Introduction
Participation in ultraendurance running (UER) has increased considerably, especially over the past 20 years the participation worldwide has risen from 5000 in 2000 to 300 000 in 2017.1 It includes running distances over 42.195 km, timed events over 6 hours duration or multiday or multistage events. Additionally, there is also an important increase in youth UER participation under the ages of 19 years.2 The long-term impact on human health due to extreme exercise bouts, such as UER, is largely unknown.
Research in UER has primarily focused on acute physiological, biochemical and medical alterations immediately or shortly after UER events but long-term health effects have rarely been investigated. UER is considered one of the sports that causes the most functional and structural damage due to its high intensity and volume.3 UER usually affects anti-inflammatory and proinflammatory responses leading to several acute preclinical and clinical issues.4 In this editorial, we aim to discuss some of the potential long-term health implications of UER based on central body systems.
Cardiovascular implications
UER may have negative effects on cardiovascular health such as acute alterations in biomarkers of cardiac damage (eg, cardiac troponin-I, ventricular natriuretic peptide)5 and potential long-term cardiac issues such as ventricular dysfunction, myocardial remodelling, atrial fibrillation, myocardial fibrosis or right ventricle exercise-induced cardiomyopathy later in life. However, the risk is low and usually depends on a pre-existing cardiovascular condition and there is a U-shaped relationship of lifetime-accumulated high-intensity endurance training.6 In addition, with the rising number of athletes participating in UER, endurance sport-associated atrial fibrillation may become increasingly prevalent in the future.
Renal function
Acute kidney injury (AKI) is commonly observed after UER but is generally minor, with full recovery post event in a few days. UER represents 96.9% of the total AKI cases among endurance athletes; some of the risk factors for AKI development include prior ingestion of nonsteroidal anti-inflammatory drugs, dehydration, heat strain, competing at moderate altitude and high physical load.3 Occasionally, severe AKI is observed, combined with rhabdomyolysis and altered renal function, which may last for weeks or months. Although there is no clear evidence that cumulative or subsequent functional or structural AKI events could contribute to future chronic damage in UER, the link between AKI and chronic kidney disease has been explored in other populations, supported by the potential maladaptive repair after cumulative AKI events and progressive renal scarring.7 In UER, if repetitive insults in the form of AKI or severe cases of AKI lead to accelerated progression of chronic kidney diseases is currently unknown. However, it may be advisable to perform prerace screening of UER athletes for baseline measurements of kidney functions and monitor UER athletes after confirmed AKI episodes.
Musculoskeletal injuries
Severe muscle damage can lead to rhabdomyolysis, whereas mild cases are typically asymptomatic. Although there is no link between these events with chronic disorders, there is a need to establish diagnostic criteria of exertional rhabdomyolysis for UER athletes3 to better identify potential asymptomatic cases.
Musculoskeletal injuries are common in UER, caused mostly by overuse and affecting the lower limbs (eg, patellofemoral pain syndrome). However, it is currently unclear if this is related to long-term or long-lasting sequelae in later life. A particular concern is the increased risk of bone stress in youth athletes. The effect of prolonged lifetime running on musculoskeletal health is not well understood, particularly when starting at a young age representing an increased lifetime risk of developing stress fractures with a lifetime prevalence of 14% compared with adults.8 Long-term studies are needed for evaluating risk factors leading to musculoskeletal injuries, and the role of training volume/intensity is essential on these potential chronic conditions.
Respiratory responses
Besides, due to long-term outdoor training and increased ventilation while running, some respiratory conditions could be developed.9 Also, the prevalence of these respiratory affections could increase due to some environmental conditions. Among the respiratory conditions, the most common conditions we can find are chronic airway inflammation with exercise-induced asthma, bronchoconstriction airway hyper-responsiveness, acute bronchial epithelial cell injury, airways inflammation, reduction in expiratory pulmonary function, respiratory muscle fatigue, pulmonary oedema and pulmonary alveolar-capillary derecruitment. However, the incidence of respiratory issues in UER seems not to be higher than in the general population. It is also known that some respiratory issues are more prevalent following a marathon than a UER, this might be a factor of work rate and intensity.10
Conclusions and future challenges
Admitting insufficient evidence that links acute health complications to future chronic outcomes, extreme repeated exercise bouts such as UER may adversely affect susceptible participants. This seems best researched in cardiovascular, musculoskeletal and renal systems, which show a U-shaped relationship between the system function and high-volume and intensity exercise bout and without a clear understanding of the future impact of these repeated exercise bouts (see figure 1). Furthermore, inflammation during and after UER might be related to functional over-reaching.4
Figure 1.
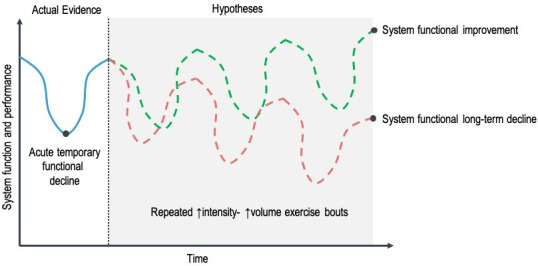
The potential impact of repeated high-intensity and high-volume bouts of ultraendurance running on cardiovascular, respiratory, musculoskeletal and renal function and structure.
Besides, the exact pathophysiology and percentage of UER that develop sports related chronic health issues are currently unknown and further studies are needed. This may be of particular interest since there is also a growing number of youth athletes participating in UER, a population with a particular risk of developing sports related chronic health complications at a younger age.
It is fundamental to note that lifelong exercisers generally have lower incidence and prevalence of chronic diseases, lower mortality rates and higher functional capacity than those with some sedentary behaviours. But finally, is there a reason for concern? Although the long-term health issues related to UER are relatively uncommon, there is still an increasing number of cases developing aftermath of acute events.
In this sense, medical staff and coaches may frequently monitor runners’ health to detect any change that could develop future adverse outcomes and optimally guide exercise prescription, avoiding loads with high volume and intensity components and promoting adequate and timely recovery between efforts. The constant athlete’s health assessment must be a topic of permanent interest to prevent, monitor any changes and treat in a timely, effective and efficient manner. In this regard, existing technologies (eg, wearables and tracking systems) and methods (eg, novel biomarkers) could stimulate researchers to conduct more high-quality studies under real running and outpatient settings, especially those with a longitudinal component. Research understanding the underlying mechanisms and variables associated with potential pathologic outcomes of UER to prevent subsequent chronic sports related health issues is needed.
Footnotes
VS and DR-V contributed equally.
Contributors: Both authors prepared and wrote the original draft, contributed to the literature search, critically revised the manuscript and approved the final version of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Scheer V. Participation trends of ultra endurance events. Sports Med Arthrosc Rev 2019;27:3–7. 10.1097/JSA.0000000000000198 [DOI] [PubMed] [Google Scholar]
- 2.Scheer V, Di Gangi S, Villiger E, et al. Participation and performance analysis in children and adolescents competing in time-limited Ultra-Endurance running events. Int J Environ Res Public Health 2020;17:1628. 10.3390/ijerph17051628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rojas-Valverde D, Sánchez-Ureña B, Crowe J, et al. Exertional rhabdomyolysis and acute kidney injury in endurance sports: a systematic review. Eur J Sport Sci 2021;21:261–74. 10.1080/17461391.2020.1746837 [DOI] [PubMed] [Google Scholar]
- 4.Barros ES, Nascimento DC, Prestes J, et al. Acute and chronic effects of endurance running on inflammatory markers: a systematic review. Front Physiol;8. 10.3389/fphys.2017.00779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patil HR, O’Keefe JH, Lavie CJ, et al. Cardiovascular damage resulting from chronic excessive endurance exercise. Mo Med 2012;109:312–21. [PMC free article] [PubMed] [Google Scholar]
- 6.Abdulla J, Nielsen JR. Is the risk of atrial fibrillation higher in athletes than in the general population? A systematic review and meta-analysis. Europace 2009;11:1156–9. 10.1093/europace/eup197 [DOI] [PubMed] [Google Scholar]
- 7.Ferenbach DA, Bonventre JV. Acute kidney injury and chronic kidney disease: from the laboratory to the clinic. Nephrol Ther 2016;12 Suppl 1:S41–8. 10.1016/j.nephro.2016.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoffman MD, Krishnan E. Health and exercise-related medical issues among 1,212 ultramarathon runners: baseline findings from the Ultrarunners longitudinal tracking (ultra) study. PLoS One 2014;9:e83867. 10.1371/journal.pone.0083867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tiller NB, Stewart GM, Illidi CR, et al. Exercise is medicine? the cardiorespiratory implications of Ultra-marathon. Curr Sports Med Rep 2020;19:290–7. 10.1249/JSR.0000000000000738 [DOI] [PubMed] [Google Scholar]
- 10.Tiller NB. Pulmonary and respiratory muscle function in response to marathon and Ultra-Marathon running: a review. Sports Med 2019;49:1031–41. 10.1007/s40279-019-01105-w [DOI] [PMC free article] [PubMed] [Google Scholar]


