Abstract
Background:
Some alcohol interventions have been found to have the adverse outcome of increasing non-alcohol-related substance use. It is unknown, however, how changes in alcohol use over the course of alcohol ignition interlocks - a common DUI intervention - may impact other substance use.
Methods:
Alcohol and cannabis use were measured using hair ethylglucuronide and Delta-9-Tetrahydrocannabinol concentrations in blood, respectively. Participants (N = 69) were measured at the interlock installation period and again 6-months later while the interlock was installed. A mixed ANOVA was conducted to examine changes in levels of ethanol and THC over time.
Results:
On measures of marijuana use, there was a significant interaction effect between the group that increased alcohol use and time F(2, 66) = 7.863, p =.001; partial η2 =.192; as well as a main effect for time F(2, 66) = 21.106, p <.001; partial η2 =.242.
Conclusions:
Installing interlocks may inadvertently increase cannabis use among those who decrease alcohol use. Crash risk associated with cannabis use is notably less than that of alcohol use, however, continued cannabis use may be problematic when the device is removed and alcohol use is expected to return to the higher pre-interlock levels.
Keywords: Marijuana use, DUI, alcohol misuse, alcohol ignition interlock
Alcohol and cannabis represent two of the most commonly used and misused substances worldwide (Substance Abuse and Mental Health Services Administration [SAMHSA], 2015). Both substances have been found to be significant contributors to automobile crashes individually (Compton & Berning, 2015), and compounded when used simultaneously (Hartman & Huestis, 2013; Wilson et al., 2014). Alcohol ignition interlock devices (IIDs) - when installed on the vehicle of a driver convicted of driving under the influence of alcohol (DUI) are designed to prevent a driver from starting a vehicle if he/she has a breath alcohol level above an established threshold (usually .02 or .03). This has resulted in many states requiring the device or else suspending the offender’s license to drive for a specified period. There is ample evidence showing that IIDs are effective interventions for preventing drinking and driving. The evidence shows that drivers adapt to IIDs on their car and reduce the frequency over time with which they provide positive breath tests indicating that they separate their drinking from their driving. (P. R. Marques et al., 1999; P. Marques et al., 2010; Vanlaar et al., 2017).
Research has also shown that when a preferred substance use pattern is disrupted it is common for the use of other substances to increase in an attempt to replace the physiological rewards being lost, cope with the physical symptoms of withdrawal, or continue to engage in escapism related behaviors (Peters & Hughes, 2010; Reiman, 2009; Sussman & Black, 2008). Indeed, among individuals in treatment for alcohol use disorders, those who engage in polysubstance use during treatment decrease the likelihood of stable abstinence during and post-treatment (Aharonovich et al., 2005; Subbaraman et al., 2017; Subbaramana et al., 2018). Among those who use alcohol, cannabis is the most commonly co-occurring substance (Falk et al., 2008). This is concerning as those who use cannabis while in treatment for alcohol use disorders are about twice as likely as those who do did not use cannabis during treatment to relapse into alcohol-related problems (Weinberger et al., 2016). Prior research has called for further examination of the relationship between cannabis and alcohol use and adverse outcomes (Weinberger et al., 2016).
Though the potential for polysubstance use has been demonstrated in clinical settings, it is less clear if the same relationship exists among drivers with IIDs. Following the paradigm established in the clinical literature, however, it would seem logical that the obstruction of alcohol use by the IID may lead to the use of another substance to replace the physical, psychological and social rewards of alcohol use. As cannabis is the substance most commonly used among alcohol users (Falk et al., 2008) and has been found to be the substance most commonly co-occurring with alcohol among drivers (Scherer, Canham et al., 2018) - it could be hypothesized that drivers on interlock are likely to increase their cannabis use to compensate for any decrease in alcohol use and at the same time, avoid interlock vehicle lockouts that are triggered by consuming even small amounts of alcohol. A unique opportunity to examine this phenomenon exists in drivers who are convicted of driving under the influence (DUI) of alcohol and then required to install an IID (Elder et al., 2011; Willis et al., 2004). While the IID is installed, users reduce the number of positive breath tests that prevent them from starting their cars, suggesting a restriction to their alcohol use (P. R. Marques et al., 1999). However, once removed, gains made while on interlock dissipate and drivers tend to revert to potentially problematic, pre-IID installation alcohol behaviors (Elder et al., 2011; Willis et al., 2004).
Unfortunately, the literature examining changes in substances other than alcohol while a driver has an IID installed on his/her car is notably limited. To address this gap in the literature, the current study examined what - if any - changes occur in patterns of cannabis use while the IID is installed on the car. It stands to reason that if the clinical paradigm can be applied to drivers with interlocks, we would expect to see an increase in cannabis use among those that decrease their alcohol use.
Methods
We performed a secondary analysis of the Managing Heavy Drinking (MHD) study conducted in Erie County, New York. The MHD is a longitudinal study of drivers convicted of a DUI who were court-mandated to install an alcohol ignition interlock device (IID) on their vehicles. Participants were surveyed near the time of IID installation (T1) and six months later (T2). Data collection for the current study began in 2015 and is currently ongoing.
Participants
Participants (N = 69) responded to fliers specifically targeting DUI offenders in Erie County, New York. Recruitment fliers were distributed at impaired driving classes, victim impact panels, alcohol ignition interlock installation centers, substance abuse treatment facilities and health centers. Participants were interviewed by trained research assistants at a research center or in a mobile office, where computer surveys and interviews were completed, and blood and hair samples were collected.
Measures
Demographic data
Participant demographic information included age, sex, race ethnicity, educational attainment, and employment.
Repeat offender status
Participants also offered information on whether they had an alcohol IID installed on a vehicle they owned at any time in the past. When possible, this information was confirmed with the Department of Motor Vehicles.
Alcohol use
Alcohol use was measured using Ethyl Glucuronide (hEtG) in hair samples provided by participants. Participants provided hair samples approximately 3 cm in length at both T1 and T2 which were shipped to a lab for further analysis. EtG, measured in hair, is a widely used biomarker used to assess alcohol use proclivity over the prior 1 to 3 months (Biondi et al., 2019), and has been used previously to examine patterns of alcohol use among drivers convicted of a DUI (P.R. Marques et al., 2014). EtG in the hair samples were measured by tandem mass spectrometry in the laboratory of Dr. Ron Agius in Bad Salzuflen, Germany.
Cannabis use
Blood samples were collected to assess for the presence THC. Blood was collected by trained phlebotomists and sent to a laboratory where screenings were conducted using enzyme-linked immunosorbent assay. Specimens screened positive were confirmed using either gas chromatography with mass spectral detection or liquid chromatography with tandem mass spectral detection.
Data analysis
Data were analyzed using IBM SPSS v.21(IBM Corp. 2012). Descriptive statistics and chi square solutions were calculated for participant demographics. Bivariate correlations were conducted to examine the intercorrelations between independent and dependent variables and to check for multicollinearity. None of the variables exceeded r = .9 and did not violate the assumption of multicollinearity (O’Brien, 2007). Similarly, we examined the Variance Inflation Factor (VIF) when conducting all regression analyses and found that no value exceeded 3.0. Both blood THC levels and hEtG alcohol levels demonstrated a skewed distribution. For the purposes of analysis, data for biological assessment were normalized using log-adjustment. A mixed between-within subjects analysis of variance was utilized to determine the potential impact of participants’ alcohol use patterns as it relates to cannabis use over the two time periods. Participants were trichotomized into three conditions based on their alcohol use patterns from T1 to T2 - those that decreased their alcohol use (i.e, hEtG levels in T2 less than 10% of their T1 hEtG levels); those that maintained their alcohol use behaviors (i.e., hEtG levels ±10% of their T1 hEtG levels); and those that increased their alcohol use (i.e., hEtG levels were greater than 10% higher than T1 levels). Interaction effects between time and THC level were of specific interest.
Results
Participant demographics
Most drivers identified as male (58.7%) with the remainder identifying as female (41.3%). The majority of the drivers identified as White, non-Hispanic (90.2%) and reported being first time DUI offenders (58.1%). The mean age for all participants was approximately 36 years (M = 36.6; SD = 12.18). See Table 1 for demographics broken down by alcohol consumption levels.
Table 1.
Demographic characteristics of study sample.
| Increase Alcohol Use | Retain Alcohol Use | Decrease Alcohol Use | Total | ||
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N | X2 (p-value) | |
| Sex | 1.030 (p =.597) | ||||
| Male | 11 (29.7) | 16 (43.2) | 10 (27.0) | 37 | |
| Female | 9 (34.6) | 8 (30.8) | 9 (34.6) | 26 | |
| Race-ethnic Group | 3.175 (p =.529) | ||||
| White, non-Hispanic | 18 (32.7) | 20 (36.4) | 17 (30.9) | 55 | |
| White, Hispanic | 1 (20.0) | 3 (60.0) | 1 (20.0) | 5 | |
| Black, non-Hispanic | 1 (100.0) | 0 (0.0) | 0 (0.0) | 1 | |
| Repeat offender status | 2.166 (p =.339) | ||||
| First time offender | 10 (27.8) | 13 (36.1) | 13 (36.1) | 36 | |
| Repeat offender | 10 (38.5) | 11 (42.3) | 5 (19.2) | 26 | |
| Mean (SD) | Mean (SD) | Mean (SD) | ANOVA | ||
| F (p-value) | |||||
| Age | 41.89 (11.90) | 38.67 (10.97) | 34.14 (11.81) | 2.223 (p =.117) |
The overall model showed a large main effect for time, Wilks lambda = .758, F(1, 66) = 21.106, p < .001, partial η2 = .242 (see Table 2), reflecting that there were overall increases in log-adjusted marijuana use across time. The main effect comparing the three levels of alcohol consumption was significant, F(2, 66) = 4.665, p = .13, partial η2 = .124, suggesting a difference in cannabis use between levels (see Figure 1). There was a significant interaction between time and alcohol use group Wilks lambda = .808, F(2, 66) = 7.863, p = .001, partial η2 = .192. Those that decreased alcohol use from T1 to T2 had significantly higher levels of blood THC levels than did those in either the Increase Alcohol Use group (p = .004) or in the Retain Alcohol Use group (p = .042). No significant differences were noted between those who retained similar alcohol use patterns at T2 as they did in T1, and those who actually increased their alcohol use in the same time period (p = .317).
Table 2.
Two-way analysis of variance results examining the effects of time and group assignment on log-adjusted THC use.
| Overall Model Fit | ||||
|---|---|---|---|---|
| F | p-value | Partial eta2 | ||
| Time | 21.106 | .000 | .242 | |
| Comparison of Alcohol Use Levels | ||||
| Referent | Comparison | Mean difference | SE | p-value |
| Increase Alcohol Use | Retain Alcohol Use | −.117 | 0.116 | 0.317 |
| Decrease Alcohol Use | −.358 | 0.120 | 0.004 | |
| Retain Alcohol Use | Increase Alcohol Use | .117 | 0.116 | 0.317 |
| Decrease Alcohol Use | −.241 | 0.116 | 0.042 | |
| Decrease Alcohol Use | Increase Alcohol Use | .358 | 0.120 | 0.004 |
| Retain Alcohol Use | .241 | 0.116 | 0.042 | |
Figure 1.
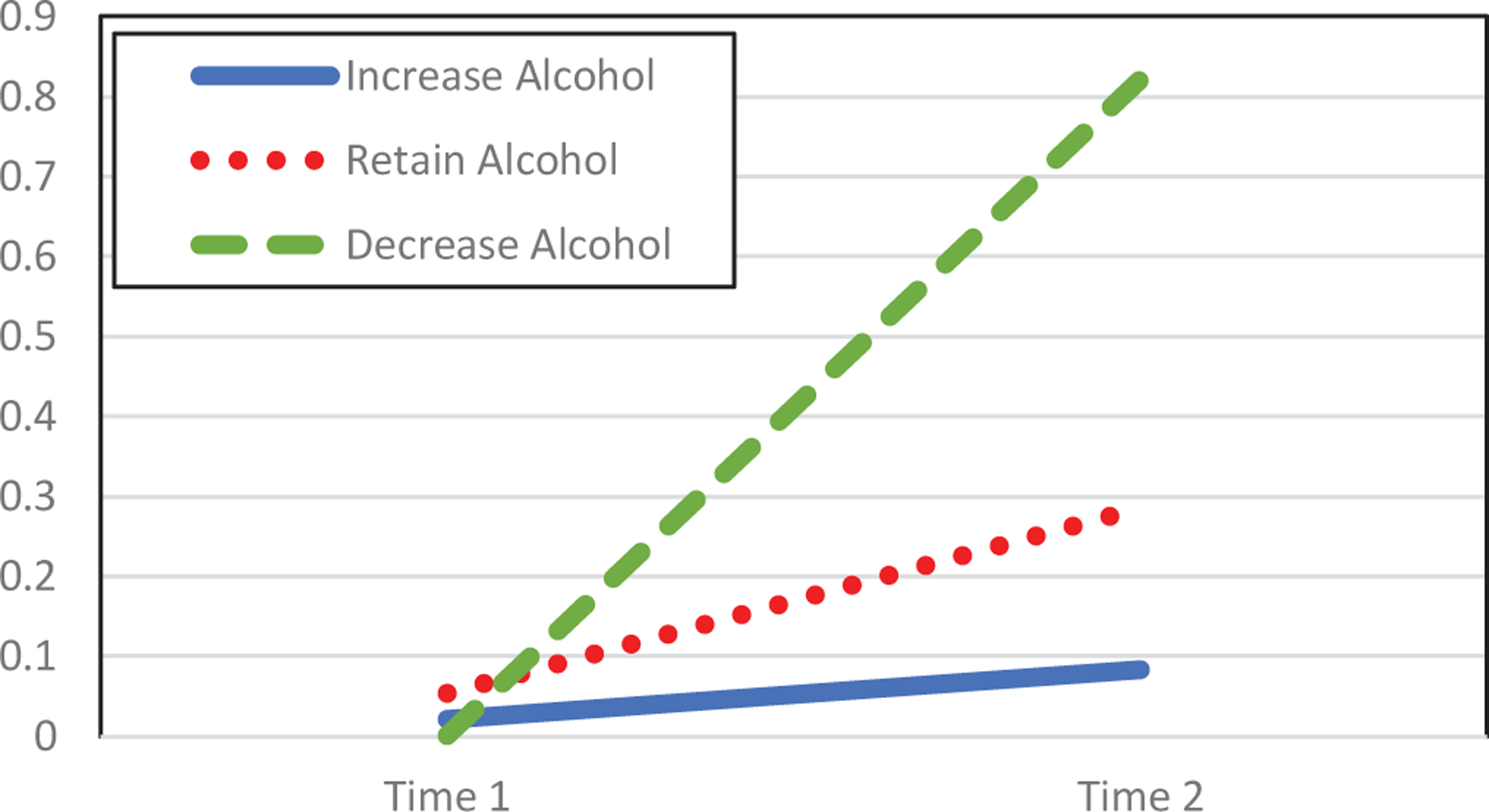
Changes in log-adjusted blood THC by conditions over time.
Discussion
The use of alcohol prior to driving poses a serious public health concern both for the driver and for those that may be involved in a vehicle crash with the driver. To attempt to address this concern, alcohol ignition interlock devices are an intervention designed to prevent drinking and driving (Elder et al., 2011; Willis et al., 2004). Though interlocks have been shown to reduce attempts to start the car with elevated BAC levels (P. Marques et al., 2010; P. R. Marques et al., 1999), when the device is removed, rates of alcohol consumption frequently reverts to levels consistent with those prior to interlock installation (Elder et al., 2011; Voas et al., 1999; Willis et al., 2004).
The impact of alcohol IIDs on other substance use, however, has not been extensively studied. In part, this may be due to the general understanding that alcohol consumption notably increases crash risk when driving a car (Peck et al., 2008; Voas et al., 2012; Zador et al., 2000). In contrast, although there is some evidence that substances like cannabis do increase crash risk relative to non-substance using drivers (Legrand et al., 2013; Rogeberg & Elvik, 2016), the relative risk associated with driving under the influence of cannabis is unclear and somewhat diminished compared to alcohol use (Brubacher et al., 2019; Romano & Pollini, 2013). However, this does not mitigate the need to understand what role a prominent intervention designed to reduce drinking and driving - such as the use of alcohol ignition interlocks - may have on other substance use. Table 2 suggests that though blood THC levels increased across all alcohol use categories, it increased significantly more among those that reduced alcohol use from pre-interlock to 6 months later while on the interlock relative to those that decreased or retained their T1 alcohol use at T2. This finding is consistent with prior literature that finds a similar relationship among participants who are seeking clinical treatment for alcohol use disorders. In those cases, it is common for participants to increase use of another substance to ease the discomfort of decreasing their alcohol use (Peters & Hughes, 2010; Reiman, 2009; Sussman & Black, 2008).
This finding is of note for several reasons. First, it may imply that for some, alcohol ignition interlocks have the unintentional side effect of increasing the likelihood of substituting another substance for alcohol while the device is installed. Such a transition could result in a displacement of risk from drunk driving to drugged driving. Second, the prior literature has established that when the interlock is removed, drivers tend to revert to their alcohol use behaviors prior to installation. This raises a question of the potential for polysubstance use after the IID. That is, if other substance use is increased while on the IID, and is maintained after its removal, while alcohol use increases again, there is the potential for drivers to be at risk of both alcohol and drug use after the IID. These drivers may be at even higher risk for crash involvement than those using either substance independently (Knoche et al., 2012; Legrand et al., 2013; Scherer, Romano et al, 2018).
Questions about the potential for polysubstance use among some IID users following removal of the device, or identification of drivers at risk for substance substitution while on the device were beyond the scope of the current study. Future studies should examine these phenomena to determine what potential impact IIDs have beyond what they demonstrate for alcohol use during and after the device. Future research should also examine if the potential for substance substitution (particularly cannabis) is potentially more pronounced in states where cannabis has been legalized recreationally or medicinally. Finally, as drivers with IIDs are required to remain in steady contract with the interlock installation centers, additional research is also needed to determine what kind of interventions might be created to retain the benefits of IIDs following their removal and/or prevent and monitor other substance use while on the device.
Several limitations of the current study must be noted. First, the current study only looked at the prevalence of cannabis use, and results reflect usage only during a brief interval prior to blood sampling. Arguably, understanding the rates at which drivers may use substances other than cannabis may be even more relevant as other substances may have a more pronounced risk of crash involvement. The current study was not able to examine patterns of substance use following device removal to determine if indeed elevated cannabis use persisted beyond the IID. This could have important implications for future research into polysubstance use and impaired driving research. Further, the current study had a limited sample size which reduces the externalizability of the findings. Such studies are appropriate for enhancing awareness of an issue, and promoting scientific understanding of a topic, which was the goal of the current endeavor. Finally, the time horizon mismatch between the brief detection interval prior to the blood sampling for cannabis and the 1–3 months of alcohol use estimated by the hair EtG is suboptimal. However, this study is not meant to be a definitive statement of a relationship between reduced alcohol use and increased cannabis use, but the results do nonetheless point to a significant relationship in that direction.
Despite these limitations, the current study provides valuable information on patterns of other drug use while the interlock is installed. Specifically, the study finds evidence that while the interlock is installed, some drivers are likely to increase their cannabis use. Drivers who decrease their overall alcohol consumption increase cannabis use significantly more than those who either retain their pre-interlock levels of alcohol use or else actually increase their alcohol use while the device is installed. Importantly, this finding does not indicate that IID installation is perilous or even ill-advised. Rather, because IIDs are successful while installed at notably reducing rates of driving under the influence of alcohol their utility is well-established. However, this finding does suggest that additional monitoring may be in order for drivers at risk of engaging in substance substitution while the IID is installed on their vehicle.
Acknowledgments
The research and preparation of this paper were conducted under a NIAAA grant (Grant ID# R01 AA022312). Points of view or opinions in this document are those of the authors and do not necessarily represent the official position or policies of the NIH.
Funding
This work was supported by the NIAAA [R01 AA022312].
References
- Aharonovich E, Liu X, Samet S, Nunes E, Waxman R, & Hasin D (2005). Postdischarge cannabis use and its relationship to cocaine, alcohol, and heroin use: A prospective study. American Journal of Psychiatry, 162(8), 1507–1514. 10.1176/appi.ajp.162.8.1507 [DOI] [PubMed] [Google Scholar]
- Biondi A, Freni F, Carelli C, Moretti M, & Morini L (2019). Ethyl glucuronide hair testing: A review. Forensic Science International, 300, 106–119. 10.1016/j.forsciint.2019.05.004 [DOI] [PubMed] [Google Scholar]
- Brubacher JR, Chan H, Erdelyi S, Macdonald S, Asbridge M, Mann RE, Eppler J, Lund A, MacPherson A, Martz W, Schreiber WE, Brant R, & Purssell RA (2019). Cannabis use as a risk factor for causing motor vehicle crashes: A prospective study. Addiction, 114(9), 1616–1626. 10.1111/add.14663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton RP, & Berning A (2015). Drug and alcohol crash risk (Traffic Safety Facts Research Note DOT HS 812 117). National Highway Traffic Safety Administration. [Google Scholar]
- Elder RW, Voas R, Beirness D, Shults RA, Sleet DA, Nichols JL, Compton R, & Task Force on Community Preventive, S. (2011). Effectiveness of ignition interlocks for preventing alcohol-impaired driving and alcohol-related crashes: A community guide systematic review. American Journal of Preventive Medicine, 40(3), 362–376. http://dx.doi.org.pire.idm.oclc.org/10.1016/j.amepre.2010.11.012 [DOI] [PubMed] [Google Scholar]
- Falk D, Yi H, & Hiller-Sturmhöfel S (2008). An epidemiologic analysis of co-occurring alcohol and drug use disorders: Findings from the National Epidemiologic Survey of Alcohol and Related Conditions (NESARC). Alcohol Research: Current Reviews, 31, 100–110. [PMC free article] [PubMed] [Google Scholar]
- Hartman RL, & Huestis MA (2013). Cannabis effects on driving skills. Clinical Chemistry, 59(3), 478–492. 10.1373/clinchem.2012.194381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knoche A, Pilgerstorfer M, Zlender B, Hagenzieker M, Alvarez J, Houwing S, Schulze H, Schumacher M, Urmeew R, Bernhoft IM, De Gier H, Drug A (2012). Driving under the influence of drugs, alcohol and medicines in Europe findings from the DRUID project. Thematic papers, 1725–9827. http://bookshop.europa.eu/uri?target=EUB:NOTICE:TDXA12006:EN:HTML [Google Scholar]
- Legrand S-A, Isalberti C, Linden TV, Bernhoft IM, Hels T, Simonsen KW, Favretto D, Ferrara SD, Caplinskiene M, Minkuviene Z, Pauliukevicius A, Houwing S, Mathijssen R, Lillsunde P, Langel K, Blencowe T, & Verstraete AG (2013). Alcohol and drugs in seriously injured drivers in six European countries. Drug Testing and Analysis, 5(3), 156–165. 10.1002/dta.1393 [DOI] [PubMed] [Google Scholar]
- Marques P, Tippetts S, Allen J, Javors M, Alling C, Yegles M, Pragst F, & Wurst F (2010). Estimating driver risk using alcohol biomarkers, interlock blood alcohol concentration tests and psychometric assessments: Initial descriptives. Addiction, 105(2), 226–239. 10.1111/j.1360-0443.2009.02738.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques PR, Tippetts AS, & Yegles M (2014). Ethylglucuronide in hair is a top predictor of impaired driving recidivism, alcohol dependence, and a key marker of the highest BAC interlock tests. Traffic Injury Prevention, 15(4), 361–369. 10.1080/15389588.2013.824569 [DOI] [PubMed] [Google Scholar]
- Marques PR, Voas RB, Tippetts AS, & Beirness DJ (1999). Behavioral monitoring of DUI offenders with the Alcohol Ignition Interlock Recorder. Addiction, 94(12), 1861–1870. 10.1046/j.1360-0443.1999.9412186111.x [DOI] [PubMed] [Google Scholar]
- O’Brien RM (2007). A caution regarding rules of thumb for variance inflation factors. Quality & Quantity, 41(5), 673–690. 10.1007/s11135-006-9018-6 [DOI] [Google Scholar]
- Peck RC, Gebers MA, Voas RB, & Romano E (2008). The relationship between blood alcohol concentration (BAC), age, and crash risk. Journal of Safety Research, 39(3), 311–319. 10.1016/j.jsr.2008.02.030 [DOI] [PubMed] [Google Scholar]
- Peters EN, & Hughes JR (2010). Daily marijuana users with past alcohol problems increase alcohol consumption during marijuana abstinence. Drug and Alcohol Dependence, 106, 111–118. 10.1016/j.drugalcdep.2009.07.027 [DOI] [PubMed] [Google Scholar]
- Reiman A (2009). Cannabis as a substitute for alcohol and other drugs. Harm Reduction Journal, 6(1), 35–40. 10.1186/1477-7517-6-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogeberg O, & Elvik R (2016). The effects of cannabis intoxication on motor vehicle collision revisited and revised. Addiction, 111(8), 1348–1359. 10.1111/add.13347 [DOI] [PubMed] [Google Scholar]
- Romano E, & Pollini RA (2013). Patterns of drug use in fatal crashes. Addiction, 108(8), 1428–1438. 10.1111/add.12180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scherer M, Canham S, Voas RB, & Furr-Holden CD (2018). Intercorrelation of alcohol and other drug use disorders among a national sample of drivers. Journal of Psychoactive Drugs, 50, 143–150. http://dx.doi.org.pire.idm.oclc.org/10.1080/02791072.2017.1366605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbaraman MS, Metrik J, Patterson D, & Swift R (2017). Cannabis use during treatment for alcohol use disorders predicts alcohol treatment outcomes. Addiction, 112(4), 685–694. 10.1111/add.13693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbaraman MS, Metrik J, Patterson D, & Stout RL (2018). Cannabis use during alcohol treatment is associated with alcohol-related problems one-year post-treatment. Drug and Alcohol Dependence, 193, 29–34. 10.1016/j.drugalcdep.2018.08020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2015). Behavioral health barometer: United States, 2015 (HHS Publication No. SMA-16-Baro-2015)., Rockville, MD. [PubMed] [Google Scholar]
- Sussman S, & Black DS (2008). Substitute addiction: A concern for researchers and practitioners. Journal of Drug Education, 38(2), 167–180. 10.2190/DE.38.2.e [DOI] [PubMed] [Google Scholar]
- Vanlaar WGM, Mainegra Hing M, & Robertson RD (2017). An evaluation of nova scotia’s alcohol ignition interlock program. Accident Analysis And Prevention, 100, 44–52. 10.1016/j.aap.2016.12.017 [DOI] [PubMed] [Google Scholar]
- Voas RB, Marques PR, Tippetts AS, & Beirness DJ (1999). The Alberta Interlock Program: The evaluation of a province-wide program on DUI recidivism. Addiction, 94(12), 1849–1859. 10.1046/j.1360-0443.1999.9412184910.x [DOI] [PubMed] [Google Scholar]
- Voas RB, Torres P, Romano E, & Lacey JH (2012). Alcohol-related risk of driver fatalities: An update using 2007 data. Journal of Studies on Alcohol and Drugs, 73(3), 341–350. 10.15288/jsad.2012.73.341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger AH, Platt J, & Goodwin RD (2016). Is cannabis use associated with an increased risk of onset and persistence of alcohol use disorders? A three-year prospective study among adults in the United States. Drug and Alcohol Dependence, 161(2), 363–367. 10.1016/j.drugalcdep.2016.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willis C, Lybrand S, & Bellamy N (2004). Alcohol ignition interlock programmes for reducing drink driving recidivism. The Cochrane Database of Systematic Reviews, 18(4), CD004168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson FA, Stimpson JP, & Pagán JA (2014). Fatal crashes from drivers testing positive for drugs in the U.S., 1993 – 2010. Public Health Reports, 129(4), 342–350. 10.1177/003335491412900409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zador P, Krawchuk SA, Voas RB, & Westat I (2000). Relative risk of fatal crash involvement by BAC, age and gender. National Highway Traffic Safety. [Google Scholar]


