Abstract
Objective
Quality of life (QOL) is a broad-ranging concept affecting an individual’s physical health, psychological state, social relationships, and relationship to their environment. Although the role of psychometrists in clinical neuropsychology is integral to the delivery of services, little is known about their QOL. The current study assessed psychometrists’ workload and aspects related to work QOL (e.g., physical and emotional exhaustion, social and work satisfaction).
Method
Psychometrists (N = 164) from 38 states completed a nationally distributed survey. Participants averaged eight years of experience, ~29% completed board certification, and worked primarily in general hospitals (~36%), academic medical centers (~21%), private practice (~15%), veterans/military hospitals (~13%), and rehabilitation hospitals (~12%).
Results
Respondents saw 5.6±2.4 (Mean±Standard Deviation) patients and spent 18.8±6.9 and 9.4±4.9 hours administering and scoring, respectively, per week. Although the majority of respondents felt satisfied with their work QOL, approximately 49% experienced emotional exhaustion, 42% experienced burnout, and 62% reported that fatigue interfered with work, family, or social life. Correlational analyses found a significant relationship between QOL variables and professional activities, particularly with time spent scoring. Additionally, patient load, time spent administering/scoring, and QOL factors varied depending on work setting.
Conclusion
The current study provides a novel characterization of psychometrists’ QOL. Specifically, the prevalence of emotional exhaustion and fatigue appears to be higher than in the general working population in the United States. In addition, these findings highlight the current variability of job responsibilities and QOL across work settings. Ongoing advocacy and practice adjustments for this field are indicated.
Keywords: Assessment, Professional issues, Quality of life
Introduction
Quality of life (QOL) is an important concept to understand given the growing evidence that shows how stress and burnout affects workplace productivity and efficiency, quality of patient care, and employee retention within healthcare systems (Duarte, Pinto-Gouveia, & Cruz, 2016; Wallace, Lemaire, & Ghali, 2009). The construct of QOL is multidimensional, involving a person’s physical, psychological, and sociocultural well-being. Moreover, two common factors related to QOL include fatigue and burnout, both of which are higher among certain medical professionals (e.g., physicians, nurses) relative to the general population (Shanafelt et al., 2012). However, little to no information is known about psychometrists’ workload, and prior research has yet to explore psychometrists’ work-related QOL.
Psychometrists are responsible for the administration and scoring of psychological and neuropsychological measures under the supervision of a trained clinical psychologist or neuropsychologist. A recent survey from Kippie and co workers (2019) provided data on 118 psychometrists in an effort to establish a better understanding of the common practices, job expectations, and compensation within the field. Responses indicated that most psychometrists see one (52.6%) or two patients (33.3%) per day, with varying lengths of time spent administering tests, ranging from 2–3 hours (geriatric), 3–4 hours (adult), and 4–5 hours (pediatric). Similar variability was seen for time spent scoring, ranging from 1–4 hours depending on the age of the patient population. All respondents’ responsibilities included administering and scoring tests, and nearly all recorded behavioral observations. In addition, the majority of respondents generated a table of scores, completed clerical duties, and provided training (Kippie et al., 2019).
Given the range of job expectations, the utility of psychometrists is clear and prior research highlights how beneficial psychometrists are to the field of neuropsychology. Approximately 55% of neuropsychologists work with a psychometrist (Sweet, Benson, Nelson, & Moberg, 2015), and settings that utilize psychometrists found a 79% increase in the number of patients evaluated and gross annual income compared to settings that did not (DeLuca & Putman, 1993). Nevertheless, a review of the literature surrounding psychometrists reveals a paucity of information pertaining to their prevalence and related training in the field.
Presently, there are approximately 423 board certified psychometrists in the United States and Canada (Board Certified Psychometrists, 2020). Similar to other certification processes, eligible candidates must complete several steps, including credentialing (e.g., a bachelor’s or master’s degree and 3000 or 2000 hours, respectively, of testing, scoring, and associated administrative experience under the supervision of a licensed psychologist or neuropsychologist), successful completion of the Certified Specialist in Psychometry examination (i.e., at or above the 70th percentile), and Continuing Education Units every two years (Board of Certified Psychometrists, 2020). Given the breadth and depth of requirements for board certification, one potential benefit to completing this process is the potential of higher compensation (Kippie et al., 2019). However, board certification is not a requirement despite the ongoing efforts to standardize the criteria (American Academy of Clinical Neuropsychology, 1999; Axelrod et al., 2000; Division 40 Task Force, 1989, 1991; Puente et al., 2006), and thus the actual number of psychometrists within the field is difficult to ascertain. Further, it is unclear whether obtaining board certification relates to psychometrists’ workload or perceived work QOL.
This study aims to provide the field of neuropsychology with an understanding of psychometrists’ QOL (e.g., fatigue, emotional exhaustion, and burnout), and to assess whether factors related to QOL are associated with workload (e.g., time spent administering measures, time spent scoring, etc.). The authors hypothesized that number of hours administering and scoring neuropsychological measures, would be negatively associated with overall work-related QOL (“I feel satisfied with my quality of life at work”), and positively associated with other factors related to work QOL (e.g., physical and emotional exhaustion). As a secondary exploratory aim, the authors characterized differences among day-to-day responsibilities and factors related to work QOL based on the current practice setting.
Method
The authors developed the current 27-item survey internally to obtain basic demographic information and professional and practice-related characteristics such as neuropsychological test administration and scoring practices (e.g., “estimated number of hours spent scoring per week”) from a sample of psychometrists. The survey also contained 11 Likert-scale items assessing factors related to QOL (for individual survey items see Supplementary material Appendix A). QOL factors were generated following a review of QOL and burnout measures utilized in different occupational and population settings (Easton & Van Laar, 2018; Rohland, Kruse, & Rohrer, 2004), and professional characteristics were obtained based on survey questions utilized in a similar sample (Kippie et al., 2019). Each QOL factor included in the current study was determined by the authors, which included neuropsychologists and psychometrists, with the goal of including questions that assessed both physical and emotional exhaustion, motivation, and effects on non-work related aspects such as social relationships and leisure activities. Although the survey was not validated (see “Limitations” section), the questions included had face validity and were used primarily for descriptive purposes. As such, the resulting QOL data did not require scoring, nor did the authors combine responses to generate summative scores. In addition, a subset of participants responded to an optional open-ended question in order to contextualize their responses and provide any additional information not directly addressed in the survey.
Recruitment
The authors obtained expedited approval from the West Virginia University Institutional Review Board prior to the commencement of this study. The authors disseminated the survey link across various clinical and professional listservs for neuropsychologists (e.g., NPSYCH) and discussion boards/forums available to psychometrist members (e.g., National Association of Psychometrists and Board Certified Psychometrists). In addition, the authors distributed the survey to colleagues who were asked to forward it to psychometrists. We offered no incentives for participation.
Data Analysis
Descriptive information & correlations: The authors analyzed data with SPSS, version 26. Descriptive statistics characterized the study sample and findings for each survey item. Spearman correlations examined the associations between factors related to QOL and psychometrists’ workload (i.e., the number of hours administering neuropsychological measures and the number of hours scoring). The authors chose Spearman rank correlations because ordinal data was acquired when assessing QOL (i.e., Likert scale). Multiple comparisons were corrected by Holm’s Sequential Bonferroni Procedure (Holm, 1979). Additionally, in order to better understand the participants’ perception of QOL, the authors sorted open-ended responses into thematic categories independently identified from the responses by two post-doctoral neuropsychology fellows.
Following descriptive statistics, a total of 26 respondents were removed when conducting group comparison analyses, outlined as follows. Respondents were removed if they reported working in multiple work settings (n = 14), did not report a work setting (n = 1), or the setting did not comprise a large enough sample for analyses (e.g., psychiatric hospital = 7, “other” = 4).
Work setting & professional activities: The authors ran two one-way ANOVAs to examine the effect of different work settings on (a) time spent administering and (b) time spent scoring. There was one independent variable with five levels (i.e., general hospital, private practice, academic medical center, VAMC, and rehabilitation hospital) and two dependent variables as stated previously. Assumptions of normality and homogeneity were met. Statistical significance at the group level was based on p < .05 and Bonferroni post hoc pairwise comparisons were applied to control for family-wise error rate.
The authors were also interested in assessing the effect of work setting on number of patients seen per week. However, the assumption of homogeneity was violated, and thus, the authors applied a non-parametric procedure (i.e., Kruskal–Wallis test) to examine the effect of work setting on patient load. Similar to the previous analyses, the work setting served as the independent variable and number of patients seen per week served as the dependent variable. Bonferroni post hoc corrections were again utilized to control for multiple comparisons.
Work setting & factors related to quality of life: Finally, chi-square analyses were performed to assess the relationship between current work setting and QOL factors. For each chi-square test, work setting served as the independent variable and each QOL factor served as the dependent variable. A total of 11 chi-square tests were performed (i.e., one for each QOL question). Bonferroni corrections were used to adjust for multiple comparisons, and statistical significance was based on p < .005 (i.e., .05/11). Cohen’s d effect sizes were applied to interpret correlational and chi-square analyses: “small, d = .2,” “medium, d = .5,” and “large, d = .8” (Cohen, 1988).
Results
Demographic Characteristics and Professional Activities
One hundred and sixty-four psychometrists from 38 states completed the anonymous Qualtrics survey. See Table 1 for demographic characteristics. See Table 2 for descriptive information regarding professional activity characteristics.
Table 1.
Demographic characteristics (N = 164)
| M ± SD or N (%) | N (%) | ||
|---|---|---|---|
| Age | 36.6 ± 11.2 | Current setting of practicea | 61 (37.2%) |
| Education | General hospital | 39 (23.8%) | |
| High school | 1 (0.6%) | Academic medical center | 24 (14.6%) |
| Bachelor’s | 72 (43.6%) | Private practice | 22 (13.4%) |
| Master’s | 87 (53.0%) | Veterans/military hospital | 20 (12.2%) |
| Doctorate | 4 (2.4%) | Rehabilitation hospital | 10 (6.1%) |
| Professional | Psychiatric hospital | 5 (3.0%) | |
| Years post-training | 7.8 ± 6.5 | Otherc | 2 (1.2%) |
| Certifiedb | 48 (29.3%) | Community mental health |
aRespondents could select more than one.
bCertified by the Board of Certified Psychometrists.
cThe most frequent response associated with an “Other” selection was offsite, satellite locations for general, academic, or military hospitals.
Table 2.
Professional activity characteristics
| N (%) or M ± SD | N (%) | ||
|---|---|---|---|
| Patient age rangea | Patient age groupsa | ||
| 6–12 | 30 (20.7%) | Pediatrics only | 7 (4.8%) |
| 13–18 | 40 (27.6%) | Adults only (≤60) | 16 (11.0%) |
| 19–35 | 88 (60.7%) | Older adults only (≥60) | 20 (13.8%) |
| 35–60 | 116 (80.0%) | Lifespan | 32 (22.1%) |
| 60+ | 121 (83.4%) | Adults and older adults | 70 (48.3%) |
| Patients per week | 5.6 ± 2.5 | ||
| Hours testing per week | 18.8 ± 6.9 | ||
| Hours scoring per week | 9.4 ± 4.9 |
aRespondents could select more than one; N = 145–164.
Quality of Life Factors and Relationship to Job Responsibilities
Respondents answered various questions assessing factors that may contribute to overall QOL. Overall, 62% agreed that fatigue interfered with work, family, or their social life, ~42% and ~49% felt physically and emotionally exhausted, respectively, and ~43% experienced “burnout” because of their work. Nonetheless, ~60% of individuals felt satisfied with their QOL at work and had enough energy for family and friends during leisure time. See Fig. 1 for additional descriptive information.
Fig. 1.
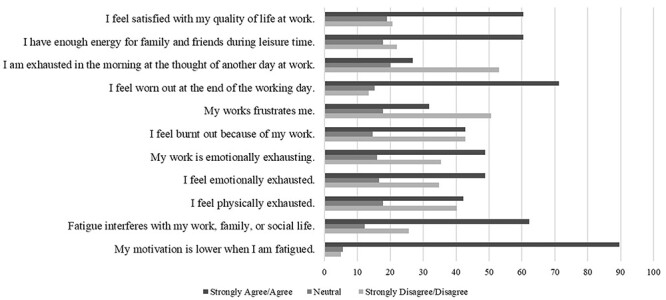
Psychometrists’ perspective on quality of life factors. Note: Percentages represent the n (%) of respondents.
We found significant associations of small magnitude (Cohen, 1988) among number of hours spent scoring per week and 8 of the 11 variables assessing QOL. Specifically, we found negative correlations between time spent scoring and feeling satisfied with QOL at work (r2 = −.282, p < .01), as well as having enough energy for family and friends during leisure time (r2 = −.241, p < .01). In addition, we found positive correlations between time spent scoring and factors of emotional exhaustion, motivation, feeling worn out, and feelings of burnout (r2 = .163–.218). Time spent administering neuropsychological measures revealed fewer significant associations with QOL variables (r2 = .164–.177). See Table 3 for a complete review of the correlational analyses.
Table 3.
Correlations between professional activities and quality of life factors
| QOL questions | Time spent testing (N = 164) | Time spent scoring (N = 161) |
|---|---|---|
| Spearman’s r | ||
| My motivation is lower when I am fatigued. | 0.003 | 0.163* |
| Fatigue interferes with my work, family, or social life. | 0.164* | 0.148 |
| I feel physically exhausted. | 0.090 | 0.068 |
| I feel emotionally exhausted. | 0.118 | 0.195* |
| My work is emotionally exhausting. | 0.177* | 0.218* |
| I feel burnt out because of my work. | 0.168* | 0.198* |
| My works frustrates me. | 0.098 | 0.123 |
| I feel worn out at the end of the working day. | 0.110 | 0.213* |
| I am exhausted in the morning at the thought of another day at work. | 0.072 | 0.184* |
| I have enough energy for family and friends during leisure time. | −0.123 | −0.241* |
| I feel satisfied with my quality of life at work. | −0.110 | −0.282* |
Note. *p < 0.05.
Effect of Work Setting on Professional Activities
Significant differences between work setting emerged for all three of the professional activities assessed including number of patients seen per week [X2 (4) = 12.02, p = .017, η2 = .088], number of hours administering tests [F (4, 133) = 3.27, p = .014, η2 = .090], and number of hours scoring [F (4, 132) = 2.51, p = .045, η2 = .071]. Bonferroni-adjusted post hoc comparisons revealed that psychometrists working within a VAMC see fewer patients per week (M = 4.26, SD = 1.52) than those at general hospitals (M = 5.96, SD = 2.13; p = .039) and academic medical centers (M = 6.27, SD = 2.64; p = .039). Additionally, those in a rehabilitation setting spend less time administering tests per week (M = 14.13 hours, SD = 8.13) than those in an academic medical center (M = 19.97 hours, SD = 7.09; p = .046), and less time scoring per week (M = 6.27 hours, SD = 3.9) than those in general hospitals (M = 10.46 hours, SD = 5.17; p = .036).
Effect of Work Setting on Quality of Life
In light of the significant difference between current setting and professional activities noted earlier, we examined the relationship between current setting and QOL factors. Responses to the statement “I am exhausted in the morning at the thought of another workday,” were significantly different between academic medical centers and VAMC [X2 (2) = 10.47, p = .005, φ = .449]. Specifically, academic medical center respondents agreed or strongly agreed at a higher rate (36.4%) relative to those in a VAMC setting (15.8%), and only 6.1% of those in an academic medical center felt neutral compared to 42.1% of VAMC respondents. We also found a similar trend between the general hospitals relative to VAMC [X2 (2) = 5.89, p = .061, φ = .275] such that those in a general hospital agreed or strongly agreed at a higher rate (30.9%) and reported feeling neutral less frequently (16.4%). Significant associations also emerged in response to the statement “My motivation is lower when I am fatigued,” when comparing rehabilitation settings to general hospitals [X2 (2) = 15.73, p = .000, φ = .474] and trended towards significance for academic medical centers [X2 (2) = 6.60, p = .037, φ = .371]. Specifically, 94.5% from general hospitals and 93.9% of respondents from academic medical centers agreed or strongly agreed to the statement regarding motivation and fatigue, relative to 66.7% of those currently in a rehabilitation setting.
Psychometrists’ Open-Ended Responses, Themes Identified
Seventy psychometrists responded to an open-ended question inquiring about additional information to contextualize or supplement their survey responses. The most frequent open-ended responses related to burnout and fatigue (cognitive, emotional, and physical; n = 34; 48.6%), followed by feeling overworked/undervalued (n = 20; 28.6%), concerns about compensation/job stagnation (n = 12; 17.1%), dissatisfaction of additional duties (n = 12; 17.1%), and variability of demands (e.g., hours, patients (n = 11; 15.7%). Psychometrists also experienced a variety of positive and meaningful aspects related to their employment (n = 8; 11.4%). See Table 4 for identified themes and examples of open-ended responses.
Table 4.
Open-ended responses and themes identified
| Theme | N | % of themes | % of respondents | Sample verbatim response |
|---|---|---|---|---|
| “Burnout” (i.e., cognitive, emotional, or physical fatigue) | 34 | 35.1 | 48.6 | “Although I do like my job, it does take a toll on me. The long testing sessions day-in and day-out, with potentially challenging patients, are emotionally and mentally exhausting. At the end of the day, there is only so much motivation and energy left to give to activities inside and outside of the home. It is very easy to feel burnt out.” |
| “…We also have some doctors who have unrealistic expectations of patients, making us give hours of testing to severely impaired patients or poor effort patients, which is frustrating for us and the patients. This environment is what has caused me to be emotionally burned out, not the actual testing or patient care.” | ||||
| “Flexibility is key to survival in this field. When the administration takes that away, burnout is higher, faster, and quality of end results suffer.” | ||||
| Feeling undervalued | 20 | 20.6 | 28.6 | “I feel more stress from my supervisors than I do my patient load. I feel there is a pressure to be as productive as possible and see as many patients as possible, so any bit of free time that may be utilized for scoring, admin work, etc. is redirected into testing patients. I feel there is little care in me as an employee/team member and more care in my productivity hours.” |
| “Our doctors have unrealistic expectations of patient work-load and turn-around time. We are expected to turn in scoring for several hours of testing in less than 30 minutes. Then, when there are errors due to time constraints, our performance is penalized. Doctors do not respect our need for a lunch-break, and we are often expected to work through lunch or eat very late in the day.” | ||||
| “Sitting a lot, difficult to find time to stretch or walk. Doctors, post docs and patients treat us terribly at times. If it were just the patients, it would not be as bad.” | ||||
| Insufficient salary & limited vertical advancement | 12 | 12.4 | 17.1 | “I think burnout for me is stemming from being underpaid for the invisible work that is done. I can go be a shift leader at a fast food restaurant for this pay. …” |
| “The position does not feel thankless as the doctors are very grateful for what we do, however, the rate of compensation does not do us any justice for the amount of work, dedication, education, training, and experience that is required for the position. The lack of mobility is another issue as there is no higher position to work towards, even for individuals with additional training and experience (i.e., you stay in one place).” | ||||
| “…our pay is well below the national average, our turnover rates are high, and our clinics overall environment is tainted with personality conflicts—making the job more difficult and exhausting than it ought to be.” | ||||
| Extra duties (e.g., administrative) | 12 | 12.4 | 17.1 | “A good portion of our time is also spent doing administrative tasks and training students.” |
| “Administrative tasks of the job are the most exhausting. Such as attaining medical records is likely the most frustrating component to the job and very time consuming…Scheduling patients can also be very challenging. Often patients are not very capable of attending their appointments. You must find family members and set up transport for patients. All these tasks are often the most draining of the job.” | ||||
| Variability in demands & expectations | 11 | 11.3 | 15.7 | “(Regarding QOL) It depends on the types of patients and the doctor/administration’s expectations, which varies.” |
| “The workload is either very light or very heavy, not a good balance. Some days you do not test at all. Other days, you test 4–5 hours and score on top of that.” | ||||
| “Our department is going through a lot of changes and with these changes it brings more work/different work. It feels as if we are reinventing the wheel at time and that adds a lot of drain on the psychometrist. For example: Mandatory overtime 1 month, followed by cutting hours and sending people home the next.” | ||||
| Positive aspects | 8 | 8.2 | 11.4 | “As a veteran, working with veterans in this capacity is the most meaningful work I’ve done to date.” |
| “I would like to specify that the work or quality of work is fantastic, I love my job and the work I do.” | ||||
| “I have an amazing boss who models excellent self-care and how to take care of our patients.” |
Note. N = 97; themes generated from responses provided by 70 participants.
Discussion
Prior research highlights how neuropsychologists have benefitted from psychometrists with regard to efficiency, patient volume, and cost-effectiveness (Axelrod et al., 2000; Malek-Ahmadi, Erickson, Puente, Pliskin, & Rock, 2012; Sweet et al., 2015). Despite the clear support of the psychometrist-model in neuropsychology practice, only recent data (Kippie et al., 2019) highlights psychometrists’ perspective of their day-to-day responsibilities. To our knowledge, this study is the first to explore the potential effects of these day-to-day responsibilities on psychometrists’ QOL.
Our findings indicate that nearly half of the respondents experienced emotional exhaustion because of their work, and a higher number endorsed feeling “worn out” at the end of the workday, as well as a lack of energy for family and friends. Relatedly, respondents’ report of fatigue appeared to be a major factor that interfered with work, family, and/or social life. The frequency of fatigue and emotional exhaustion among psychometrists are higher than in the general population (Bültmann, Kant, Kasl, Beurskens, & van den Brandt, 2002; Pawlikowska et al., 1994), and appear to be more in line with those working as nurses or physicians. Specifically, ~46% of physicians report at least one symptom of burnout (e.g., high emotional exhaustion or depersonalization) compared to ~28% of working US adults (Shanafelt et al., 2012), and nearly 30–40% of nurses experience considerable job strain, including emotional exhaustion and feeling overwhelmed by their work (Aiken et al., 2001). In contrast, respondents’ perception of work-life balance and work satisfaction were similar to that of the general US working population as ~23% of working US adults experience dissatisfaction with work-life balance (Shanafelt et al., 2012), compared to ~40% of physicians (Shanafelt et al., 2012) and 40% of nurses (Aiken et al., 2001).
In support of our hypotheses, we found significant associations between psychometrists’ professional activities and QOL variables. However, to our surprise, time spent administering measures revealed fewer associations with work-related QOL variables relative to time spent scoring. These findings suggest there may be particular aspects of scoring procedures that are less fulfilling and/or unfavorable to psychometrists’ physical and mental health, as well as work satisfaction. Speculatively, scoring practices often can be time-consuming and require an attention to detail that may be particularly challenging following long evaluations. Another possibility might relate to the variability among scoring preferences (e.g., application of different normative data depending on patient demographics and/or variability in provider approach), all of which may contribute to the overall exhaustion experienced by psychometrists.
In addition, our explorative analyses found group differences in professional activities based upon psychometrists’ practice setting. Specifically, VAMC settings see fewer patients relative to general hospitals and academic medical centers, and rehabilitation settings spend less time on evaluations and scoring relative to academic medical centers and general hospitals. These findings were consistent with the associations found between current practice setting and QOL factors, such that those practicing within an academic medical center were more likely to agree with the statement “I am exhausted in the morning at the thought of another day at work,” relative to their VAMC counterparts. Moreover, respondents within an academic medical center or general hospital experienced higher rates of reduced motivation when fatigued relative to those in a rehabilitation setting. One speculation for this may be that there are aspects within a VAMC or rehabilitation setting (e.g., number of patients evaluated, shorter evaluations, regimented schedules) that can buffer the effects of burnout. These findings are consistent with previous research examining other specialties, which found higher emotional exhaustion and greater job dissatisfaction with higher patient-to-nurse ratios (Aiken, Clarke, Sloane, Sochalski, & Silber, 2002).
The current findings also highlight that psychometrists perform numerous job duties consistent with other published findings (Kippie et al., 2019). Specifically, in addition to expectations of test administration, scoring, and writing behavioral observations, respondents could also be responsible for ordering protocols, conducting prior authorizations, training externs, and other administrative procedures. Although many respondents experienced additional fatigue and frustration from these duties, it is important to note that there were also individuals who appreciated the variability provided by this component of their job. Speculatively, the negative experiences described by this subset may be due to a lack of training and/or misleading expectations within the job requirements. Additionally, our open-ended responses indicate that a small subset of individuals experienced a lack of upward mobility and felt both underpaid and underappreciated. Consistent with Kippie et al. (2019) who found a statistical difference in salary for those with board certification and greater years of experience, the vast majority of individuals who felt such stagnancy (n = 10) were not board certified.
Limitations
Several study limitations warrant discussion. Given the smaller sample size, our overall findings may not be a true reflection of all psychometrists; however, the current sample size is consistent with, and marginally greater than, previous research of this nature (Kippie et al., 2019). We also recognize that there is an inherent selection bias in those who were interested and/or motivated to complete the survey. Another limitation relates to the fact that we did not gather data on whether psychometrists were employed full-time or part-time, nor did we collect information on additional demographic factors such as gender and ethnicity/race, all of which could be related to work QOL. To that end, given our unequal sample size across work setting (e.g., underrepresentation within private practice, VAMC, and rehabilitation hospitals), our ANOVA and post hoc test findings should to be interpreted with caution as conclusive statements cannot be made with certainty despite our attempt to control for Type I error rate by use of Bonferroni correction. Another limitation pertains to the questions utilized in the current survey. Despite this survey being exploratory and our use of face-valid questions, the survey itself was not validated. Although other QOL measures exist for a range of groups including professionals who experience vicarious trauma (Professional Quality of Life Measure; Heritage, Rees, & Hegney, 2018) and those with chronic illness (Quality of Life Scale; Burckhardt & Anderson, 2003), to the authors’ knowledge, there is no existing measure applicable to the specific challenges and experiences of psychometrists. As such, in addition to the lack of psychometric properties, the extent of open-ended responses indicated that our questions did not fully appreciate the range of psychometrists’ emotions and experiences. In addition, our work-related QOL questions focused on negative experiences/perceptions and did not address positive aspects of QOL as comprehensively. Although we touch on positive factors in the open-ended responses, further research aimed towards a better understanding of one’s sense of meaning and purpose is recommended.
Conclusions and Future Directions
The novel implications of these findings are of importance to the field in two ways. First, this study provides additional information pertaining to psychometrists’ workload, and the breadth of responsibilities/job duties. Second, this data is the first in the field to characterize the association between work QOL and workload among psychometrists. In light of the current findings, structural adjustments, such as computerized/automated scoring techniques, may be indicated in order to promote psychometrists’ work-related QOL. Given the interest in computerized assessment and scoring procedures (Parsons & Duffield, 2019), future research aimed at understanding how such implementation might affect psychometrists’ work-related QOL will be needed. Moreover, the effect of psychometrists’ work status (i.e., part- versus full-time) and board certification are two potential variables to incorporate in order to glean a better understanding of work-related QOL and quality improvement. Lastly, continued advocacy for psychometrists is called for in order to (1) promote the implementation of national standardization and credentialing for government recognition, (2) provide fair compensation and appropriate expectation of workload and job duties consistent with physician extender counterparts (e.g., other healthcare technicians), and (3) creation of “psychometrist practicing guidelines” for uniform and consistent practice.
Supplementary Material
Acknowledgments
Data contained in this manuscript was presented at the 2020 annual meeting of the International Neuropsychological Society (Denver, CO).
Contributor Information
Katherine L Zane, Ohio Health, Physician Group-Neuroscience, Columbus, OH 43215, USA.
William T McCuddy, Department of Behavioral Medicine and Psychiatry, Rockefeller Neuroscience Institute, West Virginia University School of Medicine, Morgantown, WV 26505, USA.
James J Mahoney, III, Department of Behavioral Medicine and Psychiatry, Rockefeller Neuroscience Institute, West Virginia University School of Medicine, Morgantown, WV 26505, USA; Department of Neuroscience, Rockefeller Neuroscience Institute, West Virginia University School of Medicine, Morgantown, WV 26505, USA.
Merry K Kelty, Department of Psychiatry and Neurobehavioral Sciences, University of Virginia, Charlottesville, VA 22903, USA.
David M Scarisbrick, Department of Behavioral Medicine and Psychiatry, Rockefeller Neuroscience Institute, West Virginia University School of Medicine, Morgantown, WV 26505, USA; Department of Neuroscience, Rockefeller Neuroscience Institute, West Virginia University School of Medicine, Morgantown, WV 26505, USA.
Funding
Dr. Mahoney III receives support by the National Institute of General Medical Sciences of the NIH under Award Number U54GM104942.
References
- Aiken, L. H., Clarke, S. P., Sloane, D. M., Sochalski, J. A., Busse, R., Clarke, H. et al. (2001). Nurses’ reports on hospital care in five countries. Health Affairs, 20(3), 43–53. [DOI] [PubMed] [Google Scholar]
- Aiken, L. H., Clarke, S. P., Sloane, D. M., Sochalski, J., & Silber, J. H. (2002). Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA: The Journal of the American Medical Association, 288(16), 1987–1993. [DOI] [PubMed] [Google Scholar]
- American Academy of Clinical Neuropsychology (1999). American Academy of clinical neuropsychology policy on the use of non-doctoral-level personnel in conducting clinical neuropsychological evaluations. The Clinical Neuropsychologist, 13, 385–385. [Google Scholar]
- Axelrod, B., Heilbronner, R., Barth, J., Larrabee, G., Faust, D., Pliskin, N. et al. (2000). The use of neuropsychology test technicians in clinical practice: Official statement of the National Academy of neuropsychology. Archives of Clinical Neuropsychology, 15, 381–382. [PubMed] [Google Scholar]
- Board of Certified Psychometrists . (2020). Retrieved May 13, 2020, from https://psychometristcertification.org/faqs
- Bültmann, U., Kant, I., Kasl, S. V., Beurskens, A. J., & van den Brandt, P. A. (2002). Fatigue and psychological distress in the working population: Psychometrics, prevalence, and correlates. Journal of Psychosomatic Research, 52(6), 445–452. [DOI] [PubMed] [Google Scholar]
- Burckhardt, C. S., & Anderson, K. L. (2003). The quality of life scale (QOLS): Reliability, validity, and utilization. Health and Quality of Life Outcomes, 1(1), 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Erlbaum. [Google Scholar]
- DeLuca, J. W., & Putman, S. H. (1993). The professional/technician model in clinical neuropsychology: Deployment characteristics and practice issues. Professional Psychology: Research and Practice, 24, 100. [Google Scholar]
- Division 40 Task Force on Education Accreditation Credentialing (1989). Guidelines regarding the use of non-doctoral personnel in clinical neuropsychological assessment. The Clinical Neuropsychologist, 3, 23–24. [Google Scholar]
- Division 40 Task Force on Education Accreditation Credentialing (1991). Recommendations for education and training of non-doctoral personnel in clinical neuropsychology. The Clinical Neuropsychologist, 5, 23–24. [Google Scholar]
- Duarte, J., Pinto-Gouveia, J., & Cruz, B. (2016). Relationships between nurses’ empathy, self- compassion and dimensions of professional quality of life: A cross-sectional study. International Journal of Nursing Studies, 60, 1–11. [DOI] [PubMed] [Google Scholar]
- Easton, S., & Van Laar, D. (2018). User Manual for the Work-Related Quality of Life (WRQoL) Scale: A Measure of Quality of Working Life. (2nd ed.). England: University of Portsmouth. doi: 10.17029/EASTON2018 [DOI] [Google Scholar]
- Heritage, B., Rees, C. S., & Hegney, D. G. (2018). The ProQOL-21: A revised version of the professional quality of life (ProQOL) scale based on Rasch analysis. PLoS One, 13(2), e0193478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holm, S. (1979). A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics, 6, 65–70. [Google Scholar]
- Kippie, A., Ryan, B. J., McManemy, H., Escobar Medina, M., Porter, P., & Malek-Ahmadi, M. (2019). National Association of Psychometrists: 2015 professional practices and salary survey of U.S. and Canadian psychometrists. The Clinical Neuropsychologist, 33, 13–31. [DOI] [PubMed] [Google Scholar]
- Malek-Ahmadi, M., Erickson, T., Puente, A., Pliskin, N., & Rock, R. (2012). The use of psychometrists in clinical neuropsychology: History, current status, and future directions. Applied Neuropsychology, 19, 26–31. [DOI] [PubMed] [Google Scholar]
- Parsons, T. D., & Duffield, T. (2019). National Institutes of Health initiatives for advancing scientific developments in clinical neuropsychology. The Clinical Neuropsychologist, 33, 246–270. [DOI] [PubMed] [Google Scholar]
- Pawlikowska, T., Chalder, T., Hirsch, S. R., Wallace, P., Wright, D. J. M., & Wessely, S. C. (1994). Population based study of fatigue and psychological distress. BMJ, 308(6931), 763–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puente, A. E., Adams, R., Barr, W. B., Bush, S. S., Ruff, R. M., Barth, J. T. et al. (2006). The use, education, training and supervision of neuropsychological test technicians (psychometrists) in clinical practice: Official statement of the National Academy of neuropsychology. Archives of Clinical Neuropsychology, 21, 837–838. [DOI] [PubMed] [Google Scholar]
- Rohland, B. M., Kruse, G. R., & Rohrer, J. E. (2004). Validation of a single-item measure of burnout against the Maslach burnout inventory among physicians. Stress and Health: Journal of the International Society for the Investigation of Stress, 20(2), 75–79. [Google Scholar]
- Shanafelt, T. D., Boone, S., Tan, L., Dyrbye, L. N., Sotile, W., Satele, D. et al. (2012). Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Archives of Internal Medicine, 172, 1377–1385. [DOI] [PubMed] [Google Scholar]
- Sweet, J. J., Benson, R. M., Nelson, N. W., & Moberg, P. J. (2015). The American Academy of clinical neuropsychology, National Academy of neuropsychology, and Society for Clinical Neuropsychology (APA division 40) 2015 TCN professional practice and ‘salary survey’: Professional practices, beliefs and incomes of US neuropsychologists. The Clinical Neuropsychologist, 29, 1069–1162. [DOI] [PubMed] [Google Scholar]
- Wallace, J. E., Lemaire, J. B., & Ghali, W. A. (2009). Physician wellness: A missing quality indicator. The Lancet, 374(9702), 1714–1721. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


