Abstract
BACKGROUND:
Stroke is a leading cause of disability resulting in long-term functional ambulation deficits. Conventional therapy can improve ambulation, but may not be able to provide consistent, high dose repetition of movement, resulting in variable recovery with residual gait deviations.
OBJECTIVE:
The objective of this preliminary prospective investigation is to evaluate the ability of a robotic exoskeleton (RE) to provide high dose gait training, and measure the resulting therapeutic effect on functional ambulation in adults with acute stroke.
METHODS:
Participants (n = 14) received standard of care (SOC) and RE overground gait training during their scheduled physical therapy (PT) sessions at the same inpatient rehabilitation facility. The outcome measures included distance walked during their PT training sessions (RE and SOC), and functional ambulation measures (10-meter walk test (10MWT), 6-minute walk test (6 MWT), and timed up and go (TUG)).
RESULTS:
The average total distance walked during RE and the average distance per RE session was significantly higher than SOC sessions. Total walking distance during PT (RE+SOC) showed a strong positive correlation to the total number of steps during RE sessions and number of RE sessions. All functional ambulation measures showed significant improvement at follow-up compared to baseline. The improvement in functional ambulation measures showed a positive correlation with the increase in number of RE gait training sessions.
CONCLUSION:
The RE can be utilized for inpatient rehabilitation in conjunction with SOC gait training sessions and may result in improved functional ambulation in adults with acute stroke. This preliminary research provides information on the ability of the robotic exoskeleton to provide high dose therapy and its therapeutic effect on functional ambulation in adults with acute stroke during inpatient rehabilitation.
Keywords: Wearable robotics, stroke, gait, functional measures, rehabilitation robotics, rehabilitation
1. Introduction
Stroke affects approximately 800,000 people in the United States every year and is a leading cause of long term disability (CDC Stroke Statistics, 2020). Sixty-five percent of individuals with acute stroke have mobility deficits and despite rehabilitation, over half of them present with residual functional ambulation deficits after one year, thus liming their community ambulation, independence and activities of daily living (ADL) (Friedman, 1990; Wade & Hewer, 1987). Regaining community ambulation is a priority among individuals post stroke to improve their ADLs, participation, and quality of life (QOL).
Research in gait rehabilitation has shown that high dose quality gait training can promote recovery of walking function (Cooke, Mares, Clark, Tallis, & Pomeroy, 2010; Lohse, Lang, & Boyd, 2014). Recovery of functional ambulation is dependent on the interrelationship between dosing, intensity (Hornby, Moore, Lovell, & Roth, 2016), and task-specific practice (Krishnan et al., 2019) applied during rehabilitation (Partridge et al., 2000). Recent research has shown that the dosage in a specific task is more critical than the difficulty and variations of task practice when learning new gait patterns (Krishnan et al., 2019). In particular, the same therapy with an increased number of repetitions (dosing) results in improved function (Byl, Pitsch, & Abrams, 2008; Schneider, Lannin, Ada, & Schmidt, 2016). Multiple research have demonstrated that there is a moderate relationship between dosing and improvements in gait (Lang, Lohse, & Birkenmeier, 2015; Nugent, Schurr, & Adams, 1994).
During the acute stages of recovery post-stroke, the brain is in the critical period of plasticity (a period of enhanced plasticity). During this period, providing repetitive, high dose, task-specific training has been found to enhance beneficial cortical re-organization that accelerates functional recovery by restoring healthy gait after stroke (Gillen, 2015; Kwakkel, Kollen, & Lindeman, 2004; Kwakkel, Van Peppen, et al., 2004; Langhorne, Wagenaar, & Partridge, 1996). Recovery post-stroke plateaus during chronic stages of stroke recovery with only marginal functional changes observed during this period. Research has shown that improvements during the critical window resulted in improved recovery with higher plateaus at six months compared to those that had delayed rehabilitation (Kwakkel, Kollen, et al., 2004). This suggests that better outcomes may be expected during the chronic phase of recovery if recovery takes place early during the acute phase.
Currently, physical therapists provide gait therapy for individuals with stroke to relearn gait and balance required for independent ambulation. Individuals with moderate to severe gait and balance deficits may require moderate to maximum assistance from the therapist. It is critical in rehabilitation to reduce the physical effort/exertion of the therapist while increasing the number of repetitive steps administered during a session to individuals with stroke. Although conventional therapy produces improvements in ambulation and motor function, current practices result in variable recovery of functional ambulation with residual gait deviations. As a result, of these residual ambulatory deficits, individuals with stroke often develop compensation mechanisms such as hip hiking (Kerrigan, Frates, Rogan, & Riley, 2000), circumduction (Kerrigan et al., 2000), and prolonged weight transfer in order to achieve ambulation.
Research focuses on using lower extremities exoskeletons for rehabilitation (Molteni et al., 2017; Swank, Sikka, Driver, Bennett, & Callender, 2020). Lower extremities exoskeletons are electromechanical devices that can provide complete or partial assistance to the user to walk while providing stability and balance. It has the potential to provide consistent, high dose repetition of movement for individuals requiring maximum assistance post-stroke. This reduces the physical effort of the therapist while allowing them to focus on providing feedback to drive quality gait.
Robotic exoskeletons (REs) have been used for rehabilitation during the chronic and subacute stages of stroke, where they assist the user to perform gait (Høyer, Opheim, & Jørgensen, 2020; Louie & Eng, 2016; Molteni et al., 2021; Tefertiller et al., 2018). But limited quantitative information is available regarding the feasibility of using RE to provide acute stroke rehabilitation, the ability of RE to provide high dose therapy and its effects on functional ambulation during acute stages of recovery. The ability to perform safe, independent gait in the community requires the restoration of function (i.e., endurance, balance, gait speed, and quality of gait) (Fulk, He, Boyne, & Dunning, 2017). Therefore, the objective of this preliminary investigation is to understand the utilization of RE for inpatient rehabilitation for acute stroke. The preliminary study further analyzes the ability of RE to provide high dose therapy and evaluates its therapeutic effect on functional ambulation in adults with acute stroke during inpatient rehabilitation.
2. Methodology
2.1. Participants
Twenty-one participants diagnosed with moderate to severe hemiplegic stroke (<3 months) were consented to participate from the same inpatient rehabilitation facility (IRF) in the prospective investigation and 14 participants completed the study. Seven participants did not complete the study due to early discharge from the IRF, transfer to another sub-acute facility or transfer out of the IRF for a medical procedure. No participants were withdrawn due to study procedures. All data were collected as a part of a larger ongoing investigation. All participants were current inpatients at the same IRF and received RE gait training during their scheduled physical therapy sessions. Demographic data (Table 1) including age, gender, length of stay at the IRF, time since stroke, and number of PT and RE sessions were collected and verified with medical records. The inclusion criteria were 1) be between the ages 18 and 82 years, 2) had to fit into the RE device physically (height 152.4–177.8 cm; weight < 99.7 kg; hip width 35–46”), 3) no history of injury or pathology (unrelated to their stroke) within the last 90 days; 4) joint range of motion (ROM) within normal functional limits for ambulation; 5) be able to tolerate upright standing for up to 30 minutes with assistance. Exclusion criteria were 1) contracture of joints (hip, knee, and ankle) that would prohibit a healthy ROM without pain as well as fitting the RE, 2) cardiopulmonary or other medical conditions that prevent intensive gait training. All procedures were approved by the Institutional Review Board and all participants were consented prior to participation in the study.
Table 1.
Participant Demographics
| Demographics (N = 14) | Mean±Standard Error |
| Age (years) | 61.24±1.98 |
| Height (m) | 168.18±1.99 |
| Weight (kg) | 69.78±2.28 |
| LOS (days) | 39.71±4.55 |
| Gender(number) | 10 Male, 4 Female |
| Affected side(number) | 10 Left, 4 Right |
| Time Since Injury (days) | 18.92±1.80 |
| PT Sessions | 21.29±3.33 |
| RE Sessions | 8.43±1.08 |
| SOC Sessions | 12.85±2.34 |
| Number of Steps During RE sessions | 4881.86±1114.04 |
| Number of Steps/day During RE sessions | 512.27±44.64 |
Length of Stay (LOS) –Calculated as the number of calendar days from the date of admission to the IRF to date of discharge. Time Since Injury –Calculated as the number of calendar days from the date of injury to the baseline assessment. Physical Therapy (PT) Sessions –The average number of physical therapy sessions are reported between baseline and follow-up. This includes the RE and SOC sessions. SOC sessions –The average number of SOC sessions are reported between baseline and follow-up. One session per day. RE sessions –The average number of RE sessions are reported between baseline and follow-up. One session per day.
2.2. Experimental procedures
2.2.1. Gait training
Gait training (RE or standard of care) was provided to participants for a duration of 45 minutes to 90 minutes per session. Each standard of care (SOC) session included pre-gait activities, upright activities, and gait training to promote sensory and motor recovery. Participants walked known distances during SOC training, and this information was recorded in the medical chart by the physical therapist during each session. The RE gait training was administered by a trained physical therapist using a commercially available, FDA class 2 approved exoskeleton (Ekso GT™, Ekso Bionics, Inc. Richmond, CA, USA). The device is programmed to bilaterally assist as needed to the user’s hip and knee joints in a repetitive predefined gait trajectory computed by the RE software in the sagittal plane based on the user’s anthropometrics (Fig. 1). The start and stop of the walking activity were triggered by the physical therapist using a control pad. The user initialized each additional step during a walk by shifting their center of mass laterally and offloading the hind limb. RE sessions were exchanged with SOC time to avoid patients from receiving additional therapy time throughout their inpatient rehabilitation. All participants received the same amount of therapy time overall, and a licensed physical therapist individualized RE and SOC training based on patient recovery progression.
Fig. 1.

Participant gait training with Robotic Exoskeleton.
2.2.2. Data collection
Total distance walked during physical therapy (distance walked during RE sessions and distance walked during SOC sessions) was collected during each session of IRF gait training between baseline and follow-up data collection sessions for all participants. The total number of steps during the RE sessions was also recorded. The dosing outcome measures are described in Table 2.
Table 2.
Outcome Measures
| Outcome Measure | Description |
| Total distance walked RE | The total distance walked during physical therapy in the RE only (not including SOC training) between baseline to follow-up during inpatient rehabilitation were calculated from the RE software ([RE steps x step length from Ekso bionics settings]/12 [divided by twelve to convert from inches to feet]). |
| Total distance walked SOC | The total distance walked during physical therapy in the SOC only (not including RE training) between baseline to follow-up during inpatient rehabilitation was recorded by the physical therapist and extracted from the medical chart. |
| Total distance walked during PT (RE+SOC) | The total distance walked during physical therapy including SOC+RE training between baseline to follow-up during inpatient rehabilitation. |
| Distance per session RE | The distance walked during RE sessions divided by number of RE sessions (total distance walked RE/number of RE sessions) between baseline to follow-up during inpatient rehabilitation for each subject was computed as distance per session RE. Average distance per session RE was computed as sum of distance per session RE for all subjects/ number of subjects. |
| Distance per session SOC | The distance walked during SOC sessions divided by number of SOC sessions (total distance walked SOC/number of SOC sessions) between baseline to follow-up during inpatient rehabilitation for each subject was computed as distance per session SOC. Average distance per session SOC was computed as sum of distance per session PT for all subjects/ number of subjects. |
| Distance per PT session (RE+SOC) | The distance walked during physical therapy including RE+SOC (total distance walked PT Sessions/number of PT sessions sessions) during each PT session between baseline to follow-up during inpatient rehabilitation was computed as distance per session PT for each subject. Average distance per session PT was computed as sum of distance per session PT for all subjects/ number of subjects. |
| Total number of steps RE | The total number of steps taken during all over ground walking sessions in the RE between baseline and follow-up during inpatient rehabilitation was recorded for participants. Average number of steps RE was computed as sum of all the steps by all participants/ number of participants. |
| Steps per session RE | The number of steps taken during all over ground walking sessions in the RE/number of RE sessions between baseline and follow-up during inpatient rehabilitation was computed as steps per sessions RE for each participants. Average number of steps RE was computed as steps per sessions RE by all participants/ number of participants. |
All participants completed two data collection sessions while walking without the robotic exoskeleton: baseline (before training sessions) and follow-up (within one week after completing the last training session). During walking assessments, participants were allowed to stop and rest if necessary. The following functional ambulation metrics were collected during these sessions:
Ten Meter Walk Test (10MWT): The participants performed two 10 meter walks at a fast, safe walking speed. The time to walk ten meters was recorded using a stopwatch. One meter was added at the beginning and at the end of the walk to provide sufficient ramp up and ramp down for speed (total 12 meters) and walk time during this period was not recorded (Kay & Huijbregts, 2003).
Timed Up and Go (TUG): The participants walked a distance of 3 meters from a seated position, turned around, walked back to the chair, and sat back in the chair. The time (seconds) taken to perform the task was recorded using a stopwatch (Kay & Huijbregts, 2003).
Six Minute Walk (6MWT): Participants walked as far as possible for 6 minutes. They walked back and forth around the cones along an unobstructed pathway of 15 meters. They were permitted to slow down or stop as necessary. The distance covered by the participant for the 6 minutes was recorded at an interval of every 30 seconds using a measuring wheel and stopwatch (Kay & Huijbregts, 2003). Speed during the 6-minute walk test was calculated as the distance walked during the 6-minute walk test for each subject divided by 6 minutes to compute the speed.
2.2.3. Data analysis
2.2.3.1. Distance walked between RE and SOC sessions: Dosing differences
The total distance walked between RE and SOC and distance walked per session between RE and SOC was used to quantify dosing differences between RE and SOC gait training during PT sessions between baseline and follow-up (Table 2). The difference in dosing between the sessions was determined using Wilcoxson Signed Rank test on total distance walked SOC and total distance walked RE as the Shapiro-Wilk test showed that data was not normally distributed (p < 0.05).
The difference in dosing per session between the RE and SOC sessions was determined using Paired sample t-test on distance per session RE and distance per session SOC as the Shapiro-Wilk test showed that data was normally distributed (p > 0.05).
2.2.3.2. Effect of number of steps during RE sessions on distance walked during PT (Dosing)
The effect of number of steps during RE sessions on the total distance walked during PT sessions was determined using spearman’s rank correlation as the Shapiro-Wilk test showed that total distance walked and number of steps during RE training sessions were not normally distributed (p < 0.05). Total distance walked in PT is the sum of the total distance walked in RE+SOC sessions (i.e. all PT sessions between baseline and discharge).
Effect of steps per session RE on distance walked per PT session as determined using Pearson’s rank correlation as the Shapiro-Wilk test showed data were normally distributed (p > 0.05).
2.2.3.3. Effect of the number of RE training sessions on distance walked (Dosing)
Spearman’s rank correlation was used to determine the relationship between the number of RE training sessions and total distance walked during physical therapy as the Shapiro-Wilk test showed that total distance walked and number of RE training sessions were not normally distributed (p < 0.05).
Spearman’s rank correlation was used to determine the relationship between the number of RE training sessions and distance per physical therapy session as the Shapiro-Wilk test showed that number of RE training sessions was not normally distributed (p < 0.05).
2.2.3.4. Effect of number of RE training sessions on functional measures
A paired samples t-test was used to determine the difference in the 10MWT, TUG, and 6MWT, between baseline to follow up as the Shapiro-Wilk test showed that data was normally distributed (p > 0.05).
Spearman’s rank correlation was used to determine the relationship between the number of RE sessions and functional measures (10 MWT, TUG, and 6MWT) as the Shapiro-Wilk test showed that total number of RE sessions was not normally distributed (p < 0.05).
Spearman’s rank correlation was used to determine the relationship between the number of RE sessions and speed during the 6MWT.
3. Results
3.1. Distance walked between RE and SOC sessions: Dosing differences
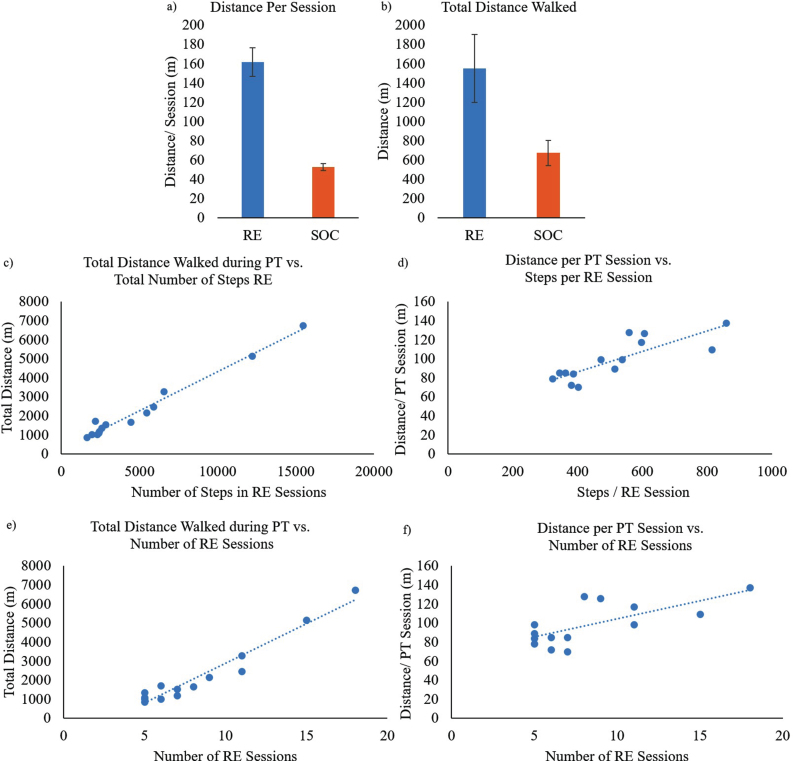
All data is presented as mean±standard error. Total distance walked RE (Fig. 2b; 1549.69±354.43 m) was significantly higher (Z = –2.794, p < 0.01) than total distance walked SOC (673.80±130.02 m). Distance per session RE (Fig. 2a; 161.77±14.89 m) was also significantly higher (t = 6.67, p < 0.01) than distance per session SOC (52.58±3.77 m).
Fig. 2.
a) Average distance per session walked during RE and SOC sessions; b) Average total distance walked during RE and SOC sessions; c) Total distance walked during PT sessions (RE + SOC) vs. number of steps during RE training sessions for all participants; d) Distance per session vs. number of steps per session during RE training for all participants; e) Total distance walked during PT sessions (RE + SOC) vs. total number of RE training sessions; f) Distance per session vs. number of RE training sessions.
3.2. Effect of number of steps during RE training on distance walked (Dosing)
A strong positive correlation (ρ (rho) = 0.908, p < 0.01) between the number of steps during RE sessions and total distance walked during PT (Fig. 2c) was observed, which was also statistically significant. This suggests that increased number of steps during RE sessions may have resulted in increased distance walked during PT.
Pearson’s rank correlation showed a strong positive correlation (r = 0.82, p < 0.01) between the number of steps per RE session and distance walked per PT session (Fig. 2d), which was also statistically significant. This suggests that increased number of steps per RE sessions may have resulted in increased distance walked per session during a rehabilitation therapy session.
3.3. Effect of the number of SOC and RE training on distance walked (Dosing)
A strong positive correlation (ρ= 0.903, p < 0.01) between the number of RE training sessions and total distance walked during PT (Fig. 2e) was observed, which was also statistically significant. This suggests that increased RE training sessions resulted in increased total distance walked during PT.
A moderate positive correlation (ρ= 0.64, p < 0.05) between the number of RE sessions and distance walked per PT session (Fig. 2f), which was also statistically significant. This suggests that increased RE sessions resulted in increased distance walked per session during their PT.
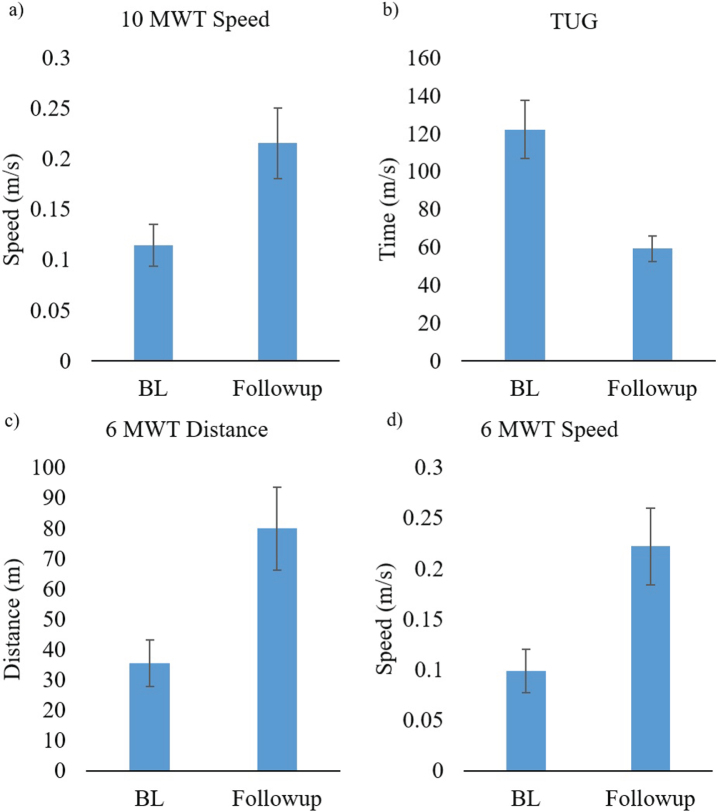
3.4. Effect of number of RE training sessions on functional ambulation
Paired samples t-test showed a significant difference between baseline and follow-up in TUG (t = 4.42, p < 0.01; Fig. 3b), 10MWT (t = –3.794, p < 0.01; Fig. 3a), 6 MWT- Distance (t = –4.62, p < 0.01; Fig. 3c), and 6 MWT- Speed (t = –4.62, p < 0.01; Fig. 3d).
Fig. 3.
Functional ambulation data is presented as mean±standard error at baseline and follow-up sessions a) speed during 10MWT; b) Time to complete the TUG; c) Distance during the 6 MWT; and d) Speed during 6 MWT.
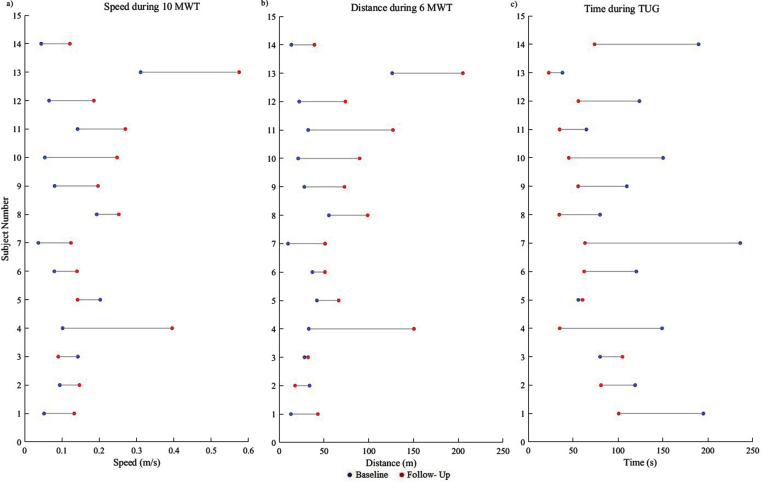
At baseline functional ambulation assessments demonstrated that all subjects had speeds less than 0.4 m/s in the 10MWT, walked less than 150m in 6MWT, and took over 30s to complete the TUG. Follow-up assessments showed that all subjects improved in speed (10MWT;Fig. 4a), distance (6 MWT; Fig. 4b) and time (TUG; Fig. 4c) at follow-up compared to baseline except 3 and 5 who did not show improvement in speed (10MWT) and TUG and subject 3 who did not show improvement in 6MWT.
Fig. 4.
Participant (n = 14) data is presented demonstrating the change from baseline to follow-up for functional ambulation a) Speed during 10MWT, b) Distance during 6 MWT and c) Time during TUG at baseline and follow- up sessions.
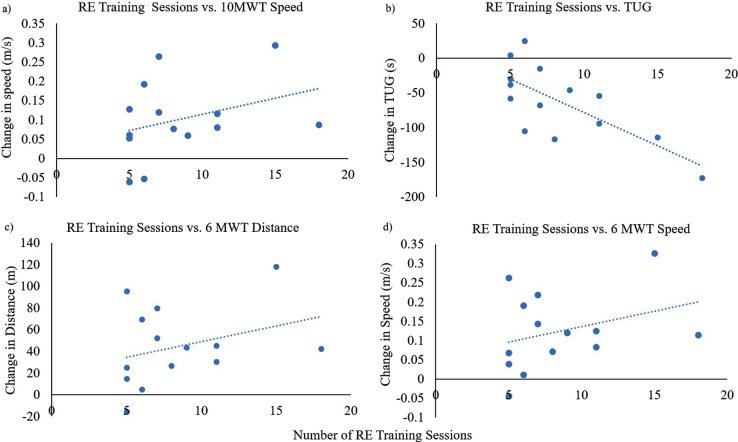
Spearman’s rank correlation showed a moderate negative correlation (ρ= –0.63, p < 0.05) between the number of RE training sessions and the change in TUG (Fig. 5b) which was statistically significant. This suggests that time required to perform timed up and go may have reduced with increased number of RE training sessions. Spearman’s rank correlation showed a moderate positive correlation between increased number of RE training sessions and change in 6MWT distance (ρ= 0.35, p > 0.05, Fig. 5c) and speed (ρ= 0.35, p > 0.05, Fig. 5d) and change in speed (Fig. 5a) during 10MWT (ρ= 0.38, p > 0.05).
Fig. 5.
a) Number of RE training sessions vs. change in 10MWT speed, b) Number of RE training sessions vs. change in time to complete the TUG (seconds); c) Number of RE training sessions vs. change in 6MWT distance, d) Number of RE training sessions vs. change in 6MWT speed.
4. Discussion
Stroke results in gait and balance deficits affecting functional ambulation and overall community ambulation and participation. Current research is focused on improving functional ambulation using REs to improve safe community ambulation (Høyer, Opheim, & Jørgensen, 2020; Louie & Eng, 2016; Molteni et al., 2021). This study focused on presenting utilization of an RE for inpatient gait rehabilitation and preliminary data demonstrating the effect of an RE on dosing and functional ambulation for acute stroke. Participants walked increased distances during their RE sessions compared to SOC sessions though the number of sessions were similar between RE and SOC. The number of steps walked during RE sessions showed a strong positive correlation to walking distance (dosing) during PT. Participants also increased their walking distance (dosing) during PT with increased use of RE.
Distance walked during physical therapy sessions was used as a measure of dosing during inpatient rehabilitation. The participants walked twice the distance during their RE sessions compared to their SOC sessions during inpatient rehabilitation as measured by the total distance walked as well as the distance per session metrics. The RE sessions were of the same duration of training (time spent during a session in inpatient rehabilitation) and were similar in number of sessions during their SOC session (Table 1). The results showed that dosing increased with increased RE gait training (distance per session, as well as total distance during physical therapy) for individuals requiring medium to maximum assistance to walk. This demonstrated that RE provided increased dosing during gait training without increasing the duration of training. In addition, the number of steps during RE session had a strong correlation to the distance walked during PT as well as the steps per RE session showed a strong correlation to distance per session during PT. Walking in the RE could increase dosing during gait rehabilitation, even in individuals with acute stroke who require maximum assistance. Research has shown that increasing the number steps (distance due to increased number of steps) is a critical variable of rehabilitation interventions that can facilitate plasticity of neuromuscular system and result in improved locomotor function (Hornby et al., 2015; Hornby et al., 2011)
Community ambulators are defined as people who can complete 10 m at a speed of 1 m/s and walk at least 205 m in 6 minutes (Fulk, Reynolds, Mondal, & Deutsch, 2010; Perry, Garrett, Gronley, & Mulroy, 1995). The TUG assessment classifies anyone taking over 30 s to complete the task as requiring assistance during gait (Hafsteinsdóttir, Rensink, & Schuurmans, 2014). This suggests that all participants at baseline in this study were non-community ambulators requiring medium to maximum assistance to walk. At follow-up, all functional measures (10MWT, 6MWT, and TUG) showed improvement from baseline. There was a moderate positive correlation between change in distance and speed during 6MWT and speed during 10MWT, and number of RE sessions during PT, and there was a moderate negative correlation between change in time taken for TUG from baseline to follow-up (i.e., reduced time in the TUG indicated improved functional ambulation), and number of RE sessions during PT.
Individuals with stroke have balance deficits and are at increased risk of falling, with the prevalence of falls as high as 73% (Czernuszenko & Czlonkowska, 2009). The important goal of rehabilitation is safe ambulation at home and in the community. TUG score correlates with balance, gait speed, and functional capacity and is a widely used reliable measure of physical mobility (Alghadir, Al-Eisa, Anwer, & Sarkar, 2018; Hafsteinsdóttir et al., 2014; Richardson, 1991). Significantly improved TUG score and moderate negative correlation of change in TUG (i.e. time to perform the task reduced at follow-up) with the number of RE sessions suggests that RE gait training provided in conjunction with SOC could be contributing to improved independent, safe functional mobility among participants.
Walking endurance, balance, and motor function are the strongest predictors of community walking activity (Fulk et al., 2017). Walking endurance, as measured by the 6MWT, was the strongest individual predictor of community walking activity (Fulk et al., 2017; Mahendran, Kuys, & Brauer, 2020). Research shows that the 6MWT is a better predictor of community ambulation due to the distance requirements for community walking (Andrews et al., 2010). Fulk et al. also found that although both the 6MWT and comfortable gait speed were strongly related to community walking, only the 6MWT was a significant predictor of community walking activity (Fulk et al., 2010). In this study, the distance and the speed during 6 MWT and walking speed from 10MWT showed a moderate correlation with the number of RE sessions suggesting that they have improved endurance, balance, and motor function, and were progressing towards community ambulation.
Current lower extremity rehabilitation is based on cortical re-organization induced by repeated high dose task-specific practice that leads to the recovery of function (Cooke et al., 2010; Lennon, Baxter, & Ashburn, 2001). Current research shows that the amount of practice in the specific task is critical for gait recovery (Krishnan et al., 2019). Multiple studies demonstrate a moderate relationship between the frequency of repetitions and improvements in motor function(Nugent et al., 1994). In particular, the same therapy with increased number of repetitions (dosing) results in improved function (Byl et al., 2008; Schneider et al., 2016). Our results are in accordance with these previous research, where increased walking distance (dose due to increased number of steps) due to RE training may have resulted in improved TUG, distance and speed during 6MWT, and speed in 10MWT. Improved functional ambulation is associated with increased community ambulation and participation, leading to improved quality of life (An, Lee, Shin, & Lee, 2015). The results indicate that increased dosing could improve the gait and balance recovery trajectory long term.
The results show the ability of RE utilization in acute stroke during inpatient rehabilitation with varying degrees of severity. Our sample of 14 participants did not have any secondary complications or falls due to the RE. A limitation of the study was not having a separate group for RE-only training and SOC-only training. Future studies should standardize the amount of training by having RE training matched to a control group.
Previous research showed that more significant improvements within the first weeks post-stroke resulted in higher plateaus at six months than improvements occurring to those that had delayed rehabilitation(Kwakkel, Kollen, et al., 2004). This suggests that better outcomes may be expected during the chronic phase of recovery if recovery takes place early during the acute phase. Our results indicate that an RE can provide the crucial increased dose training during acute inpatient rehabilitation and maybe aiding in early recovery onset.
Acknowledgments
We would like to thank the Kessler Foundation and Kessler Institute for Rehabilitation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding
This work was supported by the Rehabilitation Engineering Research Center on Wearable Robots (NIDILRR grant 90RE5021).
References
- Alghadir, A. H., Al-Eisa, E. S., Anwer, S., & Sarkar, B. (2018). Reliability, validity, and responsiveness of three scales for measuring balance in patients with chronic stroke. BMC Neurology, 18(1). 10.1186/s12883-018-1146-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- An, S., Lee, Y., Shin, H., & Lee, G. (2015). Gait velocity and walking distance to predict community walking after stroke. Nursing and Health Sciences, 17(4), 533–538. 10.1111/nhs.12234 [DOI] [PubMed] [Google Scholar]
- Andrews, A. W., Chinworth, S. A., Bourassa, M., Garvin, M., Benton, D., & Tanner, S. (2010). Update on distance and velocity requirements for community ambulation. Journal of Geriatric Physical Therapy, 33(3), 128–134. 10.1097/JPT.0b013e3181eda321 [DOI] [PubMed] [Google Scholar]
- Byl, N. N., Pitsch, E. A., & Abrams, G. M. (2008). Functional outcomes can vary by dose: Learning-based sensorimotor training for patients stable poststroke. Neurorehabilitation and Neural Repair, 22(5), 494–504. 10.1177/1545968308317431 [DOI] [PubMed] [Google Scholar]
- CDC Stroke Statistics. (n.d.). Retrieved March 7, 2020, from https://www.cdc.gov/stroke/facts.htm#:~:text=Stroke Statistics,minutes%2C someone dies of stroke.&text=Every year%2C more than 795%2C000,United States have a stroke.
- Cooke, E. V., Mares, K., Clark, A., Tallis, R. C., & Pomeroy, V. M. (2010). The effects of increased dose of exercise-based therapies to enhance motor recovery after stroke: A systematic review and meta-analysis. BMC Medicine, 8, 1–13. 10.1186/1741-7015-8-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czernuszenko, A., & Czlonkowska, A. (2009). Risk factors for falls in stroke patients during inpatient rehabilitation. Clinical Rehabilitation, 23(2), 176–188. 10.1177/0269215508098894 [DOI] [PubMed] [Google Scholar]
- Friedman, P. J. (1990). Gait recovery after hemiplegic stroke. Disability and Rehabilitation, 12(3), 119–122. 10.3109/03790799009166265 [DOI] [PubMed] [Google Scholar]
- Fulk, G. D., He, Y., Boyne, P., & Dunning, K. (2017). Predicting Home and Community Walking Activity Poststroke. Stroke, 48(2), 406–411. 10.1161/STROKEAHA.116.015309 [DOI] [PubMed] [Google Scholar]
- Fulk, G. D., Reynolds, C., Mondal, S., & Deutsch, J. E. (2010). Predicting home and community walking activity in people with stroke. Archives of Physical Medicine and Rehabilitation, 91(10), 1582–1586. 10.1016/j.apmr.2010.07.005 [DOI] [PubMed] [Google Scholar]
- Gillen, G. (2015). Stroke rehabilitation. Stroke Rehabilitation, 377(9778), 1–756. 10.1016/C2012-0-02658-0 [DOI] [Google Scholar]
- Hafsteinsdóttir, T. B., Rensink, M., & Schuurmans, M. (2014). Clinimetric properties of the timed up and go test for patients with stroke: A systematic review. Topics in Stroke Rehabilitation. 10.1310/tsr2103-197 [DOI] [PubMed]
- Hornby, T. G., Holleran, C. L., Leddy, A. L., Hennessy, P., Leech, K. A., Connolly, M.,... Roth, and E. (2015). Feasibility of Focused Stepping Practice During Inpatient Rehabilitation Poststroke and Potential Contributions to Mobility Outcomes. Neurorehabilitation and Neural Repair, 29(10), 923–932. [DOI] [PubMed] [Google Scholar]
- Hornby, T. G., Moore, J. L., Lovell, L., & Roth, E. J. (2016). Influence of skill and exercise training parameters on locomotor recovery during stroke rehabilitation. Current Opinion in Neurology, 29(6), 677–683. 10.1097/WCO.0000000000000397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornby, T., Straube, D., Kinnaird, C., Holleran, C., Echauz, A., Rodriguez, K.,... Narducci, E. (2011). Importance of specificity, amount, and intensity of locomotor training to improve ambulatory function in patients poststroke. Topics in Stroke Rehabilitation, 18(4), 293–307. 10.1310/tsr1804-293 [DOI] [PubMed] [Google Scholar]
- Høyer, E., Opheim, A., & Jørgensen, V. (2020). Implementing the exoskeleton Ekso GTTM for gait rehabilitation in a stroke unit-feasibility, functional benefits and patient experiences. Disability and Rehabilitation: Assistive Technology. 10.1080/17483107.2020.1800110 [DOI] [PubMed]
- Kay, T. M., & Huijbregts, M. (2003). Physical Rehabilitation Outcome Measures: A Guide to Enhanced Clinical Decision Making, Second Edition. Physiotherapy Canada (2nd ed., Vol. 55). Lippincott Williams & Wilkins. 10.2310/6640.2003.35271 [DOI]
- Kerrigan, D. C., Frates, E. P., Rogan, S., & Riley, P. O. (2000). Hip hiking and circumduction: Quantitative definitions. American Journal of Physical Medicine and Rehabilitation, 79(3), 247–252. 10.1097/00002060-200005000-00006 [DOI] [PubMed] [Google Scholar]
- Krishnan, C., Dharia, A. K., Augenstein, T. E., Washabaugh, E. P., Reid, C. E., Brown, S. R., & Ranganathan, R. (2019). Learning new gait patterns is enhanced by specificity of training rather than progression of task difficulty. Journal of Biomechanics, 88, 33–37. 10.1016/j.jbiomech.2019.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwakkel, G., Kollen, B., & Lindeman, E. (2004). Understanding the pattern of functional recovery after stroke: Facts and theories. Restorative Neurology and Neuroscience, 22(3-4), 281–299. [PubMed] [Google Scholar]
- Kwakkel, G., Van Peppen, R., Wagenaar, R. C., Dauphinee, S. W., Richards, C., Ashburn, A.,... Langhorne, P. (2004). Effects of augmented exercise therapy time after stroke: A meta-analysis. Stroke, 35(11), 2529–2536. 10.1161/01.STR.0000143153.76460.7d [DOI] [PubMed] [Google Scholar]
- Lang, C. E., Lohse, K. R., & Birkenmeier, R. L. (2015). Dose and timing in neurorehabilitation: Prescribing motor therapy after stroke. Current Opinion in Neurology, 28(6), 549–555. 10.1097/WCO.0000000000000256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langhorne, P., Wagenaar, R., & Partridge, C. (1996). Physiotherapy after stroke: more is better? Physiotherapy Research International: The Journal for Researchers and Clinicians in Physical Therapy, 1(2), 75–88. 10.1002/pri.6120010204 [DOI] [PubMed] [Google Scholar]
- Lennon, S., Baxter, D., & Ashburn, A. (2001). Physiotherapy based on the Bobath concept in stroke rehabilitation: A survey within the UK. Disability and Rehabilitation, 23(6), 254–262. 10.1080/096382801750110892 [DOI] [PubMed] [Google Scholar]
- Lohse, K. R., Lang, C. E., & Boyd, L. A. (2014). Is more better? Using metadata to explore dose-response relationships in stroke rehabilitation. Stroke, 45(7), 2053–2058. 10.1161/STROKEAHA.114.004695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Louie, D. R., & Eng, J. J. (2016). Powered robotic exoskeletons in post-stroke rehabilitation of gait: A scoping review. Journal of NeuroEngineering and Rehabilitation, 13(1), 1–10. 10.1186/s12984-016-0162-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahendran, N., Kuys, S. S., & Brauer, S. G. (2020). Which impairments, activity limitations and personal factors at hospital discharge predict walking activity across the first 6 months poststroke? Disability and Rehabilitation, 42(6), 763–769. 10.1080/09638288.2018.1508513 [DOI] [PubMed] [Google Scholar]
- Molteni, F., Gasperini, G., Gaffuri, M., Colombo, M., Giovanzana, C., Lorenzon, C.,... Guanziroli, E. (2017). Wearable robotic exoskeleton for overground gait training in sub-acute and chronic hemiparetic stroke patients: preliminary results. European Journal of Physical and Rehabilitation Medicine, 53(5), 676–684. 10.23736/S1973-9087.17.04591-9 [DOI] [PubMed] [Google Scholar]
- Molteni, F., Guanziroli, E., Goffredo, M., Calabrò, R. S., Pournajaf, S., Gaffuri, M.,... Franceschini, M. (2021). Gait recovery with an overground powered exoskeleton: A randomized controlled trial on subacute stroke subjects. Brain Sciences, 11(1), 1–14. 10.3390/brainsci11010104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nugent, J. A., Schurr, K. A., & Adams, R. D. (1994). A dose-response relationship between amount of weight-bearing exercise and walking outcome following cerebrovascular accident. Archives of Physical Medicine and Rehabilitation, 75(4), 399–402. 10.1016/0003-9993(94)90162-7 [DOI] [PubMed] [Google Scholar]
- Partridge, C., Mackenzie, M., Edwards, S., Reid, A., Jayawardena, S., Guck, N., & Potter, J. (2000). Is dosage of physiotherapy a critical factor in deciding patterns of recovery from stroke: A pragmatic randomized controlled trial. Physiotherapy Research International: The Journal for Researchers and Clinicians in Physical Therapy, 5(4), 230–240. 10.1002/pri.203 [DOI] [PubMed] [Google Scholar]
- Perry, J., Garrett, M., Gronley, J. K., & Mulroy, S. J. (1995). Classification of walking handicap in the stroke population. Stroke, 26(6), 982–989. 10.1161/01.STR.26.6.982 [DOI] [PubMed] [Google Scholar]
- Richardson, S. (1991). The Timed “Up & Go”: A Test of Basic Functional Mobility for Frail Elderly Persons. Journal of the American Geriatrics Society, 39(2), 142–148. 10.1111/j.1532-5415.1991.tb01616.x [DOI] [PubMed] [Google Scholar]
- Schneider, E. J., Lannin, N. A., Ada, L., & Schmidt, J. (2016). Increasing the amount of usual rehabilitation improves activity after stroke: a systematic review. Journal of Physiotherapy, 62(4), 182–187. 10.1016/j.jphys.2016.08.006 [DOI] [PubMed] [Google Scholar]
- Swank, C., Sikka, S., Driver, S., Bennett, M., & Callender, L. (2020). Feasibility of integrating robotic exoskeleton gait training in inpatient rehabilitation. Disability and Rehabilitation: Assistive Technology, 15(4), 409–417. 10.1080/17483107.2019.1587014 [DOI] [PubMed] [Google Scholar]
- Tefertiller, C., Hays, K., Jones, J., Jayaraman, A., Hartigan, C., Bushnik, T., & Forrest, G. F. (2018). Initial outcomes from a multicenter study utilizing the indego powered exoskeleton in spinal cord injury. Topics in Spinal Cord Injury Rehabilitation, 24(1), 78–85. 10.1310/sci17-00014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade, D. T., & Hewer, R. L. (1987). Functional abilities after stroke: Measurement, natural history and prognosis. Journal of Neurology Neurosurgery and Psychiatry, 50(2), 177–182. 10.1136/jnnp.50.2.177 [DOI] [PMC free article] [PubMed] [Google Scholar]