Abstract
Purpose
Patients who have undergone gastrectomy have unique symptoms that are not appropriately assessed using currently available tools. This study developed and validated a symptom-focused quality of life (QoL) questionnaire for patients who have received gastrectomy for gastric cancer.
Materials and Methods
Based on a literature review, patient interviews, and expert consultation by the KOrean QUality of life in Stomach cancer patients Study group (KOQUSS), the initial item pool was developed. Two large-scale developmental studies were then sequentially conducted for exploratory factor analyses for content validity and item reduction. The final item pool was validated in a separate cohort of patients and assessed for internal consistency, test-retest reliability, construct validity, and clinical validity.
Results
The initial questionnaire consisted of 46-items in 12 domains. Data from 465 patients at 11 institutions, followed by 499 patients at 13 institutions, were used to conduct item reduction and exploratory factor analyses. The final questionnaire (KOQUSS-40) comprised 40 items within 11 domains. Validation of KOQUSS-40 was conducted on 413 patients from 12 hospitals. KOQUSS-40 was found to have good model fit. The mean summary score of the KOQUSS-40 was correlated with the EORTC QLQ-C30 and STO22 (correlation coefficients, 0.821 and 0.778, respectively). The KOQUSS-40 score was also correlated with clinical factors, and had acceptable internal consistency (> 0.7). Test-retest reliability was greater than 0.8.
Conclusion
The KOQUSS-40 can be used to assess QoL of gastric cancer patients after gastrectomy and allows for a robust comparison of surgical techniques in clinical trials.
Keywords: Stomach neoplasms, Quality of life, Surveys and questionnaires, Validation study
Introduction
In recent years, the proportion of cases of early gastric cancer among the overall incidence of gastric cancer has increased to more than 70% in Korea [1,2]. Patients treated for early gastric cancer have excellent prognosis, and most patients can return to their routine normal lives. However, many experience a variety of symptoms following gastrectomy, which may continue long after surgery. These symptoms are collectively referred to as postgastrectomy syndromes and include early satiety, dumping syndrome, dysphagia, reflux, and psychological problems. It is essential to evaluate these symptoms and understand and design intervention to manage these symptoms properly.
To date, many instruments have been developed to assess quality of life (QoL) in patients with gastric cancer. The European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ-STO22) and the Functional Assessment of Cancer Therapy-gastric (FACT-Ga) are commonly known instruments [3,4]. The EORTC QLQ-STO22 has been translated into many languages, including Korean, and has been used in many clinical trials and retrospective studies of Korean patients with gastric cancer [5–8].
However, existing gastric cancer-specific questionnaires, such as the EORTC QLQ-STO22 and FACT-Ga, assess only general gastrointestinal symptoms and are unable to assess symptoms specifically related to gastric surgery such as postgastrectomy syndrome. The only validated tool that allows for evaluation of symptoms, living status, and QoL after gastrectomy is the Post Gastrectomy Syndrome Assessment Scale (PGSAS-45) [9]. However, the PGSAS-45 is based on expert opinion and consensus, not developed using statistical analysis of patient data. Therefore, a rigorously developed and validated patient-centered questionnaire that can assess postgastrectomy symptoms and QoL is necessary.
In this study, we report the development and validation of a QoL questionnaire for patients who have received gastrectomy for gastric cancer, with special emphasis on postgastrectomy syndrome.
Materials and Methods
1. The KOrean QUality of life in Stomach cancer patients Study group (KOQUSS)
The KOrean QUality of life in Stomach cancer patients Study group (KOQUSS) was created in January 2016 by surgeons to develop a method for assessing appropriately the QoL of gastric cancer patients who have undergone gastrectomy. Additional experts have joined the KOQUSS in the course of meetings. Currently, the KOQUSS includes a broad range of disciplines, including surgeons, oncologists, a clinical epidemiologist, and a psychometrician from 27 institutions in the Republic of Korea.
2. Study flow
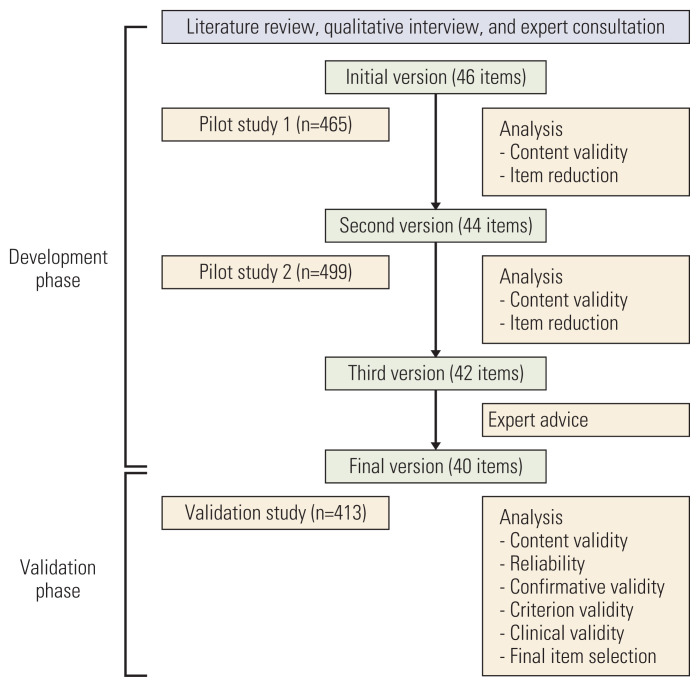
This study consisted of two phases: development and validation. Fig. 1 provides a schema of the study.
Fig. 1.
Study flowchart.
1) Development phase
A comprehensive literature review of preexisting questionnaire items and a review of patients’ self-reported symptoms as documented in outpatient clinics were first conducted to bring together items for consideration. Items were developed using a four-point Likert scale. The level of satisfaction was assessed as very satisfied, slightly satisfied, slightly dissatisfied, and very dissatisfied, while the level of agreement was assessed as disagree, somewhat agree, quite agree, strongly agree.
The items were reviewed for content by experts in the KOQUSS study group. This was followed by two sets of qualitative interviews of 30 and 50 patients to determine the readability, comprehensibility, and acceptability of each item and to invite suggestions for possible improvement. The initial items were selected by general agreement in KOQUSS task force meetings from February 2016 to January 2017.
Two separate studies were then conducted for exploratory factor analyses and item reduction. Participants were recruited from gastric cancer surveillance clinics in 11 hospitals between September to December 2017, and subsequently from 13 hospitals between May to July 2018. The eligibility criteria were as follows: (1) received gastrectomy for gastric cancer, (2) received regular follow-up within the 5 years following the operation, and (3) no communication problems. Informed consent was obtained from eligible patients. The questionnaires were self-administered. The results of factor analyses with input from expert consultation were used to select items for each domain for the validation phase. Statistical analyses are separately described below.
2) Validation phase
Participants were recruited from gastric cancer surveillance clinics in 12 hospitals for validation of the questionnaire. The eligibility criteria were the same as those of the developmental studies. Patients who had already been exposed to any previous version of the questionnaire were excluded. Participants were asked to complete the developed questionnaire, as well the EORTC QLQ-C30 and STO22, which were then used for analysis of criterion validity. Participants were also asked to mail back a completed second copy of the questionnaire within 30 days of completing the first test for test-retest analysis.
Patients’ demographic and clinicopathological data were collected through a medical chart review, namely, age, sex, marital status, education, body mass index, surgical appr-oach, extent of gastrectomy, pathological stage, and presence of adjuvant chemotherapy. The pathological stage was classified according to the American Joint Committee on Cancer, 8th edition [10]. Data on surgical resection included type of surgery (distal, proximal, pylorus-preserving, or total gastrectomy) and surgical approach (open, laparoscopic, or robotic). All instruments in this study adhere to radical gastrectomy with lymph node dissection according to gastric cancer treatment guidelines, and adjuvant chemotherapy is recommended for patients diagnosed as pathologically stage II or greater [11–13].
3. Statistical analysis
1) Sample size
The sample sizes of the two large-scale developmental studies and that of the validation study were determined based on the “rule of 10,” which states that there should be at least 10 cases for each item in the instrument [14]. The first (second) study in the developmental phase required 460 (440) participants to test 46 (44) item pools, while the validation study required 320 participants to examine 32 item pools. For test-retest reliability, a random sample of 103 subjects, each measured twice, produces a two-sided 95% confidence interval with a width of 0.2 when the estimated intra-class correlation is 0.7. Considering a 20% dropout rate, we arrived at a sample size of 129, which were enrolled competitively.
2) Developmental phase
Item scores were examined using mean and standard deviation. Skewness and kurtosis were also calculated with standard error. Principal components analysis was used to extract common factors with the criterion of eigenvalues > 1 and with reference to a scree plot. Highly correlated items (r > 0.7) were considered redundant; in such a case, the item that explained the greatest variation was chosen to remain. A weak correlation (< 0.2) between an item and the sum of the remaining items in the scale indicated that the item was not measuring the same construct as the other items [15]. Construct validity was evaluated by calculating Pearson correlation coefficients between the items and domains generated by the exploratory factor analysis. The suitability of the data for structure detection was evaluated by Kaiser-Meyer-Olkin (KMO) test and Bartlett’s test of sphericity [15]. KMO values between 0.8 and 1 were considered to denote adequate sampling for factor analysis. For Bartlett’s test of sphericity, p < 0.05 was taken to indicate possible utility of factor analysis for the data.
Factor loadings and error variance for each item and covariances between domains were evaluated for the confirmatory factor analysis. Goodness of fit was assessed by chi-squared value, Bentler comparative fit index (CFI), standardized root mean square residual (SRMR), and root mean square error of approximation (RMSEA).
3) Scoring approach for KOQUSS-40
The scoring system for the final questionnaire was generated based on methods used for EORTC QLQ-C30 and QLQ-STO22, in which raw scores (the average of the items that contribute to the domain) are divided by ranges [16]. As all items of the KOQUSS-40 were rated using a four-point Likert scale, the range of all items was 3. Therefore, the score for each domain was calculated as the [(raw score–1)/3]×100. We also adopted the principle of summary scoring used by the QLQ-C30 to develop an intuitive summary score for the KOQUSS-40 for post gastrectomy symptoms. The summary score was defined as the mean of eight equally weighted symptom domains and was included in the explorative factor analysis [17].
4) Validation phase
Internal consistency of the items was estimated using the Cronbach’s alpha; values between 0.7 and 0.9 were considered optimal [14,15,18]. Items whose removal resulted in substantial improvement of the Cronbach’s alpha were eliminated, and the Cronbach’s alpha for the remaining items were recalculated [15]. Test-retest reliability was assessed using Spearman’s correlations.
Criterion validity was assessed by comparing the scores of the KOQUSS-40 with those of the validated Korean version of the EORTC QLQ-C30 and QLQ-STO22 [19,20]. The summary scores of the EORTC QLQ-C30 were calculated as the mean of 13 of the 15 QLQ-C30 scales (the Global Quality of Life scale and the Financial Impact scale were not included), and those of the EORTC QLQ-STO22 from the mean of nine scales [17,21].
Clinical validity was evaluated by comparing the scores of the KOQUSS-40 in different patient groups. Patients were divided into two groups according to their weight loss (less than 10% vs. 10% or more), extent of surgery (partial vs. total gastrectomy), and surgical approach (open vs. laparoscopic/robotic).
Statistical analyses were performed using SAS ver. 9.4 (SAS Institute Inc., Cary, NC). p < 0.05 were considered statistically significant.
Results
1. Developmental phase
The literature review, patient interviews and expert review resulted in 46 initial items. Factor analysis was conducted using data from the first developmental study of 465 pati-ents from 11 hospitals to examine content validity and for item reduction. The KMO measure of sampling adequacy and Bartlett’s test value were 0.905 and < 0.001, respectively, indicating suitability of the data for factor analysis. The presence of 11 domains was determined by inspection of a scree plot. Eight items were considered for elimination on the basis of construct validity and internal consistency. Among these eight items, three items (“Have you ever been annoyed?” “Do you feel that food fills you up?” and “Has your hair fallen out?”) were removed on the bases of reduced internal consistency as estimated by the Cronbach’s alpha, and one item (“Do you have difficulty in defecating because of hard stools?”) was divided into two items to clarify ambiguous questioning (“Do you feel uncomfortable due to constipation?” and “Do you have hard stools?”). After discussion among the investigators, the other four items remained in the instrument given their clinical significance. Finally, the first draft instrument was reduced to 44 items with 11 domains.
The second exploratory factor analysis was performed on the data from the second developmental study of 499 patients from 13 hospitals. The KMO measure and Bartlett’s test value were 0.923 and < 0.001, respectively, and eight domains were selected by inspection of a scree plot. Among five candidate items for elimination, two (“Are you uncomfortable with bad breath?” and “Do you have watery stools?”) were deleted and three retained due to their clinical significances after discussion among the investigators. Two items (“Has your sense of taste changed?” and “Is it difficult for you to swallow food?”) from the indigestion domain had Pearson correlation coefficient of 0.7, and were removed after review by the phychometrician. The final questionnaire consisted of 40 items with 11 domains (KOQUSS-40).
2. Validation of KOQUSS-40
The structure of the KOQUSS-40 questionnaire is summarized in Table 1. Among the 40 items, 32 items address postgastrectomy symptoms in eight domains, while eight items were retained in the questionnaire given their clinical importance based on expert consensus. The eight domains are indigestion, dysphagia, reflux, dumping syndrome, bowel habit changes, constipation, psychological factors, and worry about cancer. The English version of the KOQUSS-40 was developed via translation from Korean to English by two independent bilingual translators and back-translation by two other independent bilingual translators. The English and Korean versions of the KOQUSS-40 are provided in S1 and S2 Tables.
Table 1.
Structure of the KOQUSS-40 questionnaire for evaluating postgastrectomy symptoms and quality of life
| Domain | No. of items | Items |
|---|---|---|
| General quality of life | 3 | 1, 2, 3 |
| Indigestion | 6 | 6, 7, 8, 9, 10, 11 |
| Dysphagia | 3 | 12, 13, 14 |
| Reflux | 3 | 15, 16, 17 |
| Dumping syndrome | 5 | 18, 19, 20, 21, 22 |
| Bowel habit change | 5 | 23, 24, 25, 26, 27 |
| Constipation | 2 | 28, 29 |
| Psychological factors | 5 | 30, 31, 32, 33, 34 |
| Worry about cancer | 3 | 35, 36, 37 |
| Scar problems | 3 | 4, 38, 39 |
| Financial problems | 2 | 5, 40 |
KOQUSS-40 data from 413 patients from 12 hospitals were included for the validation study. Among these participants, 140 patients completed the questionnaire twice for the test-retest analysis. The mean time and standard deviation (SD) between gastrectomy and survey response was 20.4 months (SD, 16.8), and 40.3% of the patients received gastrectomy within one year of the survey.
Table 2 shows the demographic and clinicopathological characteristics of the patients who participated in the validation study. The mean age was 59.7 years and there were more male than female patients (66.1% males). Most patients were married (86.2%), had graduated high school or university (65.1%), and had normal body mass index (58.6%). The majority of patients were stage I (75.8%), and distal gastrectomy (73.1%) and laparoscopic (67.1%) were the most frequent surgical extent and approach, respectively.
Table 2.
Patient demography and clinicopathological characteristics in the validation study
| Characteristic | No. (%) |
|---|---|
| Age, mean±SD (yr) | 59.7±10.8 |
| Sex | |
| Male | 273 (66.1) |
| Female | 140 (33.9) |
| Marital status | |
| Never married | 26 (6.3) |
| Living as married | 356 (86.2) |
| Widowed/Divorced/Separated | 18 (4.4)/12 (2.9)/1 (0.2) |
| Education | |
| Elementary school | 34 (8.2) |
| Middle school | 62 (15.0) |
| High school | 143 (34.6) |
| University or higher | 126 (30.5) |
| Unknown | 48 (11.6) |
| BMI (kg/m2) | |
| < 18.5 | 13 (3.1) |
| 18.5–25.0 | 242 (58.6) |
| > 25.0 | 158 (38.3) |
| Surgical approach | |
| Open | 121 (29.3) |
| Laparoscopic | 277 (67.1) |
| Robotic | 15 (3.6) |
| Extent of gastrectomy | |
| Distal | 302 (73.1) |
| Total | 81 (19.6) |
| Pylorus-preserving | 21 (5.1) |
| Proximal | 9 (2.2) |
| Stage | |
| 1 | 313 (75.8) |
| 2 | 58 (14.0) |
| 3 | 40 ( 9.7) |
| 4 | 2 (0.5) |
| Adjuvant chemotherapy | |
| None | 314 (76.0) |
| In chemotherapy | 38 (9.2) |
| History of complete chemotherapy | 52 (12.6) |
| History of incomplete chemotherapy | 9 (2.2) |
BMI, body mass index; SD, standard deviation.
Descriptive statistics of the 40 items showed that there was no missing data, and all item scores ranged from 1 to 4 except for item number 38 (S3 Table). Item number 38 was a question about pain in the surgical scar, and no respondents checked score 4 (strongly agree) to this question. The absolute values of skewness and kurtosis were less than 3 and 10, respectively.
Statistical modeling was used to evaluate the fit of the questionnaire structure of 32 items among eight domains for assessing postgastrectomy symptoms. The goodness of fit indices, chi-squared statistic, degrees of freedom, Bentler CFI, SRMR, and RMSEA were 1,482.92, 499, 0.830, 0.073, and 0.069 (95% confidence interval, 0.065 to 0.073), respectively. The ratio of the chi-square to the degrees of freedom was < 5, suggesting good model fit. Although the Bentler CFI failed to meet the recommended criterion according to the literature, SRMR < 0.08 was interpreted as denoting good fit. Additionally, the upper 95% confidence interval of RMSEA was < 0.08, confirming good model fit.
The correlation matrix indicated that most item-pairs were moderately correlated (r < 0.7) except for two pairs of items that were borderline high (0.7 and 0.69). The correlation coefficients between items and their own domains were acceptable and ranged from 0.2 to 0.6. Weak correlations between items and other domains were observed.
To evaluate criterion validity, the summary scores for the KOQUSS-40, EORTC QLQ-C30, and STO22 were investigated (Table 3). The summary scores of the KOQUSS were calculated as the mean of eight of the 11 domains, since the eight domains were derived from the exploratory factor analyses, but the other items were retained without statistical analysis based on expert consensus. The correlation coefficient between the KOQUSS-40 and EORTC QLQ-C30 summary scores was 0.821 (p < 0.001), and between the KOQUSS-40 and QLQ-STO22 summary scores was 0.778 (p < 0.001), both indicating that the trend in the information captured by the KOQUSS-40 followed the same trend as the other instruments. The constipation domain exhibited a high correlation coefficient only with the constipation item of the EORTC QLQ-C30, exhibiting excellent discrimination for constipation.
Table 3.
Correlation between KOQUSS-40 and EORTC QLQ-C30 and QLQ-STO22 at the level of domains, and totals
| Indigestion | Dysphagia | Reflux | Dumping | Bowel habit change | Constipation | Psychological factor | Worry about the cancer | KOQUSS-40 factor | |
|---|---|---|---|---|---|---|---|---|---|
| EORTC QLQ-C30 and STO22 total score | 0.692** | 0.586** | 0.515** | 0.610** | 0.494** | 0.320** | 0.734** | 0.545** | 0.848** |
| EORTC QLQ-C30 total score | 0.659** | 0.543** | 0.477** | 0.598** | 0.490** | 0.328** | 0.761** | 0.502** | 0.821** |
| EORTC QLQ-STO22 total score | 0.650** | 0.571** | 0.502** | 0.548** | 0.435** | 0.266** | 0.602** | 0.537** | 0.778** |
| EORTC QLQ-C30 functional scales | |||||||||
| Physical function | 0.595** | 0.409** | 0.307** | 0.380** | 0.236** | 0.119* | 0.522** | 0.372** | 0.562** |
| Role function | 0.543** | 0.374** | 0.264** | 0.357** | 0.237** | 0.110* | 0.512** | 0.369** | 0.528** |
| Emotional function | 0.436** | 0.345** | 0.319** | 0.418** | 0.316** | 0.216** | 0.750** | 0.416** | 0.606** |
| Cognitive function | 0.332** | 0.323** | 0.329** | 0.421** | 0.341** | 0.096 | 0.588** | 0.271** | 0.502** |
| Social function | 0.436** | 0.316** | 0.256** | 0.315** | 0.214** | 0.181** | 0.459** | 0.327** | 0.477** |
| EORTC QLQ-C30 symptom scales | |||||||||
| Fatigue | 0.582** | 0.420** | 0.318** | 0.478** | 0.349** | 0.187** | 0.588** | 0.459** | 0.640** |
| Nausea | 0.426** | 0.438** | 0.404** | 0.469** | 0.314** | 0.232** | 0.383** | 0.288** | 0.552** |
| Pain | 0.369** | 0.414** | 0.339** | 0.373** | 0.286** | 0.193** | 0.392** | 0.321** | 0.505** |
| Constipation | 0.230** | 0.171** | 0.282** | 0.265** | 0.178** | 0.603** | 0.348** | 0.215** | 0.431** |
| Diarrhea | 0.259** | 0.265** | 0.282** | 0.374** | 0.666** | 0.138** | 0.329** | 0.210** | 0.463** |
| Dyspnea | 0.285** | 0.332** | 0.342** | 0.423** | 0.271** | 0.178** | 0.383** | 0.179** | 0.441** |
| Appetite | 0.591** | 0.362** | 0.252** | 0.304** | 0.172** | 0.170** | 0.381** | 0.334** | 0.495** |
| Sleep disturbance | 0.325** | 0.311** | 0.233** | 0.330** | 0.298** | 0.180** | 0.603** | 0.350** | 0.495** |
| EORTC QLQ-STO22 scales | |||||||||
| Dysphagia | 0.543** | 0.582** | 0.419** | 0.431** | 0.316** | 0.205** | 0.431** | 0.421** | 0.635** |
| Pain | 0.399** | 0.391** | 0.381** | 0.481** | 0.509** | 0.215** | 0.411** | 0.295** | 0.572** |
| Reflux | 0.378** | 0.453** | 0.688** | 0.470** | 0.314** | 0.302** | 0.429** | 0.239** | 0.610** |
| Eating restriction | 0.666** | 0.515** | 0.396** | 0.470** | 0.315** | 0.177** | 0.465** | 0.435** | 0.655** |
| Anxiety | 0.401** | 0.297** | 0.210** | 0.313** | 0.326** | 0.149** | 0.397** | 0.598** | 0.515** |
| EORTC QLQ-STO22 single items | |||||||||
| Dry mouth | 0.345** | 0.259** | 0.301** | 0.290** | 0.170** | 0.098† | 0.334** | 0.154** | 0.367** |
| Taste change | 0.502** | 0.424** | 0.358** | 0.339** | 0.269** | 0.209** | 0.461** | 0.327** | 0.550** |
| Body image | 0.381** | 0.339** | 0.184** | 0.300** | 0.247** | 0.156** | 0.422** | 0.464** | 0.476** |
| Hair loss | 0.071 | 0.037 | −0.010 | 0.074 | 0.057 | 0.031 | −0.009 | 0.041 | 0.054 |
p < 0.05,
p < 0.01.
Regarding clinical validity, the mean scores of each domain were compared between patients who experienced weight loss of 10% or more after surgery and those who did not. Patients with weight loss of 10% or more had significantly lower scores in most domains, indicating that the questionnaire most likely appropriately capture the decreased QoL experienced by these patients (Table 4). Similar results were observed in patients who received total gastrectomy compared with those who received subtotal gastrectomy. Domains related to gastrointestinal symptoms did not differ significantly for patients who received open surgery and those who received laparoscopic/robotic surgery. Only worry about cancer and financial problems had higher scores and scar problems had lower scores in the laparoscopic/robotic group compared with the open group. Moreover, patients diagnosed with stage II or higher gastric cancer had higher scores for constipation and lower scores for worry about cancer and financial problems compared with those diagnosed with stage I gastric cancer. There were no significant differences in the other domains between groups (data not shown).
Table 4.
Difference in KOQUSS-40 scores by clinical characteristics
| Domains | Weight loss after gastrectomy | Extent of gastrectomy | Surgical approach | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Weight loss of less than 10% (n=277) | Weight loss of 10% or more (n=136) | p-value | Partial gastrectomy (n=332) | Total gastrectomy (n=81) | p-value | Laparoscopic /Robotic (n=292) | Open (n=121) | p-value | |
| Indigestion | 72.3±19.9 | 62.2±21.7 | < 0.001 | 70.6±20.6 | 62.3±21.9 | 0.002 | 69.4±21.5 | 68.0±20.0 | 0.530 |
|
| |||||||||
| Dysphagia | 89.9±15.2 | 80.3±20.7 | < 0.001 | 90.1±14.4 | 73.1±23.1 | < 0.001 | 87.4±17.5 | 85.3±18.4 | 0.284 |
|
| |||||||||
| Reflux | 88.8±16.0 | 82.6±20.4 | 0.002 | 87.9±17.1 | 81.9±19.8 | 0.006 | 86.5±18.7 | 87.2±15.6 | 0.693 |
|
| |||||||||
| Dumping syndrome | 89.1±11.6 | 84.1±15.7 | 0.001 | 88.8±12.2 | 82.0±15.9 | 0.001 | 87.7±13.5 | 86.9±12.9 | 0.575 |
|
| |||||||||
| Bowel habit change | 80.2±16.1 | 77.4±17.4 | 0.105 | 80.2±16.0 | 75.6±18.4 | 0.024 | 79.8±16.1 | 78.1±17.6 | 0.360 |
|
| |||||||||
| Constipation | 88.6±18.2 | 86.6±17.5 | 0.307 | 88.0±17.9 | 87.9±18.4 | 0.967 | 87.0±19.2 | 90.1±14.5 | 0.081 |
|
| |||||||||
| Psychological factors | 83.9±15.8 | 76.4±19.9 | < 0.001 | 82.3±17.1 | 77.8±19.0 | 0.036 | 81.8±17.2 | 80.6±18.5 | 0.510 |
|
| |||||||||
| Worry about cancer | 79.1±17.2 | 69.9±23.1 | < 0.001 | 78.0±17.8 | 67.9±24.9 | 0.001 | 77.7±19.0 | 71.9±21.1 | 0.006 |
|
| |||||||||
| General health | 82.6±16.6 | 76.6±20.0 | 0.003 | 82.1±17.2 | 74.8±19.6 | 0.001 | 81.0±18.0 | 79.5±18.0 | 0.444 |
|
| |||||||||
| Scar problems | 91.9±12.2 | 87.8±14.4 | 0.005 | 91.1±12.5 | 88.6±15.0 | 0.160 | 92.4±11.2 | 86.3±16.0 | < 0.001 |
|
| |||||||||
| Financial problems | 87.8±15.0 | 84.6±17.2 | 0.047 | 87.6±15.2 | 83.7±17.6 | 0.043 | 88.2±15.3 | 83.3±16.7 | 0.005 |
|
| |||||||||
| Total | 84.0±10.2 | 77.4±13.5 | < 0.001 | 83.2±10.7 | 76.1±14.0 | < 0.001 | 82.2±11.9 | 81.0±11.5 | 0.362 |
Values are presented as mean±standard deviation.
The instrument had acceptable internal consistency, with the Cronbach’s alpha for each factor in the range 0.576 to 0.868 (Table 5). In the test-retest analysis, the Spearman’s correlation coefficient between the two time points was 0.819 (p < 0.001).
Table 5.
Internal consistency of questionnaire domains
| Gastrectomy symptom domains | No. of items | Cronbach’s alpha |
|---|---|---|
| Indigestion | 6 | 0.854 |
| Dysphagia | 3 | 0.729 |
| Reflux | 3 | 0.780 |
| Dumping syndrome | 5 | 0.755 |
| Bowel habit change | 5 | 0.741 |
| Constipation | 2 | 0.749 |
| Psychological factors | 5 | 0.822 |
| Worry about cancer | 3 | 0.576 |
Discussion
This study was undertaken by the KOQUSS group to address the need to assess postgastrectomy symptoms and QoL appropriately in clinical studies. In this study, we presented the development and validation of the KOQUSS-40, a symptom-focused questionnaire for patients with gastric cancer who have received gastrectomy. The KOQUSS-40 in its final form resulted in a 40-item questionnaire consisting of 11 domains.
The most important characteristic of the KOQUSS-40 is its focus on the assessment of symptoms after gastric cancer surgery. Conventional gastric cancer-specific questionnaires, such as the EORTC QLQ-STO22 and FACT-Ga, measure general gastrointestinal symptoms instead of postgastrectomy syndrome [3,4]. These instruments were also developed for use in inoperable tumor, as well as those who received chemotherapy or radiotherapy as their primary therapy. Notably, these questionnaires do not assess symptoms that result from surgery for gastric cancer, including dumping syndrome, which is the most common symptom after gastrectomy. The KOQUSS-40 questionnaire consists of six items that address indigestion and five items that address dumping syndrome; these two domains represent the most frequent symptoms of patients who have received gastrectomy.
Recently, a Japanese study group developed the PGSAS-45 for patients after gastrectomy [9]. This questionnaire is a combination of preexisting QoL questionnaires, such as the Short Form-8 Health and the Gastrointestinal Symptom Rating Scale, and as well as the newly designed postgastrectomy syndrome-specific items. An advantage of the PGSAS-45 is that it includes a broad range of gastrointestinal symptoms, including postgastrectomy syndrome. However, PGSAS-45 is exclusively available in Japanese and has not been validated for different cultural groups. Studies using the PGSAS-45 have demonstrated differences in QoL according to the extent of gastrectomy and function preservation; however, all these studies were conducted exclusively in Japanese institutions, with Japanese patients [22–24].
A notable characteristic of the KOQUSS-40 questionnaire is its inclusion of items that clinicians have observed to be important to their patients, beyond that of postgastrectomy symptoms alone. These eight items assess general health (item nos. 1, 2, and 3), scar problems (item nos. 4, 38, and 39), and financial problems (item nos. 5 and 40). In particular, items that assess scar and financial problems are potentially helpful for examining whether QoL is improved with minimally invasive surgery. Clinical trials are currently underway to examine the utility of minimally invasive techniques for the treatment of gastric cancer. A QoL assessment tool that can capture potential benefits of minimally invasive surgery is important to assess QoL properly in trials that examine open vs. minimally invasive surgical techniques. One previous study unexpectedly reported worse QoL in patients who received laparoscopic surgery compared with those who received open surgery, and this was felt to be the result of the QoL measure being unable to capture appropriately the benefits of minimally invasive surgery [5,25]. Similarly, in a different study, no significant difference in QoL between totally laparoscopic surgery and laparoscopy-assisted surgery was found [26]. The KOQUSS questionnaire measures satisfaction with scarring and the level of financial difficulty experienced by the patient, which has potential to detect the advantages and disadvantages of a minimally invasive approach. In our clinical validation, satisfaction with the scar was significantly higher in the laparoscopic/robotic group. However, this group had lower QoL in terms of worry about cancer and financial problems compared with the open group.
A summary scoring system was developed for the KOQUSS-40 questionnaire. In conventional instruments, QoL has been assessed as a separate score for each domain, and the overall superiority of different surgical methods regarding QoL could not be determined [5,7]. Recently, a summary scoring system for the EORTC QLQ-C30 was introduced, and this was found to be better at discriminating between groups known to be clinically different compared with the conventional method [17,27]. The KOQUSS-40 was developed to allow for the examination of single domains as well as the summary scores, and is useful for evaluating both each symptom and overall symptoms (summary score) in clinical trials.
Some limitations of this study are as follows. The KOQ-USS-40 questionnaire was developed in the Korean language and has not been validated in other cultural contexts. Therefore, cross-cultural adaptation studies in other countries are necessary. Second, most patients included in this study received gastrectomy for stage I gastric cancer and had relatively favorable prognoses. Symptoms related to advanced disease or other treatment, such as chemotherapy and radiotherapy, were not included in the KOQUSS-40.
In conclusion, the KOQUSS-40 questionnaire was developed to assess QoL among patients who have received gastrectomy for gastric cancer. The KOQUSS-40 questionnaire is an effective instrument for assessing the status of patients after gastrectomy and is useful for assessing the effect of surgical techniques on QoL.
Acknowledgments
We deeply appreciate Min Jae Kang (translator) for English translation work. We thank Editage (www.editage.co.kr) for English language editing.
This work was supported by a grant of the National Cancer Center (No.1910242) and Korean Gastric Cancer Association.
Footnotes
Ethical Statement
The study protocol was approved by the institutional review boards of 18 hospitals: National Cancer Center (NCC2017-0211), Asan Medical Center (2017-1269), Keimyung University Dongsan Medical Center (DSMC 2017-10-001), Yeouido St. Mary’s Hospital (SC19QCDI0019), Yonsei University Severance Hospital (2017-2237-001), Seoul Natio-nal University of College of Medicine (1710-050-891), Kyungpook National University Chilgok Hospital (2017-12-005), Gyeongsang National University School of Medicine (GNUH 20017-09-027-001), Samsung Medical Center (SMC 2017-10-047-001), Incheon St. Mary’s Hospital (OC18OCDS0019), Inje University Haeundae Paik Hospital (HP-IRB 2018-03-009-004), Soonchunhyang University Chonan Hospital (SCHCA 2017-12-014-004), National Medical Center (H-1710-083-004), Gyeongsang National University Changwon Hospital (GNUCH 2017-12-010), Seoul National University Bundang Hospital (B-1711/433-401), Hallym University Dongtan Sacred Heart Hospital (2017-09-007-001), Dongnam Institute of Radiological and Medical Sciences (D-1710-007-002), and Ajou University Hospital (MED-OBS-17-401). Informed consent was obtained from all patients included in the study. All of the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions.
Author Contributions
Conceived and designed the analysis: Eom BW, Lee J, Lee IS, Son YG, Kim SG, Kim HI, Kong SH, Kwon OK, Park JH, An JY, Jeong SH, Yoo MW, Suh YS, Park KB, Ahn SH, Jee YS, Ahn HS, Lee S, Min JS, Kim A, Hur H, Lee HJ.
Collected the data: Eom BW, Lee IS, Son YG, Ryu KW, Kim SG, Kim HI, Kim YW, Kong SH, An JY, Kim CH, Suh BJ, Yoon HM, Son MW, Park JY, Park JM, Jeong SH, Yoo MW, Song GJ, Yang HK, Suh YS, Park KB, Ahn SH, Shin DW, Min JS, Hur H, Lee HJ.
Contributed data or analysis tools: Eom BW, Lee J, Lee IS, Son YG, Ryu KW, Kim SG, Kim HI, Kim YW, Kong SH, Kwon OK, Park JH, An JY, Kim CH, Suh BJ, Yoon HM, Son MW, Park JY, Park JM, Jeong SH, Yoo MW, Song GJ, Yang HK, Suh YS, Park KB, Ahn SH, Shin DW, Jee YS, Ahn HS, Lee S, Min JS, Kim A, Hur H, Lee HJ.
Performed the analysis: Lee J, Kwon OK, Park JH.
Wrote the paper: Eom BW, Lee J, In H, Lee HJ.
Translation: In H.
Conflicts of Interest
Conflict of interest relevant to this article was not reported.
Electronic Supplementary Material
Supplementary materials are available at Cancer Research and Treatment website (https://www.e-crt.org).
References
- 1.Information Committee of Korean Gastric Cancer Association. Korean Gastric Cancer Association Nationwide Survey on Gastric Cancer in 2014. J Gastric Cancer. 2016;16:131–40. doi: 10.5230/jgc.2016.16.3.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Samm N, Han WH, Yoon HM, Ryu KW, Cho H, Lee S, et al. Prognostic implications of the eighth edition of the union for international cancer control - classification for gastric cancer patients from specialized treatment centers in Germany and Korea: a STOBE-Compliant large-scale cohort study. Medicine (Baltimore) 2020;99:e18922. doi: 10.1097/MD.0000000000018922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sprangers MA, Cull A, Bjordal K, Groenvold M, Aaronson NK The European Organization for Research and Treatment of Cancer. Approach to quality of life assessment: guidelines for developing questionnaire modules. EORTC Study Group on Quality of Life. Qual Life Res. 1993;2:287–95. doi: 10.1007/BF00434800. [DOI] [PubMed] [Google Scholar]
- 4.Eremenco SL, Cashy J, Webster K, Ohashi Y, Locker GY, Pelletier G, et al. FACT-Gastric: a new international measure of QOL in gastric cancer. J Clin Oncol. 2004;22(14 Suppl):8123. [Google Scholar]
- 5.Kim YW, Baik YH, Yun YH, Nam BH, Kim DH, Choi IJ, et al. Improved quality of life outcomes after laparoscopy-assisted distal gastrectomy for early gastric cancer: results of a prospective randomized clinical trial. Ann Surg. 2008;248:721–7. doi: 10.1097/SLA.0b013e318185e62e. [DOI] [PubMed] [Google Scholar]
- 6.Park JY, Kim YW, Ryu KW, Nam BH, Lee YJ, Jeong SH, et al. Assessment of laparoscopic stomach preserving surgery with sentinel basin dissection versus standard gastrectomy with lymphadenectomy in early gastric cancer: a multicenter randomized phase III clinical trial (SENORITA trial) protocol. BMC Cancer. 2016;16:340. doi: 10.1186/s12885-016-2336-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim SM, Cho J, Kang D, Oh SJ, Kim AR, Sohn TS, et al. A randomized controlled trial of vagus nerve-preserving distal gastrectomy versus conventional distal gastrectomy for postoperative quality of life in early stage gastric cancer patients. Ann Surg. 2016;263:1079–84. doi: 10.1097/SLA.0000000000001565. [DOI] [PubMed] [Google Scholar]
- 8.Lee JH, Lee HJ, Choi YS, Kim TH, Huh YJ, Suh YS, et al. Postoperative quality of life after total gastrectomy compared with partial gastrectomy: longitudinal evaluation by European Organization for Research and Treatment of Cancer-OG25 and STO22. J Gastric Cancer. 2016;16:230–9. doi: 10.5230/jgc.2016.16.4.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nakada K, Ikeda M, Takahashi M, Kinami S, Yoshida M, Uenosono Y, et al. Characteristics and clinical relevance of postgastrectomy syndrome assessment scale (PGSAS)-45: newly developed integrated questionnaires for assessment of living status and quality of life in postgastrectomy patients. Gastric Cancer. 2015;18:147–58. doi: 10.1007/s10120-014-0344-4. [DOI] [PubMed] [Google Scholar]
- 10.Brierley JD, Gospodarowicz MK, Wittekind C. TNM classification of malignant tumours. 8th ed. Chichester: Wiley-Blackwell; 2017. [Google Scholar]
- 11.Guideline Committee of the Korean Gastric Cancer Association (KGCA), Development Working Group & Review Panel. Korean practice guideline for gastric cancer 2018: an evidence-based, multi-disciplinary approach. J Gastric Cancer. 2019;19:1–48. doi: 10.5230/jgc.2019.19.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Japanese Gastric Cancer Associaion. Japanese gastric cancer treatment guidelines 2014 (ver. 4) Gastric Cancer. 2017;20:1–19. doi: 10.1007/s10120-016-0622-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ajani JA, Bentrem DJ, Besh S, D’Amico TA, Das P, Denlinger C, et al. Gastric cancer, version 2.2013: featured updates to the NCCN guidelines. J Natl Compr Canc Netw. 2013;11:531–46. doi: 10.6004/jnccn.2013.0070. [DOI] [PubMed] [Google Scholar]
- 14.Hopkins WG. Measures of reliability in sports medicine and science. Sports Med. 2000;30:1–15. doi: 10.2165/00007256-200030010-00001. [DOI] [PubMed] [Google Scholar]
- 15.Streiner DL, Norman GR. Health measurement scales: a practical guide to their development and use. 3rd ed. Oxford; Oxford University Press; 2003. [Google Scholar]
- 16.EORTC Data Center. EORTC QLQ-C30 scoring manual [Inter-net] Brussels: EORTC; c2001. [cited 2020 Dec 28]. Available from: https://www.eortc.org/app/uploads/sites/2/2018/02/SCmanual.pdf. [Google Scholar]
- 17.Giesinger JM, Kieffer JM, Fayers PM, Groenvold M, Petersen MA, Scott NW, et al. Replication and validation of higher order models demonstrated that a summary score for the EORTC QLQ-C30 is robust. J Clin Epidemiol. 2016;69:79–88. doi: 10.1016/j.jclinepi.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 18.Streiner DL, Norman GR. Health measurement scales: a practical guide to their development and use. 2nd ed. Oxford: Oxford Medical Publications; 1995. [Google Scholar]
- 19.Yun YH, Park YS, Lee ES, Bang SM, Heo DS, Park SY, et al. Validation of the Korean version of the EORTC QLQ-C30. Qual Life Res. 2004;13:863–8. doi: 10.1023/B:QURE.0000021692.81214.70. [DOI] [PubMed] [Google Scholar]
- 20.Bae JM, Kim S, Kim YW, Ryu KW, Lee JH, Noh JH, et al. Health-related quality of life among disease-free stomach cancer survivors in Korea. Qual Life Res. 2006;15:1587–96. doi: 10.1007/s11136-006-9000-8. [DOI] [PubMed] [Google Scholar]
- 21.Pompili C, Koller M, Velikova G, Franks K, Absolom K, Callister M, et al. EORTC QLQ-C30 summary score reliably detects changes in QoL three months after anatomic lung resection for Non-Small Cell Lung Cancer (NSCLC) Lung Cancer. 2018;123:149–54. doi: 10.1016/j.lungcan.2018.07.021. [DOI] [PubMed] [Google Scholar]
- 22.Takahashi M, Terashima M, Kawahira H, Nagai E, Uenosono Y, Kinami S, et al. Quality of life after total vs distal gastrectomy with Roux-en-Y reconstruction: use of the Postgastrectomy Syndrome Assessment Scale-45. World J Gastroenterol. 2017;23:2068–76. doi: 10.3748/wjg.v23.i11.2068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fujita J, Takahashi M, Urushihara T, Tanabe K, Kodera Y, Yumiba T, et al. Assessment of postoperative quality of life following pylorus-preserving gastrectomy and Billroth-I distal gastrectomy in gastric cancer patients: results of the nationwide postgastrectomy syndrome assessment study. Gastric Cancer. 2016;19:302–11. doi: 10.1007/s10120-015-0460-9. [DOI] [PubMed] [Google Scholar]
- 24.Nishigori T, Okabe H, Tsunoda S, Shinohara H, Obama K, Hosogi H, et al. Superiority of laparoscopic proximal gastrectomy with hand-sewn esophagogastrostomy over total gastrectomy in improving postoperative body weight loss and quality of life. Surg Endosc. 2017;31:3664–72. doi: 10.1007/s00464-016-5403-y. [DOI] [PubMed] [Google Scholar]
- 25.Lee SS, Ryu SW, Kim IH, Sohn SS. Quality of life beyond the early postoperative period after laparoscopy-assisted distal gastrectomy: the level of patient expectation as the essence of quality of life. Gastric Cancer. 2012;15:299–304. doi: 10.1007/s10120-011-0113-6. [DOI] [PubMed] [Google Scholar]
- 26.Woo J, Lee JH, Shim KN, Jung HK, Lee HM, Lee HK. Does the difference of invasiveness between totally laparoscopic distal gastrectomy and laparoscopy-assisted distal gastrectomy lead to a difference in early surgical outcomes? A prospective randomized trial. Ann Surg Oncol. 2015;22:1836–43. doi: 10.1245/s10434-014-4229-x. [DOI] [PubMed] [Google Scholar]
- 27.Hinz A, Einenkel J, Briest S, Stolzenburg JU, Papsdorf K, Singer S. Is it useful to calculate sum scores of the quality of life questionnaire EORTC QLQ-C30? Eur J Cancer Care (Engl) 2012;21:677–83. doi: 10.1111/j.1365-2354.2012.01367.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.