Abstract
In countries where headache services exist at all, their focus is usually on specialist (tertiary) care. This is clinically and economically inappropriate: most headache disorders can effectively and more efficiently (and at lower cost) be treated in educationally supported primary care. At the same time, compartmentalizing divisions between primary, secondary and tertiary care in many health-care systems create multiple inefficiencies, confronting patients attempting to navigate these levels (the “patient journey”) with perplexing obstacles.
High demand for headache care, estimated here in a needs-assessment exercise, is the biggest of the challenges to reform. It is also the principal reason why reform is necessary.
The structured headache services model presented here by experts from all world regions on behalf of the Global Campaign against Headache is the suggested health-care solution to headache. It develops and refines previous proposals, responding to the challenge of high demand by basing headache services in primary care, with two supporting arguments. First, only primary care can deliver headache services equitably to the large numbers of people needing it. Second, with educational supports, they can do so effectively to most of these people. The model calls for vertical integration between care levels (primary, secondary and tertiary), and protection of the more advanced levels for the minority of patients who need them. At the same time, it is amenable to horizontal integration with other care services. It is adaptable according to the broader national or regional health services in which headache services should be embedded.
It is, according to evidence and argument presented, an efficient and cost-effective model, but these are claims to be tested in formal economic analyses.
Keywords: Headache disorders, Public health, Health policy, Barriers to care, Needs assessment, Health-technology assessment, Structured headache services, Service organization and delivery, Primary care, Global Campaign against Headache
Introduction
Governments, politicians and health-service managers concerned about the cost of headache care for very large numbers of people fail to recognize a fundamentally important aspect of the economics of headache disorders: untreated, they are a huge financial drain. The high levels of disability repeatedly attributed to headache, and migraine in particular [1–9], are expressed not only as lost health but also in lost productivity [10–15] and detriments to gross domestic product (GDP) [16–19].
In an enlightened view, this is an opportunity. A wealth of evidence attests the efficacy of treatments for migraine and other primary headache disorders that can well be provided by non-specialists [20]. In a reasonable expectation, good health care delivering these treatments efficiently to those who will benefit from them will substantially reduce the ill-health burden of headache. The costs may be high – because there are very many such people – but, again in a reasonable expectation, interventions achieving this purpose will be cost-effective [21]. In many economies they may be cost saving, through the recovery of lost work time [22].
Regrettably, throughout the world, the opportunity is missed: health-care systems that ought to provide this care either do not exist or, where they do, fail to reach many who need it [23, 24].
In this manuscript, a product of the Global Campaign against Headache [24–26], we aim to show the solid basis of these expectations. In so doing, we aim, more pertinently, to generate political recognition of the need to address this health-care failure and the educational failures lying behind it [22]. Further, by setting out a model of how they can be addressed, we lay the foundations for economic analyses demonstrating the value of treating headache.
Methods
Experts from all world regions, in headache, health service organization or health-technology assessment, were brought together to contribute to these proposals through email correspondence. The group was diverse, with members drawn from high-, middle- and low-income countries.
They took evidence from the published literature and, using this, built a headache-care model by developing and refining previous proposals for headache service organisation [27–29] put forward by Lifting The Burden (LTB) [26] and the European Headache Federation (EHF) [30]. They extended the applicability of the model beyond Europe through their own expertise and local knowledge and by drawing from experience and understanding gained by the Global Campaign against Headache during its 16 years of activities worldwide [26].
The problems
The challenge of numbers
Headache disorders are common, and, although most are episodic, in many cases they are lifelong conditions. They are also acknowledged to be among the top three causes of disability in the world [5–9]. Three – migraine, tension-type headache (TTH) and medication-overuse headache (MOH) – account for almost all headache-attributed burden [1, 5–8]: burden expressed in personal suffering, disability, impaired quality of life and financial cost as well as impact extending beyond those immediately affected [10].
Given all of this, it is unsurprising that large numbers of people with headache seek health care [31–33]. For example, in a United Kingdom (UK) study based in primary care 20 years ago, 17% of registered patients aged 16–65 years had consulted a general practitioner (GP) because of headache [33]. This is a good example because, in the UK, virtually everyone is registered with a GP.
However, existence of a health disorder, even one that is manifestly burdensome, does not translate directly into need for professional health care. Need in the context of health economics and policy is defined with regard to potential for benefit. Effective treatments exist [20, 34], but the proposal that everyone with headache has need for professional care is not arguable in a resource-limited world. Need is predicated on anticipated benefit, but this must rise above a threshold of benefit, itself judged against benefit achievable by other means (cost-effectiveness).
Headache-related health care needs assessment
Thresholds are hard to set objectively, although needs assessments are highly sensitive to them.
A previous estimate – essentially based on expert opinion – is that 50% of people with headache can manage themselves, using, if necessary, simple over-the-counter (OTC) medications [28]. They do not, or rather should not, need professional health care. While this estimate reflects the proportion of successful outcomes in clinical trials of OTC medications, these have almost all been conducted in patients, who are not the relevant denominator.
Many people do manage themselves, a large proportion through necessity, others from choice, none of them necessarily effectively. Those who choose self-management are not only the less severely affected [35]: they include a number who, for whatever reason and despite significant disability [36, 37], expect the marginal benefit of professional involvement in their care to be small (sub-threshold benefit negates need). Here is a problem, because expectations are quite often unrealistic – too high, or sometimes too low – so that needs assessment based on what people currently do [31–33, 35–47] has very questionable validity. This is more so when service improvement is planned: a better service – if “better” means delivering enhanced benefit – should see greater usage than a poor service it replaces (discovered need). While planning must factor this in, it is difficult to estimate.
Aside from these consumer-driven issues, another is also threshold-dependent. Cash-limited health services seek value for money: they will discount assessed needs, however great, whenever utility gain per unit of health-care resource consumption will be low. In headache medicine, the potential for benefit from professional health care is generally greatest among those worst affected, so that health policy might reasonably focus on these. Further, both migraine and MOH can, in most cases, be treated not only effectively but also at rather low cost [20, 21].
What follows – an assessment of how much professional headache care should be provided as a matter of policy – updates earlier estimates [27–29]. The approach adopted is conservative: it will under- rather than overestimate need. As will become apparent, any other approach would be unhelpful.
As with all economic assessments, there are many assumptions.
The first is that only those with disabling headache need professional care. The implication that others can adequately look after themselves is possibly unfair, but the assumption respects a reasonable view of priority. It effectively and helpfully removes most people with episodic TTH from consideration, this disorder generally (again perhaps unfairly [48]) being regarded as not significantly disabling [49] (There is also little that professional care can do for most episodic TTH beyond offering OTC medications [20]).
About two thirds (66%) of the world’s population are aged 15–64 years [50], these being the years during which headache disorders tend to be troublesome. About 25% are aged 14 or under [51]. Thus, with regional variations, in every million people living in the world there are 660,000 and 250,000 in these age groups respectively. Primary headache is less common, and less troublesome, in older people [1], who therefore contribute negligibly to expected numbers.
Best current epidemiological evidence suggests that a global average of about 15% of adults aged 15–64 have migraine [1, 6]. Further evidence is that 80% of these 15% (ie, 12%) are significantly disabled through pain and associated symptoms [52]. In every million people in the world, therefore, there are 80,000 adults (12% of the 660,000 aged 15–64 years) who need care because of migraine-attributed disability. A small proportion of adults have chronic TTH. While this is likely to be disabling, their numbers are not reliably known, partly because epidemiological data are limited and partly because conflation with MOH makes these data unreliable. As for MOH, the proportion varies greatly from country to country, with the best and most recent estimate suggesting a global mean prevalence of 1.5% [53]: another 10,000 (1.5% of the 660,000) needing care for two reasons. MOH is rated as highly disabling [49, 54], not surprisingly since it is frequently recurring by definition and very painful when present [55]. Although medication overuse may be the means by which many people with MOH nonetheless remain (partly) functional, it always requires professional care because it will not otherwise resolve.
The total of 90,000 per million (13.5% of the 660,000), which ignores TTH for reasons stated, is only one third of the estimated prevalence of all headache including TTH [1, 6] – substantially less than the 50% proposed earlier as being the proportion in need of professional care [28]. It may be over-conservative: it is somewhat below the UK finding (above) that 17% of GP-registered adults consult for headache [33], but this, although essentially a population-based observation, was a reflection of demand, not need. These, as we argue below, are not the same.
Needs arise in the child and adolescent populations also, but are more difficult to quantify, partly because there are fewer data – and none that are reliable in very young children (below 6 years) [1, 56]. In the age range 6–14 years, headache is apparently as common as in adults [1, 56, 57], but it has different characteristics. While migraine prevalence is lower, dependent upon age and reaching adult levels during the course of adolescence, undifferentiated headache (UdH) largely fills its place, albeit with less disabling consequences [57]. Furthermore, even migraine in these age groups tends to be short-lasting. In the absence of better data, a conservative but reasonable working basis is that headache-care needs in these age groups, in terms of numbers, are, proportionately, half those of adults [28, 29]: another 17,000 (0.5*13.5% of the 250,000 aged 14 or under) in each million of the population.
Service provision requirement
From these statistics, with some further assumptions, we can make arguably fair estimates of service requirements.
First is an assumption about demand. Need and demand overlap, but are not the same – each can exist without the other. Need for professional headache care, defined as above (ie, with regard to potential for benefit), becomes demand only in those who seek care. On the other hand, care may also be sought in the absence of need (as defined). Complex and poorly understood factors govern health-care seeking behaviour and care utilization by people with headache [35]. On the negative side are the obstacles to care described below (see The “patient journey”, and “care pathway”), which act as deterrents. Failed self-management is a positive driver. False expectations – too high or too low - have positive or negative influences accordingly. Evidence suggesting that demand for headache care is expressed by as few as half of those who might be considered in need [33, 35, 36, 58] is unreliable, because studies reporting this were not well able to judge need for care. Further, it is uncertain whether needs assessment for the purpose of service provision should reflect needs expression rather than a more objective assessment of need (as we wrote earlier, needs assessment based on what people currently do has very questionable validity). But we will adopt this estimate, pragmatically, because no other exists. If demand is indeed suppressed by barriers to care, better and more accessible services, dismantling these barriers, will generate increase. We assume that take-up of improved services will still not be 100%, but 75%, representing a closure of half the currently estimated gap [21].
Second are multiple assumptions about time (Table 1). These are based on expert views of requirement [21, 28, 29] but tempered with conservatism. They consider only ambulatory care: inpatient management is ignored in view of the minimal requirement for it. Admission is sometimes good practice, because of comorbidities or for detoxication in MOH, but only in a tiny percentage of patients.
Table 1.
Assumptions in estimating service requirements to meet headache-care demand in a population (updated and revised from [29])
| Assumption | Argument |
|---|---|
| The average consultation need per adult patient is 1.25 h per 2 years. | This average is within a wide range of variation. In some countries (eg, Portugal) consultation times are subject to legal recommendations but, otherwise, consultation need varies mostly according to diagnosis and to level within the health-care system. Primary-care needs can usually be met by a first visit of 15–20 min’ duration for diagnosis and impact assessment followed by 10-min visits for monitoring and prescription of acute and preventative therapies, initially after 2–4 weeks then after each 3–6 months (totalling five or six in 2 years). At higher levels of care, first consultations are usually longer (up to 45 min), reflecting case-complexity, but follow-up visits are fewer. |
| The average consultation need per child or adolescent patient is greater: 2 h per 2 years. | Expert opinion cites the need for additional enquiry into family dynamics, schooling and peer relationships as issues relevant to management success. |
| No wastage occurs through failures by patients to attend appointments. | This assumption appears manifestly false, but wastage of this sort is difficult to predict in the context of proposals for service improvement. At present, it is commonly discounted by overbooking. |
| A health-care provider, if working full time on headache without other clinical responsibilities, is available for consultation for 1380 h/year.a | At any level, 1 day per week is assumed for non-clinical work (administration, audit and continuing professional development); each week therefore allows 4 days, each of 7.5 h, of patient-contact time. Only 46 weeks are worked per year. |
aThis assumption allows estimates based on full-time equivalence (see Table 2). It is immaterial that full-time commitment to headache is rare except in level 3
Notwithstanding the conservatism pervading the assumptions, Table 2 sets out very challenging estimates of service requirement. We say more about this below (see The health-care solution).
Table 2.
Estimated service requirements to meet headache-related health-care demand in a population of 1 million (from [29])
| Estimated numbers expressing demanda | Expected demand | |
|---|---|---|
| Hours/year of medical consultation time | FTE health-care providersb required to deliver | |
| Adults: 67,500 (75% of 90,000) | 42,200 | 37 |
| Children and adolescents: 12,750 (75% of 17,000) | 12,750 | 9 |
FTE Full-time equivalent; aassuming 75% of those with need; bone FTE provider does not necessarily imply one provider engaged full-time on headache; it could, for example, be two engaged half time on headache, or ten working 10% of full time
The failing status quo: inefficient and inequitable services, and not only in low-income countries
The “patient journey”, and “care pathway”
Evidence from throughout the world is that headache care reaches a minority of those who need it [22, 35–40] (to say nothing about its quality).
The primary reason is a worldwide context of low priority accorded to headache disorders in the queue for health-care resources, evident for over 20 years [59]. A decade ago, the World Health Organization (WHO) published its Atlas of Headache Disorders and Resources in the World 2011, recording the worldwide ill health caused by headache [22]. Noting that this was mostly untreated, WHO called for change, in a message distributed to the health ministries of every country [22]. In the 10 years since, change has not been in evidence [9, 23], although attention among WHO’s member states is beginning now to fall on neurological diseases (including headache) [60].
We estimated above that two thirds of people with headache could manage themselves, needing no more than advice from pharmacists [36]. As we will show, keeping these people out of the health-care system is crucial to efficient and equitable implementation of care. But many people who might succeed in self-management lack the small amount of knowledge on which success depends, and receive neither educational nor practical support to help them. Instead, they join the queue for health care, thus, unnecessarily, embarking upon the “patient journey”.
The one third who do need professional care are likely to find the patient journey overcrowded and frustrating, with headache services fragmentary or difficult to access and the “care pathway” a mere misnomer – winding and beleaguered by culs-de-sac and poor signposting [61]. One consequence is direct presentation to emergency departments, without justifying medical need but benefiting the patient (at high cost) by bypassing the care pathway altogether [62, 63].
“Headache services”, if existing at all, are too often equated with headache clinics, usually located sporadically and in big urban centres according more to market forces than objective assessment of need. Public perception is often the driver, encouraged by policies in many countries that allow direct (and often unguided) self-referral to specialists. Iran, a country with well-developed health services, is a good example, with many people taking fruitless paths to neurosurgeons, otorhinolaryngologists, ophthalmologists or pain clinics (the poorly signposted care pathway [61]). In Russia, one in every three people receiving care for migraine have gone directly to neurologists [18]. In Estonia, also a country of the former USSR but with well-developed primary care and a referral system, the proportion sent by GPs to neurologists prior to an educational intervention was a not dissimilar 39.5% [64]. In Western Europe, also one in three people treated for headache in Spain, and one in four in Luxembourg, see specialists for this purpose [40]. In Greece, only one fifth of people with headache seek professional care, but most of these do so from private neurologists [65]. In the UK, where GPs maintain a gatekeeper role as an essential feature of the national health service, the proportion (9%) referred to secondary care [33] was in line with reasonable expectation (see below: Division of caseload). Neurologists, however, receiving most of these referrals, reported that up to a third of all their patients consulted for headache, more than for any other neurological condition [31].
Of course, specialist clinics are needed [66], but only by those with complex disorders requiring high-end multidisciplinary care, who are a small minority [28, 29]. If specialist clinics with their very limited capacity are at the centre rather than the apex of headache services, this purpose is likely to be thwarted by the overload of patients whose needs should be met elsewhere. Most people with headache have one of only a few very common disorders, which ought to be wholly familiar to primary-care providers and only rarely present diagnostic or management difficulties [20, 28]. But the underlying problem is that non-specialist care for headache is variable at best.
There are illustrative and revealing studies. To begin in high-income countries [67], in a population-based study in United States of America (USA) and UK, only two thirds of adults with migraine were found to be correctly diagnosed [35]. Half were consulting health-care providers (HCPs) – too many according to our earlier (conservative) estimate – but over 60% of those not consulting exhibited high migraine-related disability [35]. There was probable ascertainment bias in this study, but nonetheless it was indicative of malfunctioning care pathways in both countries. More recently, the Eurolight study in 10 European Union (EU) countries found that, among participants with frequent migraine and an unambiguous need for preventative medication (more than five headache days per month), fewer than 20% had received medical care at any level [68, 69]. Incorporating indices of adequacy of care, this study identified adequate acute treatment in barely half of these (ie, fewer than 10% in most of the countries) and even smaller proportions with the preventative medication for which they were clearly eligible [40]. In upper-middle-income Russia [67], again in a population-based survey, only 15% nationwide of people with headache were consulting, one third, as noted, with specialists [18, 41]. In lower-middle-income Nepal [67], also in a population-based survey, a much higher 58% of participants with headache had consulted a professional HCP in the previous year, and 8% had seen a specialist of some sort [42]. While these findings suggest better availability of health care in Nepal than in many other, much wealthier countries (Japan [38] and Taiwan [43], EU countries [40, 44] and UK and North America [35, 45, 46, 52]), all is not as it seems. The count of “medical consultations” in Nepal included a very wide range of HCPs, some with no counterparts or who would not be accredited as health professionals in other countries [42]. With pharmacist consultations (15%) excluded, the consulting proportion fell to 43% [42], similar to the 47% in China [47]. In the most salient comparison, with only physician-consultations considered, the proportion fell further to 19% (GPs 11%, specialists 8% [42]), much lower than those elsewhere [35, 38, 43, 45–47, 52] – except for Russia [18, 41]. Further, since there are no headache specialists and few neurologists in Nepal, “specialist” consultations were mostly with ophthalmologists, otorhinolaryngologists or psychiatrists [42]. In other words, these findings reflected high demand without indicating good care: on the contrary, headache-attributed burden in Nepal remains egregiously high [70].
Educational failures – the root of the problem
The origins of these health-care failures are clearly traceable to educational failures, occurring at every level [22].
On the political level, few governments appear willing to take concerted action against headache [9, 23, 71]. This is puzzling [8, 22]. It indicates a lack of awareness either of its substantial population ill-health burden (increasingly unlikely, since the Global Burden of Disease [GBD] study repeatedly affirms this [2–8]) or of its equally substantial but potentially reversible economic burdens on society [11–19, 21].
Among HCPs, very limited training in headache [22] does little to engender interest, good outcomes or, ultimately, satisfaction among themselves or their patients. For doctors this is a problem sewn in medical schools, the consequence, again, of low priority: worldwide, only 4 h are committed to headache disorders in 4–6 years of formal undergraduate medical training [22].
Among the general public, headaches – neither fatal nor contagious, and often invisible – are trivialized as “normal”, and, far worse, seen by some, in those who complain of them, as no more than an excuse to avoid responsibility [23, 72].
All of these need to change.
The health-care solution
The numbers estimated above (see Service provision requirement) cannot be regarded as precise: they are sensitive to the multiple assumptions, particularly those related to time (Table 1). But, from them, two conclusions are certain.
First of these is that specialist care, with its very limited capacity, cannot meet all needs, or even a substantial part of them. Systems or practice that lead to large numbers of headache referrals to neurologists or other specialists must be questioned.
Second, and the corollary to this, is that headache care in the main belongs and must be delivered in primary care. This is not undesirable for two principal reasons (others have to do with efficiency and cost containment). On a neutral level there is, as noted, no clinical objection to it: education may be required, but the necessary skills exist in primary care [20, 28]. On the plus side, since WHO’s Declaration of Alma-Ata of over 40 years ago [73], wherever health-care reform is in progress there is emphasis on strengthening primary care, with its benefits of continuity and care in the community [60, 73–77]. While models of health care vary throughout the world, whatever the overarching system of care, primary care has a recognized and important role nearly everywhere. In highly rural regions, those of sub-Saharan Africa, for example, primary care in whatever form it takes is the only point of contact for most patients.
Structured headache services
Systems approach to health care
Drawing from engineering theory, a systems approach to a problem or need first identifies it (“understanding the problem space” – which the foregoing has done) and then pulls together system elements that, working together, will resolve the problem or meet the need (“the solution space”) [78]. There are steps in the process, working from needs to requirements and from design to integration to delivery [78], but these do not need to be detailed here. The key feature shared by all well-functioning systems – in health care as much as in engineering – is that “their elements together produce results not obtainable by the same elements alone” [78]. Applicable particularly to health care, a systems approach involves “integrating the necessary disciplines into a team who then use a structured process to deliver a system” [78]. The health-care solution to headache is envisioned through applying this approach to headache care.
Nationwide structured and educationally supported headache services embedded and integrated within a country’s health-care system are the means of efficiently, effectively and equitably mitigating the personal and societal burdens of headache to the greatest extent possible with resources available, a proposition put forward by LTB and endorsed by WHO a decade ago [22]. Structured headache services pull elements together from primary, secondary and specialist (tertiary) care, and, importantly, from pharmacy services. Equally importantly, they also harness self-management. Educational supports are an additional element, required at all system levels and including public education on when and how to make correct use of these services. Integration within the broader health-care system is crucial: if headache services merely develop ad hoc, driven not by coherent policy but opportunistically by interested individuals, as is now the case in most countries providing any service at all, they can be neither efficient nor equitable.
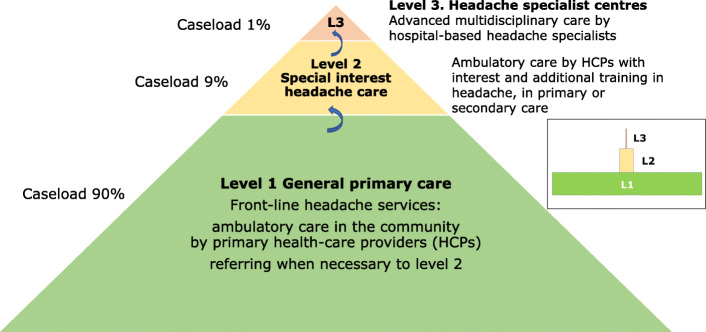
The essential purposes of headache-service organization are two-fold: to create capacity matched to need, and to divide service provision rationally between provider levels. The guiding principle in both purposes is that management of patients should be at the lowest level commensurate with good care. Achieving this makes most efficient use of allocated resources. Basing headache services in primary care (Fig. 1) extends reach and affords ease of access [60, 73–77]. Higher levels are reserved for those with high-frequency, complex or rare headache disorders, perhaps complicated by comorbidities that require multidisciplinary care [28, 29, 66].
Fig. 1.
Graphic depiction of headache services organized on three levels, but based in primary care, with predicted caseloads (see text and Table 3 for explanation). Inset: arguably a better depiction
A model of headache-service organization
The focus of headache services should be on migraine and MOH (see above: Headache-related health care needs assessment [27–29]). This does not exclude other headache disorders, but TTH, the most prevalent headache, is almost always self-manageable [20, 28, 79] while other primary headaches are far less common. As for secondary headaches, their management is of the causative disorder, and therefore, with a few exceptions (notably MOH), outside the ambit of headache services. But provision is needed for their recognition, since this is the responsibility of the services to which affected patients present – most likely to be headache services when headache is the symptom.
While organized headache services, if they are to be efficient and equitable, must be embedded in national or regional health services, these vary throughout the world, differently structured and not always adequately resourced. The model proposed (Fig. 2; Table 3), incorporating three interdependent levels with facilitated but controlled pathways between them while expanding the contribution from primary care, is a general guide and template adaptable to these variations. It is the interventional model adopted as the health-care solution to headache by the Global Campaign against Headache [24, 25]. The account here develops and refines earlier proposals [27–29].
Fig. 2.
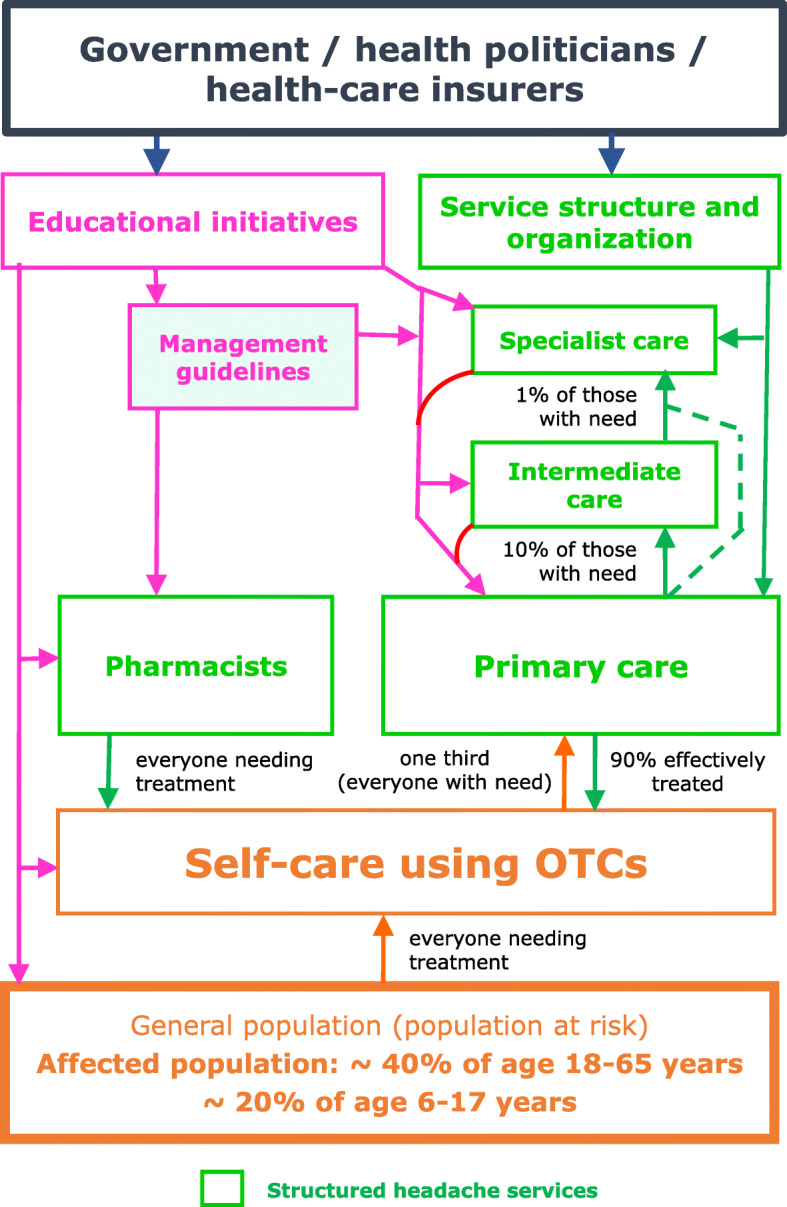
Template for structured headache services supported by educational initiatives, and expected patient flows (adapted and updated from [26, 27]; see text for explanation)
Table 3.
| Level 1. General primary care |
• front-line headache services (accessible first contact for most people with headache) • ambulatory care delivered in the community by primary health-care providers (physicians, clinical officers, nurses and/or community health workers) • referring when necessary, and (according to setting) acting as gatekeeper, to: |
| Level 2. Special-interest headache care |
• ambulatory care delivered by physicians, clinical officers or nurses with a special interest and additional training in headache, in primary or secondary care • referring when necessary to: |
| Level 3. Headache specialist centres | • advanced multidisciplinary care delivered by headache specialists in hospital-based centres |
Level 1. General primary care
Primary care is the front line of headache services (Figs. 1 and 2), available locally and accessible to all who need them. This is not everyone with headache: the estimated two thirds able to manage themselves (see above: Headache-related health care needs assessment) should do so, with advice from pharmacists and guidance from public educational programmes built into the model (see below: Educational implications).
Pharmacy services (perhaps level 0) need to be highlighted here. They are often greatly underutilized. Pharmacists are experts in the effects (wanted and unwanted) and uses of medications and generally the most easily accessible of all HCPs. Pharmacists can give guidance and advice not only on self-management but also on when further professional care should be sought [36].
Level 1 is provided by non-specialist HCPs, not necessarily physicians in a health-care system more dependent on other practitioners (clinical officers, nurses or community health workers, for example), although authority to prescribe is a requirement for non-OTC medications. Occupational health services can be a helpful adjunct, also provided in proximity to need (especially given the impact of headache on work). Whatever their background, HCPs providing level-1 care will need basic knowledge and understanding of headache disorders for this purpose, and many will therefore require some training in headache (see below: Educational implications). But the model does not require every HCP in primary care to offer headache services if they can share caseload between themselves according to their skills and interests, an arrangement that may be administratively easy in group practices or health centres.
Management aids designed to facilitate non-expert care are an important support to level 1 [20]. With these and the educational supports, this level should competently meet the needs of most people needing professional care for headache [28, 80]: most cases of migraine (and almost all of TTH, if needing care) can be diagnosed and managed here by HCPs who should be familiar with recommended acute and preventative drugs [30] and aware of the constraints in managing fertile women (important since these are a high proportion of people with migraine). Cluster headache, MOH and some other common secondary headache disorders listed in Table 4 should be recognized but not necessarily managed, and red-flag warnings of serious secondary headaches should also be recognized and duly acted upon [20]. Channels for referral to levels 2 and 3, urgently when necessary, should be in place for these cases, and for other patients who are diagnostically complex or difficult to manage [28, 29].
Table 4.
| Primary headache disorders | Secondary headache disorders |
|---|---|
|
1.1 Migraine without auraa 1.2 Migraine with auraa 1.2.3 Typical aura without headachea 2.1 Infrequent episodic tension-type headachea 2.2 Frequent episodic tension-type headachea 2.3 Chronic tension-type headache 3.1.1 Episodic cluster headache 3.1.2 Chronic cluster headache |
5.2.1 Chronic post-traumatic headache attributed to moderate or severe head injury 6.2.2 Headache attributed to subarachnoid haemorrhage 6.4.1 Headache attributed to giant cell arteritis 7.2 Headache attributed to low cerebrospinal fluid (CSF) pressure 7.4.1 Headache attributed to increased intracranial pressure or hydrocephalus caused by neoplasm 8.2 Medication-overuse headachea 9.1 Headache attributed to intracranial infection 10.3 Headache attributed to arterial hypertension 11.3.1 Headache attributed to acute glaucoma 13.1.1 Classical trigeminal neuralgia |
aManagement of most of these should be within the competence of level 1
Level 1 therefore controls flow to higher levels. There is more to be said about this (see below: The gatekeeper role within the model).
Finally, this level should continue the long-term care of patients discharged with treatment plans (as they should be) from levels 2 or 3 [28, 29, 66, 82].
Level 2. Special-interest headache care
Level 2 may be in primary care, provided by HCPs (usually but not essentially GPs), but in many countries it is more likely to be offered in secondary-care polyclinics or district hospitals and by neurologists (sometimes general physicians, specialists in other fields of internal medicine or psychiatrists). Either fits the model, with training in headache to a more advanced but not specialist level (see below: Educational implications).
Level 2 provides more skilled ambulatory care, and has capacity only for the relatively small proportion of patients needing this (Figs. 1 and 2, and see below: Division of caseload). Competence should embrace the diagnosis and management of more difficult cases of primary headache, with experience in using the full range of medications. It should extend to some secondary headache disorders, though not those that are very rare [66]. Ideally, HCPs at level 2 should have access to other services such as neuroimaging, psychology and physiotherapy. Where this is not possible, and anyway for the minority of their patients outside their competence (Table 5), they require a referral channel to level 3 [28, 29].
Table 5.
Patients likely to be referred to level 3 within optimally structured headache servicesa (adapted from [29])
| Patients with: | |
| • Refractory disabling headache of any type; | |
| • Cluster headache and other trigeminal autonomic cephalalgias, at first presentation; | |
| • High and low cerebrospinal fluid-pressure headaches; | |
| • Trigeminal and other cranial neuralgias or painful lesions of the cranial nerves; | |
| • Rare primary or secondary headaches; | |
| • Medication-overuse headache involving drugs of dependence, where personality mitigates against withdrawal of medication or where withdrawal attempts have failed; | |
| • Other probable or certain serious secondary headache; | |
| • Headaches with severe physical and/or psychological comorbidities. | |
| Cases of persisting diagnostic uncertainty. | |
| Patients in whom risk of serious underlying disorders demands specialist investigation. | |
| Patients who may participate in specific level-3 research projects (including clinical trials) [66]. |
adepending in some cases on the facilities and skills available at level 2
To maintain efficiency, level 2 should repatriate patients to level 1, with management plans, as soon as is clinically appropriate.
Level 3. Headache specialist centres
Specialized headache centres sit at the apex of structured headache services (Fig. 1) [66].
In many countries, they remain an unfulfilled aspiration; in others, they exist – disadvantageously to them – without the lower levels in place, or are inequitably distributed. As an example of the last, a survey in Brazil identified 243 “headache specialists” in 2004/2005. These were more than twice the number estimated to be needed for Brazil’s 198 million people [83] in a well-functioning 3-level system (see below: Division of caseload), but 68% were in the south-east region catering for only 42.6% of the country’s population; by contrast, 12.4% were in the north-east for 28.1%, and five of Brazil’s 27 States had none [84].
The first and foremost role of specialized headache centres, as tertiary referral centres, is to manage the very small proportions of patients with primary headache disorders that are especially difficult to diagnose or treat, or with secondary headaches requiring multidisciplinary management [81], and those who for other reasons, such as comorbidities, need specialist intervention [28, 66, 82, 85, 86] (Figs. 1 and 2; Table 5). For this role, they employ accredited headache specialists or neurologists, and concentrate experience in the rare headache disorders and cranial neuralgias [28, 66]. They have access to equipment and specialists in other disciplines for the diagnosis and management of the underlying causes of all secondary headache disorders [66]. They provide limited but full-time inpatient facilities (see below: Division of caseload). Specialized headache centres are therefore situated within or closely affiliated (with access rights) to a university or other major hospital [66].
In their second role, level-3 centres support non-specialists at levels 1 and 2 through clinical advice, training and development of national management guidelines [66]. Sustained through bidirectional links, this is a symbiotic relationship: well-functioning lower levels reduce demand on the very limited capacity at level 3. In this role, level 3 both maintains standards throughout the system and protects its ability to perform its first role.
Repatriation of patients to level 1 (or 2) as soon as is clinically appropriate also protects this ability. Again, this should be with management plans.
Less essential additional roles, including locally mandated or broader-based research, have been described [66].
Provision for children and adolescents
Although their needs may differ, the model of care is the same for these age groups, with front-line services (level 1) in primary care. To the extent that neurological services provide higher levels of care, these may be replaced by child neurology or paediatric services. The latter, in some countries, are better developed than neurological services.
Division of caseload
Quantitative estimates of the proportions of patients with care needs at each level are largely based on expert opinion [27–29], but with some empirical support [33]. They shape the model as a broad-based pyramid with a narrow apex (Fig. 1). Assuming all levels are in place and functioning efficiently, they predict 90% managed at level 1 and about 10% at higher levels, with no more than 1% of all headache patients at level 3 [28] (Fig. 2).
On these estimates and the earlier assumptions about consultation times (Table 1), one full-time equivalent (FTE) HCP at levels 1, 2 or 3 can provide care at those levels to populations no larger than 25,000, 200,000 and 2 million respectively [28, 29]. (One FTE HCP does not necessarily imply one engaged full-time in headache services; it could, for example, be two HCPs engaged half time in headache, or ten engaged for 10% of full time.)
For inpatients – the very few with difficult comorbidities, or with MOH requiring detoxication – a recommended minimum is two beds per million population [28].
The gatekeeper role within the model
The model expands the role of primary care, and shifts demand in structured services downwards towards it – a move that is both clinically appropriate and economically efficient [60, 73–77]. This brings into focus the gatekeeper role of primary care as an organizational element of the model [74, 82, 87–89]. It is a controversial role.
On the one hand, patients cannot be blamed for seeking direct access to perceived experts, and gatekeeping is not a norm in many countries’ health systems. On the other, ostensibly, gatekeeping guides patients along the “care pathway”, efficiently and in their best interests through the health system according to their needs, not their demands [87]. This is a well-intentioned purpose, although arguably somewhat paternalistic. In truth, gatekeeping is the means of preventing overload in specialist services, which would deny access to some who really need it. This is a more defensible consideration. But gatekeeping is also a means of cost containment, because specialist care is costly (especially when unnecessary). Gatekeeping therefore attracts a hostile perception as a means of rationing [87–89].
How essential is it? Health systems in which gatekeeping is the norm will accommodate it easily within headache services; others may not. More important in all cases, both to effectiveness of the model [88] and to the equity of it, is efficiency at the interfaces between levels (“seams in service continuity” [82, 89]), so that no delays are system-created against those who do need specialist care. Efficient interfaces are matters of implementation, best determined in the context of local health services. If the model is implemented well, with all levels in place and adequate provision at each, demand within the levels is likely to be self-regulating, effectively governed by waiting lists.
Flexibility of the model
Two principal factors determine how this model might be implemented in a country (or region or district): the resources allocated to headache services and the structure of the health service accommodating them. The model has considerable flexibility, allowing adaptations in many ways without altering its intrinsic structure (Table 6).
Fig. 3.
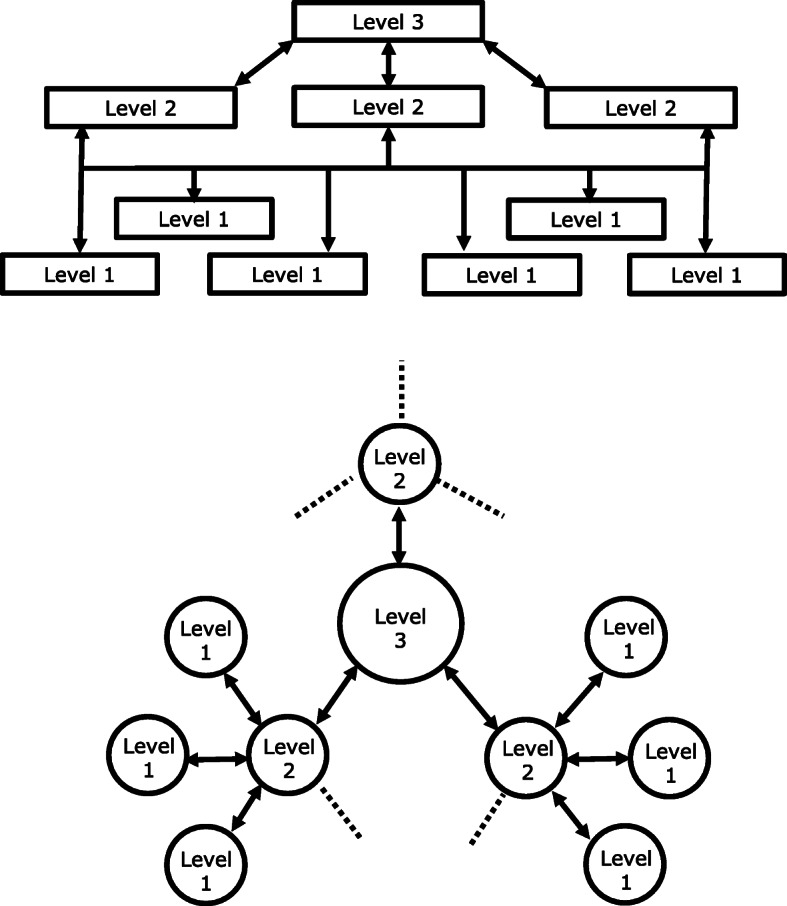
Layered (above) and hub-and-spoke (below) structures. The bi-directional arrows indicate patient flows from lower levels to higher, and clinical and educational supports from higher to lower. Each structure is amenable to top-down or bottom-up organization for integration within existing health services, although bottom-up is more likely in layered structures and top-down in hub-and-spoke. Hybrid structures are possible
Table 6.
Adaptability of the model according to local requirements and resources (adapted from [29])
| Requirement | Adaptation |
|---|---|
| Doctors vs other health-care providers (HCPs) | Many countries, as policy, are expanding the health-care roles of HCPs other than doctors. Systems in some countries may depend on service provision at level 1, and perhaps level 2, by clinical officers, nurses and/or community health workers. This is the way forward, supported by training, if the alternative is nothing. |
| Primary vs secondary care | Level 1 is in primary care. Level 2, on the other hand, can be in primary or secondary care: common options include neurologists or physicians (trained but non-specialist) in community or district hospitals or polyclinics. |
| 2-level systems | Level-3 centres are in secondary care (or tertiary care in countries that make this distinction). Level 3 is therefore costly and may be unaffordable. When it cannot be fully implemented within this model, or at all, this does not detract from the benefits that can be provided to the great majority by levels 1 and 2. |
| Combined levels |
Level 1 is by its nature community based. It is possible nonetheless, and may be appropriate, for certain level-2 centres also to offer local level-1 care. Similarly, there is no intrinsic reason why one centre cannot provide both level-2 and level-3 care. |
| Division of caseload | The 90:9:1% split between levels 1, 2 and 3 are estimates of need based largely on expert opinion. Throughout the world, there are variations in prevalence and characteristics of the common headache disorders, particularly in the frequency of medication-overuse headache [53]. The division of caseload between levels and capacity at each level may need adjustment, ideally based on locally gathered empirical data. The model will accommodate this without fundamental change. |
| Integration within existing services | The model adapts equally comfortably to layered and to hub-and-spoke structures, or hybrids of these, according to a country’s broader health-service structure. It permits bottom-up organization (patient flows driven upwards by demand at lower levels) or top-down (flows induced upwards by available capacity at higher levels) (Fig. 3). |
Table 7 provides illustrations of how, with these adaptations, it might be implemented in various countries.
Table 7.
Illustrations of how the model might be implemented, with adaptations, in various countries
| Country | World Bank income level [67] | Model levels | Structure | Proposed organization (placement of levels and provision of care) | Comments |
|---|---|---|---|---|---|
| Abu Dhabi | High | 3 | Layered, bottom-up |
Level-1 services provided by GPs in each State-owned primary health-care centre. Level-2 services provided either by GPs in selected primary health-care centres, or by hospital-based neurologists. A single level-3 centre in a specialist neurology department within a hospital-based multidisciplinary health-care facility. |
Total population is about 1.5 million. There are 27 State-owned primary health-care centres, but 500 GPs, many in the private sector. |
| Azerbaijan | Upper-middle | 3 | Hybrid system, bottom-up |
Level-1 services provided in remote rural areas by GPs in primary care, in urban areas by GPs in ambulatory-polyclinic services. Level-2 services provided either in the same polyclinics, where so-called district therapists/GPs can redirect to a neurologist (or to level 3), or by neurologists working in private clinics or outpatient clinics in private hospitals. Level-3 services provided in central regional hospitals with neurological beds. |
Neurologists at level 2 can provide clinical and educational support to GPs in their locality in a hub-and-spoke arrangement. |
| Brazil | Upper-middle | 3 | Layered, bottom-up |
Level-1 services provided in the community by GPs in primary care. Level-2 services provided by neurologists working either in the community or in hospital-based secondary care. Level-3 services provided by neurological centres, often university-based, in the larger cities. |
Total population is 210 million (70% covered by public health services, 25% by supplementary health services, 5% uncovered), served by 35,000 GPs, 5000 neurologists and 500 (uncertified) “headache specialists”. Despite apparently adequate capacity at all levels (albeit unevenly distributed geographically [84]), fewer than 5% of candidates for migraine preventative drugs currently receive them [90]. |
| Bulgaria | Upper-middle | 3 | Layered, bottom-up |
Level-1 services provided in the community by GPs in primary care. Level-2 services provided by neurologists working either in the community or in hospital-based secondary care. Level-3 services provided by neurological centres, often university-based, in the larger cities. |
Well-developed primary care operating a gatekeeper role, but GPs currently cannot prescribe many drugs without a specialist diagnosis. |
| China | Upper-middle | 3 | Hub and spoke, top down |
Level-3 services provided by neurologists in provincial or university hospitals. Level-2 services provided by neurologists in county, district or municipal hospitals. Level-1 services provided by GPs in community health centres or rural clinics or hospitals. |
This system is implemented in parts of the country [91]. Medical facilities at all levels provide either Western or Traditional Chinese medicine. |
| Colombia | Upper-middle | 3 | Layered, bottom-up |
Level-1 services provided in the community by GPs in primary care. Level-2 services provided by neurologists in hospital-based secondary care in intermediate and larger cities. Level-3 services provided by neurological centres, often university-based, in the larger cities |
Services are overseen by the State but insurance-based, provided by multiple private or public companies, each with different organizations. Currently, there is a lack of neurologists, with most located only in larger cities [92, 93]. Neurological conditions in general are not a listed priority for the health-care system [94]. |
| Estonia | High | 3 | Layered, bottom-up |
Level-1 services provided in the community by GPs in primary care. Level-2 services provided by neurologists working in regional/county hospitals in private or public sectors. Level-3 services provided by a subspecialty division of a university-based hospital neurology department. |
Total population is about 1.3 million. There is only one university-based hospital in the country, which provides all level-3 services. |
| Ethiopia | Low | 2 | Layered, bottom-up |
Level-1 services provided in the community by community health workers, nurses, clinical officers and GPs in rural health posts, local health centres and primary hospitals. Level-2 services provided by GPs, internists and neurologists working either in secondary-care general hospitals in district towns or in tertiary-care specialized university-based hospitals in larger cities. |
Total population is estimated at 114 million, with the majority still using traditional medicines despite increasing health-service coverage. The gatekeeper role can be effectively integrated into the existing health-service system by training HCPs in primary care. |
| Georgia | Upper-middle (recently upgraded from lower-middle) | 2 | Layered, top down |
Level-2 services provided by headache-trained neurologists in private headache clinics in major cities. Level-1 and some level-2 services provided by GPs or neurologists in urban health-care facilities elsewhere. |
A system of interdependent private headache clinics currently operates outside the State system [95]: there is no State-supported alternative, and primary care is poorly developed. Level-3 centres are aspirational. |
| Greece | High | 3 | Layered, bottom-up |
Level-1 services provided by GPs in private or public health-care sectors. Level-2 services provided by neurologists in private or public settings. Level-3 centres provided by headache specialists in neurology departments within hospital-based multidisciplinary health-care facilities. |
Many people with headache are currently un- or under-treated. A 2018 national general population survey by the Hellenic Headache Society (HHS) found that one fifth seek professional care, most commonly from private neurologists [65]. Under the umbrella of HHS there are, currently, 14 headache centres in the public sector, three academic (level 3) [96]. |
| Iceland | High | 3 | Layered, bottom-up |
Level-1 services provided by GPs in primary health-care centres. Level-2 services provided by GPs with a special interest and neurologists in district health-care institutions. Level-3 services provided by headache specialists in hospitals providing specialist services. |
Population is 364,000, served by 12 district health-care institutions and two university or teaching hospitals, both providing general and specialized services. |
| India (Karnataka State) | Lower-middle | 3 | Hub and spoke, top down |
A single level-3 centre in the National Institute of Mental Health and Neurosciences (NIMHANS) in Bangalore. Level-2 services provided by physicians with training in headache in affiliated district or subdistrict hospitals. Level-1 services provided in urban areas by GPs in health centres and in rural areas by medical officers in community health centres and primary health centres and by health workers in subcentres. Where available, pharmacists may provide level-1 care. |
State health care is primary (in community and primary health centres), secondary (in sub-district hospitals) and tertiary (in district hospitals and medical colleges). Many people favour traditional remedies. The hub-and-spoke top-down system promotes the educational and clinical supportive roles of the level-3 centre to levels below. |
| Iran | Upper-middle | 3 | Layered, bottom-up |
Level-1 services provided by GPs in the community or in primary-care centres. Level-2 services provided by neurologists working either in the community or in hospital-based secondary care. Level-3 services provided by neurological centres, often university-based, in the larger cities. |
Services are supported in governmental centres and hospitals, but there are also many private clinics. |
| Italy | High | 3 | Layered, bottom-up |
Level-1 services provided by GPs in primary care. Level-2 services provided by hospital- or clinic-based neurologists or other specialists with interest in headache in public or private sectors. Level-3 services provided in academic hospital-based centres by headache specialists working in multidisciplinary teams. |
Italy’s Health Care System is national but also regulated at its 21 regional levels. Its population of 60 million is served by more than 80 headache and migraine centres (public, private but recognized for reimbursement, or fully private). National legislation [97] recognizes chronic primary headache disorders as disabling and requiring care. |
| Mali | Low | 3 | Layered, bottom-up |
Level-1 services provided by doctors, nursing assistants and health technicians in community health centres. Level-2 services provided by GPs and internists, nurses and health technicians in reference health centres at district level or in regional hospitals. Level-3 services provided by specialists in national hospitals and university hospital centres. |
Mali’s health services are built on 4 levels in a pyramid structure: community health centres at level 1 (community); reference health centres at level 2 (district); regional hospitals at level 3; national and university hospitals at level 4. In Mali, health systems must accommodate simultaneous use of conventional and traditional medicines to respect long-established cultural preferences and practices. Finding the right formula to integrate these remains a challenge in health services generally. |
| Mongolia | Lower-middle | 3 | Layered, bottom-up |
Level-1 services provided by GPs in primary health-care centres or soum health centres and inter-soum hospitals. Level-2 services provided by neurologists in aimag- or district-based hospitals. Level-3 services provided by neurologists in central State hospitals. |
Aimags are first-level administrative divisions, soums are second-level. Total population is 3.3 million, with primary care services reaching 70%. Many people favour traditional remedies. Level 3 currently is largely aspirational because of a lack of headache specialists. |
| Morocco | Lower-middle | 3 | Hybrid system in public sector with layered bottom-up and hub-and-spoke top-down elements; top-down in private sector |
Level-3 services provided by neurologists in regional and university hospitals or in private hospitals. Level-2 services provided by neurologists and GPs with special interest in district clinics or provincial hospitals or in private practices. Level-1 services provided by GPs in public primary health-care centres or private practices, or, in some rural areas, by nurses. |
Morocco has a mix of HCPs: public (State-sponsored and free) and private (reimbursed through insurance or paid out-of-pocket). Primary care has a gatekeeper function, which is not always respected, while access to specialists is direct in private care. Through telemedicine, specialists in Morocco reach and advise patients living far from regional hospitals, a hub-and-spoke system that can also provide clinical and educational support to non-specialists at lower levels. |
| Nepal (Bagmati Province, Kavre District) | Lower-middle (recently upgraded from low) | 3 | Hub and spoke, top down |
A single level-3 headache centre in Dhulikhel hospital, Kathmandu University Hospital (DH-KUH). Level-2 services provided by clinical officers and/or physicians in DH-KUH’s outreach health centres. Level-1 services provided by community health workers in outreach primary care centres or health posts. |
Outreach health centres are around 20 in number in and around Kavre and adjoining districts. Many people favour traditional remedies. Countrywide, level 3 is currently aspirational in a geographically diverse country with major accessibility challenges [98] but, in a population survey, over half of adults with headache had engaged with HCPs of varying sorts [42], indicating capacity to build on. |
| Norway | High | 3 | Layered, bottom up |
Level-1 services provided by GPs in primary care. Level-2 services provided by neurologists (and nurses) working in hospital-based neurological departments, or neurologists or GPs with special interest in headache working outside hospitals. Level-3 services provided by headache specialists and nurses in academic hospitals, working in multidisciplinary teams. |
A process to establish a national system for headache care is commencing now in collaboration with the Norwegian Ministry of Health. |
| Pakistan | Lower-middle | 3 | Hub and spoke, top down |
Level-3 services provided by headache-trained neurologists in private and public tertiary health centres. Level-2 services provided by neurologists in private headache clinics in larger cities. Level-1 and some level-2 services provided by neurologists and GPs in urban, suburban and rural health-care facilities and clinics. |
Public health-system infrastructure is fragmented, but both private and public level-3 services exist in larger cities. Most adults seeking headache treatments go first to GPs, but direct access to specialists is available in both public and private sectors. Therefore, level-1 and level-2 services may currently be provided by neurologists or specialists. A hub-and-spoke top down model, especially with the use of telemedicine, can boost education and support for GPs and remote practice locations, thereby improving service structure and reducing inappropriate demand at level 3. |
| Perú | Upper-middle | 3 | Layered, bottom-up in public sector; unstructured in private sector |
Level-1 services provided by GPs, nurses, nursing assistants and pharmacists in primary-care health centres. Level-2 services provided by neurologists in regional hospitals and private clinics. Level-3 services provided by specialist accredited neurologists (neurology services are subdivided into areas of care, including headache) in hospitals and institutes providing high-complexity care in departmental capital cities. |
Perú is multicultural, with 31 million population. Its decentralized health-care system is administered by five entities (Ministry of Health, Social Health Insurance, Armed Forces, National Police and the private sector) and suffers from low investment and lack of horizontal integration. As in most of Latin America, headache has low priority. Many (doctors and general public) believe only neurologists can resolve it. Structured headache services offer solutions to these challenges, with technological supports (telemedicine can overcome geographic and economic obstacles to transfer of patients). |
| Portugal | High | 3 | Layered, bottom up |
Level-1 services provided by GPs in primary health-care centres. Level-2 services provided by neurologists in referral hospitals (community hospitals). Level-3 services provided by neurologists with specialist training in headache in central and/or academic hospitals. |
Well-developed occupational medicine services ally efficiently and helpfully with community health services. |
| Russia | Upper-middle | 3 | Layered, bottom up |
Level-1 services provided by GPs in primary health-care centres or district-based polyclinics. Level-2 services provided by neurologists in each regional centre. Level-3 services provided by neurologists with specialist training in headache in each interregional municipal centre. |
Russia has 147 million people, 565,200 physicians, 28,600 neurologists, > 50 tertiary headache centres (mostly private) and about 200 “headache specialists” [99]. Up to half of people with headache consult a physician, most often a neurologist, yet fewer than 1% with migraine use preventative medications [100]. Russia is only slowly divesting itself of arcane traditions in clinical practice, exemplified in headache management by entrenched preferences for vasoactive, nootropic and so-called neuroprotector drugs instead of evidence-based preventative drugs [101]. Ministry of Health recommendations for management of migraine [102] and mandatory inclusion of headache care in under- and postgraduate medical education are addressing care deficiencies nationally, but a headache-service implementation project in Sverdlovsk Oblast (Yekaterinburg) lacks government support [103]. |
| Saudi Arabia (National Guard Health Affairs [NGHA]) | High | 2/3 | Layered, bottom up |
Level-1 services provided by GPs in primary health centres. Levels 2 and 3 are hospital-based, provided by neurologists, sometimes in specialized clinics. |
NGHA offers one of Saudi Arabia’s health-care systems, with two medical cities, five hospitals and over 70 primary health-care centres providing full coverage for employees and their dependants. Additionally, it offers services to the general public for certain diseases and for emergencies (providing about 50% of their secondary and tertiary care, to 1.7 million people). |
| Serbia | Upper-middle | 3 | Layered, bottom up |
Level-1 services provided by GPs in public health centres. Level-2 services provided by neurologists working either in a polyclinic system within the same public health centres or in local hospitals. Level-3 services provided by specialists in neurological centres, usually academic, located in the larger cities. |
Well-developed primary care with a gatekeeper role but, currently, many medications cannot be prescribed by GPs without diagnosis by a neurologist, and many are not reimbursed. |
| Turkey | Upper-middle | 3 | Layered, bottom up |
Level-1 services provided by GPs in public health centres. Level-2 services provided by neurologists in private or government polyclinics. Level-3 services provided by neurologists with specialist training in headache in private or government university headache centres. |
Government-funded Medicaid provides free health insurance to all but is under-resourced. Not all drugs are reimbursed, while GPs in level 1 currently cannot prescribe all medications, and tend to over-prescribe analgesics. The consequence is too many patients in level-2, many with medication-overuse headache. |
| United Kingdom | High | 3 | Layered, bottom up |
Level-1 services provided by GPs in each practice. Level-2 services provided by GPs with special interest (GPwSIs), sometimes with support from specialist nurse practitioners, or by neurologists based in or visiting district hospitals. Level-3 centres staffed by specialists, often supported by nurse practitioners, in neurology departments within selected multidisciplinary hospitals. |
The gatekeeper role of primary care is entrenched. GPwSIs in particular fields are appointed for local areas with the purpose of avoiding unnecessary referrals to specialist care, or by local commissioning groups as local or regional leads, or by larger group practices to take a lead role within the practice [104]. |
| United States of America (Medicaid system) | High | 3 | Layered, bottom up |
Level-1 services provided by primary care physicians. Level-2 services provided by neurologists. Level-3 services provided by specialists within neurology departments, typically in university settings. |
Medicaid (funded jointly by Federal and State governments but run by each State separately) provides free health insurance to 74 million people whose income and resources are insufficient to pay for health care. Existing Federal adult and childhood quality-of-care measures do not include headache outcome measures. Adding these could educate providers and improve usage of layered headache care, with better outcomes expected. Telemedicine referrals from rural areas could be employed between levels 1 and 2 in each State, and for follow up. |
| Zambia | Lower-middle | 3 | Layered, bottom up |
Level-1 services provided in urban areas in district hospitals by clinical officers, with or without a physician, and in rural areas by clinical officers and community health workers in community health centres or rural health posts. Level-2 services provided by physicians or clinical officers in provincial or general hospitals. Level-3 services provided by neurologists in the country’s level-3 hospitals (usually university-affiliated). |
These levels correspond with the 3 levels of State-provided health care, in which clinical officers substantially outnumber doctors. Level 3 is only recently a possibility with the graduation of Zambia’s first adult and paediatric neurologists. In the near-term, very small numbers of these specialists will severely limit level-3 capacity, increasing dependence on level 2. |
GP General practitioner, HCP Health-care provider
Educational implications
Public education has three main purposes. Firstly, it is needed to improve people’s understanding of headache. Secondly, it should explain the use and limitations of OTC medication [79] while warning against self-mismanagement, the attendant dangers of medication overuse and the unsupervised purchase of analgesics from supermarkets and other unlicensed outlets rather than from pharmacists. Thirdly, it should explain how to make appropriate use of headache services, what to expect from them and, in this context, the likely futility of non-adherence [105, 106].
WHO identified professional education as the most pressing requirement in headache services improvement [22]. Separate educational initiatives are required at each level. Pharmacists are not generally expected to diagnose, having neither the training nor the facilities required, but they should have the knowledge to recognise treatment failures and incipient or established medication overuse [79]. Limited knowledge is required at level 1 [28, 64], but better than usually exists. Enhanced but still non-specialist knowledge is needed in level 2 [28]. In both, education should be coupled with availability – and use – of evidence-based guidelines [20, 64, 107, 108] adapted to local resource availability. Specialist expertise and competence are expected in level 3, gained through high-level training and maintained through practice, continuous professional development and participation in professional networks (national or international) allowing exchange of ideas and experience [66]. In the USA, the United Council for Neurologic Subspecialities (UCNS) offers examination-based certification (and recertification) in headache medicine as a subspecialty [109], although there is no requirement for a physician practising as a “headache specialist” to be certified [110]. For some countries, training at this level will require attendance at specialist centres abroad. Several schemes exist for this. The University of Copenhagen and Danish Headache Centre, and Sapienza University in Rome, both offer Master degree courses in headache medicine, open to students from all countries [111, 112]. Training scholarships are offered by the International Headache Society (IHS) [113] and EHF (EHF-SAS [114]).
The major political and logistic implications of these requirements, especially at level 1 in view of the numbers of HCPs who need training, are probably the greatest barrier to nationwide implementation. Far-reaching national training must be part and parcel of effective headache-service reform, and it needs to commence in medical schools. Within the 3-level care system proposed, a training role for each higher level towards the level below can be envisaged (Fig. 2). The entire structure may depend upon these roles being developed.
A comment on service quality
Effective service implementation does not of itself guarantee quality of care. Quality-assurance measures are necessary, as in all fields of medicine.
Standards and indicators exist for headache service quality evaluation (SQE), developed by LTB specifically to support implementation of structured headache services [108]. They are themselves undergoing evaluation at the various levels [66, 115–118].
A comment on cost
Headache services delivering care equitably and nationwide to large numbers of people will undoubtedly enhance the headache patients’ journey and improve outcomes. They will also consume substantial health-care resources, and require major up-front investment. Cost-effectiveness becomes a key consideration. While preliminary economic analyses are highly favourable [21], there is a cost incurred by doing nothing.
There is promise of even greater savings to offset the cost – if improvements to services recover the lost productivity due to headache, or even a small part of it [11–19, 22]. This promise needs testing in formal economic analyses. If it proves to be sound, these savings foregone as a result of doing nothing become the financial penalty of inaction [29].
Concluding remarks
Many problems beset the current compartmentalized division of headache services between primary, secondary and tertiary care. The model described seeks vertical integration. It recognizes that the demand for headache care dictates delivery for the most part in primary care, and that this is a perfectly good way forward in terms of accessibility and effectiveness of care. The model is amenable to horizontal integration with other care services, and capable of adaptation to suit local cultures and health-care systems.
The need for better – and better resourced – headache services exists in all countries, differing only quantitatively. At a time when momentum is again developing for health-service reform diverting resources from secondary to primary care [60, 77], there is opportunity for change. In low- and middle-income countries in particular, the growing shift of emphasis in health policy towards chronic non-communicable diseases [119] creates a fair climate for change.
Political will, needed for change to happen [9, 22, 60], will be driven by economic (cost-effectiveness) analyses. These, so far, have been highly encouraging [21], but more thorough evaluations are needed.
Acknowledgements
Not applicable.
Abbreviations
- EHF
European Headache Federation
- EU
European Union
- FTE
Full-time equivalent
- GBD
Global burden of disease (study)
- GDP
Gross domestic product
- GP
General practitioner
- HCP
Health-care provider
- ICHD
International classification of headache disorders
- IHS
International Headache Society
- LTB
Lifting The Burden
- MOH
Medication-overuse headache
- OTC
Over-the-counter
- TTH
Tension-type headache
- UdH
Undifferentiated headache
- UK
United Kingdom
- USA
United States of America
- USSR
Union of Soviet Socialist Republics
- WHO
World Health Organization
Authors’ contributions
TJS, RJ, ZK and LJS developed the model from earlier proposals, with contributory input from DU, MLi, JO, KP and MTi, as a product of the Global Campaign against Headache conducted by LTB. All other authors contributed to its refinement. ZK, LJS, DU, LA, MAlJ, AMAlK, MA, MB, SB, JHE, RG-G, JBG-G, LSG, AAH, NKa, NKi, GBK, ERL, MLe, OL, YM, IM, DDM, TM, VO, KP, MFPP, GQ, GNR, AR, ERdlT, DS, MTo, S-YY, MZ, YZZ and JZ-T provided input based on local knowledge and expertise into adaptations of the model for various countries. TJS drafted the manuscript. All authors contributed to manuscript revision and approved the final version.
Funding
None.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
TJS, RJ, ZK, LJS and DU are the Directors and Trustees of Lifting The Burden. Otherwise, no author declares a conflict of interest in relation to the content of this manuscript.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Stovner LJ, Hagen K, Jensen R, Katsarava Z, Lipton R, Scher AI, Steiner TJ, Zwart J-A. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27(3):193–210. doi: 10.1111/j.1468-2982.2007.01288.x. [DOI] [PubMed] [Google Scholar]
- 2.Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J, Ackerman I, Aggarwal R, Ahn SY, Ali MK, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Bahalim AN, Barker-Collo S, Barrero LH, Bartels DH, Basáñez MG, Baxter A, Bell ML, Benjamin EJ, Bennett D, Bernabé E, Bhalla K, Bhandari B, Bikbov B, Bin Abdulhak A, et al. Years lived with disability (YLD) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, Charlson F, Davis A, Degenhardt L, Dicker D, Duan L, Erskine H, Feigin VL, Ferrari AJ, Fitzmaurice C, Fleming T, Graetz N, Guinovart C, Haagsma J, Hansen GM, Hanson SW, Heuton KR, Higashi H, Kassebaum N, Kyu H, Laurie E, Liang X, Lofgren K, Lozano R, MacIntyre MF, Moradi-Lakeh M, Naghavi M, Nguyen G, Odell S, Ortblad K, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2015;386(9995):743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.GBD 2015 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016;388(10053):1545–1602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vos T, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, Abdulkader RS, Abdulle AM, Abebo TA, Abera SF, Aboyans V, Abu-Raddad LJ, Ackerman IN, Adamu AA, Adetokunboh O, Afarideh M, Afshin A, Agarwal SK, Aggarwal R, Agrawal A, Agrawal S, Ahmadieh H, Ahmed MB, Aichour MTE, Aichour AN, Aichour I, Aiyar S, Akinyemi RO, Akseer N, Al Lami FH, Alahdab F, Al-Aly Z, Alam K, Alam N, Alam T, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2017;390(10100):1211–1259. doi: 10.1016/S0140-6736(17)32154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stovner LJ, Nichols E, Steiner TJ, Abd-Allah F, Abdelalim A, Al-Raddadi RM, Ansha MG, Barac A, Bensenor IM, Doan LP, Edessa D, Endres M, Foreman KJ, Gankpe FG, Gururaj G, Goulart AC, Gupta R, Hankey GJ, Hay SI, Hegazy MI, Hilawe EH, Kasaeian A, Kassa DH, Khalil I, Khang Y-H, Khubchandani J, Kim YJ, Kokubo Y, Mohammed MA, Moradi-Lakeh M, Nguyen HLT, Nirayo YL, Qorbani M, Ranta A, Roba KT, et al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. 2018;17(11):954–976. doi: 10.1016/S1474-4422(18)30322-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392:1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.GBD 2019 Diseases and Injuries Collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steiner TJ, Stovner LJ, Vos T, Jensen R, Katsarava Z. Migraine is first cause of disability in under 50s: will health politicians now take notice? [editorial] J Headache Pain. 2018;19(1):17. doi: 10.1186/s10194-018-0846-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steiner TJ, Gururaj G, Andrée C, Katsarava Z, Ayzenberg I, Yu SY, Al Jumah M, Tekle-Haimanot R, Birbeck GL, Herekar A, Linde M, Mbewe E, Manandhar K, Risal A, Jensen R, Queiroz LP, Scher AI, Wang SJ, Stovner LJ. Diagnosis, prevalence estimation and burden measurement in population surveys of headache: presenting the HARDSHIP questionnaire. J Headache Pain. 2014;15(1):3. doi: 10.1186/1129-2377-15-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hu XH, Markson LE, Lipton RB, Stewart WF, Berger ML. Burden of migraine in the United States: disability and economic costs. Arch Intern Med. 1999;159(8):813–818. doi: 10.1001/archinte.159.8.813. [DOI] [PubMed] [Google Scholar]
- 12.Selekler MH, Gökmen G, Steiner TJ. Productivity impact of headache on a heavy-manufacturing workforce in Turkey. J Headache Pain. 2013;14(1):88. doi: 10.1186/1129-2377-14-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Linde M, Gustavsson A, Stovner LJ, Steiner TJ, Barré J, Katsarava Z, Lainez JM, Lampl C, Lantéri-Minet M, Rastenyte D, Ruiz de la Torre E, Tassorelli C, Andrée C. The cost of headache disorders in Europe: the Eurolight project. Eur J Neurol. 2012;19(5):703–711. doi: 10.1111/j.1468-1331.2011.03612.x. [DOI] [PubMed] [Google Scholar]
- 14.Raggi A, Leonardi M. Burden and cost of neurological diseases: a European north-south comparison. Acta Neurol Scand. 2015;132(1):16–22. doi: 10.1111/ane.12339. [DOI] [PubMed] [Google Scholar]
- 15.Raggi A, Leonardi M. Burden of brain disorders in Europe in 2017 and comparison with other non-communicable disease groups. J Neurol Neurosurg Psychiatry. 2020;91(1):104–105. doi: 10.1136/jnnp-2019-320466. [DOI] [PubMed] [Google Scholar]
- 16.Steiner TJ, Rao GN, Kulkarni GB, Gururaj G, Stovner LJ. Headache yesterday in Karnataka state, India: prevalence, impact and cost. J Headache Pain. 2016;17(1):74. doi: 10.1186/s10194-016-0669-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yu S, Liu R, Zhao G, Yang X, Qiao X, Feng J, Fang Y, Cao X, He M, Steiner T. The prevalence and burden of primary headaches in China: a population-based door-to-door survey. Headache. 2012;52(4):582–591. doi: 10.1111/j.1526-4610.2011.02061.x. [DOI] [PubMed] [Google Scholar]
- 18.Ayzenberg I, Katsarava Z, Sborowski A, Chernysh M, Osipova V, Tabeeva G, Steiner TJ. Headache-attributed burden and its impact on productivity and quality of life in Russia: structured healthcare for headache is urgently needed. Eur J Neurol. 2014;21(5):758–765. doi: 10.1111/ene.12380. [DOI] [PubMed] [Google Scholar]
- 19.Mbewe E, Zairemthiama P, Paul R, Birbeck GL, Steiner TJ. The burden of primary headache disorders in Zambia: national estimates from a population-based door-to-door survey. J Headache Pain. 2015;16(1):36. doi: 10.1186/s10194-015-0513-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Steiner TJ, Jensen R, Katsarava Z, Linde M, MacGregor EA, Osipova V, Paemeleire K, Olesen J, Peters M, Martelletti P, on behalf of the European Headache Federation and Lifting The Burden: the Global Campaign against Headache (2019) Aids to management of headache disorders in primary care (2nd edition). J Headache Pain 20:57 [DOI] [PMC free article] [PubMed]
- 21.Linde M, Steiner TJ, Chisholm D. Cost-effectiveness analysis of interventions for migraine in four low- and middle-income countries. J Headache Pain. 2015;16(1):15. doi: 10.1186/s10194-015-0496-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization and Lifting The Burden (2011) Atlas of headache disorders and resources in the world 2011. WHO, Geneva Available at: http://www.who.int/mental_health/management/atlas_headache_disorders/en/2011
- 23.Katsarava Z, Steiner TJ. Neglected headache: ignorance, arrogance or insouciance? [editorial] Cephalalgia. 2012;32(14):1019–1020. doi: 10.1177/0333102412459478. [DOI] [PubMed] [Google Scholar]
- 24.Steiner TJ. Lifting the burden: the global campaign against headache. Lancet Neurol. 2004;3(4):204–205. doi: 10.1016/S1474-4422(04)00703-3. [DOI] [PubMed] [Google Scholar]
- 25.Steiner TJ. Lifting The Burden: the global campaign to reduce the burden of headache worldwide. J Headache Pain. 2005;6(5):373–377. doi: 10.1007/s10194-005-0241-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lifting The Burden. The global campaign against headache. http://www.l-t-b.org. Accessed 6 June 2021
- 27.Antonaci F, Valade D, Lanteri-Minet M, Láinez JM, Jensen J, Steiner TJ (2008) Proposals for the organisation of headache services in Europe. Intern Emerg Med 3:S25–S28 [DOI] [PubMed]
- 28.Steiner TJ, Antonaci F, Jensen R, Lainez MJ, Lanteri-Minet M, Valade D. Recommendations for headache service organisation and delivery in Europe. J Headache Pain. 2011;12(4):419–426. doi: 10.1007/s10194-011-0320-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steiner TJ, Jensen R, Katsarava Z, Uluduz D, Tinelli M, Thomas H, Stovner LJ. The healthcare solution to headache. Ch 15. In: Steiner TJ, Stovner LJ, editors. Societal impact of headache. Burden, costs and response. Cham: Springer Nature; 2019. pp. 203–224. [Google Scholar]
- 30.European Headache Federation. https://ehf-org.org. Accessed 6 June 2021
- 31.Hopkins A, Menken M, De Friese GA. A record of patient encounters in neurological practice in the United Kingdom. J Neurol Neurosurg Psychiatry. 1989;52(4):436–438. doi: 10.1136/jnnp.52.4.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wiles CM, Lindsay M. General practice referrals to a department of neurology. J Roy Coll Physicians. 1996;30:426–431. [PMC free article] [PubMed] [Google Scholar]
- 33.Laughey WF, Holmes WF, MacGregor AE, Sawyer JPC. Headache consultation and referral patterns in one UK general practice. Cephalalgia. 1999;19:328–329. doi: 10.1046/j.1468-2982.1999.019007692.x. [DOI] [Google Scholar]
- 34.Tfelt-Hansen P. Review. Pharmacological strategies to treat attacks of episodic migraine in adults. Exp Opin Pharmacother. 2020;22(3):305–316. doi: 10.1080/14656566.2020.1828347. [DOI] [PubMed] [Google Scholar]
- 35.Lipton RB, Scher AI, Steiner TJ, Kolodner K, Liberman J, Stewart WF. Patterns of health care utilization for migraine in England and in the United States. Neurology. 2003;60(3):441–448. doi: 10.1212/WNL.60.3.441. [DOI] [PubMed] [Google Scholar]
- 36.Mehuys E, Paemeleire K, Van Hees T, Christiaens T, Van Bortel LM, Van Tongelen I, De Bolle L, Remona J-P, Boussery K. Self-medication of regular headache: a community pharmacy-based survey. Eur J Neurol. 2012;19(8):1093–1099. doi: 10.1111/j.1468-1331.2012.03681.x. [DOI] [PubMed] [Google Scholar]
- 37.Edmeads J. Understanding the needs of migraine patients. Drugs. 2006;66:1–8. doi: 10.2165/00003495-200666003-00002. [DOI] [Google Scholar]
- 38.Takeshima T, Ishizaki K, Fukuhara Y, Ijiri T, Kusumi M, Wakutani Y, Mori M, Kawashima M, Kowa H, Adachi Y, Urakami K, Nakashima K. Population-based door-to-door survey of migraine in Japan: the Daisen study. Headache. 2004;44(1):8–19. doi: 10.1111/j.1526-4610.2004.04004.x. [DOI] [PubMed] [Google Scholar]
- 39.Radtke A, Neuhauser H. Prevalence and burden of headache and migraine in Germany. Headache. 2009;49(1):79–89. doi: 10.1111/j.1526-4610.2008.01263.x. [DOI] [PubMed] [Google Scholar]
- 40.Katsarava Z, Mania M, Lampl C, Herberhold J, Steiner TJ. Poor medical care for people with migraine in Europe – evidence from the Eurolight study. J Headache Pain. 2018;19(1):10. doi: 10.1186/s10194-018-0839-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ayzenberg I, Katsarava Z, Sborowski A, Obermann M, Chernysh M, Osipova V, Tabeeva G, Steiner TJ. Headache yesterday in Russia: its prevalence and impact, and their application in estimating the national burden attributable to headache disorders. J Headache Pain. 2015;16(1):7. doi: 10.1186/1129-2377-16-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Manandhar K, Risal A, Linde M, Steiner TJ. Health-care utilization for headache disorders in Nepal: a population-based door-to-door survey. J Headache Pain. 2018;19(1):116. doi: 10.1186/s10194-018-0942-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang SJ, Fuh JL, Young YH, Lu SR, Shia BC. Frequency and predictors of physician consultations for headache. Cephalalgia. 2001;21(1):25–30. doi: 10.1046/j.1468-2982.2001.00138.x. [DOI] [PubMed] [Google Scholar]
- 44.Lampl C, Buzath A, Baumhackl U, Klingler D. One-year prevalence of migraine in Austria: a nation-wide survey. Cephalalgia. 2003;23(4):280–286. doi: 10.1046/j.1468-2982.2003.00509.x. [DOI] [PubMed] [Google Scholar]
- 45.Lipton RB, Scher AI, Kolodner K, Liberman J, Steiner TJ, Stewart WF. Migraine in the United States: epidemiology and patterns of health care use. Neurology. 2002;58(6):885–894. doi: 10.1212/WNL.58.6.885. [DOI] [PubMed] [Google Scholar]
- 46.Edmeads J, Findlay H, Tugwell P, Pryse-Phillips W, Nelson RF, Murray TJ. Impact of migraine and tension-type headache on life-style, consulting behaviour, and medication use: a Canadian population survey. Can J Neurol Sci. 1993;20(2):131–137. doi: 10.1017/S0317167100047697. [DOI] [PubMed] [Google Scholar]
- 47.Liu R, Yu S, He M, Zhao G, Yang X, Qiao X, Feng J, Fang Y, Cao X, Steiner TJ. Health-care utilization for primary headache disorders in China: a population-based door-to-door survey. J Headache Pain. 2013;14(1):47. doi: 10.1186/1129-2377-14-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Steiner T, Lange R, Voelker M. Episodic tension-type headache (ETTH): evidence of prolonged disability from a placebo-controlled comparison of aspirin and paracetamol. Cephalalgia. 2003;23:630. doi: 10.1046/j.1468-2982.2003.00470.x. [DOI] [PubMed] [Google Scholar]
- 49.Salomon JA, Haagsma JA, Davis A, de Noordhout CM, Polinder S, Havelaar AH, Cassini A, Devleesschauwer B, Kretzschmar M, Speybroeck N, Murray CJ, Vos T. Disability weights for the global burden of disease 2013 study. Lancet Glob Health. 2015;3(11):e712–e723. doi: 10.1016/S2214-109X(15)00069-8. [DOI] [PubMed] [Google Scholar]
- 50.World Bank. https://data.worldbank.org/indicator/SP.POP.1564.TO.ZS. Accessed 6 June 2021
- 51.World Bank. https://data.worldbank.org/indicator/SP.POP.0014.TO.ZS. Accessed 6 June 2021
- 52.Lipton RB, Diamond S, Reed M, Diamond ML, Stewart WF. Migraine diagnosis and treatment: results from the American migraine study II. Headache. 2001;41(7):638–645. doi: 10.1046/j.1526-4610.2001.041007638.x. [DOI] [PubMed] [Google Scholar]
- 53.Westergaard ML, Hansen EH, Glumer C, Olesen J, Jensen RH. Definitions of medication-overuse headache in population-based studies and their implications on prevalence estimates: a systematic review. Cephalalgia. 2014;34(6):409–425. doi: 10.1177/0333102413512033. [DOI] [PubMed] [Google Scholar]
- 54.Togha M, Nadjafi-Semnani F, Martami F, Mohammadshirazi Z, Vahidpour N, Akbari-sari A, Daroudi R. Economic burden of medication-overuse headache in Iran: direct and indirect costs. Neurol Sci. 2020;42(5):1869–1877. doi: 10.1007/s10072-020-04716-8. [DOI] [PubMed] [Google Scholar]
- 55.Lauwerier E, Paemeleire K, Van Damme S, Goubert L, Crombez G. Medication use in patients with migraine and medication-overuse headache: the role of problem-solving and attitudes about pain medication. Pain. 2011;152(6):1334–1339. doi: 10.1016/j.pain.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 56.Kyu HH, Pinho C, Wagner JA, Brown JC, Bertozzi-Villa A, Charlson FJ, Coffeng LE, Dandona L, Erskine HE, Ferrari AJ, Fitzmaurice C, Fleming TD, Forouzanfar MH, Graetz N, Guinovart C, Haagsma J, Higashi H, Kassebaum NJ, Larson HJ, Lim SS, Mokdad AH, Moradi-Lakeh M, Odell SV, Roth GA, Serina PT, Stanaway JD, Misganaw A, Whiteford HA, Wolock TM, Wulf Hanson S, Abd-Allah F, Abera SF, Abu-Raddad LJ, AlBuhairan FS, Amare AT, et al. Global and national burden of diseases and injuries among children and adolescents between 1990 and 2013: findings from the global burden of disease 2013 study. JAMA Pediatr. 2016;170(3):267–287. doi: 10.1001/jamapediatrics.2015.4276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wöber C, Wöber-Bingöl C, Uluduz D, Aslan TS, Uygunoglu U, Tüfekçi A, Alp SI, Duman T, Sürgün F, Emir GK, Demir CF, Balgetir F, Özdemir YB, Auer T, Siva A, Steiner TJ. Undifferentiated headache: broadening the approach to headache in children and adolescents, with supporting evidence from a nationwide school-based cross-sectional survey in Turkey. J Headache Pain. 2018;19(1):18. doi: 10.1186/s10194-018-0847-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lyngberg AC, Rasmussen BK, Jørgensen T, Jensen R. Secular changes in health care utilization and work absence for migraine and tension-type headache: a population based study. Eur J Epidemiol. 2005;20(12):1007–1014. doi: 10.1007/s10654-005-3778-5. [DOI] [PubMed] [Google Scholar]
- 59.American Association for the Study of Headache, International Headache Society Consensus statement on improving migraine management. Headache. 1998;38(10):736. doi: 10.1046/j.1526-4610.1998.t01-1-3810736.x. [DOI] [PubMed] [Google Scholar]
- 60.World Health Assembly . Synergies in addressing the burden of epilepsy and other neurological disorders. WHA73_5_en WHO 2020. 2020. [Google Scholar]
- 61.Davies PTG, Lane RJM, Astbury T, Fontebasso M, Murphy J, Matharu M. The long and winding road: the journey taken by headache sufferers in search of help. Prim Health Care Res Dev. 2019;20:e4. doi: 10.1017/S1463423618000324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Doretti A, Shestaritc I, Ungaro D, Lee J-I, Lymperopoulos L, Kokoti L, Guglielmetti M, Mitsikostas DD, Lampl C, on behalf of the School of Advanced Studies of the European Headache Federation (EHF-SAS) Headaches in the emergency department –a survey of patients’ characteristics, facts and needs. J Headache Pain. 2019;20:100. doi: 10.1186/s10194-019-1053-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Southwell J, Afridi SK. The burden of migraine on acute and emergency services in a London teaching hospital. Cephalalgia. 2021;18:333102420981734. doi: 10.1177/0333102420981734. [DOI] [PubMed] [Google Scholar]
- 64.Braschinsky M, Haldre S, Kals M, Iofik A, Kivisild A, Korjas J, Koljal S, Katsarava Z, Steiner TJ. Structured education can improve primary-care management of headache: the first empirical evidence, from a controlled interventional study. J Headache Pain. 2016;17(1):24. doi: 10.1186/s10194-016-0613-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Constantinidis T, Arvaniti A, Fakas N, Rudolf J, Kouremenos E, Giannouli E, Mitsikostas DD, on behalf of the Hellenic Headache Society A population-based survey for disabling headaches in Greece: prevalence, burden and treatment preferences. Cephalalgia. 2021;41(7):810–820. doi: 10.1177/0333102421989630. [DOI] [PubMed] [Google Scholar]
- 66.Steiner TJ, Göbel H, Jensen R, Lampl C, Paemeleire K, Linde M, Braschinsky M, Mitsikostas D, Gil-Gouveia R, Katsarava Z, on behalf of the European Headache Federation and Lifting The Burden: the Global Campaign against Headache (2019) Headache service quality: the role of specialized headache centres within structured headache services, and suggested standards and criteria as centres of excellence. J Headache Pain 20:24 [DOI] [PMC free article] [PubMed]
- 67.World Bank . World bank country and lending groups – country classification. 2020. [Google Scholar]
- 68.Andrée C, Stovner LJ, Steiner TJ, Barré J, Katsarava Z, Lainez JM, Lair M-L, Lanteri-Minet M, Mick G, Rastenyte D, Ruiz de la Torre E, Tassorelli C, Vriezen P, Lampl C. The Eurolight project: the impact of primary headache disorders in Europe. Description of methods. J Headache Pain. 2011;12(5):541–549. doi: 10.1007/s10194-011-0356-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Steiner TJ, Stovner LJ, Katsarava Z, Lainez JM, Lampl C, Lantéri-Minet M, Rastenyte D, Ruiz de la Torre E, Tassorelli C, Barré J, Andrée C. The impact of headache in Europe: principal results of the Eurolight project. J Headache Pain. 2014;15(1):31. doi: 10.1186/1129-2377-15-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Manandhar K, Risal A, Linde M, Steiner TJ. The burden of headache disorders in Nepal: estimates from a population-based survey. J Headache Pain. 2016;17:3. doi: 10.1186/s10194-016-0594-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Martelletti P, Steiner TJ, Bertolote JM, Dua T, Saraceno B. The definitive position of headache among the major public health challenges. An end to the slippery slope of disregard [editorial] J Headache Pain. 2007;8(3):149–151. doi: 10.1007/s10194-007-0382-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Steiner TJ, Olesen J. Advocacy for patients with headache. Ch 30. In: Grisold W, Struhal W, Grishold T, editors. Advocacy in neurology. Oxford: Oxford University Press; 2019. pp. 339–346. [Google Scholar]
- 73.World Health Organization International Conference on Primary Health Care . Declaration of Alma-Ata. Geneva: WHO; 1978. [Google Scholar]
- 74.Tarino E, Webster EG. Primary health care concepts and challenges in a changing world. Alma-Ata revisited. Geneva: WHO; 1995. [Google Scholar]
- 75.Coulter A. Shifting the balance from secondary to primary care. BMJ. 1995;311(7018):1447–1448. doi: 10.1136/bmj.311.7018.1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Walley J, Lawn JE, Tinker A, de Francisco A, Chopra M, Rudan I, Bhutta ZA, Black RE, the Lancet Alma-Ata Working Group Primary health care: making Alma-Ata a reality. Lancet. 2008;372:1001–1007. doi: 10.1016/S0140-6736(08)61409-9. [DOI] [PubMed] [Google Scholar]
- 77.World Health Organization and United Nations Children’s Fund (UNICEF) Global Conference on Primary Health Care . Declaration of Astana. From Alma-Ata towards universal health coverage and the sustainable development goals. Astana: WHO/UNICEF; 2018. [Google Scholar]
- 78.Clarkson J, Dean J, Ward J, Komashie A, Bashford T. A systems approach to healthcare: from thinking to practice. Future Healthcare J. 2018;5(3):151–155. doi: 10.7861/futurehosp.5-3-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Haag G, Diener H-C, May A, Meyer C, Morck H, Straube A, Wessely P, Evers S. Self-medication of migraine and tension-type headache: summary of the evidence-based recommendations of the Deutsche Migräne und Kopfschmerzgesellschaft (DMKG), the Deutsche Gesellschaft für Neurologie (DGN), the Österreichische Kopfschmerzgesellschaft (ÖKSG) and the Schweizerische Kopfwehgesellschaft (SKG) J Headache Pain. 2011;12(2):201–217. doi: 10.1007/s10194-010-0266-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.World Health Organization . Headache disorders and public health. Education and management implications. Geneva: WHO (WHO/MSD/MBD/00.9); 2000. [Google Scholar]
- 81.Headache Classification Committee of the International Headache Society The international classification of headache disorders, 3rd edition. Cephalalgia. 2018;38:1–211. doi: 10.1177/0333102417738202. [DOI] [PubMed] [Google Scholar]
- 82.Steiner TJ. Health-care systems for headache: patching the seam between primary and specialist care. J Headache Pain. 2003;4(suppl 1):S70–S74. doi: 10.1007/s101940300014. [DOI] [Google Scholar]
- 83.Populationpyramid.net. https://www.populationpyramid.net/brazil/2010. Accessed 6 June 2020
- 84.Masruha MR, Souza JA, Barreiros H, Piovesan EJ, Kowacs F, Queiroz LP, Ciciarelli MC, Peres MFP. Distribution of “Brazilian headache specialists”. Analyses of Brazilian Headache Society members. Einstein. 2007;5:48–50. [Google Scholar]
- 85.Harpole LH, Samsa GP, Jurgelski AE, Shipley JL, Bernstein A, Matchar DB. Headache management program improves outcome for chronic headache. Headache. 2003;43(7):715–724. doi: 10.1046/j.1526-4610.2003.03128.x. [DOI] [PubMed] [Google Scholar]
- 86.Diener H, Gaul C, Jensen R, Göbel H, Heinze A, Silberstein S. Integrated headache care. Cephalalgia. 2011;31(9):1039–1047. doi: 10.1177/0333102411409075. [DOI] [PubMed] [Google Scholar]
- 87.Ferris TG, Chang Y, Blumenthal D, Pearson SD. Leaving gatekeeping behind – effects of opening access to specialists for adults in a health maintenance organization. NEJM. 2001;345(18):1312–1317. doi: 10.1056/NEJMsa010097. [DOI] [PubMed] [Google Scholar]
- 88.Jones R, Lamont T, Haines A. Setting priorities for research and development in the NHS: a case study on the interface between primary and secondary care. BMJ. 1995;311(7012):1076–1080. doi: 10.1136/bmj.311.7012.1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Preston C, Cheater F, Baker R, Hearnshaw H. Left in limbo: patients views on care across the primary/secondary interface. Qual Health Care. 1999;8(1):16–21. doi: 10.1136/qshc.8.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Peres MF, Amado DK, Gonçalves AL, Ribeiro R, Pagura JR, Queiroz LP. The need for preventive therapy in primary headaches. Headache Med. 2011;2:46–49. doi: 10.48208/HeadacheMed.2011.10. [DOI] [Google Scholar]
- 91.Yu S, Zhang M, Zhou J, Liu R, Wan Q, Li Y. Headache care in China. Headache. 2014;54(4):601–609. doi: 10.1111/head.12330. [DOI] [PubMed] [Google Scholar]
- 92.Restrepo Miranda D, Ortiz Monsalve L. Aproximaciones a la estimación de la oferta y la demanda de médicos especialistas en Colombia, 2015–2030. Observatorio De Talento Humano En Salud. 2017. [Google Scholar]
- 93.Muñoz Cerón J. A survey about neurology practice in Colombia. Acta Neurol Colomb. 2011;28:180–186. [Google Scholar]
- 94.Ministerio de Salud y Seguridad Social . Resolución 0256 de 2016. Boletín Judicial N° 2. 2016. [Google Scholar]
- 95.Giorgadze G, Mania M, Kukava M, Dzagnidze A, Mirvelashvili E, Steiner TJ, Katsarava Z. Implementation of effective, self-sustaining headache services in the Republic of Georgia: evaluation of their impact on headache-related disability and quality of life of people with headache. Cephalalgia. 2018;38(4):639–645. doi: 10.1177/0333102417702131. [DOI] [PubMed] [Google Scholar]
- 96.Hellenic Headache Society. http://www.kefalalgia.gr/index.php/el/. Accessed 6 June 2021
- 97.Gazzetta Ufficiale della Repubblica Italiana. LEGGE 14 luglio 2020, n. 81. Disposizioni per il riconoscimento della cefalea primaria cronica come malattia sociale. At https://www.gazzettaufficiale.it/eli/id/2020/07/28/20G00100/SG. Accessed 6 June 2021
- 98.Risal A, Manandhar K, Steiner TJ, Holen A, Koju R, Linde M. Estimating prevalence and burden of major disorders of the brain in Nepal: cultural, geographic, logistic and philosophical issues of methodology. J Headache Pain. 2014;15(1):51. doi: 10.1186/1129-2377-15-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Federal Office for State Statistics, Government of the Russian Federation (EMISS). Number of doctors of all specialties (individuals) in organizations providing medical services to the population at the end of the reporting year. https://www.fedstat.ru/indicator/31547. Accessed 6 June 2021
- 100.Lebedeva ER, Kobzeva NR, Gilev DV, Olesen J (2017) The quality of diagnosis and management of migraine and tension-type headache in three social groups in Russia. Cephalalgia 37(3):225–235. 10.1177/0333102416642603 [DOI] [PubMed]
- 101.Osipova VV, Azimova JE, Tabeeva GR, Tarasova SV, Amelin AV, Kutsemelov IB, Moldovanu IV, Odobesku SS, Naumova GI. Diagnosis of headache disorders in Russia and in post-Soviet countries: state of the problem and ways to solve it (in Russian) Ann Clin Exp Neurol. 2012;6:16–21. [Google Scholar]
- 102.Osipova VV, Filatova EG, Artemenko AR, Lebedeva ER, Azimova YY, Latysheva NV, Sergeev AV, Amelin AV, Koreshkina MI, Skorobogatyh KV, Ekusheva EV, Naprienko MV, Isaguljan YD, Rachin AP, Danilov AB, Kurushina OV, Parfenov VA, Tabeeva GR, Gekht AB, Yahno NN. Diagnosis and treatment of migraine: recommendations of the Russian experts. Zh Nevrol Psikhiatr Im S S Korsakova. 2017;117(1. Vyp. 2):28–42. doi: 10.17116/jnevro20171171228-42. [DOI] [PubMed] [Google Scholar]
- 103.Lebedeva ER, Olesen J, Osipova VV, Volkova LI, Tabeeva GR, Steiner TJ. The Yekaterinburg headache initiative: an interventional project, within the global campaign against headache, to reduce the burden of headache in Russia. J Headache Pain. 2013;14(1):101. doi: 10.1186/1129-2377-14-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.UK Department of Health . Guidelines for the appointment of general practitioners with special interests in the delivery of clinical services: headaches. London: Department of Health; 2003. [Google Scholar]
- 105.Hedenrud T, Jonsson P, Linde M. Beliefs about medicines and adherence among Swedish migraineurs. Ann Pharmacother. 2008;42(1):39–45. doi: 10.1345/aph.1K354. [DOI] [PubMed] [Google Scholar]
- 106.Mulleners WM, Whitmarsh TE, Steiner TJ. Noncompliance may render migraine prophylaxis useless, but once-daily regimens are better. Cephalalgia. 1998;18(1):52–56. doi: 10.1046/j.1468-2982.1998.1801052.x. [DOI] [PubMed] [Google Scholar]
- 107.Braschinsky M, Haldre S, Kals M, Arge M, Saar B, Niibek M, Katsarava Z, Steiner TJ. Structured education to improve primary-care management of headache: how long do the benefits last? A follow-up observational study. Eur J Neurol. 2018;25(3):497–502. doi: 10.1111/ene.13524. [DOI] [PubMed] [Google Scholar]
- 108.Peters M, Jenkinson C, Perera S, Loder E, Jensen R, Katsarava Z, Gil Gouveia R, Broner S, Steiner T. Quality in the provision of headache care. 2: defining quality and its indicators. J Headache Pain. 2012;13(6):449–457. doi: 10.1007/s10194-012-0465-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.United Council for Neurologic Subspecialities . Headache medicine certification. 2020. [Google Scholar]
- 110.American Headache Society . Tool kit for UCNS headache board certification. 2020. [Google Scholar]
- 111.University of Copenhagen . Master of Headache Disorders. 2020. [Google Scholar]
- 112.Sapienza Università di Roma . Master in Headache Medicine. 2020. [Google Scholar]
- 113.International Headache Society . Grants, awards and training programmes. 2020. [Google Scholar]
- 114.European Headache Federation (2020). https://ehf-org.org/educational-activities/. Accessed 6 June 2021
- 115.Katsarava Z, Gil Gouveia R, Jensen R, Gaul C, Schramm S, Schoppe A, Steiner TJ (2015) Evaluation of headache service quality indicators: pilot implementation in two specialist-care centres. J Headache Pain 16(1):53. 10.1186/s10194-015-0537-1 [DOI] [PMC free article] [PubMed]
- 116.Schramm S, Uluduz D, Gil Gouveia R, Jensen R, Siva A, Uygunoglu U, Gvantsa G, Mania M, Braschinsky M, Filatova E, Latysheva N, Osipova V, Skorobogatykh K, Azimova J, Straube A, Emre Eren O, Martelletti P, De Angelis V, Negro A, Linde M, Hagen K, Radojicic A, Zidverc-Trajkovic J, Podgorac A, Paemeleire K, De Pue A, Lampl C, Steiner TJ, Katsarava Z. Headache service quality: evaluation of quality indicators in 14 specialist-care centres. J Headache Pain. 2016;17(1):111. doi: 10.1186/s10194-016-0707-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Pellesi L, Benemei S, Favoni V, Lupi C, Mampreso E, Negro A, Paolucci M, Steiner TJ, Ulivi M, Cevoli S, Guerzoni S. Quality indicators in headache care: an implementation study in six Italian specialist-care centres. J Headache Pain. 2017;18(1):55. doi: 10.1186/s10194-017-0762-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Steiner TJ, Jensen R, Gil-Gouveia R, Katsarava Z. Evaluation: quality in headache services. Ch 16. In: Steiner TJ, Stovner LJ, editors. Societal impact of headache. Burden, costs and response. Cham: Springer Nature; 2019. pp. 225–236. [Google Scholar]
- 119.World Health Organization . Noncommunicable diseases. 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.