Abstract
Background & Aims:
While abstinence-promoting behavioral and pharmaco-therapies are part of the therapeutic foundation for alcohol use disorder (AUD) and alcohol-associated liver disease (ALD), these therapies, along with alcohol screening and education, are often underutilized. Our aim was to examine provider attitudes and practices for alcohol screening, treatment and education in patients with liver disease.
Methods:
We conducted a survey of primarily (89%) hepatology and gastroenterology providers within (80%) and outside the US (20%). Surveys were sent to 921 providers with 408 complete responses (44%), of whom 343 (80%) work in a tertiary liver transplant center.
Results:
While alcohol screening rates in liver disease patients was nearly universal, less than half of providers reported practicing with integrated addiction providers, using alcohol biomarkers and screening tools. Safe alcohol use by liver disease patients was felt to exist by 40% of providers. While 60% of providers reported referring AUD patients for behavioral therapy, 71% never prescribed AUD pharmacotherapy due to low comfort (84%). Most providers (77%) reported low addiction education and 90% desired more during GI/hepatology fellowship training. Amongst prescribers, baclofen was preferred, but with gaps in pharmacotherapy knowledge. Overall, there was low adherence to the 2019 AASLD practice guidance for ALD, although higher in hepatologists and experienced providers.
Conclusions:
While our survey of hepatology and gastroenterology providers demonstrated higher rates of alcohol screening and referrals for behavioral therapy, we found low rates of prescribing AUD pharmacotherapy due to knowledge gaps from insufficient education. Further studies are needed to assess interventions to improve provider alignment with best practices for treating patients with AUD and ALD.
Keywords: alcohol use disorder, alcohol-associated liver disease, alcohol pharmacotherapy, addiction medicine, alcohol survey
Introduction
The prevalence of alcohol use disorder (AUD) and alcohol-associated liver disease (ALD) are on the rise in the United States.1,2 Since patients with ALD are initially seen at more advanced stages of liver disease compared to others like hepatitis C, it follows that ALD accounted for >50% of cirrhosis-related healthcare costs in a privately insured US cohort.3,4 Alcohol is responsible for half of all cirrhosis-related deaths in the US and ALD is now the leading indication for liver transplantation (LT) in the US.5,6
While early detection of hazardous drinking and AUD are critical to reversing these trends, routine screening for alcohol misuse is often lacking by busy front-line healthcare providers despite decades of societal recommendations.7,8 Low provider confidence in clinical skills due to limited addiction education is also a barrier to providing appropriate alcohol-related care.9 Effective treatment of AUD and ALD requires a multidisciplinary approach, often involving specialists in addiction/psychiatry, gastroenterology (GI)/hepatology and social work, which may not be readily available.10
Abstinence-promoting behavioral and pharmaco-therapies are part of the long-standing therapeutic foundation for AUD and ALD. However, these therapies are often underutilized with a potential negative impact on survival.11 Despite AUD treatment being a quality measure in patients with liver disease, little is known about the clinical approaches of providers who deliver this care, particularly specialists in GI and hepatology.12 Our aim was to examine provider attitudes and practices for alcohol screening, treatment and education in patients with liver disease.
Methods
Survey Design
A working group from the American Association for the Study of Liver Diseases (AASLD) ALD Special Interest Group (SIG) developed a survey stemming from an online discussion on the AASLD Engage Community platform. The survey was pretested among the study authors, iteratively revised based on feedback to reduce response errors or question problems prior to distribution to study participants. (Supplemental Material)
Survey questions were organized into five sections according to a conceptual model for provider decision-making, including provider demographics, provider practices, cognitive factors, behavioral factors, and a knowledge assessment:13 (Supplemental Figure 1)
Demographics (10 questions): gender, race/ethnicity, clinical experience, provider type, practice type, and location.
Provider practices (10 questions): provider practices regarding screening for alcohol use, safe alcohol use, monitoring alcohol use with biomarkers, and integration of addiction providers in clinic.
Cognitive factors (3 questions): previous addiction education and its perceived value, and sources of information on AUD treatment guidelines.
Behavioral factors (12 questions): provider comfort, practices, and barriers to prescribing of AUD pharmacotherapy, behavioral therapy, and referral to addiction providers.
Knowledge assessment (2 questions): knowledge of AUD pharmacotherapy approved for use by the Food and Drug Administration (FDA).
Participants
The survey was conducted among primarily hepatology and GI providers practicing in private outpatient offices, safety-net hospitals, community-based hospitals, Veterans Affairs (VA) hospitals, and tertiary referral hospitals mostly in the US, but also other countries from every continent except Australia and Antarctica. A survey was sent to ≥1 provider in all 50 states and the District of Columbia, Puerto Rico, and Guam. A designated provider in each contacted state or country distributed the survey to providers at their institution. The total number of distributed surveys were recorded to determine the response rate. Provider email addresses were obtained from study authors, publications, internet searches or AASLD ALD SIG. Eligible providers included hepatology and GI physicians, LT surgeons, GI and transplant hepatology fellows, advanced practice providers (APPs), such as nurse practitioners and physician assistants, and addiction medicine providers. The study was approved by the institutional review board at the University of Michigan.
Survey Information
The survey was distributed to providers between 2/28/2020 and 3/25/2020 using an anonymous, web-based platform (Qualtrics, Provo, UT) and was designed to only allow one survey completion per individual. In an initial email, potential participants were informed of the study purpose, its voluntary nature without incentive and contact information. A reminder email was sent two weeks after the initial email. The survey had a total of 37 questions and took an average of 10 minutes to complete.
Statistical Analysis
Survey responses were reported using descriptive statistics. Item non-responses to specific questions were excluded from analysis. All variables were categorical and chi-squared or Fisher’s exact tests were performed to identify factors associated with provider practices. Statistical significance was defined as a P-value of <0.05. Statistical analysis was performed using Qualtrics analysis software (Qualtrics, Provo, UT).
Results
Provider and institutional characteristics
Out of 921 surveys sent, 430 were partially completed and 408 were completed, representing a 44% response rate. Characteristics of responding providers and their practice settings are summarized in Table 1. Nearly all (90%) providers were physicians and physician trainees; mostly hepatologists and gastroenterologists, representing 51% and 39% of the survey total, respectively. APPs (9%) and other provider types (1%) including addiction medicine specialists, psychiatrists, psychologists, social workers, and transplant surgeons composed the remainder. About half of the responding providers were men (57%), non-Hispanic white (49%) and practicing for ≤5 years (50%). Most (80%) reported practicing at an urban, tertiary referral hospital affiliated with a LT center in the US; a total of 33 states were represented. (Supplemental Figure 2) South American and Canadian providers (11% and 6%, respectively) and a small minority (3%) from Europe, Asia, Africa and the Middle East composed the remainder of the survey respondents. Most providers (59%) reported spending >75% of their time in clinical care, with >80% seeing ALD patients on a weekly basis.
Table 1.
Provider and Institutional Characteristics (n = 430)
| Total (N, %) | |
|---|---|
| Number of providers | 430 |
| Gender | |
| Male | 245 (57.0%) |
| Female | 176 (40.9%) |
| Non-binary | 3 (0.7%) |
| Prefer not to disclose | 6 (1.4%) |
| Ethnicity | |
| Non-Hispanic White | 212 (49.3%) |
| Asian/Pacific Islander | 113 (26.3%) |
| Hispanic | 50 (11.6%) |
| Black | 13 (3.0%) |
| Other | 27 (6.3%) |
| Prefer not to disclose | 15 (3.5%) |
| Clinician type | |
| Physician | 290 (67.4%) |
| Physician Trainee | 97 (22.6%) |
| Advanced Practice Providers | 38 (8.8%) |
| Other | 5 (1.2%) |
| Specialty | |
| Hepatology | 218 (50.7%) |
| Gastroenterology | 163 (37.9%) |
| Other | 49 (11.4%) |
| Years in clinical practice | |
| 0–5 years | 214 (49.8%) |
| 6–10 years | 78 (18.1%) |
| 11–15 years | 43 (10.0%) |
| 16–20 years | 32 (7.4%) |
| >20 years | 63 (14.7%) |
| Time spent on clinical care | |
| 0–25% | 29 (6.7%) |
| 26–50% | 36 (8.4%) |
| 51–75% | 110 (25.6%) |
| 76–100% | 255 (59.3%) |
| Primary practice location | |
| United States | 345 (80.2%) |
| North America (non-United States) | 27 (6.3%) |
| South America | 46 (10.7%) |
| Europe | 4 (0.9%) |
| Asia | 4 (0.9%) |
| Africa | 2 (0.5%) |
| Middle East | 2 (0.5%) |
| Institution type | |
| Tertiary referral hospital with LT center | 343 (79.8%) |
| Tertiary referral hospital without LT center | 49 (11.4%) |
| Veterans Affairs hospital | 17 (4.0%) |
| Community-based hospital | 12 (2.8%) |
| Safety-net hospital | 1 (0.2%) |
| Private practice | 8 (1.9%) |
| Practice setting | |
| Urban | 371 (86.3%) |
| Suburban | 50 (11.6%) |
| Rural | 9 (2.1%) |
| Integrated addiction provider in clinic | 134 (31.0%) |
LT, liver transplantation
Provider attitudes and practices regarding alcohol screening
Survey results of provider attitudes and practices for alcohol screening, treatment and education in patients with liver disease are reported in Table 2. During an initial visit with a liver disease patient, nearly all providers reported routine screening for alcohol use (94%), alcohol use frequency (91%), amount used (81%) and felt comfortable asking (93%). There were higher rates of questioning by providers spending >50% on clinical care compared to <50% (96% vs 85%, P= .004), but no significant differences between hepatologists and non-hepatologists (P >.05). The most common barriers to universal alcohol use screening reported were lack of time (61%), insufficient resources available to address alcohol use (60%) and focus on chief complaint (55%). Less than one-quarter of providers “usually” or “always” administer a screening tool to evaluate for hazardous drinking such as the Alcohol Use Disorders Identification Test-Concise (AUDIT-C), Single Alcohol Screening Question (SASQ) or CAGE questionnaire. While there was no difference between hepatologists and non-hepatologists (28% v 17%, P= .08), a significant difference between years of experience and use (“usually” or “always”) of an alcohol screening tool was seen: 17% of providers with 0–5 years of experience compared to 33% with >10 years of experience, respectively; P= .008. (Supplemental Table 1)
Table 2.
Provider Attitudes and Practices for Alcohol Screening, Treatment and Education in Patients with Liver Disease (n = 420)
| Provider question | Data |
|---|---|
| How often do you ask about alcohol use to a new patient with liver disease? | |
| Never/rarely | 0 |
| Sometimes | 3 (0.7%) |
| Usually | 21 (5.0%) |
| Always | 396 (94.3%) |
| How often you ask about frequency of alcohol use? | |
| Never/rarely | 1 (0.2%) |
| Sometimes | 3 (0.7%) |
| Usually | 32 (7.6%) |
| Always | 384 (92.4%) |
| How often do you ask about quantity of alcohol use? | |
| Never/rarely | 2 (0.5%) |
| Sometimes | 15 (3.6%) |
| Usually | 62 (14.8%) |
| Always | 341 (81.2%) |
| How often do you use a brief screening tool in a new patient with liver disease?* | |
| Never/rarely | 198 (47.1%) |
| Sometimes | 129 (30.7%) |
| Usually | 56 (14.8%) |
| Always | 37 (8.8%) |
| How often do you monitor alcohol use with biomarkers? | |
| Never/rarely | 121 (28.8%) |
| Sometimes | 131 (31.2%) |
| Usually | 113 (26.9%) |
| Always | 55 (13.1%) |
| How often do you personally prescribe AUD pharmacotherapy? | |
| Never/rarely | 288 (70.6%) |
| Sometimes | 93 (22.8%) |
| Usually | 16 (3.9%) |
| Always | 11 (2.7%) |
| How comfortable are you prescribing AUD pharmacotherapy?+ | |
| Not comfortable | 227 (55.6%) |
| Somewhat comfortable | 115 (28.2%) |
| Comfortable | 42 (10.3%) |
| Very comfortable | 24 (5.9%) |
| What proportion of your AUD patients are taking any AUD pharmacotherapy? (on- or off-label)+ | |
| 0–25 | 353 (86.5%) |
| 26–50 | 42 (10.3%) |
| 51–75 | 9 (2.2%) |
| 76–100 | 4 (1.0%) |
| Provider education in addiction medicine+ | |
| None | 105 (25.7%) |
| <1 month | 209 (51.2%) |
| 1–3 month | 39 (9.6%) |
| >3 month | 20 (4.9%) |
| Other/unknown | 35 (8.6%) |
AUD, alcohol use disorder
Such as the Alcohol Use Disorders Identification Test—Concise, the Single Alcohol Screening Question, or the CAGE questionnaire
n = 408
About 40% of providers believed in a safe amount of alcohol use (other than total abstinence) in patients with any liver disease, which increased to 72% among physician trainees. Hepatologists and providers spending <50% in clinical care were more likely to believe in safe alcohol use than non-hepatologists and providers spending >50% in clinical care (47% and 57% vs 35% and 38%, P= .009 and .005, respectively). Alcohol biomarkers such as urine ethyl glucuronide (EtG) or blood phosphatidylethanol (PEth) were “usually” or “always” used to monitor abstinence in patients with AUD and ALD by 40% of providers. While there were no differences based on years of experience, hepatologists were more likely than non-hepatologists to report using alcohol biomarkers (52% vs 30%, P< .001). Similar associations of alcohol biomarker use were seen in community hospitals and tertiary referral hospitals with a LT center compared to other practice settings: 46% vs 16%, P< .001. One-third of providers reported having ≥1 integrated addiction provider embedded within their clinic, with most identified as psychiatrists or social workers. Hepatologists were more likely to report practicing in integrated clinics than non-hepatologists (37% vs 27%, P= .03). Providers in these integrated clinics reported lower rates of barriers to universal alcohol use screening. (Supplemental Figure 3) Reported alcohol biomarker usage did not differ between clinics with and without an integrated addiction provider, P= .39.
Provider attitudes about addiction education
Over three-quarters of providers reported having <1 month of addiction education during their healthcare schooling and training, including one-quarter who reported none. Hepatologists were more likely to report no addiction education than non-hepatologists (36% vs 17%, P <.001). Nearly all providers, regardless of provider type or experience, believed that GI/hepatology fellowships should include addiction education. The most common information sources on AUD treatment reported by providers were GI/hepatology society guidelines (76%), UpToDate and other medical websites (62%), and colleagues (44%).
Provider attitudes and practices regarding pharmacotherapy for alcohol use disorder
Nearly all providers (87%) reported that less than one-quarter of their AUD patients are receiving AUD pharmacotherapy, on- or off-label. No differences were seen between hepatologists and non-hepatologists (88% vs 85%, P= .19). Most providers felt “uncomfortable” (56%) or “somewhat comfortable” (28%) with prescribing AUD pharmacotherapy, regardless of practice setting, P= .06. This was consistent with a significant majority (71%) reporting never having personally prescribed AUD pharmacotherapy. Trainees were especially unlikely to prescribe AUD pharmacotherapy: 69% felt “uncomfortable” and none “usually” or “always” prescribe. Hepatologists were more likely than non-hepatologists to report any prescribing of AUD pharmacotherapy (35% vs 25%, P= .005). Providers reporting <1 month of addiction education felt more uncomfortable (60%) prescribing than those reporting >1 month (30%), P< 0.001. Hepatologists and providers with >10 years of experience felt more comfortable prescribing compared to non-hepatologists and providers with 0–5 years of experience (22% and 27% vs 12% and 9%, P= .007 and P= .001, respectively).
A significant proportion of providers reported not ever prescribing AUD pharmacotherapy to non-cirrhotic patients with liver disease (43%), patients with cirrhosis (53%) and LT recipients (70%). (Figure 1) Prescribing providers favored baclofen in all three clinical scenarios, followed by naltrexone then acamprosate in patients with non-cirrhotic liver disease, and gabapentin then acamprosate in patients with cirrhosis and after LT. Providers with >10 years of experience were more likely to prescribe routinely than those with <10 years, although still at low rates (12% vs 4%, P= .005). Pharmacotherapy side-effects (18%), patient motivation (14%), and co-morbid psychiatric conditions (12%) were the top considerations when prescribing AUD pharmacotherapy in patients with ALD. (Figure 2) The most commonly cited barriers to prescribing were lack of training and unfamiliarity with prescribing (30%), preference for others to manage (20%) and pharmacotherapy side-effects (18%). (Figure 3)
Figure 1.
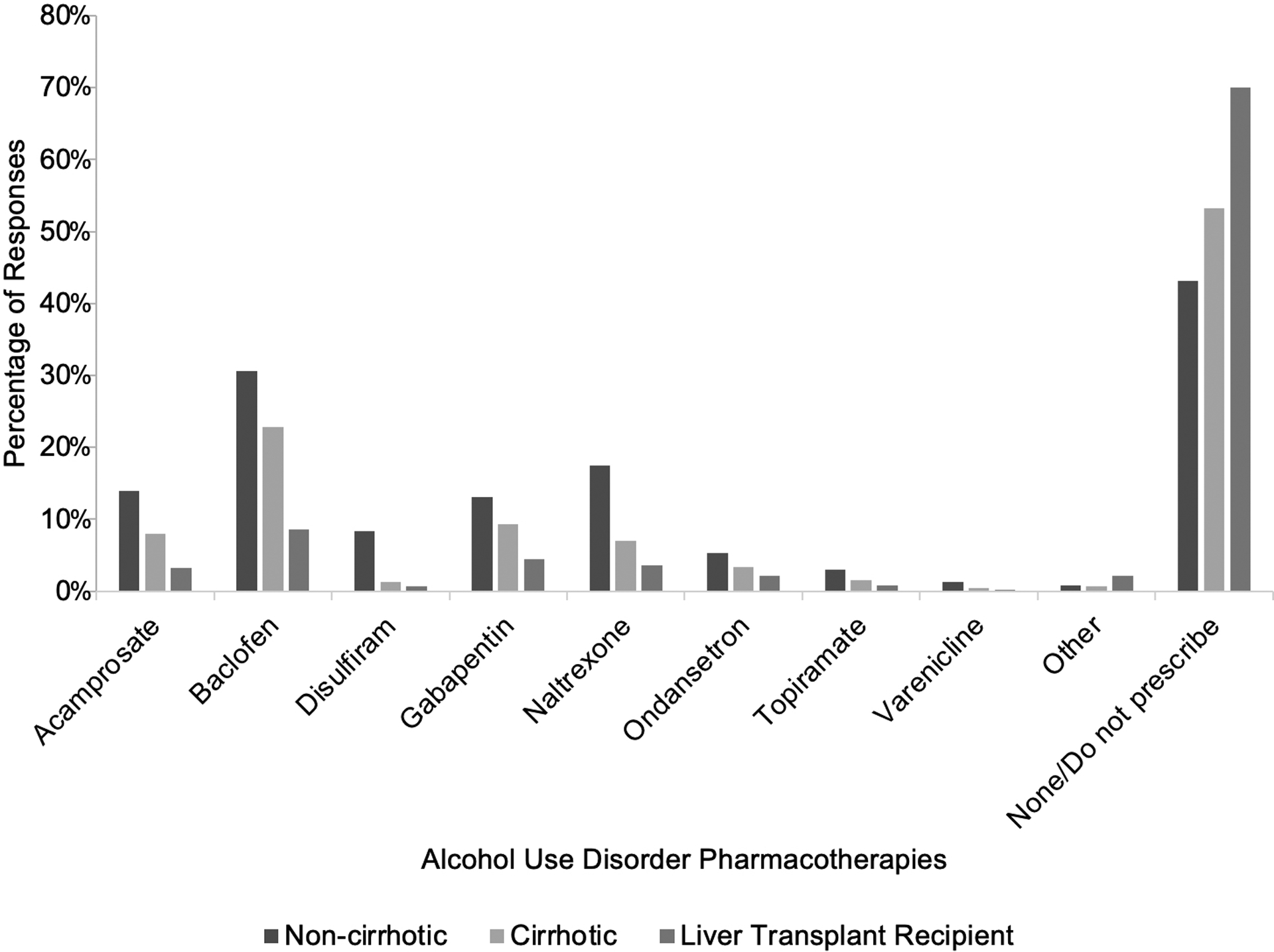
Alcohol Use Disorder Pharmacotherapy Prescribing Patterns Based on Liver Disease Stage
Figure 2.
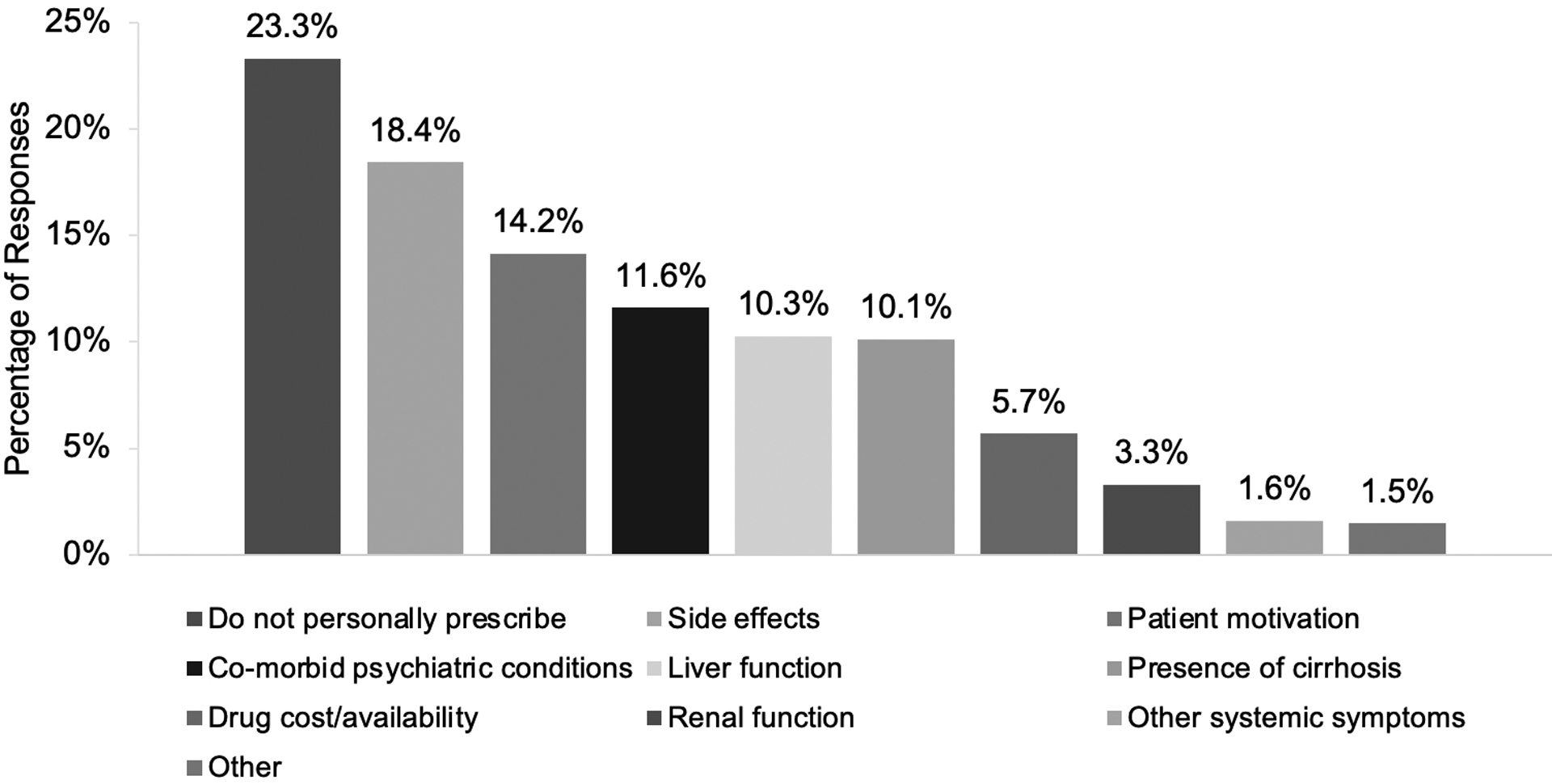
Provider Considerations when Prescribing Alcohol Use Disorder Pharmacotherapy in Patients with Alcohol-associated Liver Disease
Figure 3.
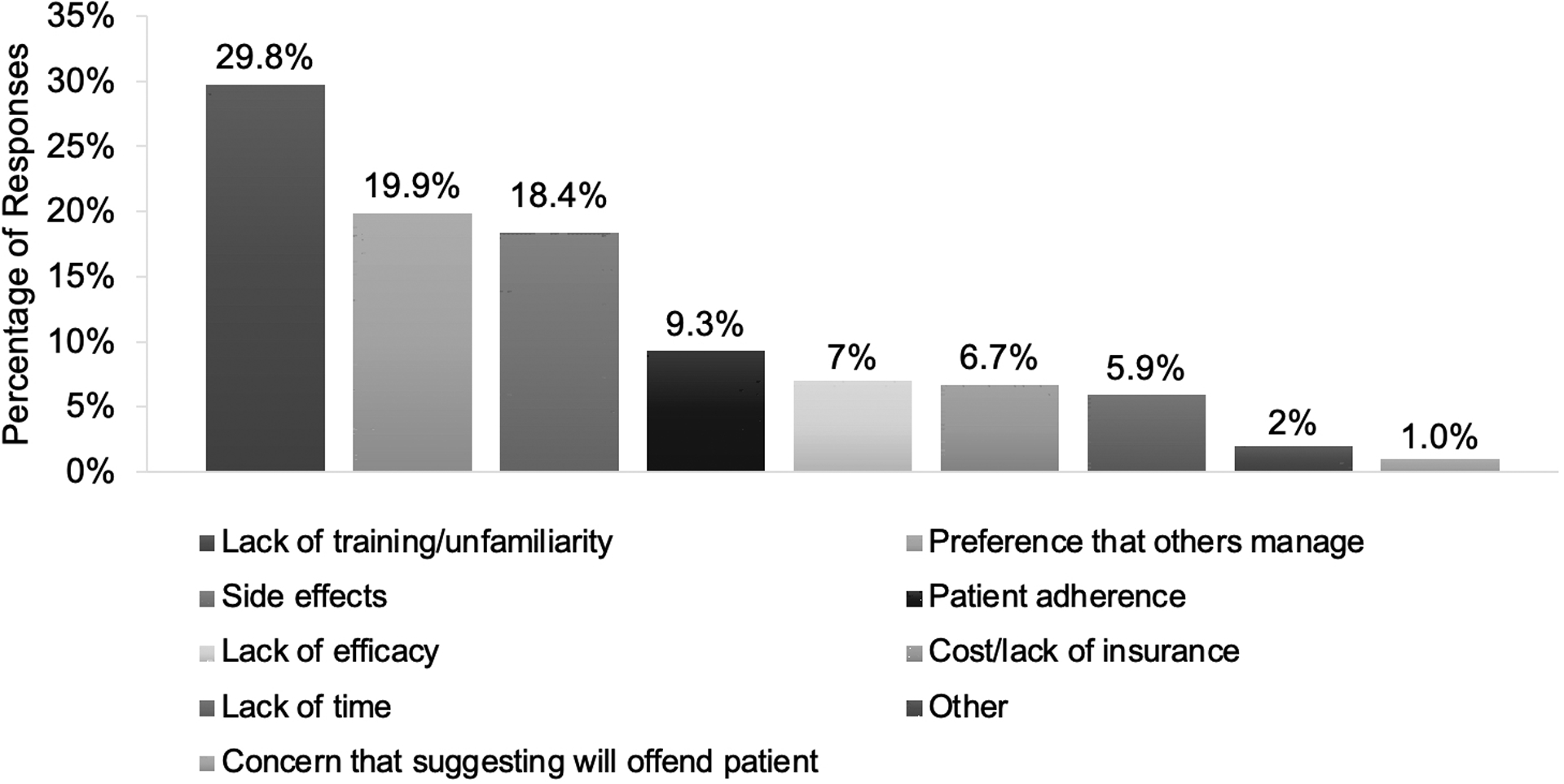
Provider Barriers to Personally Prescribing Alcohol Use Disorder Pharmacotherapy
Provider attitudes and practices regarding behavioral therapy
For patients with AUD, 60% of providers reported “usually” or “always” referring to an addiction provider, with hepatologists and providers with >10 years of experience more likely to refer than non-hepatologists and providers with <10 years (72% and 69% vs 51% and 57%, P< .001 and P= .02, respectively). For AUD patients requiring behavioral therapy, the most common “next-step” referrals were to outpatient alcohol rehabilitation, social worker, then addiction specialist. The most commonly cited barriers for AUD patients to undergo behavioral therapy were felt to be patient reluctance (25%), lack of insurance coverage (19%), cost (16%), and distance to care (15%).
Knowledge assessment of AUD pharmacotherapy
Disulfiram, acamprosate, and naltrexone as the 3 FDA approved AUD pharmacotherapies were correctly identified by 52%, 50% and 48% of providers, respectively. (Supplemental Figure 4) Only 17% of US providers (25% of non-US) correctly answered that there are no FDA approved AUD pharmacotherapies in patients with cirrhosis. (Supplemental Figure 5) There were no differences in knowledge assessment results based on time spent on clinical care, years of experience or hepatologist status. More than half (53%) of all providers reported being unsure about FDA approved AUD pharmacotherapies in this special population.
Adherence to the 2019 AASLD ALD Practice Guidance
There were low rates of provider-reported adherence to the 2019 AASLD practice guidance for ALD regarding alcohol screening, counseling and treatment.14 (Table 3) Hepatologists were more likely than non-hepatologists to prescribe behavioral and pharmaco-therapies, use alcohol biomarkers, have leniency about alcohol use in patients liver disease, and practice with integrated addiction providers, but had similar rates of alcohol screening, use of screening questionnaires and knowledge of AUD pharmacotherapy.
Table 3.
Provider Reported Adherence to 2019 AASLD Alcohol-Associated Liver Disease Practice Guidance
| Guidance statement | Provider Reported Adherence (“Usually” or “Always”) |
|---|---|
| All patients receiving care in primary care and GI/hepatology outpatient clinics, ED, and inpatient admissions should be screened routinely for alcohol use using validated questionnaires. | 22% |
| Alcohol biomarkers can be used to aid in diagnosis and support recovery. Urine and hair EtG, urine EtS, and PEth are not affected by liver disease, and therefore are preferable. | 40% |
| Referral to AUD treatment professionals is recommended for patients with advanced ALD and/or AUD, to ensure access to the full range of AUD treatment options. | 61% |
| Patients with ALD or other liver diseases, in particular NAFLD, NASH, viral hepatitis, and hemochromatosis, should be counseled that there is no safe level of drinking, and that they should abstain. | 60% |
| Based on limited data, the use of acamprosate or baclofen can be considered for the treatment of AUD in patients with ALD. | 29%* |
AASLD, American Association for the Study of Liver Diseases; ALD, alcohol-associated liver disease; AUD, alcohol use disorder, ED, emergency department; EtG, ethyl glucuronide; EtS, urine ethyl sulfate; GI, gastroenterology; NAFLD, nonalcoholic fatty liver disease; NASH, nonalcoholic steatohepatitis; PEth, phosphatidylethanol.
Combined reported rates of acamprosate and baclofen prescribing in patients with AUD and ALD.
Discussion
To our knowledge, this study represents the first nationally representative survey examining hepatology and GI provider attitudes and practices for alcohol screening, treatment and education in patients with liver disease. While nearly all providers routinely ask about alcohol use in patients with liver disease, a large majority felt uncomfortable treating AUD due to a lack of addiction education as demonstrated by the suboptimal knowledge of AUD pharmacotherapies assessed in this survey. Overall, provider responses to this AASLD ALD SIG survey demonstrated low rates of adherence to the 2019 AASLD ALD practice guidance; particularly for routine use of alcohol biomarkers, validated questionnaires and acamprosate or baclofen prescribing for AUD in patients with ALD. In general, hepatologists and experienced providers (practicing >10 years) reported higher adherence to guidance recommendations.
Although nearly all providers reported feeling comfortable screening for alcohol use, a minority routinely used screening questionnaires, primarily due to time limitations. However, AUDIT-C (3 questions) and SASQ (1 question) usually take seconds, not minutes, to administer and are well-validated tools to identify hazardous drinking. AUDIT-C can increase alcohol use detection by 15% over a history taken by a hepatologist in a post-LT population.15 Furthermore, AUDIT, AUDIT-C and SASQ are recommended for use by the US Preventive Services Task Force for all adults and are included in several quality-reporting and payment programs sponsored by commercial payers and government agencies.8,16 Integrating AUDIT-C or SASQ into the electronic health record may improve utilization and is worthy of future study. Reported insufficient resources may pertain to lacking an integrated addiction provider or deficiencies in provider knowledge, which are both supported in this study.
One-third of providers reported having ≥1 integrated addiction provider embedded within their clinic. While hepatologists practicing in tertiary care settings with a LT center were more likely to report this than non-hepatologists and those in other practice settings, this proportion was higher than expected.17 Although monitoring alcohol use in patients before and after LT is an important activity in a LT center, the reported alcohol biomarkers usage was only 40%; although higher amongst hepatologists, but not associated with having an integrated addiction provider. Test costs and availability may be issues. Studies of urine EtG and blood PEth in patients with liver disease are more recent and may not yet be widely adopted by LT centers.18
Whether there is a safe or healthy amount of alcohol use is controversial, given its variable effects on cardiovascular, metabolic, cancer and liver outcomes.19 Evidence against alcohol use in patients with liver disease, including NASH, is growing and the AASLD ALD practice guidance now recommends abstinence in patients with liver disease. Surprisingly, hepatologists (and trainees) were more likely than non-hepatologists to report a safe amount of alcohol use to exist in patients with liver disease. We suspect that conflicting data and/or question misinterpretation (i.e. safety of very rare alcohol use) may have influenced responses. These results require further study and may suggest the need for improved provider education.
The provider-reported referral rate (60%) of patients with AUD to behavioral therapy had the highest rate of adherence with the AASLD practice guidance. This result is significantly higher than the 13% rate found in a recent VA study of cirrhotic patients with newly diagnosed AUD.12 Similarly, studies of US national data found very low lifetime exposure to AUD treatment.1,20 Greater recognition of the need for multidisciplinary care of AUD in patients with ALD, as reflected in the recent practice guidelines of the AASLD and other GI/hepatology societies may have led to the higher rates of behavioral therapy reported in our study.14,17 Hepatologists and providers in LT centers may include more ‘early adopters’ and have more resources available. The presence of integrated addiction providers in one-third aligns with this speculation.
A significant majority (84%) of providers were less than comfortable prescribing AUD pharmacotherapy, with 71% having never prescribed it due to unfamiliarity and preference for others to prescribe. Since providers reported <25% of their AUD patients are on AUD pharmacotherapy, this suggests that other collaborating providers are not prescribing it either. As such, these results reveal a missed opportunity for care. Providers with less experience, less addiction education and non-hepatologists were less likely to prescribe due to low comfort. The low prescribing rates of AUD pharmacotherapy in patients with liver disease found in our study are consistent with the very low rates (~1%) found in the previously mentioned VA study.11 Patient reluctance was also reported as a barrier to AUD pharmacotherapy prescribing, consistent with prior studies.21 The lack of options and suboptimal efficacy of current AUD pharmacotherapies may also be factors.
Despite its off-label use, baclofen, a γ aminobutyric acid (GABA) B-receptor agonist, was the most commonly prescribed AUD pharmacotherapy in patients with non-cirrhotic liver disease, cirrhosis and after LT. Baclofen is the only AUD pharmacotherapy studied in a randomized controlled trial in patients with cirrhosis, supporting its safety and efficacy.22 AUD pharmacotherapy prescribing was very low for LT recipients, possibly due to concerns about interactions with immunosuppression, hepatotoxicity, or a perceived lower need after LT.23 Prospective trials of FDA-approved AUD pharmacotherapy, particularly acamprosate, in patients with advanced liver disease and after LT are needed.
While provider-reported referral of AUD patients to behavioral therapy had the highest rate of adherence with the AASLD practice guidance, it was not universal. In addition, the knowledge assessment of AUD pharmacotherapy revealed a significant knowledge gap among providers across all experience levels, and a universal desire for improved addiction education during GI/hepatology fellowship training. These results are consistent with recent surveys of US medical schools: <1 hour of addiction education and only 8% with formal addiction curriculum.24,25 Targeted educational efforts are needed to improve comfort and competency levels of providers in AUD treatment such as addiction medicine electives and brief intensive immersion programming.26,27
This survey also revealed “siloing” of AUD educational resource utilization. GI/hepatology society guidelines and UpToDate were commonly used, but high quality resources from the NIAAA and psychiatry/addiction societies were not. Crosstalk between specialists in addiction and GI/hepatology could be encouraged by co-sponsored activities at societal meetings and would promote AUD co-management, resource-sharing and research. Addiction treatment integration could be accomplished by co-locating addiction providers in a multidisciplinary ALD clinic, leveraging telementoring programs, streamlining consults, and incorporating formal addiction education and training.28 Telephone or web-based treatment initiatives that overcome barriers like geographic proximity and the scarcity of local addiction providers are also promising, both in efficacy and cost-effectiveness.29
Strengths of this study include its large sample size, high response rate, national representation and inclusion of APPs and international providers. There are several limitations. First, nearly 80% of surveyed providers practice in US tertiary referral hospitals with LT centers, limiting generalizability, but any contemporary assessment of alcohol use treatment by GI/hepatologists are lacking. Second, survey respondents were generally inexperienced, with half in fellowship training or within 5 years of practice. Our results also carry the risk of a response bias, with responses not accurately reflective of their actual practice. Finally, the survey did not restrict providers from internet searches while taking it, potentially leading to over-estimations of provider knowledge.
In conclusion, provider-reported adherence to the 2019 AASLD ALD practice guidance was low. While our survey of hepatology and gastroenterology providers demonstrated higher rates of alcohol use screening and referrals for behavioral therapy, we found low rates of comfort and prescribing of AUD pharmacotherapy due to knowledge gaps from insufficient education. Further studies are needed to assess interventions to improve provider alignment with best practices for treating patients with AUD and ALD.
Supplementary Material
Acknowledgments:
The study authors acknowledge Kate Boyd for figure design assistance and John Lingerfelt for administrative support of the AASLD ALD SIG.
Financial support:
All study authors have no support or conflicts to report.
Abbreviations:
- AASLD
American Association for the Study of Liver Diseases
- APP
advanced practice providers
- AUD
alcohol use disorder
- ALD
alcohol-associated liver disease
- FDA
Food and Drug Administration
- LT
liver transplantation
- SIG
special interest group
Contributor Information
Gene Y. Im, Icahn School of Medicine at Mount Sinai, Division of Liver Diseases, Recanati/Miller Transplantation Institute, New York, NY.
Jessica L. Mellinger, Division of Gastroenterology and Hepatology, University of Michigan, Ann Arbor, Michigan.
Adam Winters, Vatche and Tamar Manoukian Division of Digestive Diseases, Department of Medicine David Geffen School of Medicine at UCLA Los Angeles, California.
Elizabeth S. Aby, Division of Gastroenterology, Hepatology, and Nutrition, University of Minnesota, Minneapolis, Minnesota
Zurabi Lominadze, Division of Gastroenterology, Department of Medicine, University of Maryland, Baltimore, MD.
John Rice, Division of Gastroenterology and Hepatology, University of Wisconsin School of Medicine, Madison, Wisconsin.
Michael R. Lucey, Division of Gastroenterology and Hepatology, University of Wisconsin School of Medicine, Madison, Wisconsin
Juan P Arab, Departamento de Gastroenterología, Escuela de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile.
Aparna Goel, Division of Gastroenterology and Hepatology, Stanford University School of Medicine, Stanford, California.
Loretta L. Jophlin, Division of Gastroenterology and Hepatology, Department of Medicine, Mayo Clinic, Rochester, Minnesota
Courtney B. Sherman, Division of Gastroenterology and Hepatology, University of California, San Francisco, CA
Richard Parker, Leeds Liver Unit, St. James’s University Hospital, Leeds, United Kingdom.
Po-Hung Chen, Division of Gastroenterology and Hepatology, Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, MD..
Deepika Devuni, Division of Gastroenterology, Department of Medicine, University of Massachusetts Medical School, Worcester, MA.
Sandeep Sidhu, Department of Gastroenterology, Dayanand Medical College and Hospital, Ludhiana, Punjab, India..
Winston Dunn, Department of Internal Medicine, The University of Kansas Medical Center, Kansas City, Kansas.
Gyongyi Szabo, Division of Gastroenterology and Hepatology, Department of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts.
Ashwani K. Singal, Division of Gastroenterology and Hepatology, Department of Medicine, Avera McKennan University Hospital Transplant Institute, University of South Dakota Sanford School of Medicine, Sioux Falls, South Dakota
Vijay H. Shah, Division of Gastroenterology and Hepatology, Department of Medicine, Mayo Clinic, Rochester, Minnesota
References
- 1.Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-Month Alcohol Use, High-Risk Drinking, and DSM-IV Alcohol Use Disorder in the United States, 2001–2002 to 2012–2013: Results From the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry 2017;74:911–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tapper EB, Parikh ND. Mortality due to cirrhosis and liver cancer in the United States, 1999–2016: observational study. BMJ 2018;362:k2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shah ND, Ventura-Cots M, Abraldes JG, et al. Alcohol-Related Liver Disease Is Rarely Detected at Early Stages Compared With Liver Diseases of Other Etiologies Worldwide. Clin Gastroenterol Hepatol 2019;17(11):2320–2329.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mellinger JL, Shedden K, Winder GS, et al. The high burden of alcoholic cirrhosis in privately insured persons in the United States. Hepatology 2018;68:872–882. [DOI] [PubMed] [Google Scholar]
- 5.Rehm J, Samokhvalov AV, Shield KD. Global burden of alcoholic liver diseases. J Hepatol 2013;59:160–168. [DOI] [PubMed] [Google Scholar]
- 6.Cholankeril G, Ahmed A. Alcoholic Liver Disease Replaces Hepatitis C Virus Infection as the Leading Indication for Liver Transplantation in the United States. Clin Gastroenterol Hepatol 2018;16(8):1356–1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.https://www.centeronaddiction.org/addiction-research/reports/national-survey-primary-care-physicians-patients-substance-abuse. Accessed 5/15/2020.
- 8.US Preventive Services Task Force, Curry SJ, Krist AH, Barry MJ, et al. Screening and Behavioral Counseling Interventions to Reduce Unhealthy Alcohol Use in Adolescents and Adults: US Preventive Services Task Force Recommendation Statement. JAMA 2018;320(18):1899–1909. [DOI] [PubMed] [Google Scholar]
- 9.Bazzi A, Saitz R. Screening for Unhealthy Alcohol Use. JAMA 2018;320(18):1869–1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khan A, Tansel A, White DL, et al. Efficacy of Psychosocial Interventions in Inducing and Maintaining Alcohol Abstinence in Patients With Chronic Liver Disease: A Systematic Review. Clin Gastroenterol Hepatol 2016;14:191–202.e194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rogal S, Youk A, Zhang H, et al. Impact of Alcohol Use Disorder Treatment on Clinical Outcomes among Patients with Cirrhosis. Hepatology 2019; 10.1002/hep.31042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kanwal F, Kramer J, Asch SM, et al. An explicit quality indicator set for measurement of quality of care in patients with cirrhosis. Clin Gastroenterol Hepatol 2010;8:709–717. [DOI] [PubMed] [Google Scholar]
- 13.Rich NE, Yang JD, Perumalswami PV, et al. Provider Attitudes and Practice Patterns for Direct-Acting Antiviral Therapy for Patients With Hepatocellular Carcinoma. Clin Gastroenterol Hepatol 2020;18(4):974–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Crabb DW, Im GY, Szabo G, et al. Diagnosis and Treatment of Alcohol-Associated Liver Diseases: 2019 Practice Guidance From the American Association for the Study of Liver Diseases. Hepatology 2020;71:306–333. [DOI] [PubMed] [Google Scholar]
- 15.Donnadieu-Rigole H, Olive L, Nalpas B, et al. Follow-Up of Alcohol Consumption After Liver Transplantation: Interest of an Addiction Team? Alcohol Clin Exp Res 2017;41(1):165–170. [DOI] [PubMed] [Google Scholar]
- 16.Kanwal F, Tapper EB, Ho C, et al. Development of Quality Measures in Cirrhosis by the Practice Metrics Committee of the American Association for the Study of Liver Diseases. Hepatology 2019;69:1787–1797. [DOI] [PubMed] [Google Scholar]
- 17.Donnadieu-Rigole H, Jaubert L, Ursic-Bedoya J, et al. Integration of an Addiction Team in a Liver Transplantation Center. Liver Transpl 2019;25(11):1611–1619. [DOI] [PubMed] [Google Scholar]
- 18.Andresen-Streichert H, Beres Y, Weinmann W, et al. Improved detection of alcohol consumption using the novel marker phosphatidylethanol in the transplant setting: results of a prospective study. Transpl Int 2017;30(6):611–620. [DOI] [PubMed] [Google Scholar]
- 19.GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2018;392(10152):1015–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mellinger JL, Fernandez A, Shedden K, et al. Gender Disparities in Alcohol Use Disorder Treatment Among Privately Insured Patients with Alcohol-Associated Cirrhosis. Alcohol Clin Exp Res 2019;43(2):334–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mellinger JL, Winder GS, DeJonckheere M, et al. Misconceptions, preferences and barriers to alcohol use disorder treatment in alcohol-related cirrhosis. J Subst Abuse Treat 2018;91:20–27. [DOI] [PubMed] [Google Scholar]
- 22.Addolorato G, Leggio L, Ferrulli A, et al. Effectiveness and safety of baclofen for maintenance of alcohol abstinence in alcohol-dependent patients with liver cirrhosis: randomised, double-blind controlled study. Lancet 2007;370:1915–1922. [DOI] [PubMed] [Google Scholar]
- 23.Weinrieb RM, Van Horn DH, McLellan AT, et al. Alcoholism treatment after liver transplantation: lessons learned from a clinical trial that failed. Psychosomatics 2001;42(2):110–116. [DOI] [PubMed] [Google Scholar]
- 24.https://twitter.com/ASAMorg/status/857628307965304833. Accessed 5/19/2020.
- 25.https://www.nytimes.com/2018/09/10/health/addiction-medical-schools-treatment.html. Accessed 5/19/2020.
- 26.Klimas J, Ahamad K, Fairgrieve C, et al. Impact of a brief addiction medicine training experience on knowledge self-assessment among medical learners. Subst Abus 2017;38(2):141–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.https://www.centeronaddiction.org/addiction-research/reports/addiction-medicine-closing-gap-between-science-and-practice. Accessed 5/5/2020.
- 28.Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med 2011;364(23):2199–2207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gustafson DH, McTavish FM, Chih MY, et al. A smartphone application to support recovery from alcoholism: a randomized clinical trial. JAMA Psychiatry 2014;71(5):566–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


