Abstract
Full dynamics of biofluid biomarkers have been unknown in patients with Parkinson’s disease (PD). Using data from 396 PD patients and 182 controls in the Parkinson's Progression Markers Initiative (PPMI) database, we estimated long-term temporal trajectories of CSF α-synuclein (α-syn), amyloid-β (Aβ), total tau (t-tau), phosphorylated tau (p-tau) and serum neurofilament light chain (NfL) by integrating function between the baseline levels and annual changes. At baseline, PD patients showed lower CSF α-syn, Aβ, t-tau and p-tau levels than those of the controls. In all PD patients, CSF α-syn and Aβ decreased in a negative exponential pattern before the onset of motor symptoms, whereas CSF t-tau and p-tau, and serum NfL increased. Patients with cognitive impairment exhibited faster decline of Aβ and α-syn and faster rise of t-tau, p-tau and NfL, when compared to those without. Similarly, low Aβ group showed earlier decline of α-syn, faster rise of t-tau, p-tau and NfL, and faster decline of cognitive performances, when compared to high Aβ group. Our results suggest that longitudinal changes in biomarkers can be influenced by cognitive impairment and Aβ burden at baseline. PD patients with Aβ pathology may be associated with early appearance of α-synuclein pathology, rapid progression of axonal degeneration and neurodegeneration, and consequently greater cognitive decline.
Subject terms: Biomarkers, Neurology, Parkinson's disease
Introduction
About 80% of Parkinson’s disease (PD) patients become demented in their clinical course with variable time intervals between the onset of motor symptoms and deterioration of cognition1–3. Pathologically, greater amount of cortical and limbic Lewy bodies (LB), amyloid-β (Aβ) plaque and neurofibrillary tangles are related with the development of dementia in PD4,5. CSF biomarkers for each pathological protein may reflect the pathological burden in brain, and thereby, long-term changes in CSF biomarkers may be related with both pathological and clinical progression in PD.
However, several studies observed inconsistent results of longitudinal changes in CSF biomarkers. Some exhibited an increase in CSF α-synuclein (α-syn) along with the disease progression and an association of α-syn with further deterioration of motor and cognitive deficits6,7, while others reported a decrease in CSF α-syn8,9. Likewise, contradictory results of the longitudinal changes in CSF Aβ1-42 were reported10,11. These studies observed the changes occurring in relatively short time period (from 18 months to 4 years) at different time points of disease course, and therefore, were insufficient for providing full dynamics of CSF biomarkers.
In the present study, using the longitudinal data for the biomarkers in the Parkinson's Progression Markers Initiative (PPMI) study, we estimated long-term temporal trajectories of CSF α-syn, Aβ1-42, total tau (t-tau), phosphorylated tau (p-tau) and serum neurofilament light chain (NfL) by integrating the function between baseline level and annual change rates12,13. In addition, we investigated effects of cognitive impairment and low CSF Aβ1-42 level on the temporal trajectories of CSF biomarkers.
Results
Demographics, clinical measurement and biomarker levels at baseline
Demographic characteristics, clinical measurement and biomarker levels at baseline are summarized in Table 1. In total, 396 PD and 182 control subjects were included in the analyses. PD patients had lower CSF Aβ1-42 (β = − 106.9, SE 39.9, p = 0.008), α-syn (β = − 183.1, SE 65.0, p = 0.005), t-tau (β = − 24.3, SE 5.7, p < 0.001) and p-tau levels (β = − 2.7, SE 0.6, p < 0.001) than those of the controls, while the serum NfL levels did not exhibit a significant difference. In addition, PD patients showed worse cognitive performance in MoCA and HVLT delayed recall (MoCA, β = − 1.3, SE 0.2, p < 0.001; HVLT, β = − 3.9, SE 1.0, p < 0.001). Lower CSF α-syn and t-tau levels showed a trend of association with higher MDS-UPDRS III total scores at baseline, however, generalized linear models did not reach statistical significance (CSF α-syn, β = − 7.15, SE 3.85, p = 0.065; CSF t-tau, β = − 0.62, SE 0.34, p = 0.069).
Table 1.
Baseline demographics, biomarker levels and cognitive outcomes in PD and control subjects.
| Control | Total PD | High CSF Aβ1-42 | Low CSF Aβ1-42 | PDCU | PDCI | |
|---|---|---|---|---|---|---|
| n | 182 | 396 | 274 | 122 | 311 | 85 |
| Age | 60.6 ± 11.5 | 61.7 ± 9.7 | 61.5 ± 9.7 | 62.1 ± 9.8 | 60.91 ± 9.7 | 64.5 ± 9.5* |
| Sex (M:F) | 115: 67 | 264: 132 | 181: 93 | 83: 39 | 204: 107 | 60:25:00 |
| Education years | 15.9 ± 2.9 | 15.5 ± 3.0 | 15.6 ± 2.9 | 15.5 ± 3.1 | 15.7 ± 3.0 | 15.1 ± 2.7 |
| Disease duration | n.a | 2.0 ± 2.0 | 2.0 ± 2.0 | 2.0 ± 2.1 | 2.0 ± 1.9 | 2.1 ± 2.4 |
| APOE ε4 + (n) | 45/166 | 98/360 | 52/198* | 46/64 | 80/282 | 18/78 |
| MDS-UPDRS III | n.a | 21.3 ± 9.0 | 21.3 ± 8.8 | 21.4 ± 9.4 | 20.7 ± 8.7 | 23.5 ± 9.6* |
| H&Y stage (I/II/III) | n.a | 169/225/2 | 119/154/1 | 50/71/1 | 136/174/1 | 33/51/1 |
| CSF Aβ1-42 | 1022.6 ± 502.1 | 916.0 ± 414.8* | 1094.7 ± 373.7* | 514.6 ± 109.1 | 913.5 ± 416.3 | 925.0 ± 412.0 |
| CSF α-syn | 1701.3 ± 770.7 | 1528.7 ± 678.7* | 1693.0 ± 686.9* | 1173.0 ± 503.5 | 1512.3 ± 646.7 | 1588.7 ± 786.5 |
| CSF t-tau | 192.9 ± 80.4 | 170.5 ± 57.9 | 181.1 ± 53.9 | 144.2 ± 59.2 | 169.8 ± 56.5 | 173.0 ± 63.3 |
| CSF p-tau | 17.6 ± 8.5 | 15.0 ± 5.4* | 15.5 ± 5.0* | 13.3 ± 6.0 | 14.8 ± 5.2 | 15.6 ± 6.1 |
| Serum NfL | 12.4 ± 9.9 | 13.7 ± 11.8 | 13.7 ± 13.0 | 13.6 ± 8.7 | 13.5 ± 12.9 | 14.3 ± 6.3 |
| MoCA | 28.2 ± 1.1 | 27.1 ± 2.3* | 27.1 ± 2.3 | 27.4 ± 2.2 | 28.1 ± 1.3 | 23.6 ± 1.7* |
| HVLT-DR | 48.8 ± 11.0 | 44.8 ± 11.1* | 44.9 ± 11.0 | 44.5 ± 11.4 | 46.2 ± 10.8 | 39.6 ± 10.7* |
| LNS | 10.9 ± 2.6 | 10.6 ± 2.6 | 10.5 ± 2.7 | 10.7 ± 2.4 | 10.8 ± 2.6 | 9.5 ± 2.4* |
Data are presented as mean ± SD. *P < 0.05 for total PD vs. controls, low CSF Aβ1-42 vs. high CSF Aβ1-42, PDCU vs. PDCI.
PDCU cognitively unimpaired PD; PDCI cognitively impaired PD patients; APOE apolipoprotein E; MDS-UPDRS III Movement Disorder Society sponsored Unified Parkinson’s Disease Rating Scale part III; H&Y stage Hoehn & Yahr stage; Aβ1-42 amyloid-β1-42; α-syn α-synuclein; t-tau total tau; p-tau = phosphorylated tau; NfL neurofilament light chain; MoCA total scores of Montreal Cognitive Assessment; HVLT-DR delayed recall score in Hopkins Verbal Learning Test; LNS total scores of Letter-Number Sequencing test; n.a. not available.
311 PD patients showed MoCA total scores greater than 25 at baseline and were classified as PDNC. Although the PDCI group was older age and showed worse parkinsonian motor deficits at baseline than the PDNC, there was no clear difference in baseline biomarker levels between the two groups. According to the baseline CSF Aβ1-42, 274 PD patients were classified as high Aβ1-42 group and remaining 122 patients as low Aβ1-42. PD patients with low Aβ1-42 showed higher frequency of APOE ε4 allele and lower baseline CSF α-syn and p-tau than those with high CSF Aβ1-42. Serum NfL and cognitive performances did not show significant differences between the two groups.
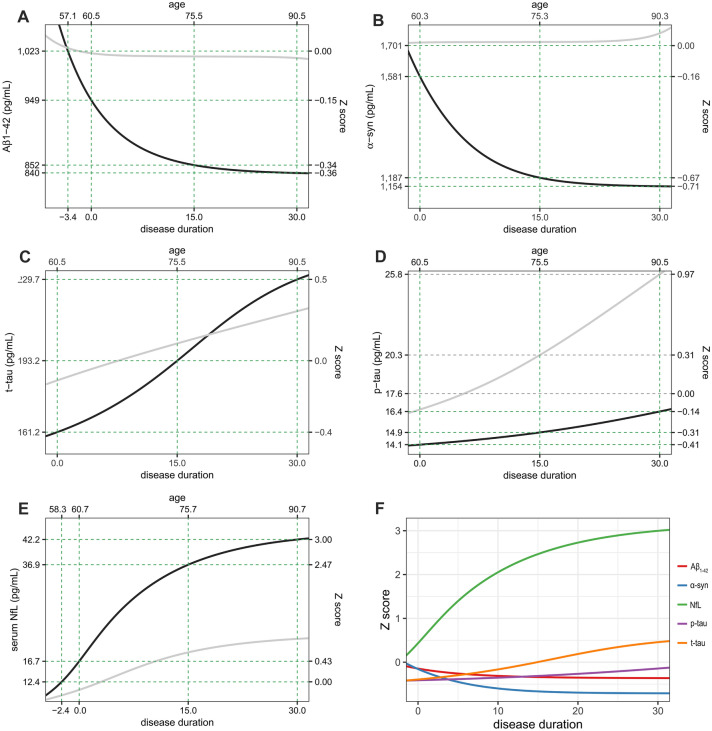
During the follow-up periods, entire PD patients showed an overall trend of decrease in CSF α-syn and Aβ1-42, whereas serum NfL were increased. CSF t-tau and p-tau levels remained almost constant from the baseline to 3rd year of follow-up (Fig. 1). In group comparisons using linear mixed effect models using age, sex and groups (PD and controls) as fixed effects and subjects as random effect, PD patients showed lower CSF α-syn (estimate − 285.9, SE 56.8, p < 0.001), Aβ1-42 (estimate − 143.2, SE 37.0, p < 0.001), t-tau (estimate − 28.4, SE 5.7, p < 0.001) and p-tau (estimate − 3.1, SE 0.6, p < 0.001) than control subjects, whereas serum NfL did not exhibit a significant difference during study period.
Figure 1.
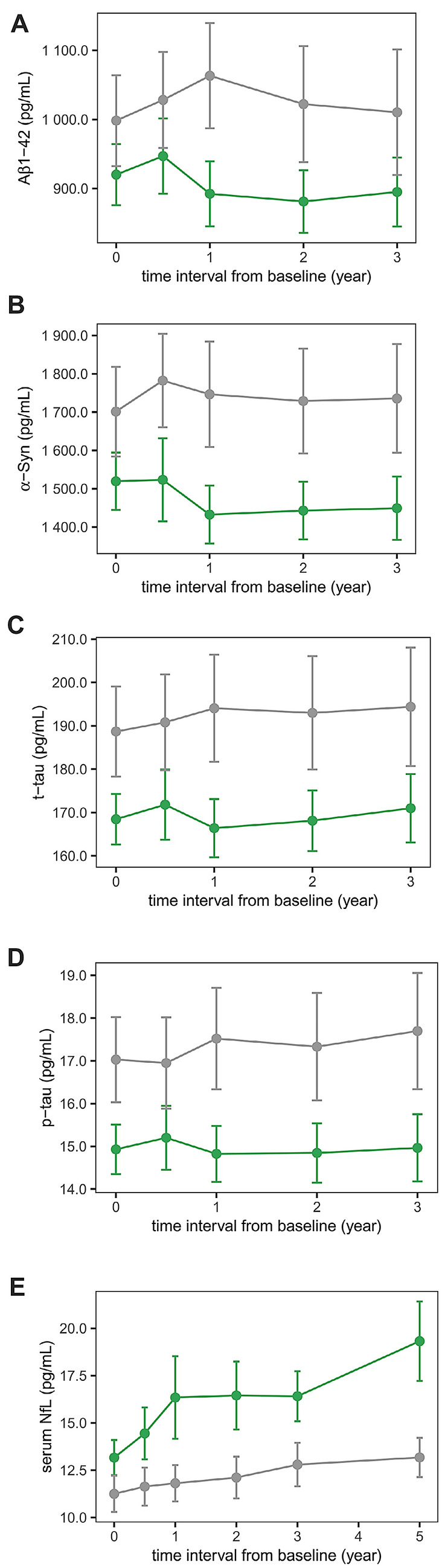
Measured biomarker levels in the PPMI study. Dots represent mean values of biomarkers at each follow-up visit. Error-bars denote 95% confidence interval (green lines and dots = PD patients; gray lines and dots = controls). Figures are illustrated using ggplot2 and patchwork packages in R software. Aβ1-42 amyloid-β1-42; α-syn α-synuclein; t-tau total tau; p-tau phosphorylated tau; NfL neurofilament light chain.
Temporal trajectories in total PD patients
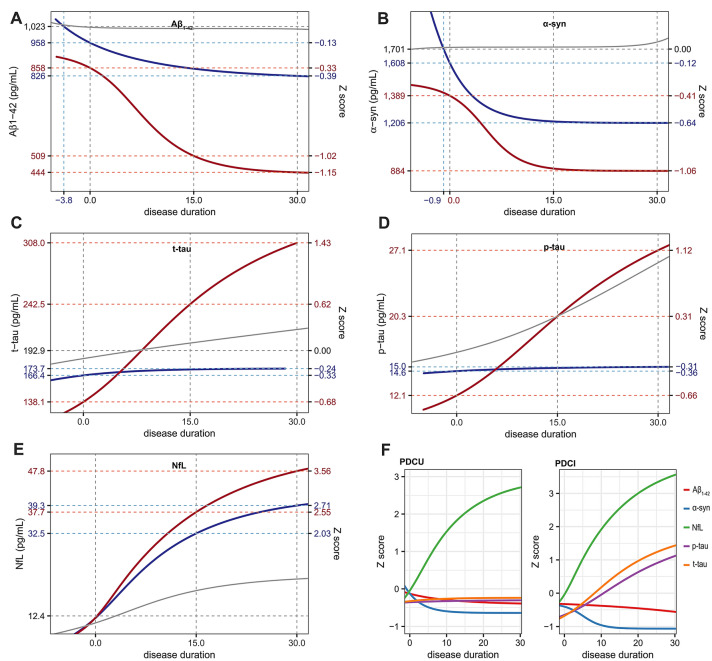
The restricted cubic spline function for baseline values vs. annual changes in CSF Aβ1-42 showed lower estimated annual changes in PD group than control subjects. Estimated annual changes were positive under 839 pg/mL of baseline baseline Aβ1-42 and 1014.1 pg/mL in controls, and then converted into negative at higher levels (Supplementary Fig. S1A). As a result, temporal trajectory of CSF Aβ1-42 in PD group initially showed a rapid decline from the premotor phase until about 5 years after the onset of motor symptoms and then slowly approached a plateau. Overall changes in CSF Aβ1-42 during the 30 years after the onset was estimated as − 12% (Fig. 2A). In contrast, trajectory in control group exhibited stable CSF Aβ1-42 values during estimated period.
Figure 2.
Estimated trajectories of biofluid markers in PD (black line) and control groups (gray line) as function of time. The temporal trajectories were acquired by modified Euler’s method for solving the first order differential equation. Temporal trajectories of CSF Aβ1-42 and α-syn show negative exponential pattern with suspicious plateau (A,B), while those of the CSF t-tau and p-tau, and serum NfL show steady increase pattern (D) or sigmoid appearance (C,E). Z score change in serum NfL was the largest within biofluid markers (F). Figures are illustrated using ggplot2 and patchwork packages in R software. Aβ1-42 amyloid-β1-42; α-syn α-synuclein; t-tau total tau; p-tau phosphorylated tau; NfL neurofilament light chain.
Restricted cubic spline curves for CSF α-syn showed similar pattern to those for Aβ1-42. Estimated annual changes continuously decreased along with the increase of baseline level, and converted into negative above 1,152 pg/mL of baseline in PD group and 1,715 pg/mL in control group (Supplementary Fig. S1B). Temporal trajectory of CSF α-syn showed a decline from the premotor phase, and then slowly approached a plateau. Overall changes in CSF α-syn during the 30 years after the onset was estimated as − 26.9% whereas trajectory of CSF in α-syn control group showed nearly steady level (Fig. 2B).
Estimated annual changes of CSF t-tau level in control group were slightly positive against baseline values, however, PD patients were estimated to exhibit negative annual changes over 242 pg/mL of baseline t-tau level (Supplementary Fig. S1C). In the estimated trajectories, PD patients had a lower CSF t-tau (161.2 pg/mL) at disease duration 0 than controls (184.6 pg/mL). Estimated temporal trajectories of CSF t-tau in PD and control groups exhibited increase of biomarker levels over time, however, CSF t-tau levels in PD group became higher about 19 years after motor onset compared to controls. Estimated CSF t-tau in PD group increased by 42% during 30 years of motor stage (Fig. 2C).
PD patients exhibited a lower CSF p-tau level at motor onset than that of the controls and the mean annual changes in CSF p-tau was close to zero (0.06 pg/mL/year) and smaller than those in controls (0.31 pg/mL/year; Supplementary Fig. S1D). Although the temporal trajectory of CSF p-tau showed a steady increase even after 30 years after the onset (Fig. 2D), it did not rose above the Z-score 0.
Finally, the curve for the estimated annual changes of serum NfL against baseline levels in PD group showed an inverted-U shape with a peak at 18.8 pg/mL of baseline. Restricted cubic spline curve for control group exhibited similar pattern, however estimated annual changes at peak (0.61 pg/mL/year at 13.4 pg/mL) was lower than that of PD patients (2.0 pg/mL/year). (Supplementary Fig. S1E). Temporal trajectory of serum NfL thereby showed a rapid increase compared to controls, and the increase rate was slowly decreased after 10 years after the onset. Compared to the estimated level at the onset, serum NfL in PD group showed an increase of 153% over the 30 years of symptomatic period (Fig. 2E), which was larger change than CSF Aβ1-42, α-syn, t-tau and p-tau. (Fig. 2F).
Influence of cognitive impairment at baseline on temporal trajectories of biomarkers
Linear mixed effect models using groups (PDCU and PDCI), disease duration, and interaction between groups and disease duration and subjects as random effect showed significant effect of interaction between disease duration and groups in progressions of CSF Aβ1-42, α-syn, t-tau and p-tau levels. Compared to PDCU group, patients with cognitive impairment at baseline exhibited slower decrement of CSF Aβ1-42 (estimate 22.94, SE 9.52, p = 0.016) and α-syn (estimate 63.3, SE 18.9, p < 0.001) and faster increase of t-tau (estimate 4.41, SE 1.29, p = 0.001) and p-tau (estimate 0.34, SE 0.10, p = 0.001; Supplementary Table S1).
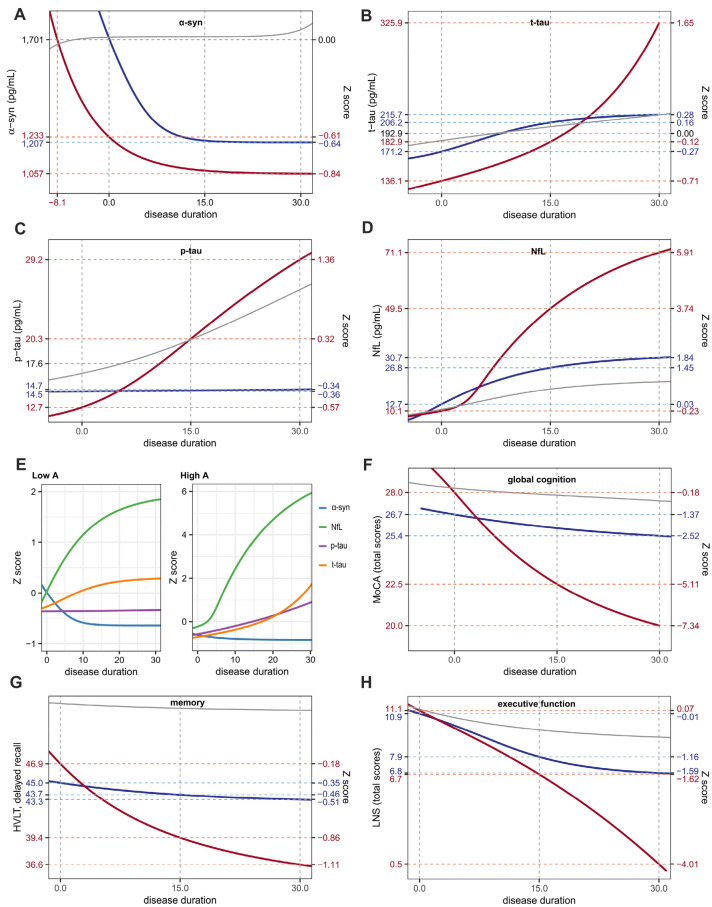
In the estimated trajectory, PDCI group showed a rapid decline of CSF Aβ1-42 and, while the PDCU group did not. During the 30 years of symptomatic period, PDCI group showed much greater change in CSF Aβ1-42 (− 48%) than PDCU group (− 14%; Fig. 3A). In the trajectories of CSF α-syn, both PDCU and PDCI groups approached plateau about 15 years from motor onset. However, PDCI group had lower α-syn level at motor onset and exhibited greater reduction (− 36%) during the 30 years of motor phase than PDCU patients (− 25%; Fig. 3B).
Figure 3.
Temporal trajectories of biomarkers in PD patients with and without cognitive impairment at baseline. PD patients with cognitive impairment (red lines) show greater change in all five biomarkers (A: Aβ1-42, B: α-syn, C: t-tau, D: p-tau, E: NfL) across the disease course than those without (blue lines). NfL showed the most remarkable changes both in PDCU and PDCI groups (F). Gray lines represent temporal trajectories in control group. Figures are illustrated using ggplot2 and patchwork packages in R software. Aβ1-42 amyloid-β1-42; α-syn α-synuclein; t-tau total tau; p-tau phosphorylated tau; NfL neurofilament light chain.
PDCU subset had a lower CSF t-tau level than PDCI group. In the estimated trajectories, PDCU group showed a little increment of t-tau (increase of 4.4% during 30 years after motor onset), whereas estimated t-tau levels in PDCI group showed a consistent rise (increase of 123.0% during 30 years after the onset). Estimated CSF t-tau levels of PDCI group at motor onset was lower than those of PDCU and control groups, however, became higher 5 and 8 years after motor onset, respectively (Fig. 3C). Similarly, CSF p-tau level in PDCI group was estimated to be lower than that in the PDCU and control groups at the onset. However, temporal trajectory of CSF p-tau in PDCI group exhibited steadily increasing pattern (increase by 124% during 30 years after the onset) close to that of controls. In contrast, the estimated CSF p-tau level barely changed throughout the disease course in PDCU group (increase by only 3% during 30 years after the onset; Fig. 3D). Trajectories of serum NfL showed initial rapid rise and later deceleration pattern in both two groups. Serum NfL levels in both PDCU and PDCI groups were estimated to be higher than control group for 30 years after motor onset. PDCI group showed greater change in serum NfL level (285%) than PDCU group (217%; Fig. 3E). In both PDCU and PDCI groups, changes of z scores were most remarkable in serum NfL (Fig. 3F).
Effect of CSF Aβ1-42 on temporal trajectories of biomarkers and cognitive outcomes
In the comparison of measured biomarker levels for 5 years, PD patients with low Aβ1-42 showed significantly lower CSF α-syn (estimate − 438.43, SE 83.41, p < 0.001), t-tau (estimate − 40.66, SE 7.21, p < 0.001) and p-tau levels (estimate − 2.64, SE 0.71, p < 0.001), whereas serum NfL did not exhibit significant difference (Supplementary Table S2). In addition, linear mixed effect models showed rapid decline of cognitive performance for 6-years of study period (interaction between group and disease duration; MoCA, estimate − 0.22, SE 0.03, p < 0.001; HVLT, estimate − 0.49, SE 0.15, p = 0.001; LNS, estimate − 0.07, SE 0.03, p = 0.023; Supplementary Table S3).
Low Aβ1-42 group showed earlier reduction of CSF α-syn below Z-score 0 (8.1 years before the onset) than high Aβ1-42 group (0.1 years after the onset). As the trajectories of CSF α-syn approached to plateau, difference in CSF α-syn levels between two groups gradually decreased. However, low CSF Aβ1-42 group exhibited still lower estimated CSF α-syn level than that of the high CSF Aβ1-42 group (Fig. 4A). Although low CSF Aβ1-42 group showed lower estimated CSF t-tau and p-tau levels at baseline than high Aβ1-42 group, temporal trajectory of CSF tau proteins in low Aβ1-42 group showed rapid rise throughout the disease course (Fig. 4B and C), and eventually CSF t-tau and p-tau levels in low Aβ1-42 group became higher than those in the high Aβ1-42 group about 20 years (t-tau) and 5 years (p-tau) after motor onset. Compared to trajectories in control group, CSF t-tau in PD patients with low CSF Aβ1-42 became higher about 19 years after motor onset, whereas p-tau levels showed similar increase during estimated 30 years. For serum NfL, PD patients with high and low CSF Aβ1-42 exhibited rapid increase of biomarker level compared to controls. In high CSF Aβ1-42 group, estimated serum NfL level increased up to 30.7 pg/mL (Z-score = 1.84) for 30 years, while low CSF Aβ1-42 group showed steady increase in serum NfL level up to 71.1 pg/mL (Z-score = 5.91) at 30 years after the onset (Fig. 4D). Temporal trajectories of serum NfL showed higher z score changes for 30 years after motor onset compared to other biofluid markers (Fig. 4E).
Figure 4.
Temporal trajectories of biomarkers and cognitive performances in PD patients with high and low CSF Aβ1-42 at baseline. PD patients with low CSF Aβ1-42 levels (red lines) show greater change in four biomarkers (A: α-syn, B: t-tau, C: p-tau, D: NfL) and cognitive decline (F: global cognition, G: memory, H: executive function) across the disease course than those with high CSF Aβ1-42 (blue lines). NfL showed the greater changes in the temporal trajectory among biomarkers (E). Gray lines represent temporal trajectories in control group. Figures are illustrated using ggplot2 and patchwork packages in R software. α-syn α-synuclein; t-tau total tau; p-tau phosphorylated tau; NfL neurofilament light chain; MoCA Montreal Cognitive Assessment; LNS Letter-Number Sequencing test; HVLT Hopkins Verbal Learning Test.
Both groups showed similar cognitive performances at the onset of motor symptoms. However, low CSF Aβ1-42 group exhibited faster decline of cognitive performances than high Aβ1-42 group. During the course of 30 years of symptomatic period, there was a greater reduction in MoCA total score in low CSF Aβ1-42 group (− 28.6%) than that in high CSF Aβ1-42 group (− 4.8%; Fig. 4F). Compared to control group, PD patients had lower estimated HVLT delayed recall scores regardless of baseline CSF Aβ1-42 classification. HVLT delayed recall scores showed a greater reduction in low CSF Aβ1-42 (− 22.0%) than high CSF Aβ1-42 group (− 3.8%; Fig. 4G). Compared to the high CSF Aβ1-42 group, low CSF Aβ1-42 exhibited similar reduction of LNS total score during the first decade from the onset. However, after that time point, decline in high CSF Aβ1-42 group was attenuated, thus difference between both groups was increased up to 6.1 (Z score = 2.42) at 30 years after the onset (Fig. 4H).
Discussion
Our temporal trajectory models exhibited that CSF Aβ1-42 and α-syn levels progressively decreased in a negative exponential pattern even before the onset of motor symptoms and approached a plateau. In contrast, CSF t-tau and p-tau, and serum NfL levels increased with the disease progression. These temporal changes in biomarkers were more likely to be greater in the PD patients with a cognitive impairment at baseline and in those with low CSF Aβ1-42 at baseline. PD patients with low CSF Aβ1-42 showed faster decline of cognitive performance than those with high CSF Aβ1-42 at baseline. Therefore, longitudinal changes in biomarkers can be influenced by the underlying cognitive impairment and amyloid-β pathology in PD.
We applied restricted cubic spline function to annual changes of biomarkers and integration of annual changes using ordinary differential equation modeling. These methods do not provide any statistical metrics, thus our analyses suggest a trend of further changes in biomarkers rather than a confirmative conclusion. Statistical analyses using empirical measurements would provide relatively conclusive results, however, as stated above, it is practically difficult to compose a cohort investigating long-term changes in biofluid markers. Moreover, statistical analysis requires a pre-defined assumption for shape of the trajectory. Without such a priori assumption, we attempted the mathematical model to predict long-term changes of biomarkers. Therefore, our study requires further cross-validation by longitudinal measurement of biofluid markers.
Previous studies investigating the longitudinal changes in CSF biomarkers in PD patients have reported inconsistent results6–11,14. An increase in CSF α-syn level was observed in a subset of PD patients selected by diagnostic likelihood over 90% in Deprenyl and Tocopherol Antioxidative Therapy for Parkinsonism (DATATOP) study7, whereas a contrary result was found in a study analyzing full dataset of the same cohort8. In PD without dementia, an increase in CSF α-syn level was observed only in the patients with disease duration longer than 5 years11. Moreover, contrary to our results, a previous analysis including 173 subjects PPMI database reported a significant increase in CSF Aβ1-42 during one year from baseline10. In our temporal trajectory models obtained from all PD patients in PPMI database, overall changes in CSF α-syn, Aβ1-42, t-tau and p-tau levels were only less than Z-score 1.0 during 30 years from the onset and more prominent in the patients with cognitive impairment and low CSF Aβ1-42. We suspect that the inconsistency between the previous studies was attributable to the relatively small long-term changes in CSF biomarkers and a heterogeneity of PD patients included. Indeed, a previous study including full dataset of PPMI demonstrated progressive decline of CSF Aβ1-42 during 3 years from baseline15. Therefore, a consistent and meaningful change can be expected by much longer observational period in a large number of PD patients with relatively homogeneous clinical features vulnerable to changes in CSF biomarkers.
Although the precise mechanism remains unclear, it was postulated that reduced CSF α-syn in PD may reflect altered dynamic of α-syn, possibly due to sequestration in intracellular LB pathology or enhanced extracellular clearance in α-synucleinopathy16–18. Nuclear imaging studies showed that decrease in CSF Aβ1-42 and increase in CSF t-tau and p-tau were correlated with increased amyloid and tau burden in brain19,20. Therefore, our results suggest that PD patients with cognitive impairment at early stage can be a phenotype resulting from an early appearance of LB load and rapid accumulation of amyloid and tau pathologies. LB and amyloid plaque pathologies in cortical and limbic regions are highly associated with the occurrence of dementia in the clinical course of PD4,5,21, and the patients with PD dementia were more likely to show lower CSF Aβ1-42 and higher CSF t-tau and p-tau levels, when compared to those with normal cognition22–24. Similar to our results, PD patients with low CSF Aβ1-42 at early stage showed worse cognitive performance25,26 and faster decline of cognitive performance in memory, executive and visuospatial function than those with high CSF Aβ1-4227,28.
NfL is a subunit of neurofilament protein, which is a major component of neuronal cytoskeleton and abundant in myelinated axons with large caliber29,30. Axonal degeneration preceding neuronal death and damaged white matter integrity in cellular model and patients with Alzheimer's disease are, for instance, the evidences for an involvement of white matter in neurodegenerative diseases31–33. Thus, CSF NfL level can be a biomarker for neuroaxonal damage in various kinds of neurodegenerative diseases34. A recent study showed a significant correlation between CSF and serum levels of NfL in PD patients, suggesting that serum NfL also can be a potential biomarker for neurodegeneration replacing CSF NfL35. Although some studies did not find an increased CSF NfL in PD6,30,36, the other studies observed an increased CSF or plasma NfL level in PD patients compared to the healthy elderly35,37. In a large biomarker study including over 3,000 subjects with dementia, patients with late onset AD or dementia with Lewy body (DLB) showed higher CSF NfL than PD subjects30. Therefore, we may expect that additional amyloid pathology in PD enhances an increase of NfL in both CSF and serum. It is interesting to note that estimated changes in serum NfL was much greater than CSF biomarkers in our study. Moreover, PD patients suspicious for having amyloid pathology exhibited great amount (almost 550%) of increase in serum NfL level over the 30 years. This suggests that the NfL level may be a potential biomarker for neurodegeneration induced by amyloid pathology6 or monitoring the disease progression in PD37.
It has been suggested that the dynamics of CSF α-syn, Aβ1-42, t-tau and p-tau may be intercorrelated in PD patients. Postmortem studies showed an association between cortical LB burden, amyloid plaque and tau grade38,39. Greater postmortem cortical LB burden was expected by the lower antemortem CSF Aβ1-42 level40. In transgenic mice model expressing cortical amyloid, early appearance of widespread α-syn pathology can be induced by an injection of preformed α-syn fibril into the hippocampus41. Similarly, α-syn pathology promoted fibrillization and phosphorylation of tau proteins in cellular and transgenic animal models42,43. Several studies demonstrated a correlation between CSF α-syn, Aβ1-42 and p-tau levels6,25,44,45. Therefore, amyloid load in central nervous system of PD patients may cause not only neurodegenerative process related with Alzheimer’s disease, but accelerated propagation of α-syn pathology. As stated above, our estimated trajectory of serum NfL suggested a possible impact of amyloid burden on neuroaxonal integrity, and disruption of white matter integrity are related to deterioration of cognitive performance in working memory, attention and executive function, visuospatial skills, and psychomotor speed46. Our estimated trajectories are consistent with previous studies showing predictive value of CSF Aβ1-42 for global and domain specific cognitive decline15.
In this study, we stratified PD group either by CSF Aβ1-42 or cognition at the time point of baseline assessment in PPMI database. Because the patients had various disease duration at baseline, our study can be limited by the absence of synchronization of CSF Aβ1-42 and cognition levels in dichotomizing groups. In addition, we extrapolated biomarker levels and cognitive outcomes about 30 years of disease duration using longitudinal measurement of 5–7 years. Because the PPMI database only included the PD patients in their early stage of disease course, our study is limited by missing biomarker data for the far advanced PD patients and the changes in biomarkers might be underestimated. Therefore, our temporal trajectory models require to be further revised by including advanced PD patients.
In summary, our temporal trajectory models suggest that longitudinal changes in biomarkers can vary with amyloid burden or cognitive impairment in PD patients. Early occurrence of cognitive impairment can be a clinical feature suspecting more rapid growth of LB and AD type pathologies. PD patients with low CSF Aβ1-42 may be more vulnerable to LB pathology, neuroaxonal damage, and cognitive impairment in their clinical course. Our study results raised a possibility for the potential role of future amyloid-lowering therapy for delaying the pathological progression and cognitive decline in PD.
Methods
Participants
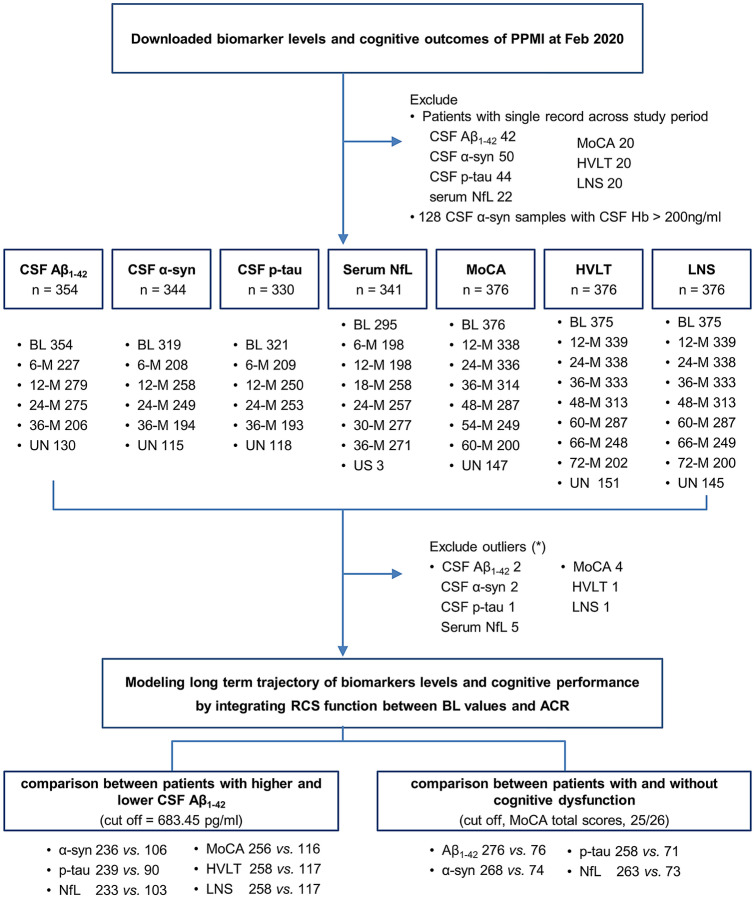
Study design is summarized in Fig. 5. From the PPMI database (http://ppmi-info.org), anonymized and de-identified results as of Feb 2020 were downloaded. Briefly, the PPMI study is an observational cohort study aimed at identifying biomarkers of PD progression. The eligibility criteria include PD patients older than 30 years of age, diagnosed with PD within the last 2 years with a Hoehn & Yahr (H&Y) stage not greater than II, untreated, and exhibiting striatal dopaminergic dysfunction on 123I-N-3-fluoropropyl-2β-carbomethoxy-3β-4-iodophenyl tropane (123I-FP-CIT) single photon emission computed tomography (SPECT). The detailed study protocol can be found at www.ppmi-info.org.
Figure 5.
Study design. *Outliers were defined as patients with more than 3 interquartile ranges below the first quartile or above the third quartile in baseline biomarker levels, or patients with cognitive outcomes beyond the mean ± 4 SD. PPMI Parkinson's Progression Markers Initiative; NfL neurofilament light chain; Hb Hemoglobin; MoCA Montreal Cognitive Assessment, total scores; HVLT Hopkin's Verbal Learning test, total scores of delayed recall; LNS Letter-Number-Sequencing test, total scores; BL baseline; 6-, 12-, 18-, 24-, 30-, 36-, 48-, 54-, 60-, 66-, 72-M = months from baseline visit; UN unscheduled measurement; ACR annual change rates; RCS restricted cubic spline.
We included PD and control subjects who had undergone measurement of CSF α-syn, Aβ1-42, p-tau and serum NfL at least twice. Age-at-onset (AAO) was defined as the time interval between date of birth and self-declared motor onset, and disease duration as the time interval between the self-declared motor onset and sampling date. The severity of parkinsonian motor deficits was assessed by the Movement Disorder Society sponsored Unified Parkinson Disease Rating Scale (MDS-UPDRS) part III and H&Y stage. To estimate the effect of baseline CSF Aβ1-42 on longitudinal cognitive performance, we included total scores of Montreal Cognitive Assessment (MoCA), Letter-Number Sequencing (LNS) test, and delayed recall scores of Hopkins Verbal Learning Test (HVLT). In addition, genotyping of Apolipoprotein E (APOE) was included in the analyses. We classified PD patients into cognitively unimpaired (PDCU, MoCA total scores > 25) and cognitively impaired (PDCI, MoCA total scores ≤ 25) groups47.
The PPMI study is registered at ClinicalTrials.gov (NCT01141023). Each PPMI site received approval from an ethics committee on human experimentation prior to study initiation. All research was performed in accordance with the relevant guidelines and regulations. The institutional review board of Pusan National University approved secondary analyses of publically shared data. The informed written consent has been waived off by the institutional review board of Pusan National University.
Measurement of biomarkers
CSF was collected by standardized lumbar puncture procedures. Shipment and storage were performed as described in the PPMI biological manual (http://ppmi-info.org) and elsewhere26,48. The coded frozen aliquots of CSF were transferred from the PPMI Biorepository Core laboratories to the University of Pennsylvania and to Covance for analyses. CSF Aβ1-42, t-tau and p-tau were measured using the electrochemiluminescence (ECL) immunoassays on a fully automated cobas e601 analyzer (Elecsys, Roche diagnostic). The concentration of α-syn in CSF samples were analyzed using commercially available sandwich type ELISA kits (Covance, Dedham, MA), as previously described26. Serum NfL level was measured by the 2-step digital immunoassay using Single Molecule Array (Simoa) technology (NF-light; UmanDiagnostics, Umeå, Sweden). In the present study, CSF α-syn samples with low hemoglobin (< 200 ng/mL)9 were included in the analyses. As proposed by a recent study analyzing PPMI database15, we used cut-off 683.45 pg/mL for deciding high and low Aβ1-42 groups. In addition, we excluded the PD patients with baseline biomarker levels more than 3 interquartile ranges below first quartile or above the third quartile.
Estimation of temporal trajectories
As described in the previous literatures12,13, we first applied linear regression for each subject to calculate the annual change rates of CSF biomarker levels over time. Linear regression model of each subject had disease duration (year) as predictor and biomarker or scores of cognitive function tests as responder variable. In case of control group, time interval from baseline (year) was used as predictor term. In addition, CSF biomarker levels and scores of cognitive function tests at the onset of motor symptoms were calculated using the linear regression model. Then, we acquired a curve for annual changes in each biomarker as a function of baseline values by using restricted cubic spline with 4 knots. The knots were placed at 5-, 35-, 65- and 95-percentile values of baseline levels. When sample size was under 100, we applied 3 knots at 5-, 50-, 95-percentile values. Estimated levels as a function of time in year were acquired by using the modified Euler’s method for solving the first order differential equation. Finally, based on the calculated biomarker levels at motor onset, we plotted trajectories of estimated CSF biomarker levels between the time points at 5 years before and 30 years after the onset of motor symptoms. To compare with control subjects, we also calculated Z-score using the mean and SD obtained from baseline values of control groups. In addition, we estimated temporal trajectories of biomarkers and scores of cognitive function tests in control group using same method. Calculated trajectories of control group were anchored to time axis (age) using mean values of biomarkers and cognitive performances and median age at baseline visit of PPMI study. For comparison between PD and control groups, we converted age into disease duration using following formula: disease duration = age – median of age at motor onset in PD patients.
Statistical analyses
Age, disease duration, education period and MDS-UPDRS III total scores were compared using independent t-test. Chi-square test was employed to compare categorical variables including sex ratio, APOE e4 allele frequency, and H&Y stage. Comparison of longitudinal biomarker levels and cognitive outcomes between groups were testing by linear mixed effect models using group, disease duration, and interaction between group and disease duration as fixed effects and subjects as random effect. Biomarker levels and cognitive outcomes at baseline were tested using generalized linear model covariated with age and sex. Statistical significance was defined as p < 0.05. Estimation of temporal trajectories and statistical analyses were conducted by custom script written in R software (version 3.6.2; r-project.org) with Hmisc and rms packages.
Supplementary Information
Acknowledgements
Parkinson's Progression Markers Initiative (PPMI)—a public-private partnership—is funded by the Michael J. Fox Foundation for Parkinson's Research and funding partners, including AbbVie, Allergan, Amathus Therapeutics, Avid, Biogen, BioLegend, Bristol-Myers Squibb, Celgene, Denali, GE Healthcare, Genentech, GlaxoSmithKline, Golub Capital, Handl Therapeutics, Insitro, Janssen Neuroscience, Lilly, Lundbeck, Merck, MesoScaleDiscovery, Pfizer, Piramal, Prevail Therapeutics, Roche, Sanofi Genzyme, Servier, Takeda, TEVA, UCB, Verily, and Voyager Therapeutics.
Author contributions
M.S.B. contributed with: conception and design, data analysis and interpretation, and manuscript writing. M.J.L. contributed with: conception and design, collection and assembly of data, data analysis and interpretation, manuscript writing, and final approval of manuscript. H.K.K. contributed with: collection and assembly of data, data analysis and interpretation. C.H.L. contributed with: conception and design, data analysis and interpretation, administrative support. M.J.L. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Funding
This research was supported by a grant from Korean Neurological Association (KNA-19-MI-12) and Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2017R1A2B2006694).
Data availability
The full dataset from the PPMI study is available at www.ppmi-info.org.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-94345-8.
References
- 1.Aarsland D, Andersen K, Larsen JP, Lolk A, Kragh-Sorensen P. Prevalence and characteristics of dementia in Parkinson disease: An 8-year prospective study. Arch. Neurol. 2003;60:387–392. doi: 10.1001/archneur.60.3.387. [DOI] [PubMed] [Google Scholar]
- 2.Hughes TA, et al. A 10-year study of the incidence of and factors predicting dementia in Parkinson's disease. Neurology. 2000;54:1596–1602. doi: 10.1212/WNL.54.8.1596. [DOI] [PubMed] [Google Scholar]
- 3.Aarsland D, et al. The effect of age of onset of PD on risk of dementia. J. Neurol. 2007;254:38–45. doi: 10.1007/s00415-006-0234-8. [DOI] [PubMed] [Google Scholar]
- 4.Mattila PM, Rinne JO, Helenius H, Dickson DW, Roytta M. Alpha-synuclein-immunoreactive cortical Lewy bodies are associated with cognitive impairment in Parkinson's disease. Acta Neuropathol. 2000;100:285–290. doi: 10.1007/s004019900168. [DOI] [PubMed] [Google Scholar]
- 5.Irwin DJ, Lee VM, Trojanowski JQ. Parkinson's disease dementia: Convergence of alpha-synuclein, tau and amyloid-beta pathologies. Nat. Rev. Neurosci. 2013;14:626–636. doi: 10.1038/nrn3549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hall S, et al. CSF biomarkers and clinical progression of Parkinson disease. Neurology. 2015;84:57–63. doi: 10.1212/WNL.0000000000001098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Majbour NK, et al. Longitudinal changes in CSF alpha-synuclein species reflect Parkinson's disease progression. Mov. Disord. 2016;31:1535–1542. doi: 10.1002/mds.26754. [DOI] [PubMed] [Google Scholar]
- 8.Stewart T, et al. Cerebrospinal fluid alpha-synuclein predicts cognitive decline in Parkinson disease progression in the DATATOP cohort. Am. J. Pathol. 2014;184:966–975. doi: 10.1016/j.ajpath.2013.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mollenhauer B, et al. Longitudinal analyses of cerebrospinal fluid alpha-Synuclein in prodromal and early Parkinson's disease. Mov. Disord. 2019;34:1354–1364. doi: 10.1002/mds.27806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mollenhauer B, et al. Longitudinal CSF biomarkers in patients with early Parkinson disease and healthy controls. Neurology. 2017;89:1959–1969. doi: 10.1212/WNL.0000000000004609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hall S, et al. Longitudinal measurements of cerebrospinal fluid biomarkers in Parkinson's disease. Mov. Disord. 2016;31:898–905. doi: 10.1002/mds.26578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jack CR, Jr, et al. Brain beta-amyloid load approaches a plateau. Neurology. 2013;80:890–896. doi: 10.1212/WNL.0b013e3182840bbe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baek MS, et al. Temporal trajectories of in vivo tau and amyloid-beta accumulation in Alzheimer's disease. Eur. J. Nucl. Med. Mol. Imaging. 2020;47:2879–2886. doi: 10.1007/s00259-020-04773-3. [DOI] [PubMed] [Google Scholar]
- 14.Forland MG, et al. Evolution of cerebrospinal fluid total alpha-synuclein in Parkinson's disease. Parkinson. Relat. Disord. 2018;49:4–8. doi: 10.1016/j.parkreldis.2018.01.018. [DOI] [PubMed] [Google Scholar]
- 15.Irwin DJ, et al. Evolution of Alzheimer's disease cerebrospinal fluid biomarkers in early Parkinson's disease. Ann. Neurol. 2020;88:574–587. doi: 10.1002/ana.25811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parnetti L, Cicognola C, Eusebi P, Chiasserini D. Value of cerebrospinal fluid alpha-synuclein species as biomarker in Parkinson's diagnosis and prognosis. Biomark. Med. 2016;10:35–49. doi: 10.2217/bmm.15.107. [DOI] [PubMed] [Google Scholar]
- 17.Diamandis EP, et al. Immunofluorometric assay of human kallikrein 6 (zyme/protease M/neurosin) and preliminary clinical applications. Clin. Biochem. 2000;33:369–375. doi: 10.1016/S0009-9120(00)00145-4. [DOI] [PubMed] [Google Scholar]
- 18.Spencer B, et al. Lentivirus mediated delivery of neurosin promotes clearance of wild-type alpha-synuclein and reduces the pathology in an alpha-synuclein model of LBD. Mol. Ther. 2013;21:31–41. doi: 10.1038/mt.2012.66. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 19.La Joie R, et al. Associations between [(18)F]AV1451 tau PET and CSF measures of tau pathology in a clinical sample. Neurology. 2018;90:e282–e290. doi: 10.1212/WNL.0000000000004860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Almdahl IS, et al. Cerebrospinal fluid levels of amyloid beta 1–43 mirror 1–42 in relation to imaging biomarkers of Alzheimer's disease. Front. Aging Neurosci. 2017;9:9. doi: 10.3389/fnagi.2017.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aarsland D, et al. Cognitive decline in Parkinson disease. Nat. Rev. Neurol. 2017;13:217–231. doi: 10.1038/nrneurol.2017.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mollenhauer B, et al. alpha-Synuclein and tau concentrations in cerebrospinal fluid of patients presenting with Parkinsonism: A cohort study. Lancet Neurol. 2011;10:230–240. doi: 10.1016/S1474-4422(11)70014-X. [DOI] [PubMed] [Google Scholar]
- 23.Buongiorno M, et al. Cross-sectional and longitudinal cognitive correlates of FDDNP PET and CSF amyloid-beta and tau in Parkinson's disease1. J. Alzheimers Dis. 2017;55:1261–1272. doi: 10.3233/JAD-160698. [DOI] [PubMed] [Google Scholar]
- 24.Compta Y, et al. Cerebrospinal tau, phospho-tau, and beta-amyloid and neuropsychological functions in Parkinson's disease. Mov. Disord. 2009;24:2203–2210. doi: 10.1002/mds.22594. [DOI] [PubMed] [Google Scholar]
- 25.Murakami H, et al. Correlated levels of cerebrospinal fluid pathogenic proteins in drug-naive Parkinson's disease. BMC Neurol. 2019;19:113. doi: 10.1186/s12883-019-1346-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kang JH, et al. CSF biomarkers associated with disease heterogeneity in early Parkinson's disease: The Parkinson's Progression Markers Initiative study. Acta Neuropathol. 2016;131:935–949. doi: 10.1007/s00401-016-1552-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin CH, Wu RM. Biomarkers of cognitive decline in Parkinson's disease. Parkinsonism Relat. Disord. 2015;21:431–443. doi: 10.1016/j.parkreldis.2015.02.010. [DOI] [PubMed] [Google Scholar]
- 28.Siderowf A, et al. CSF amyloid beta 1–42 predicts cognitive decline in Parkinson disease. Neurology. 2010;75:1055–1061. doi: 10.1212/WNL.0b013e3181f39a78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Petzold A. Neurofilament phosphoforms: Surrogate markers for axonal injury, degeneration and loss. J. Neurol. Sci. 2005;233:183–198. doi: 10.1016/j.jns.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 30.Skillback T, et al. CSF neurofilament light differs in neurodegenerative diseases and predicts severity and survival. Neurology. 2014;83:1945–1953. doi: 10.1212/WNL.0000000000001015. [DOI] [PubMed] [Google Scholar]
- 31.Alobuia WM, Xia W, Vohra BP. Axon degeneration is key component of neuronal death in amyloid-beta toxicity. Neurochem. Int. 2013;63:782–789. doi: 10.1016/j.neuint.2013.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mito R, et al. Fibre-specific white matter reductions in Alzheimer's disease and mild cognitive impairment. Brain. 2018;141:888–902. doi: 10.1093/brain/awx355. [DOI] [PubMed] [Google Scholar]
- 33.Hoy AR, et al. Microstructural white matter alterations in preclinical Alzheimer's disease detected using free water elimination diffusion tensor imaging. PLoS ONE. 2017;12:e0173982. doi: 10.1371/journal.pone.0173982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bridel C, et al. Diagnostic value of cerebrospinal fluid neurofilament light protein in neurology: A systematic review and meta-analysis. JAMA Neurol. 2019;76:1035–1048. doi: 10.1001/jamaneurol.2019.1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oosterveld LP, et al. CSF or serum neurofilament light added to alpha-Synuclein panel discriminates Parkinson's from controls. Mov. Disord. 2020;35:288–295. doi: 10.1002/mds.27897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marques TM, et al. Serum NFL discriminates Parkinson disease from atypical parkinsonisms. Neurology. 2019;92:e1479–e1486. doi: 10.1212/WNL.0000000000007179. [DOI] [PubMed] [Google Scholar]
- 37.Lin CH, et al. Blood NfL: A biomarker for disease severity and progression in Parkinson disease. Neurology. 2019;93:e1104–e1111. doi: 10.1212/WNL.0000000000008088. [DOI] [PubMed] [Google Scholar]
- 38.Lashley T, et al. Cortical alpha-synuclein load is associated with amyloid-beta plaque burden in a subset of Parkinson's disease patients. Acta Neuropathol. 2008;115:417–425. doi: 10.1007/s00401-007-0336-0. [DOI] [PubMed] [Google Scholar]
- 39.Irwin DJ, et al. Neuropathologic substrates of Parkinson disease dementia. Ann. Neurol. 2012;72:587–598. doi: 10.1002/ana.23659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Irwin DJ, et al. CSF tau and beta-amyloid predict cerebral synucleinopathy in autopsied Lewy body disorders. Neurology. 2018;90:e1038–e1046. doi: 10.1212/WNL.0000000000005166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bassil F, et al. Amyloid-beta (Abeta) plaques promote seeding and spreading of alpha-synuclein and tau in a mouse model of lewy body disorders with abeta pathology. Neuron. 2020;105:260–275. doi: 10.1016/j.neuron.2019.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Duka T, Duka V, Joyce JN, Sidhu A. Alpha-Synuclein contributes to GSK-3beta-catalyzed Tau phosphorylation in Parkinson's disease models. FASEB J. 2009;23:2820–2830. doi: 10.1096/fj.08-120410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guo JL, et al. Distinct alpha-synuclein strains differentially promote tau inclusions in neurons. Cell. 2013;154:103–117. doi: 10.1016/j.cell.2013.05.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Goldman JG, et al. Cerebrospinal fluid, plasma, and saliva in the BioFIND study: Relationships among biomarkers and Parkinson's disease Features. Mov. Disord. 2018;33:282–288. doi: 10.1002/mds.27232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Majbour NK, et al. Oligomeric and phosphorylated alpha-synuclein as potential CSF biomarkers for Parkinson's disease. Mol. Neurodegener. 2016;11:7. doi: 10.1186/s13024-016-0072-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tomimoto H. White matter integrity and cognitive dysfunction: Radiological and neuropsychological correlations. Geriatr. Gerontol. Int. 2015;15(Suppl 1):3–9. doi: 10.1111/ggi.12661. [DOI] [PubMed] [Google Scholar]
- 47.Dalrymple-Alford JC, et al. The MoCA: Well-suited screen for cognitive impairment in Parkinson disease. Neurology. 2010;75:1717–1725. doi: 10.1212/WNL.0b013e3181fc29c9. [DOI] [PubMed] [Google Scholar]
- 48.Kang JH, et al. Association of cerebrospinal fluid beta-amyloid 1–42, T-tau, P-tau181, and alpha-synuclein levels with clinical features of drug-naive patients with early Parkinson disease. JAMA Neurol. 2013;70:1277–1287. doi: 10.1001/jamaneurol.2013.3861. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The full dataset from the PPMI study is available at www.ppmi-info.org.