Abstract
Although pandemics are rare, planning and preparation for responding to them plays a crucial role in preventing their spread. The management and control of pandemics such as COVID-19 relies heavily on a country's health capacity. Measuring vulnerability to pandemics in geographical areas could potentially delay a pandemic's exponential growth and reduce the number of cases, which would alleviate the disease impact on communities and the health care sector. The aim of this study is to generate an area-level COVID-19 Pandemic Vulnerability Index (CPVI) and to assess its correlation with COVID-19 cases. Data were collected for Local Government Areas (LGAs) across Australia from different sources including Australia Bureau of Statistics, Australian Institute of Health and Welfare, and General Transit Feed Specification. Based on recent official reports about the COVID-19 outbreak, 18 factors were identified as influencing vulnerability to the disease within LGAs. Using factor analysis, four latent factors were identified and named as sociodemographic, medical conditions, transportation, and land use. Predicted factor scores were summed to generate a CPVI for each LGA. The CPVI was evaluated by correlating with confirmed cases of COVID-19 standardised by adult population in New South Wales and Victoria, the two Australian states with the highest numbers of confirmed cases. There was a statistically significant correlation between the CPVI and COVID-19 in New South Wales (r = 0.49) and Victoria (r = 0.48). LGAs scoring higher on the CPVI also had a higher absolute number of cases. The CPVI could be used by policymakers to identify at-risk areas and to develop preparedness and response plans to help mitigate the spread of COVID-19 and future pandemics.
1. Introduction
The coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome whose spread, and reach has been declared a pandemic by the World Health Organization (WHO) (WHO 2020). As a result of COVID-19, many cities around the world have experienced a large-scale disaster, causing significant loss of lives and resulting in substantial social and economic impacts (Ahmar and del Val 2020; Nicola et al., 2020). At the time of writing, COVID-19 has spread from China to 29 countries across the world and reached Australia on January 25, 2020. The total number of new cases initially grew steeply in Australia and then stabilised to about 350 per day around 22 March, and started dropping at the beginning of April to about 25 per day by April 13 (DoH, 2020). As at the May 3, 2020, a total of 6711 cases had been reported in Australia, with the highest number being in New South Wales (NSW) with 2,926, followed by Victoria with 1344 confirmed cases.
Although pandemics such as the influenza pandemic, Severe acute respiratory syndrome (SARS), the Middle East respiratory syndrome (MERS), and COVID-19, do not occur very often, planning and preparation of appropriate responses play an essential role in preventing or minimising their spread. Preparedness plans and strategies enhance the capability of local governments to overcome the impacts of pandemics through different approaches (Garoon and Duggan 2008; Gilbert et al., 2020). At this stage, nonpharmaceutical interventions (NPIs) are the most effective interventions to slow the transmission of pandemics. After the influenza pandemic, WHO (WHO 2006) recommended nonpharmaceutical public health interventions to contain infection, delay spread, and reduce the impact of pandemic disease. NPIs are also known as a community mitigation strategy, and includes a combination of personal protective measures, community measures, and environmental factors. According to Hilfiker et al. (2018), the conceptual framework of NPIs is based on the early and targeted application of several nonpharmaceutical measures that must be identified earlier than the spread of pandemic waves in the community.
Some groups in the population are more vulnerable to pandemics than others. Mitigating disease severity for vulnerable communities and people based on their age, health conditions and neighbourhood environment could be a primary goal for targeted interventions to lessen the risk of pandemics. Since human-to-human transmission has occurred among close interpersonal contacts, identifying measures that help to prevent or reduce transmission must be implemented, especially among aged populations who experience higher risk of infection (Balica et al., 2012; Li et al., 2020). Accordingly, an index that pre-emptively measures the vulnerability of different communities and helps delay the exponential growth of the disease, reduces the pandemic peak, and decreases the number of incidents, may be a critical tool in preventing future pandemics.
A variety of indexes have been developed to measure different levels of disaster vulnerably at various geographic and population scales (Tate 2012). Although previous studies have measured the influence of urbanization (Acharya and Porwal 2020) and travel time to urban areas (Macharia et al., 2020), none to date appear to have yet considered the behavioural and built environment features of urban and transport factors. Hence, this study introduces and evaluates a novel COVID-19 Pandemic Vulnerability Index (CPVI) to assess the multifactorial vulnerability of areas to pandemics across four domains: sociodemographic, premedical conditions, transportation, and land use.
2. Factors associated with pandemic vulnerability
Since the outbreak of COVID-19 in China, scientific research has identified different factors that have influenced the spread of this pandemic in different communities. Based on the pandemic features of the COVID-19 disease, all individuals are susceptible to infection (WHO 2020). However, recent research reveals several factors that markedly increase the risk of infection.
Based on cases confirmed by WHO, most are people aged 30–69 years, while the infection rate in persons below 18 years is moderately low. The mortality rate also increases with age, with the highest mortality among individuals over 80 years of age (21.9%) (WHO 2020). An investigation of inpatient adults with confirmed COVID-19 cases and those who had been discharged or had died by January 2020 in Wuhan, China indicated that the risk of death in hospital increases with age in adults (Zhou et al., 2020). Moreover, according to WHO (2020), the high mortality rate of decedents who reported “retiree” as their occupation confirms the high risk of mortality for seniors.
According to published records, families have been recognized as one of the most important sources of human-to-human transmission of the COVID-19 virus, while the secondary attack rate by household contacts has been found to be around 8%.: this may indicate that individuals living in larger households are at greater risk than their counterparts in smaller households (Cho 2020).
Community transmission increases the rate of spread of infected individuals. Transportation links and hubs and human mobility are another important source of pandemic transmission. Previous studies examining the influenza pandemic indicated that more dense areas in terms of public transport infrastructure could be an influential factor for the transmission of contagious diseases (Cooley et al., 2011; Zhang et al., 2015).
Patients with underlying conditions such as hypertension, diabetes, cardiovascular disease, chronic respiratory disease, and cancer are at high risk of severe outcomes for COVID-19 (Wang et al., 2020). Findings from a study conducted by Zhou et al. (2020) in Wuhan, China, revealed that of 191 patients hospitalized, 48% had a comorbidity, with hypertension being the most common (30% of patients), followed by diabetes (19% of patients) and coronary heart disease (8% of patients).
2.1. Vulnerability measures
Vulnerability indices typically assess characteristics such as sociodemographic and pre-existing medical conditions to identify vulnerable populations (Chau et al., 2014). Previous approaches, such as those discussed below, have defined different variables or domains derived from a deductive methodology (Yoon 2012), then combined them into a score which is a representative measure of the overall vulnerability of each geographic unit (Cutter et al., 2012).
2.2. Infectious disease vulnerability index (IDVI)
Moore et al. (2016) created an index for identifying potentially vulnerable countries and then ranked countries by their overall vulnerability score. They developed an infectious disease vulnerability index (IDVI) which comprised seven factors relating to demographics, health care, public health, disease dynamics, domestic and international politics, and economics.
2.3. Social vulnerability index (SVI)
The SVI (Flanagan et al., 2011) measures the resilience of communities when confronted by external stresses on human health, such as natural or human-caused disasters, or disease outbreaks. According to the SVI, the extent to which a community responds to, and recovers from, a disaster decreases human suffering and reduces post-disaster costs to society. Flanagan et al. (2011) developed the SVI from 15 census variables at the census tract level, Unites States. Variables used in the index were categorised under four main domains including socioeconomic status (Cutter et al., 2003; Brodie et al., 2006), household composition and disability (Madrid et al., 2006; Martin et al., 2006), minority status and language (Elliott and Pais 2006; Peguero 2006; Bolin and Kurtz 2018), housing and transportation (Daley et al., 2005, Donner 2007).
2.4. Epidemic risk index (ERI)
The ERI (Poljanšek et al., 2018) measures the different combined effects of each country's epidemic transmission risk, infrastructure, vulnerability, and coping capacity. According to this index, vulnerability describes how simply and how severely people can be affected by infectious hazards. Hence, the vulnerability dimensions illustrate health vulnerability due to the social, economic, ecological, movement, behaviour and hazard attributes of the country.
Despite their methodological differences, the above-mentioned indices provide a composite score for the quantification of factors contributing to a population's susceptibility, readiness to respond, and ability to recover from, hazards. In terms of pandemic diseases, the creation of an index to measure the vulnerability of different regions to the virus may assist policymakers to develop their coping capacity and enduring capabilities to effectively prevent, detect, and respond to disease threats at the earliest stage. The following section presents a method for the development of an area-level COVID-19 Pandemic Vulnerability Index (CPVI) which incorporates data on sociodemographic characteristics, medical conditions, transportation access, and land use.
3. Methods
This study introduces a COVID-19 Pandemic Vulnerability Index (CPVI) that adopts a deductive method and combines individual and environmental vulnerability. Its development involved the selection of relevant vulnerability domains and the assessment of geographical vulnerability in Australia's Local Government Areas (LGAs). The CPVI proposed in this research, expands existing vulnerability indices by including land use and transportation measures. The rationale for the vulnerability domains used in the current investigation is described in the following sections.
3.1. Study areas and datasets
The CPVI was calculated for all 563 Local Government Areas (LGAs) in Australia, covering the whole of the country without gaps or overlaps. LGAs have an average population of 45,000 people and cover an average area of 2500 square kilometres.
3.2. Exposure variable (CPVI components)
Table 1 shows the sub-domains and sources of data used to create the CPVI, and the sections that follow describe the rationale for inclusion of each sub-domain and the relevant variables.
Table 1.
COVID-19 pandemic vulnerability index (CPVI) and data sources.
| Domains | Factor | Measure | Source of database |
|---|---|---|---|
| Socio-demographic | Age | Distribution of age categories above 65 years | Australian Bureau of Statistics (ABS) a,b,c, 2016 |
| Household size | Number of people in household | ||
| IRSD | SEIFA Australia - Index of Relative Socio-Economic Disadvantage (IRSD) | ||
| Medical | Diabetes | Share of diabetes related deaths | Australian Institute of Health and Welfare (AIHW), 2013–2017 d |
| Cardiovascular disease | Share of cardiovascular disease-related deaths | ||
| Chronic respiratory | Share of chronic respiratory disease-related deaths | ||
| Cancer | Share of all cancer-related deaths | ||
| Flu/Pneumonia | Share of flu/pneumonia-related deaths | ||
| Transportation | Local transportation | Transit stop density (number of stops to LGA area) | General Transit Feed Specification (GTFS), latest feed as of April 18, 2020 e |
| Travel Behaviour | Share of public transit use for work trips | Australian Bureau of Statistics (ABS)b, 2014–2017 | |
| Land use | Population density | Population per sq.km | Australian Bureau of Statistics (ABS) f, 2016 |
| Commercial areas | Proportion of commercial areas in each LGA | ||
| Education centres | Proportion of educational areas in each LGA | ||
| Medical services | Proportion of medical areas in each LGA |
Australian Bureau of Statistics (ABS, 2018a, ABS, 2018b), Population and people, Local Government Areas, 2011–2018.
Australian Bureau of Statistics (ABS, 2018a, ABS, 2018b), Family and Community, Local Government Areas, 2011, 2018.
Australian Bureau of Statistics (ABS, 2018a, ABS, 2018b), Economy and Industry, Local Government Areas, 2011, 2018.
Australian Institute of Health and Welfare (AIHW 2017), Local Government Areas 2013–2017.
General Transit Feed Specification (GTFS) data for New South Wales, Victoria, South Australia, Western Australia, Northern Territory, Tasmania and Australian Capital Territory from www.transitfeeds.com, and GTFS and railway stops data for Queensland from www.data.qld.gov.au. Stops are aggregated based on the stop name to avoid duplications.
Australian Bureau of Statistics (ABS 2016), Census of Population and Housing.
3.3. Socio-demographic
Several demographic factors impact the extent of vulnerability of people to pandemic diseases. The WHO has identified older people as more likely to become severely affected by infectious diseases. Hence in the current study, elderly people were categorised into five categories: 65 to 69, 70 to 74, 75 to 79, 80 to 84 and more than 85 years old. Data for age categories obtained from the Australian Bureau of Statistics (ABS, 2018a, ABS, 2018b) captured the number and percentage of people in each LGA. Living in a household with other people, increased the risk of infection. Hence, average household size was used as one of the sociodemographic measures. In order to locally contextualise the index, we included the Index of Relative Socio-economic Disadvantage (IRSD), as another sociodemographic measure. IRSD is a general socio-economic index that summarises a range of information about the economic and social conditions of people and households within an area. The Australian Medical Association (AMA) has recently reported a higher proportion of COVID-19 cases were associated with lower IRSD scores in Local Government Areas (Talevski et al., 2021).
3.4. Medical conditions
We obtained the number of deaths in each LGA resulting from five major diseases that are associated with greater vulnerability to a pandemic infectious disease, including any type of cancer, diabetes, major cardiovascular disease, respiratory disease, and influenza/pneumonia. Raw values obtained from Australian Institute of Health and Welfare (AIHW 2017), were then transformed into the percentage of deaths for each disease relative to total deaths in each LGA.
3.5. Transportation
Recent research emphasizes the crucial role of exposure on public transit in the outbreak of the pandemic (Sohrabi et al., 2020). Accordingly, we extracted the share of public transit to work trips as well as geospatial data geolocating transit stop and/or station density in LGAs. Share of transit use was obtained from the ABS (ABS, 2018a, ABS, 2018b) and number of stops and stations were collected from Open Street Map (GFTS 2020). We hypothesized that areas with greater levels of access to public transit and higher transit stop densities are more likely to be vulnerable to the spread of pandemics due to higher levels of transportation activities and movement of people (Morrow 1999; Moore et al., 2016).
Land use.
Since areas with a higher population density are more vulnerable to infectious disease (Moore et al., 2016), we calculated the population density of each LGA, and hypothesized that LGAs with higher densities would be more vulnerable to the spread of pandemics. We also calculated the proportion of land allocated to commercial education and medical uses in each LGA. This was on the assumption that areas with higher density have a higher proportion of these land uses.
Table 1 shows the four domains included in the CPVI. The sociodemographic category contains the distribution of age categories above 65 years at five-year intervals, household size and index of socio-economic disadvantage (IRSD). Premedical conditions include five groups of serious underlying medical conditions, including cancer, diabetes, major cardiovascular, respiratory disease, and influenza/pneumonia. The transportation domain contains the transit stop density and percentage of use of public transit for work trips. Finally, the land use category, population density and proportion of commercial, education and medical land uses were considered for LGAs. The datasets were collected from different sources, as indicated in Table 1.
Table 2 shows the descriptive statistics for LGAs for each of the factors comprising the CPVI.
Table 2.
Statistics describing the COVID-19 Pandemic vulnerability domains for all Local Government Areas (n = 563) in Australia.
| Measurements (Unit) | Mean | S.D. | Minimum | Maximum |
|---|---|---|---|---|
| Sociodemographic | ||||
| Share of adults 65–69 years old | 5.52 | 2.23 | 0.00 | 15.10 |
| Share of adults 70–74 years old | 4.06 | 1.84 | 0.00 | 9.90 |
| Share of adults 75–79 years old | 2.84 | 1.35 | 0.00 | 7.50 |
| Share of adults 80–84 years old | 1.88 | 0.98 | 0.00 | 5.40 |
| Share of adults 85 years or older and over | 1.84 | 1.14 | 0.00 | 5.60 |
| Average of household size (No. of persons in a household) | 2.44 | 0.61 | 0.00 | 5.30 |
| IRSD1 using the score for each LGA | 956.48 | 109.18 | 404.00 | 1123.00 |
| Medical | ||||
| Share of total deaths by cancer deaths | 16.50 | 7.27 | 0.00 | 34.09 |
| Share of total deaths by diabetes deaths | 19.49 | 8.03 | 0.00 | 37.78 |
| Share of total death by major cardio disease | 0.19 | 0.64 | 0.00 | 7.78 |
| Share of total deaths by respiratory disease | 1.56 | 1.32 | 0.00 | 7.45 |
| Share of total deaths by influenza/pneumonia | 3.15 | 2.52 | 0.00 | 16.99 |
| Transportation | ||||
| Public transit stops density (No. of stops divided by LGA area) | 2.22 | 5.13 | 0.00 | 26.63 |
| Share of public transit trips to work | 5.22 | 8.14 | 0.00 | 55.26 |
| Land use factors | ||||
| Population density (per sq. kilometre) | 48.95 | 145.52 | 0.00 | 958.50 |
| Proportion of commercial areas | 0.98 | 3.31 | 0.00 | 41.36 |
| Proportion of education centre areas | 0.59 | 1.39 | 0.00 | 10.93 |
| Proportion of medical service areas | 0.09 | 0.40 | 0.00 | 5.83 |
1 A low IRSD score indicates relatively greater disadvantage in general. IRSD is a combined measure of 18 variables including percentage of dwellings with no internet connection, labourers, people with no post-school qualifications, people earning incomes between $13,000 and $20,799, households renting from government or community organizations, people unemployed, one parent families with dependent offspring, households paying less than $120 per week for rent, people with a long-term health condition or disability, occupied private dwellings with no car, aboriginal and/or Torres Strait Islander peoples, occupied private dwellings requiring one or more extra bedrooms, people aged 15 years and over who are separated or divorced, employed people classified as machinery operators and drivers, people aged 15 years and over who did not go to school, employed people classified as low skill community and personal service workers, and people who do not speak English well.
3.6. Outcome variable (COVID-19 confirmed cases in New South Wales and Victoria)
Confirmed counts of COVID-19 cases divided by the adult population aged 18 years old and older in each LGA in the states of New South Wales (NSW) and Victoria were used as the outcome variable in this study. COVID-19 case data were obtained from each state's Department of Health (DHHS 2020; NSW 2020). As of May 3rd, 2020, the total number of confirmed cases in NSW was 2926, with an average of 22.6 per LGA, range 0–181. In Victoria at the corresponding timepoint, the total number of confirmed cases was 1344, with an average of 19.5 per LGA, range 0–89. Adult population data were obtained from the 2016 national census (ABS 2016).
3.7. Data analysis
To develop the CPVI, analyses were conducted in five steps. First, we used Confirmatory factor analysis (CFA) within a structural equation modelling (path analysis) framework. CFA is a common approach in generating composite indices (OECD 2008; Cappon and Laughlin 2013; Kusurkar et al., 2013). CFA allows for the investigation of associations between latent and observed variables prior to specifying theory-derived models (Mueller and Hancock 2001). Using Amos v.25, we defined four latent factors for each of the four vulnerability domains of sociodemographic, medical, transport and urban. Second, after examining the 18 variables comprising the four defined latent factors, we used Principal Component Analysis (PCA) with Varimax rotation to predict scores for each latent factor. Third, we investigated the correlation and potential multicollinearity between the predicted latent factors using pairwise correlation analysis and Variance Inflation Factors (VIFs). Thereafter, in the next step, the predicted latent factors were combined to generate the COVID-19 Pandemic Vulnerability Index (CPVI). Since there was no clear justification for different weightings, we equally weighted each latent factor (Daras et al., 2019). In the final step, generated index, was assessed using COVID-19 cases data from Victoria and NSW as the most affected states in Australia.
4. Results
4.1. COVID-19 pandemic vulnerability index (CPVI) calculation
CFA was used to examine whether the 18 explanatory variables are statistically significant under a given latent factor. Standardised regression weights from the CFA are presented in Table 3 (see Fig. 2 in the supplementary document for the path diagram). As shown in the table, all the variables were statistically significant.
Table 3.
Standardised regression weight estimates for confirmatory factor analysis with four latent factors for all Local Government Areas (n = 563) in Australia.
| Variables | Latent Factors | Estimate |
|---|---|---|
| Share of adults 65–69 years old | Sociodemographic | 0.85 |
| Share of adults 70–74 years old | Sociodemographic | 0.92 |
| Share of adults 75–79 years old | Sociodemographic | 0.98 |
| Share of adults 80–84 years old | Sociodemographic | 0.90 |
| Share of adults 85 years and over | Sociodemographic | 0.80 |
| Average of household size2 | Sociodemographic | 0.12 |
| IRSD scores | Sociodemographic | 0.37 |
| Share of total deaths by cancer deaths | Medical | 0.68 |
| Share of total death by major cardio disease | Medical | 1.05 |
| Share of total deaths by respiratory disease | Medical | 0.13 |
| Share of total deaths by influenza/pneumonia | Medical | 0.32 |
| Share of total deaths by diabetes deaths | Medical | 0.42 |
| Share of public transit trips to work | Transport | 0.77 |
| Public transit stops density | Transport | 1.02 |
| Population density (per sq. kilometre) | Urban | 0.12 |
| Proportion of commercial areas | Urban | 0.57 |
| Proportion of education centre areas | Urban | 0.92 |
| Proportion of medical service areas | Urban | 0.60 |
Bold figures are significant at 0.05 level.
1 Average household size was reversed to be in the same direction as other variables under sociodemographic latent factor.
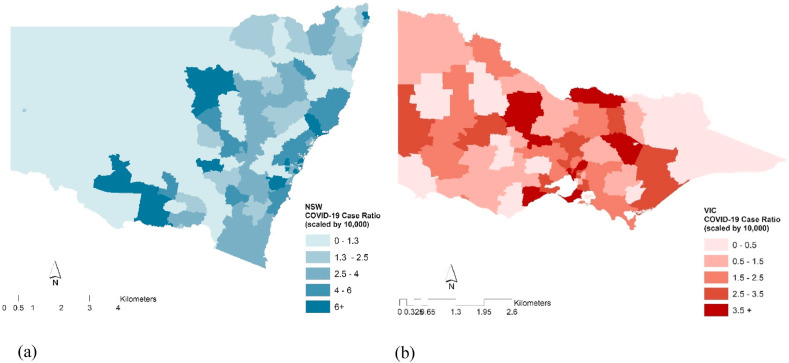
Fig. 2.
Cumulative numbers of COVID-19 confirmed cases by LGAs (as of May 3, 2020) in NSW (a) and Victoria (a), Australia.
Table 4 presents summary statistics for the predicted factors (see Fig. 1 in the supplementary document for the distribution maps of predicted latent factors). The correlation between the two latent factors of Urban and Transport was 0.73, which although considered a strong association, was not sufficiently large to result in collinearity (Tabachnick et al., 2007). In addition, VIFs for all models were less than 3.0, suggesting that multicollinearity was not a cause for concern (Allison 1999). (results of correlation and VIFs are provided in the supplementary document, see Table 2, Table 3).
Table 4.
Descriptive statistics of COVID-19 confirmed cases as of May 3, 2020.a
| COVID-19 Confirmed Cases Ratiob | Mean | Std. | Minimum | Maximum |
|---|---|---|---|---|
| New South Walesc | 4.99 | 4.66 | 0.56 | 33.00 |
| Victoriad | 2.59 | 1.78 | 0.27 | 9.84 |
| Overall | 4.00 | 3.92 | 0.27 | 33.00 |
total number of 161 LGAs from which 94 from New South Wales and 67 from Victoria.
Number of cases divided by adult population in each LGA to calculate case ratio. Figures are scaled by 10,000.
New South Wales Government, Department of Health (https://www.health.nsw.gov.au).
Victoria State Government, Department of Health and Human Services (https://www.dhhs.vic.gov.au).
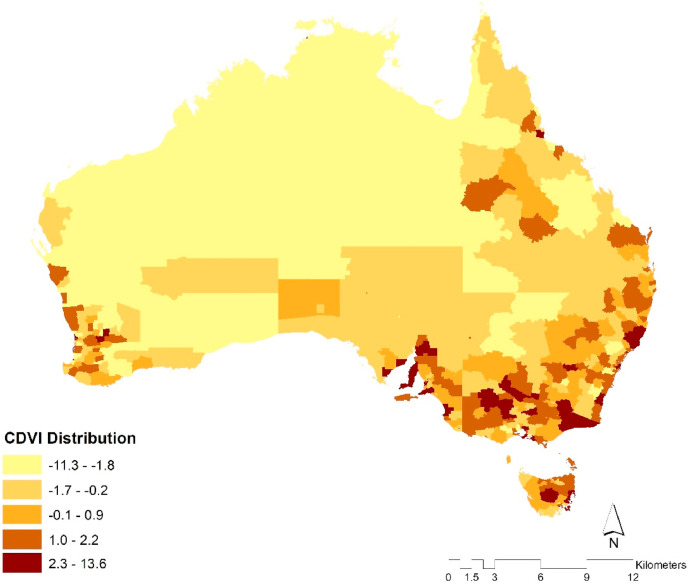
Fig. 1.
Distribution of the COVID-19 pandemic vulnerability index across all local government areas (n = 563) in Australia.
Summary statistics of the predicted latent factors for all LGAs are provided in the supplementary document (see Table 1). The four latent factors were summed to create the CPVI. The predicted index for Australia had a mean value of 0.18 (SD 3.61) and ranged from −11.28 to 13.58. Fig. 1 shows the distribution of CPVI across all LGAs in Australia. As expected, the more populated urban areas in the east and south-east, where three large metropolitan areas (Brisbane, Sydney, and Melbourne) are located, are categorised among the higher percentiles. The same occurs in the south-west where Perth, another metropolitan area with a smaller population, is located. More specifically, areas with higher value of CPVI are more vulnerable areas for pandemic risk.
4.2. CPVI assessment
In order to evaluate and assess the CPVI, we correlated with a COVID-19 case ratio calculated for LGAs in NSW and Victoria, the most affected states in Australia (Table 4). Table 4 provides the descriptive statistics of confirmed cases in those states.
Fig. 2 illustrates the cumulative numbers of COVID-19 confirmed cases by LGAs in NSW and Victoria. In each state, LGAs with higher numbers of cases are located around the metropolitan areas of Melbourne and Sydney.
In order to evaluate the performance of the CPVI, we examined the association between the ratio of COVID-19 confirmed cases and CPVI values in Victoria and NSW using a correlation analysis (Flanagan et al., 2011; Chau et al., 2014). Analysis results, showed that there was a statistically significant correlation between the CPVI and COVID-19 in New South Wales (r = 0.49, p < 001) and Victoria (r = 0.48, p < .001).
5. Discussion
Based on previous research, this study developed a CPVI to measure the vulnerability of LAGs to COVID-19 pandemic in Australia. As Chau et al. (2014) state, vulnerability does not only take account of natural disasters but also health hazards and emergencies. The findings of this present study show that LGAs with CPVIs above average are mostly located around main metropolitan areas. The assessment of the CPVI with COVID-19 confirmed cases in Victoria and NSW, indicated a statistically significant relationship. These findings will provide useful information for stakeholders involved in emergency preparedness of the most vulnerable residential areas and/or populations (Gusmano et al., 2006) in terms of planning and implementing future interventions. For example, to prevent transmission, additional preventive strategies may be needed for residents in high rise buildings where there are shared facilities and access and egress is by elevators. This is likely to be even more important in overcrowded apartment complexes such as those occupied by lower socioeconomic residents (Adlakha and Sallis 2020; Maroko et al., 2020).
There are strengths and weaknesses related to the CPVI developed in this study. First, the CPVI is applicable to diverse urban areas based on a flexible calculation technique. If data are available for different geographical units, standardised values can be readily calculated and ranked accordingly. Furthermore, the use of routinely available official statistics in generating the index enables continual, constant updating. This CPVI measures the spatial location of older populations and those with pre-existing health conditions that puts them at greater risk of infection and combines this with environmental factors likely to increase risk of exposure to infection: population density, land use, and transit access at the LGA level. Hence, this approach with the same set of variables may be applied to different geographic locations and smaller scales, which permits a comparison of the relative vulnerability of areas to specific health hazards.
The study highlights areas where there is a need for greater efforts to introduce targeted interventions. Not only in terms of the demographics of at-risk population groups, but also due to the environment in which they live. For example, higher density areas with access to more destinations and higher levels of amenities and public transit access are likely to increase risk because there are greater numbers of people spending more time circulating in these areas more often than people living in lower density neighbourhoods with no local amenities. Although there is no evidence that higher density development per se, is associated with the transition of COVID-19, as some of the most dense cities in the world have managed the risk COVID-19 using strict and rapid public health interventions (Adlakha and Sallis 2020; Jinjarak et al., 2020).
There are several strengths and limitations to our study. However, we believe this is the first composite index of area vulnerability of COVID-19 developed for Australia. The proposed index drives underlying socioeconomic and medical as well as urban and transport factors at a spatial level that is extremely useful for local policy planning. This study was limited by the unavailability of data at a smaller spatial scale both for components of the CPVI and COVID-19 confirmed cases. While statistics for finer geographical units may not be available in the public domain, the government could make them available to researchers in order to enable the development of a more accurate CPVI. Alternatively, confronted with a future pandemic, governments could adopt the methodology here, and use more fine-grained area-level data to identify areas of risk to mobilise preventive interventions. Identifying vulnerable areas at finer levels, gives governments more flexibility in applying interventions to hotspot areas at smaller scales. Besides, when aggregating data to larger areal units, modifiable areal unit problem (MAUP) may occur, which can lead to larger estimates of the correlation coefficient (Charlton et al., 2009, Keeler and Emch, 2017). Thus applying analysis to a smaller geographical scale may decrease the chance of MAUP occurring. Our use of confirmed COVID-19 case ratios to assess the predictive validity of the CPVI was a limitation, as case-ratio of infectious disease reflects testing access and uptake and hence contain bias. Arguably, a less biased approach would have been to use deaths and hospitalisations as these are not dependent on testing and uptake: however, there was insufficient data for these vital statistics available for this study (Daras et al., 2021). Nevertheless, their use is recommended for future research data permitting. In addition, conducting our analyses at an aggregated level might have increased the risk of an ecological fallacy, as the area-level associations observed in this study may not have been present (or may have been different) if examined at smaller scales. Hence, future studies should also consider using individual level data if available.
6. Conclusion
The present study offers a flexible pandemic vulnerability index that is adaptable to local spatial contexts, and that could be applied elsewhere to identify at risk populations requiring early and targeted intervention. Nevertheless, in terms of global application, it is acknowledged that the availability of data is always a barrier to the production of indices in cities in some countries. Furthermore, because of contextual differences in cities, alternative domain-specific variables may be needed. For example, in cities with overcrowded (and/or informal) housing the CPVI might be especially useful in highlighting the combinations of individual and environmental factors that increases risk of both exposure and infection. Moreover, some of the factors used in the CPVI might be different depending on the pathogen of a given pandemic, including its primary modes of transmission and clinical/epidemiologic features. The relative scores of each LGA's vulnerability to pandemic disease highlight the areas of highest need and risk, which may inform policymakers and service providers in their efforts to plan and prioritize emergency preparedness, early intervention, and relief measures. The use of the CPVI and similar indexes may also be a useful tool for mapping vulnerable areas and allocating adequate medical and associated equipment, resources, and staff well in advance. Indexes like the CPVI may also help governments and communities anticipate the potential threat to their communities and to prepare accordingly, including building local social capital that will enable the community to respond promptly to potential threats.
Acknowledgment
Funding declaration: TS was supported by the Australian Prevention Partnership Centre #9100003, and BGC by an NHMRC Senior Principal Research Fellowship GNT1107672.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.healthplace.2021.102629.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Abs . vol. 2016. Australian Bureau of Statistics; Australia: 2016. (Census of Population and Housing: Mesh Block Counts). [Google Scholar]
- Abs . Australian Bureau of Statistics; 2018. Local Government Area, 2011-2018. [Google Scholar]
- Abs . Australian Bureau of Statistics; 2018. Local Government Areas, 2011, 2018. [Google Scholar]
- Acharya R., Porwal A. A vulnerability index for the management of and response to the COVID-19 epidemic in India: an ecological study. 2020;8(9):e1142–e1151. doi: 10.1016/S2214-109X(20)30300-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adlakha D., Sallis J.F. Activity-friendly neighbourhoods can benefit Non-communicable and infectious diseases. Cities and Health. 2020:1–5. https://doi-org.ezproxy.lib.rmit.edu.au/10.1080/23748834.2020.1783479 [Google Scholar]
- Ahmar A.S., Del Val E.B. Sutte ARIMA: Short-term forecasting method, a case: Covid-19 and stock market in Spain. Sci. Total Environ. 2020;729:1–6. doi: 10.1016/j.scitotenv.2020.138883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aihw . Australian Institute of Health and Welfare; 2017. Mortality over Regions and Time (MORT) Books, Local Government Areas, 2013-2017. [Google Scholar]
- Allison P.D. SAS Publishing; Cary, N.C., United States: 1999. Logistic Regression Using the SAS System: Theory and Application. [Google Scholar]
- Balica S.F., Wright N.G., Van der Meulen F. A flood vulnerability index for coastal cities and its use in assessing climate change impacts. Nat. Hazards. 2012;64(1):73–105. [Google Scholar]
- Bolin B., Kurtz L.C. Handbook of Disaster Research. Springer; 2018. Race, class, ethnicity, and disaster vulnerability; pp. 181–203. [Google Scholar]
- Brodie M., Weltzien E., Altman D., Blendon R.J., Benson J.M. Experiences of hurricane katrina evacuees in houston shelters: implications for future planning. Am. J. Publ. Health. 2006;96(8):1402–1408. doi: 10.2105/AJPH.2005.084475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cappon P., Laughlin J. Canada’s Composite Learning Index: a path towards learning communities. 2013;59(4):505–519. [Google Scholar]
- Charlton M., Kitchin R., Thrift N. Elsevier; Oxford: 2009. Quantitative Data. International Encyclopedia of Human Geography; pp. 19–26. [Google Scholar]
- Chau P.H., Gusmano M.K., Cheng J.O., Cheung S.H., Woo J. Social vulnerability index for the older people-Hong Kong and New York City as examples. J. Urban Health. 2014;91(6):1048–1064. doi: 10.1007/s11524-014-9901-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho H.-W. A long journey back to normal life. Osong Public Health and Research Perspectives. 2020;11(2):65. doi: 10.24171/j.phrp.2020.11.2.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooley P., Brown S., Cajka J., Chasteen B., Ganapathi L., Grefenstette J., Hollingsworth C.R., Lee B.Y., Levine B., Wheaton W.D. The role of subway travel in an influenza epidemic: a New York City simulation. J. Urban Health. 2011;88(5):982. doi: 10.1007/s11524-011-9603-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutter S.L., Boruff B.J., Shirley W.L. Social vulnerability to environmental hazards. Soc. Sci. Q. 2003;84(2):242–261. [Google Scholar]
- Cutter S.L., Boruff B.J., Shirley W.L. Routledge; 2012. Social Vulnerability to Environmental Hazards. Hazards Vulnerability and Environmental Justice; pp. 143–160. [Google Scholar]
- Daley W.R., Brown S., Archer P., Kruger E., Jordan F., Batts D., Mallonee S. Risk of tornado-related death and injury in Oklahoma, May 3, 1999. Am. J. Epidemiol. 2005;161(12):1144–1150. doi: 10.1093/aje/kwi142. [DOI] [PubMed] [Google Scholar]
- Daras K., Alexiou A., Rose T.C., Buchan I., Taylor-Robinson D., Barr B. How Does Vulnerability to COVID-19 Vary between communities in England? Developing a small area vulnerability index (SAVI) J. Epidemiol. Community Health. 2021;75(8):729–734. doi: 10.1136/jech-2020-215227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daras K., Green M.A., Davies A., Barr B., Singleton A. Open data on health-related neighbourhood features in Great Britain. Scientific Data. 2019;6(1):1–10. doi: 10.1038/s41597-019-0114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DHHS . Department of Health and Human Services; Victoria, Australia: 2020. Coronavirus Update for Victoria. [Google Scholar]
- DoH . Department of Health, Australian Governement; 2020. Coronavirus (COVID-19) Current Situation and Case Numbers. [Google Scholar]
- Donner W.R. The political ecology of disaster: an analysis of factors influencing US tornado fatalities and injuries, 1998–2000. Demography. 2007;44(3):669–685. doi: 10.1353/dem.2007.0024. [DOI] [PubMed] [Google Scholar]
- Elliott J.R., Pais J. Race, class, and Hurricane Katrina: social differences in human responses to disaster. Soc. Sci. Res. 2006;35(2):295–321. [Google Scholar]
- Flanagan B.E., Gregory E.W., Hallisey E.J., Heitgerd J.L., Lewis B. A social vulnerability index for disaster management. J. Homel. Secur. Emerg. Manag. 2011;8(1):1–22. doi: 10.2202/1547-7355.1792. [DOI] [Google Scholar]
- Garoon J.P., Duggan P.S. Discourses of disease, discourses of disadvantage: a critical analysis of national pandemic influenza preparedness plans. Soc. Sci. Med. 2008;67(7):1133–1142. doi: 10.1016/j.socscimed.2008.06.020. [DOI] [PubMed] [Google Scholar]
- Gfts . 2020. General Transit Feed Specification (Gfts)https://gtfs.org [Google Scholar]
- Gilbert M., Pullano G., Pinotti F., Valdano E., Poletto C., Boëlle P.-Y., D'Ortenzio E., Yazdanpanah Y., Eholie S.P., Altmann M., Gutierrez B., Kraemer M.U.G., Colizza V. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. Lancet. 2020;395(10227):871–877. doi: 10.1016/S0140-6736(20)30411-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gusmano M., Rodwin V., Cantor M. Urban ecology of old age in New York City (NYC): helping vulnerable older persons. Final report to the New York Community Trust. 2006;11 [Google Scholar]
- Hilfiker R., Meichtry A., Eicher M., Balfe L.N., Knols R.H., Verra M.L., Taeymans J. Exercise and other non-pharmaceutical interventions for cancer-related fatigue in patients during or after cancer treatment: a systematic review incorporating an indirect-comparisons meta-analysis. Br. J. Sports Med. 2018;52(10):651–658. doi: 10.1136/bjsports-2016-096422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jinjarak Y., Ahmed R., Nair-Desai S., Xin W., Aizenman J. Vol. 4. National Bureau of Economic Research; 2020. Accounting for Global COVID-19 Diffusion Patterns, January-April 2020; pp. 515–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keeler C., Emch M., Quah S.R. International Encyclopedia of Public Health. second ed. Academic Press; Oxford: 2017. Geographic information systems (GIS) in public health; pp. 253–255. [Google Scholar]
- Kusurkar R., Ten Cate T.J., Vos C., Westers P., Croiset G.J. How motivation affects academic performance: a structural equation modelling analysis. Adv. Health Sci. Educ. 2013;18(1):57–69. doi: 10.1007/s10459-012-9354-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Ren R., Leung K.S., Lau E.H., Wong J.Y. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macharia P.M., Joseph N.K., Okiro E.A. A vulnerability index for COVID-19: spatial analysis at the subnational level in Kenya. BMJ Global Health. 2020;5(8):1–12. doi: 10.1136/bmjgh-2020-003014. e003014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madrid P.A., Grant R., Reilly M.J., Redlener N.B. Challenges in meeting immediate emotional needs: short-term impact of a major disaster on children’s mental health: building resiliency in the aftermath of Hurricane Katrina. Pediatrics: Off. J. Am. Acad. Pedi. 2006;117(4):448–453. doi: 10.1542/peds.2006-0099U. [DOI] [PubMed] [Google Scholar]
- Maroko A., Nash D., Pavilonis B.T. Vol. 97. 2020. Covid-19 and Inequity: a comparative spatial analysis of New York City and Chicago hot spots; pp. 461–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin S.D., Bush A.C., Lynch J.A. A national survey of terrorism preparedness training among pediatric, family practice, and emergency medicine programs. Pediatrics. 2006;118(3):e620–e626. doi: 10.1542/peds.2005-1875. [DOI] [PubMed] [Google Scholar]
- Moore M., Gelfeld B., Okunogbe A., Christopher P. Identifying future disease hot spots: infectious disease vulnerability index. Rand Health Quart. 2016;6(3):5. [PMC free article] [PubMed] [Google Scholar]
- Morrow B.H. Identifying and mapping community vulnerability. Disasters. 1999;23(1):1–18. doi: 10.1111/1467-7717.00102. [DOI] [PubMed] [Google Scholar]
- Mueller R.O., Hancock G.R. 2001. Factor analysis and latent structure, confirmatory. [Google Scholar]
- Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C., Agha M., Agha R. The socio-economic implications of the coronavirus and COVID-19 pandemic: a review. Int. J. Surg. 2020;78:185–193. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NSW . Department of Health; NSW, Australia: 2020. Latest COVID-19 Case Locations in NSW. [Google Scholar]
- OECD . OECD publishing; 2008. Handbook on Constructing Composite Indicators: Methodology and User Guide. [Google Scholar]
- Peguero A.A. Latino disaster vulnerability: the dissemination of hurricane mitigation information among Florida’s homeowners. Hisp. J. Behav. Sci. 2006;28(1):5–22. https://doi-org.ezproxy.lib.rmit.edu.au/10.1177/0739986305284012 [Google Scholar]
- Poljanšek K., Marin-Ferrer M., Vernaccini L., Messina L. EUROPEAN UNION (EU); 2018. Incorporating Epidemics Risk in the INFORM Global Risk Index. [Google Scholar]
- Sohrabi C., Alsafi Z., O’Neill N., Khan M., Kerwan A., Al-Jabir A., Iosifidis C., Agha R. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int. J. Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick B.G., Fidell L.S., Ullman J.B. Pearson Boston; MA: 2007. Using Multivariate Statistics. [Google Scholar]
- Talevski J., Bird S., Olsen S.B. Low socio-economic status and impact of COVID-19 in Victoria. 2021. https://insightplus.mja.com.au/2021/5/low-socio-economic-status-and-impact-of-covid-19-in-victoria/ from.
- Tate E. Social vulnerability indices: a comparative assessment using uncertainty and sensitivity analysis. Nat. Hazards. 2012;63(2):325–347. [Google Scholar]
- Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., Wang B., Xiang H., Cheng Z., Xiong Y. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. Jama. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Who Group, world health organization writing, nonpharmaceutical interventions for pandemic influenza, international measures. Emerg. Infect. Dis. 2006;12(1):81. doi: 10.3201/eid1201.051370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Who . World Health Organization; 2020. Report of the Who-china Joint Mission on Coronavirus Disease 2019 (Covid-19) [Google Scholar]
- Yoon D.K. Assessment of social vulnerability to natural disasters: a comparative study. Nat. Hazards. 2012;63(2):823–843. [Google Scholar]
- Zhang M., Meng R., Verbraeck A. Proceedings of the Conference on Summer Computer Simulation. 2015. Including public transportation into a large-scale agent-based model for epidemic prediction and control. [Google Scholar]
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X., Guan L., Wei Y., Li H., Wu X., Xu J., Tu S., Zhang Y., Chen H., Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.