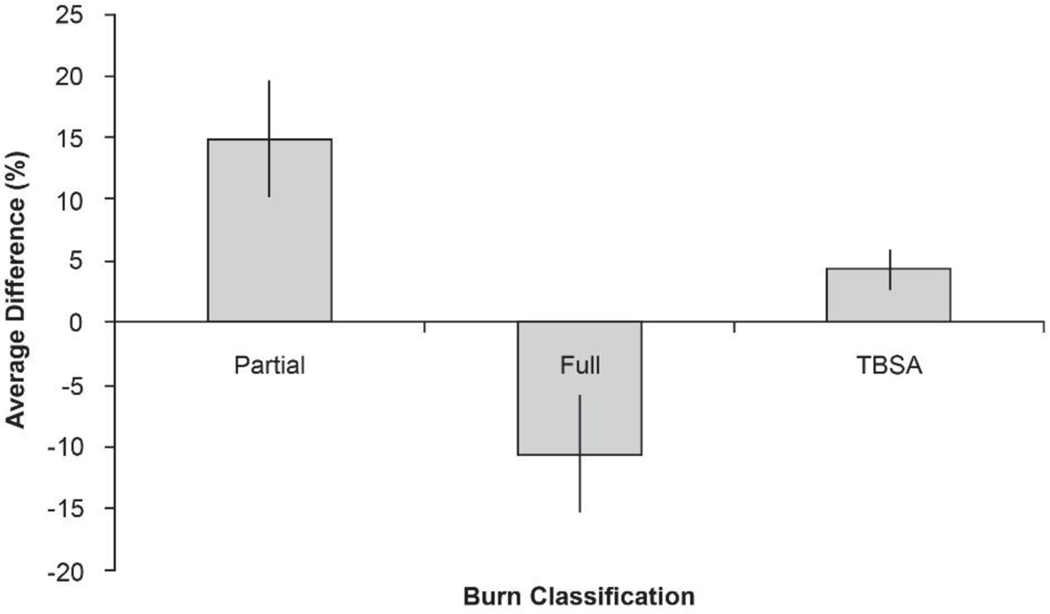
For each patient, the areas marked as partial-thickness burns differed between Lund and Browder diagrams and BurnCase 3D. Similar differences were noted for full-thickness burns and TBSA burned. We observed an average 15% overestimation of partial-thickness burns, 11% underestimation of full-thickness burns, and 4% overestimation of TBSA burned (Figure 2).
Figure 2.
Difference in percent burn obtained using Lund and Browder diagrams and BurnCase 3D. Differences are shown for full-thickness burns (Full; −11 ± 5%), partial-thickness burns (Partial; 15 ± 5%), and TBSA burns (4 ± 2%). Data are presented as the mean ± SEM (%).
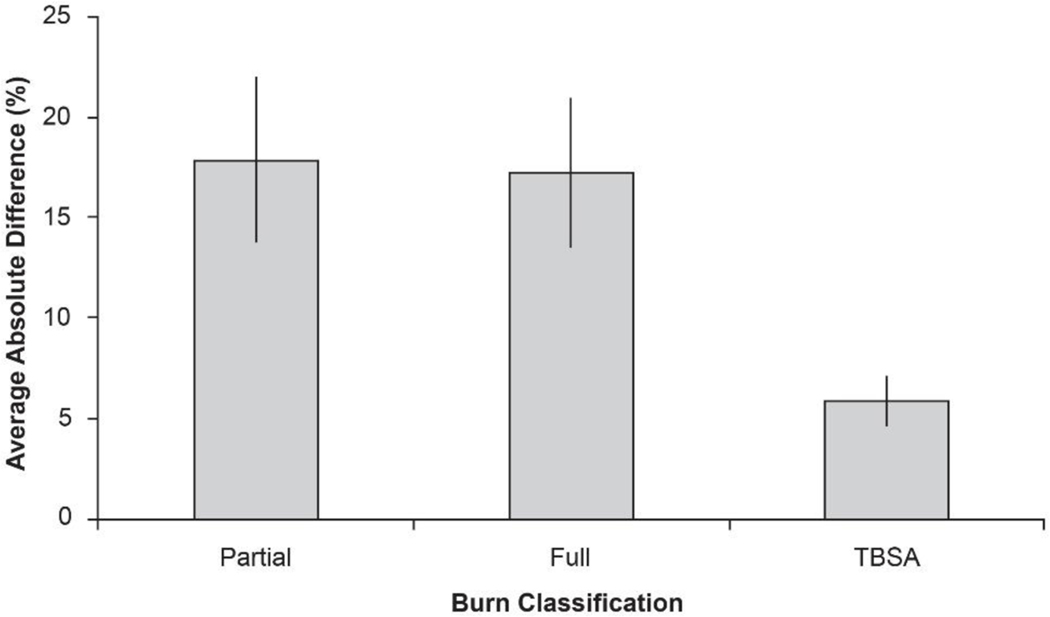
To determine the true extent of error between the Lund and Brower diagram and BurnCase 3D, we analyzed the absolute values of differences. Using this approach, we found that the extent of the incorrectly marked burn area was 18% for partial-thickness burns, 17% for full-thickness burns, and 6% for the TBSA burned (Figure 3).
Figure 3.
Absolute difference in percent burn obtained using Lund and Browder diagrams and BurnCase 3D. Differences are shown for partial-thickness burns (Partial; 18 ± 4%), full-thickness burns (Full; 17 ± 4%), and TBSA (6 ± 1%). Data are presented as the mean ± SEM (%).
When comparing burn sizes estimated by faculty and BurnCase 3D, we found that the percent partial-thickness burned, full-thickness burned, and TBSA burned were similar. The average difference in the percent burned area marked on faculty Lund and Browder diagrams and BurnCase 3D was 1%. No differences were detected between each physician’s estimation, demonstrating that this method has minimal subjectivity. The absence of significant differences between BurnCase 3D and physician-completed Lund and Browder diagrams supports the idea that the use of BurnCase 3D by a nonphysician yields burns size estimations that are as accurate as those derived from physician-completed diagrams. On the other hand, a comparison of faculty estimations with those of residents and clinical fellows revealed differences for partial-thickness burns (P = .004) and full-thickness burns (P = .037).
DISCUSSION
The accuracy of the initial burn diagram is important because the resulting burn size estimate is used not only for initial assessment and treatment but also throughout the patient’s hospitalization as a baseline to assess the progress of wound healing.3,10 Thus, initial diagrams are important for estimating chance of survival and cost of hospitalization as well as predicting length of hospital stay.11,15–17 An accurate calculation of burn size is needed for implementing an individualized treatment plan, identifying surgical needs, and determining fluid and daily caloric goals through discharge and even after.1,2,4,13 Our results show that percent TBSA burned estimated by residents or clinical fellows using Lund and Browder diagrams is inaccurate although estimations performed by faculty using the same technique are not significantly different to estimations derived from BurnCase 3D. The cascading effect that results from improved documentation of the burned area may lead to better patient care, outcome predictors, and research possibilities.
We believe that BurnCase 3D, used by a nonmedical person, is less subjective and subsequently more accurate than the documentation of burns on paper diagrams by a nonfaculty burn physician. This is because one must trace the burn directly from a photograph onto the diagram, rather than trying to replicate what is observed from the patient onto a diagram. Wachtel et al10 suggested recruitment of a medical artist trained with the knowledge of an experienced burn surgeon. However, we believe that using a computer program that allows the user to trace the burn area and that calculates the percent burn is a more feasible alternative.11,18 Computerized 3D models such as BurnCase 3D have been shown to have positive results and be more objective than current methods.5,11,14,19 Therefore, we chose to compare the standard practice of drawing burned areas on a paper diagram to a more technically accurate approach involving tracing burns from photographs onto a 3D computerized diagram. It is important to point out that BurnCase 3D does not need to be used by a burn specialist; it can also be used by medical students or even research associates. However, for the assessment of burn depth, a trained physician’s assistance is recommended. An additional advantage of BurnCase 3D is that it can be adapted to different body types by adjusting parameters such as height, weight, age, gender, and overall build (normal or corpulent). These adjustments may increase accuracy of burn size estimations19 although further investigation is warranted.
In 1957, Artz and Reiss stated “overestimation is common[ly]” observed on burn diagrams, and more than 50 years later the problem remains.6,10,11,20 The standard method for documenting TBSA burned on 2D burn diagrams is antiquated in today’s technological era.10,19 Inaccurate estimation is due to the nature of translating what is seen on a 3D person to a 2D paper diagram, coupled with perception and human factor.11,14,18,19,21 Therefore, updating a 70-year-old method of documentation (i.e., Lund and Browder diagram) to something more fitting in the current age of technology is reasonable.13 Other common methods of estimating burn size that often lead to overestimation are use of the patient’s hand to represent 1% TBSA and the rule of nines.12,22 Some descriptions of using the patient’s hand to represent 1% of the TBSA include the fingers, whereas others exclude the fingers; these inconsistent methods of measurement are problematic.23 The rule of nines is often used as a quick estimation, but it only accommodates average-sized adults and children over 9 years of age.1,3,8,12 Several studies have shown that the use of the rule of nines also leads to an overestimation of burn size.10,24 Thus, none of these methods are without error.
In 1944, Lund and Browder noted that the “proportionate area [of skin burned] has now become of even greater importance as a guide to treatment.”13 Accordingly, the search for the best method of documenting TBSA burned should be ongoing to create the most accurate and individualized treatment plan for burned patients. In 1983, Wachtel and Fortune4 noted “[c]omputer programs often allow more precise resuscitation because they make frequent reassessment possible.” Technology has improved over time, and with these improvements come better methods of documentation (i.e., implementation of electronic medical records although documenting burn diagrams electronically has yet to become standard).
The results regarding estimates by the residents and clinical fellows duplicate those found in several other studies. That is, a general overestimation of the percent burn is common.11,25 The amount of error described in this study is significant and can affect already critically ill burn patients.5–7 Several studies have demonstrated that computerized 3D programs are the most accurate method for analyzing a 3D object.18,21,26 Computerized systems are based on mathematical formulas and empirical data, and they lack a human element and subjectivity. BurnCase 3D allows for patient assessments to be objective and reproducible. Ultimately, better methods of documentation can provide information to improve patient care.
There is a learning curve with the initial use of any computer program. BurnCase 3D is no exception although the user becomes more proficient with time. Thus, practicability of implementation may be an issue as an adequate amount of time is required to produce an accurate burn diagram using BurnCase 3D; however, this is true with any method of documentation.5 Because it is important to initiate the resuscitation process quickly, an initial burn diagram should be made without pictures as a guideline. A more thorough diagram created with superimposed photographs should then follow. An additional limitation is cost, as purchasing the software and camera could be rather expensive. Other limitations include the use of photographs to assess burn depth. Boccara et al15 found that photographs could be used to assess the burn depth accurately more than three quarters of the time; the most common error was overestimation of full-thickness burns. A limitation of this study is the small number of patients. However, because individual patient results were comparable with those of the entire group, we have confidence in our findings. This study was undertaken to obtain preliminary data for further clinical trials, which will validate the method among different burn care providers and characterize the training and time needed for the accurate use of BurnCase 3D.
Our results indicate that sizes of partial-thickness burns, full-thickness burns, and TBSA burns were substantially different between BurnCase 3D and resident- and clinical fellow–completed diagrams. There appeared to be a tendency to overestimate partial-thickness burns and underestimate full-thickness burns. It should be noted that estimated burn size was used in combination with other factors such as vital signs, urine output, acidosis, and pulmonary edema, to guide resuscitation, and all patients received optimal care. Nevertheless, the underestimation of full-thickness burns can be detrimental, affecting one’s ability to assess surgical needs, determine skin substitute requirements, and predict blood loss.
In summary, it is necessary to point out that the BurnCase 3D software needs to be validated for accuracy and reliability. As a future direction, this validation can be done assessing the test–retest reliability of single raters and also by comparing the results of several raters using interrater correlations. Furthermore, additional studies are mandatory to analyze how experience impacts the burn size calculations performed either by residents or other burn care providers. This can be done comparing residents and faculty ratings using the same 3D software, or by comparing the ratings performed with 2D Lund and Browder diagrams, considered to be standard of care at our institution. BurnCase 3D has to be validated to be compared in further studies to additional programs such as the SAGEII Burn Diagram (Sage-Diagram, LLC., Portland, OR) or WoundFlow (U.S. Army Institute of Surgical Research at Fort Sam Houston, TX).
The results of this current study show that, with a greater degree of experience, a more accurate estimation of injury is possible. Wachtel et al10 showed that those with less than 1 year or greater than 2 years of burn experience had the least variability in burn size estimations. Here, diagrams completed by faculty, but not by residents and clinical fellows, were comparable to BurnCase 3D diagrams. At our institution, residents and clinical fellows commonly complete the Lund and Browder diagram, which is then used to obtain a baseline measurement and is included in the patient’s chart. Therefore, BurnCase 3D could be used by all levels of providers to obtain a burn size estimate as accurate as those provided by an experienced physician.
ACKNOWLEDGMENTS
We thank the staff of the intensive care unit and operating room at the University of Texas Medical Branch and Shriners Hospitals for Children for their valuable assistance, especially Jerry Gwinn, Cherry Song, MD, Preetha Muthayya, MD, Karel Capek, MD, and Felicia Williams, MD. In addition, we thank Dr. Kasie Cole for editing and proofreading of the article.
This study was supported by UTMB BP Remembering the 15, Burn Research Education (565450), SHC Special Shared Facility for Clinical Research (84080), National Institutes of Health (P50-GM060338, R01-GM056687, and R01-HD049471), Shriners Hospitals for Children (71006, 71008, 71009), National Institute for Disabilities and Rehabilitation Research (H133A070026 and H133A70019), and Clinical and Translational Science Award (UL1TR000071).
This work was presented in abstract form at the American Burn Association’s 2013 Meeting.
REFERENCES
- 1.Warden GD. Outpatient management of thermal injuries. In: Boswick JA, editors. The art and science of burn care. Rockville, MD: Aspen; 1987. p. 45–51. [Google Scholar]
- 2.Mlcak RP, Buffalo MC, Jimenez CJ. Pre-hospital management, transportation and emergency care. In: Herndon DN, editors. Total Burn Care. 4 edition. London: Elsevier Saunders; 2012. p. 93–102. [Google Scholar]
- 3.McDougal WS, Slade CL, Pruitt BA. Initial Treatment. In: Egdahl RH, editor. Comprehensive manuals of surgical specialties: manual of burns. New York: Springer-Verlag; 1978. p. 31–37. [Google Scholar]
- 4.Wachtel TL, Fortune JB. Fluid resuscitation for burn shock. In: Wachtel TL, Kahn V, Frank HA, editors. Current topics in burn care. London: Aspen; 1983. p. 45–49. [Google Scholar]
- 5.Parvizi D, Kamolz LP, Giretzlehner M, et al. The potential impact of wrong TBSA estimations on fluid resuscitation in patients suffering from burns: things to keep in mind. Burns 2014;40:241–5. [DOI] [PubMed] [Google Scholar]
- 6.Berry MG, Goodwin TI, Misra RR, Dunn KW. Digitisation of the total burn surface area. Burns 2006;32:684–8. [DOI] [PubMed] [Google Scholar]
- 7.Nichter LS, Bryant CA, Edlich RF. Efficacy of burned surface area estimates calculated from charts–the need for a computer-based model. J Trauma 1985;25:477–81. [DOI] [PubMed] [Google Scholar]
- 8.Livingston EH, Lee S. Percentage of burned body surface area determination in obese and nonobese patients. J Surg Res 2000;91:106–10. [DOI] [PubMed] [Google Scholar]
- 9.Hidvegi N, Nduka C, Myers S, Dziewulski P. Estimation of breast burn size. Plast Reconstr Surg 2004;113:1591–7. [DOI] [PubMed] [Google Scholar]
- 10.Wachtel TL, Berry CC, Wachtel EE, Frank HA. The interrater reliability of estimating the size of burns from various burn area chart drawings. Burns 2000;26:156–70. [DOI] [PubMed] [Google Scholar]
- 11.Giretzlehner M, Dirnberger J, Owen R, Haller HL, Lumenta DB, Kamolz LP. The determination of total burn surface area: How much difference? Burns 2013;39:1107–13. [DOI] [PubMed] [Google Scholar]
- 12.Laing JH, Morgan BD, Sanders R Assessment of burn injury in the accident and emergency department: a review of 100 referrals to a regional burn unit. Ann R Coll Surg Engl 1991;73:329–31. [PMC free article] [PubMed] [Google Scholar]
- 13.Lund CC, Browder NC. The estimation of areas of burns. Surg Gynecol Obstet. 1944;19:352–8. [Google Scholar]
- 14.Dirnberger J, Giretzlehner M, Owen R, et al. Objective assessment and measurement of burned body surface area. Burns. 2009;35(Supplement 1):S1–48.22737746 [Google Scholar]
- 15.Boccara D, Chaouat M, Uzan C, Lacheré A, Mimoun M. Retrospective analysis of photographic evaluation of burn depth. Burns 2011;37:69–73. [DOI] [PubMed] [Google Scholar]
- 16.Rittenbury MS, Schmidt FH, Maddox RW, Beazley W III, Ham WT Jr, Haynes BW Jr. Factors significantly affecting mortality in the burned patient. J Trauma 1965;5:587–600. [DOI] [PubMed] [Google Scholar]
- 17.Zawacki BE, Azen SP, Imbus SH, Chang YT. Multifactorial probit analysis of mortality in burned patients. Ann Surg 1979;189:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Igathinathane C, Davis JD, Purswell JL, Columbus EP. Application of 3D scanned imaging methodology for volume, surface area, and envelope density evaluation of densified biomass. Bioresour Technol 2010;101:4220–7. [DOI] [PubMed] [Google Scholar]
- 19.Haller HL, Dirnberger J, Giretzlehner M, Rodemund C, Kamolz L. “Understanding burns”: research project BurnCase 3D–overcome the limits of existing methods in burns documentation. Burns 2009;35:311–7. [DOI] [PubMed] [Google Scholar]
- 20.Artz CP, Reiss E. General immediate care. In: Artz CP, Moncrief JA, editors. Treatment of burns. London: Saunders; 1957. p. 17–25. [Google Scholar]
- 21.Prieto MF, Acha B, Gómez-Cía T, Fondón I, Serrano C. A system for 3D representation of burns and calculation of burnt skin area. Burns 2011;37:1233–40. [DOI] [PubMed] [Google Scholar]
- 22.American Burn Association. Advanced Burn Life Support Student Manual. 1 edition. Chicago, IL: American Burn Association; 2007. [Google Scholar]
- 23.Jose RM, Roy DK, Vidyadharan R, Erdmann M. Burns area estimation-an error perpetuated. Burns 2004;30:481–2. [DOI] [PubMed] [Google Scholar]
- 24.Hammond JS, Ward CG. Transfers from emergency room to burn center: errors in burn size estimate. J Trauma 1987;27:1161–5. [DOI] [PubMed] [Google Scholar]
- 25.Chan QE, Barzi F, Cheney L, Harvey JG, Holland AJ. Burn size estimation in children: still a problem. Emerg Med Australas 2012;24:181–6. [DOI] [PubMed] [Google Scholar]
- 26.Yu CY, Lin CH, Yang YH. Human body surface area database and estimation formula. Burns 2010;36:616–29. [DOI] [PubMed] [Google Scholar]