Abstract
Mesothelial cyst of the spleen is a developmental disorder. Previous reports have elaborated on the radiological features of splenic mesothelial cysts as being unilocular with a smooth and well-defined margin. However, due to its rarity, it is unclear whether these characteristics are representative and specific for the diagnosis of mesothelial cysts. Herein, this case report presents an atypical case of splenic mesothelial cyst mimicking a malignant tumour, especially splenic metastasis in a 66-year-old woman with ascending colon cancer. Due to an overlapping imaging finding of hypodense splenic lesions, and considering the clinical history, a mesothelial cyst that developed as a multilocular hypodense mass from an ill-defined small nodule was inevitably misdiagnosed as metastasis. Although rare, it is important to consider the possibility of mesothelial cyst in a patient with multilocular hypodense lesions of the spleen.
Keywords: Spleen, cysts, mesothelial cyst, metastasis, tomography, X-ray computed, diagnostic imaging
Introduction
A mesothelial cyst is a rare form of cyst that is lined by a trabeculated wall consisting of hyalinized connective tissue and simple or stratified epithelial cells. 1 While the prevalence of mesothelial cysts is unknown, they are more common in children and young adults and are found in various anatomical structures, such as the diaphragm, spleen, falciform ligament, ovary and mesentery.2–4
The radiological features of splenic mesothelial cysts have been described as cystic lesions that are unilocular, smooth and with well-defined margins.5,6 However, due to the rarity of these cysts, it remains unclear whether these characteristics are representative and specific enough for diagnosis.
Herein, this current report describes an atypical case of a splenic mesothelial cyst that mimicked a malignant tumour, especially splenic metastasis, in a patient with ascending colon cancer. This current report also discusses its significance and the differences between a mesothelial cyst and other masses of the spleen.
Case report
A 66-year-old woman visited the Chungbuk National University Hospital, Cheongju, Republic of Korea with ascending colon cancer that was incidentally found during a health screening in December 2013. At the time of presentation, she had no symptoms and her medical history was unremarkable except for hypertension. She underwent a right hemicolectomy for a well-differentiated tubular adenocarcinoma of the ascending colon in January 2014. At the time of the surgery, the tumour had invaded the muscularis propria with lymphovascular invasion (T2), but there was no regional lymph node metastasis (N0) or distant metastasis (M0). The patient was regularly followed up by abdominopelvic computed tomography (CT), chest CT and colonofiberoscopy at 1-year intervals; and blood tests (serum carcinoembryonic antigen [CEA] and carbohydrate antigen 19-9 levels) at 6-month intervals.
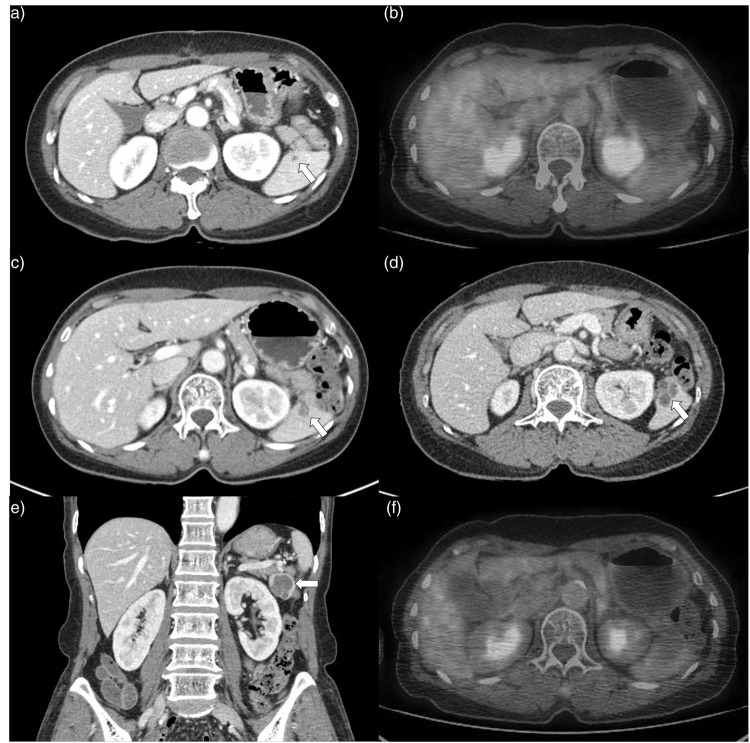
During a regular check-up, an ill-defined hypodense lesion at the spleen, with a maximum diameter of approximately 3 mm, was incidentally identified on an abdominopelvic CT scan performed in July 2014 (Figure 1a). A positron emission tomography CT (PET-CT) scan performed to exclude possible splenic metastasis revealed no significant 18F-fluorodeoxyglucose (FDG) uptake and no other remarkable findings (Figure 1b). During a follow-up CT scan in January 2017, the lesion was found to have increased in size to 1.2 × 0.7 cm and was ill-defined and lobulated with heterogeneously enhancing features (Figure 1c).
Figure 1.
Splenic mesothelial cyst in a 66-year-old woman with ascending colon cancer. Contrast-enhanced abdominopelvic computed tomography (CT) at first postoperative follow-up shows a 3-mm sized, ill-defined hypodense lesion (arrow) at the spleen (a). There was no significant 18F-fluorodeoxyglucose (FDG) uptake and no other remarkable findings on a positron emission tomography CT (PET-CT) scan (b). After the 3-year follow-up, the lesion had grown to 1.2 × 0.7 cm and had ill-defined, lobulated and heterogeneously enhancing features (arrow) on a CT scan (c). The lesion progressively enlarged and measured 2.3 × 2.5 cm 3 years later (6 years after the surgery). The characteristics had changed to being relatively well-defined, multilocular and low attenuation with enhancing septa (arrow) on axial (d) and coronal (e) CT images. There was no FDG uptake at the splenic lesion on a repeated PET-CT scan (f). The colour version of this figure is available at: http://imr.sagepub.com.
The lesion progressively enlarged to 2.3 × 2.5 cm by January 2020. It was relatively well-defined, multilocular and had low attenuation with enhancing septa (Figures 1d and 1e). A repeat PET-CT scan in January 2020 showed no FDG uptake at the splenic lesion (Figure 1f). Serum CEA level remained in the normal range throughout the follow-up period.
Despite the negative results on the PET-CT scan, the possibility of metastasis could not be ruled out due to the enlarging size and slight enhancement of the splenic lesion in a patient with primary ascending colon cancer. In particular, the enhancing wall or septae accompanying the splenic lesion is known as an important characteristic to distinguish a malignant cystic lesion from a benign cystic lesion because it could reflect viable cancerous tissue. In addition, another characteristic that can be differentiated from benign cystic lesions was that the borders were ill-defined. Since this lesion had an unclear margin from the beginning to the middle of the follow-up period, it was necessary to differentiate for metastasis. Furthermore, a metastatic lesion can look like this due to cystic or necrotic changes inside the tumour that occur as the tumour increases in size and cystic metastasis may have also resulted in a false-negative finding on PET-CT. Finally, a laparoscopic splenectomy was performed in February 2020. The resected spleen measured 7.0 × 4.5 × 4.5 cm, with the multi-lobulated cyst measuring 2.8 × 2.5 × 2.5 cm (Figure 2).
Figure 2.

The macroscopic view of the resected spleen containing a multilobulated cyst measuring 7.0 × 4.5 × 4.5 cm in a 66-year-old woman with ascending colon cancer. The colour version of this figure is available at: http://imr.sagepub.com.
The cyst was filled with a gelatinous material. Microscopic evaluation revealed a multilocular cyst lined with cuboidal-to-flat epithelial cells (Figures 3a and 3b). The adjacent splenic parenchyma appeared unremarkable. On immunohistochemistry, the lining cells were positive for calretinin and D2-40, which are mesothelial cell markers (Figures 3c and 3d). A final diagnosis of a mesothelial cyst of the spleen was established. The patient had no complications for up to 1 year postoperatively.
Figure 3.
Histopathological examination of the splenic mesothelial cyst from a 66-year-old woman with ascending colon cancer. Microscopic findings showed a multilocular cyst identified in the splenic parenchyma (haematoxylin and eosin, scale bar 500 µm) (a). The multilocular cyst was lined by cuboidal-to-flat epithelial cells and the adjacent splenic parenchyma appeared unremarkable (haematoxylin and eosin, scale bar 50 µm) (b). On immunohistochemical analysis, the lining cells appear positive for calretinin (scale bar 50 µm) (c) and D2-40 (scale bar 50 µm) (d), which are mesothelial cell markers. The colour version of this figure is available at: http://imr.sagepub.com.
This study was approved by the Institutional Review Board of Chungbuk National University Hospital (IRB No. 2021-01-025). All patient details have been de-identified. Written informed consent was obtained from the patient for treatment and publication of this manuscript and any accompanying images. The case report was produced in compliance with the EQUATOR Network CARE guidelines. 7
Discussion
Splenic cysts are rare and have a reported incidence of 0.07% in large autopsy studies and 0.5% in splenectomy studies. 8 They are classified as parasitic or non-parasitic in origin. 8 Non-parasitic cysts include primary cysts characterized by epithelial lining and secondary cysts (pseudocysts), which are more frequent and usually generated by traumatic events. 8 Primary epithelial cysts, which account for 10% of all splenic cysts, are further divided into dermoid, epidermoid or mesothelial, depending on the type of the lining cells on histopathological examination. 5
Mesothelial cysts may develop congenitally due to incomplete fusion and invagination of mesothelial-lined peritoneal surfaces, with subsequent secretion of fluid. 9 This theory explains the usual location of mesothelial cysts in the small bowel, mesentery, mesocolon and omentum. Other hypotheses explaining the genesis of primary splenic epithelial cysts include epithelial cell metaplasia from adjacent structures or vascular endothelium from peritoneal inclusions and embryonic inclusion of epithelial cells from adjacent structures. 9 Although common in children and young adults, mesothelial cysts are rare in older people. 4 However, in this current case, the mesothelial cyst was observed in a 66-year-old woman and it was suspected that the increase in the size of the splenic lesion was due to fluid accumulation within a late activated mesothelial cyst.
Most primary splenic epithelial cysts are clinically silent and are often found incidentally or due to an abdominal mass or abdominal pain on imaging techniques, such as ultrasound (USG) or CT.1,5,10 They are typically well-defined hypoechoic and hypodense lesion, with a thin or imperceptible wall, on USG and CT, respectively.1,5,6,10 On magnetic resonance imaging, the cysts are hypointense on T1-weighted images and hyperintense on T2- weighted images, without reinforcement after contrast injection.11–13 However, the signal intensity may vary depending on the contents of the cyst. 14 Mesothelial cysts of the spleen have been described in the literature as unilocular with smooth and well-defined margins, without enhancing portions.1,6,8,10 However, there are a few reports on multilocular mesothelial cysts, some of which were misdiagnosed as hydatid cysts due to their shape.5,15,16 The imaging findings and clinical characteristics of previously reported cases of splenic mesothelial cysts are detailed in Table 1.1,5,6,10–13,17
Table 1.
Summary of clinical characteristics and radiological features of previously reported cases of splenic mesothelial cyst.1,5,6,10–13,17
| Author | Age, years | Sex | Symptom | Finding on USG | Finding on CT | Finding on MRI | Treatment | Pathology | Follow-up |
|---|---|---|---|---|---|---|---|---|---|
| Kuwabara et al., 1993 1 | 29 | F | Abdominal mass | Splenomegaly containing anechoic well-marginated lesion with posterior enhancement | Splenomegaly including low density mass with calcified wall | NA | Splenectomy | Cyst originated from mesothelium | NA |
| Parihar et al., 2016 5 | 38 | F | Left upper abdominal pain | NA | Large, oval, multilocular, non-enhancing and cystic lesion | NA | Splenectomy | Multilocular mesothelial cyst | NED at 6 months |
| Vijayaraghavan et al., 2010 6 | 3rd decade | F | Left flank and upper abdominal pain | Features of a cyst | A splenic cyst | NA | Splenectomy | Mesothelial cyst | NED at 1 year |
| Elosua González et al., 2018 10 | 21 | F | Dyspepsia, left epigastrium-hypochondrium pain upon eating and weight loss | A 7-cm splenic lesion that was isoechoic, with little acoustic enhancement and well-defined contours | Oval-shaped lesion with well-defined contours in the spleen without both internal enhancements and solid poles | NA | Laparoscopic fenestration | Mesothelial cyst | NED at 6 months |
| Zvizdić et al., 2013 11 | 10 | F | Mild tenderness in left hypochondriac region | Solitary cyst with smooth wall and anechoic central areas | NA | Cyst larger than 5 cm | Partial splenectomy | Mesothelial cyst | NED at 9 days |
| Trompetas et al., 2002 12 | 21 | F | Fever and nausea | Large cyst | Large cyst | Large cyst | En bloc resection | Mesothelial cyst | NED at 2 months |
| Lucandri et al., 2011 13 | 25 | F | Pain in the left flank and hypochondrium, nausea and vomiting | Round mass at the splenic hilum with a fluid consistency and internal thin septa | Cystic mass with calcification of its wall | Cystic mass with many inner septa | Robotic splenectomy | Mesothelial cyst | NED at 6 days |
| Reddi et al., 1998 17 | 26 | M | Left upper abdominal mass | Cystic lesion without calcification | NA | NA | Splenectomy | Mesothelial cyst | NED at 10 months |
USG, ultrasound; CT, computed tomography; MRI, magnetic resonance imaging; F, female; NA, data not available; NED, no evidence of disease; M, male.
Hypodense lesions of the spleen are commonly found on CT images of the abdomen. 18 While most hypodense splenic lesions can be considered benign, additional findings, such as an ill-defined margin, the presence of a solid portion with contrast enhancement and the presence of an underlying malignancy, are important predictors of malignant splenic lesions, and more attention should be paid in such cases.19,20
Isolated splenic metastasis from colon cancer is extremely rare.21,22 Most cases of splenic metastasis occur at advanced stages (III or IV).21,22 However, there has been a report of metachronous isolated splenic metastasis from stage I colon cancer without blood vessel invasion. 22 On contrast-enhanced CT images, findings of ill-defined, hypodense and contrast-enhanced lesions in patients with known malignant tumours should be considered as splenic metastases until proven otherwise. Malignant tumours, including metastases, can appear as single or multiple cystic masses, complicating diagnosis.18,20,23 In this current case, due to overlapping imaging findings of hypodense splenic lesions, and considering the clinical history, it was acceptable that a mesothelial cyst that developed as a multilocular hypodense mass from an ill-defined small nodule in the patient with primary colon cancer was inevitably misdiagnosed as metastasis. Hydatid cysts, lymphangioma, haemangioma and epithelial cysts were differential diagnoses based on the appearance of the splenic lesion on the last follow-up CT scan.
Mesothelial cysts are considered benign with a good prognosis. 8 The accepted indications for treatment of splenic cysts include symptomatic cysts and cysts that are ≥ 5 cm due to a high risk of complications, such as rupture, bleeding and infection. 10 There are high rates of recurrence and complications with percutaneous treatment, such as aspiration and treatment with alcohol. 10 Surgery includes total or partial splenectomy, decapsulation (complete membrane extirpation) and fenestration (resection that puts the cavity of the cyst in contact with the peritoneum). 10 The current trend is toward spleen-sparing techniques to prevent immunosuppression and thrombocytosis. 24 Since the diagnosis considered in this current case was metastasis, complete splenectomy was performed regardless of size. 18
The present case shows that there can be diagnostic confusion on radiological imaging findings. In retrospect, the initial shape of the lesion was not that of a typical benign cystic lesion and increased in size, but the lesion grew slowly over a long period of time and was a relatively well-defined cystic lesion in the later stage. It has been overlooked that more consideration could be given to the possibility of benign cystic lesion rather than a malignant tumour. In the diagnosis of splenic lesions, both imaging findings and the patient's clinical history should be considered. However, certain CT imaging findings tend to overlap in several diseases, making it difficult to reliably distinguish between them. Unlike in other organs, USG-guided spleen biopsy may not be preferred because of the high risk of bleeding and unfavourable access due to poor acoustic windows. Therefore, the final diagnosis can only be made by histopathological examination of surgical specimens as previously suggested. 5
In conclusion, this current case report presented an atypical case of splenic mesothelial cyst mimicking a malignant tumour, especially splenic metastasis, in a patient with ascending colon cancer. Due to the overlapping imaging findings of the hypodense splenic lesions and consideration of the clinical history, a mesothelial cyst that developed as a multilocular hypodense mass from an ill-defined small nodule was inevitably misdiagnosed as metastasis. Although rare, it is important to consider the possibility of a mesothelial cyst as a differential diagnosis for multilocular hypodense lesions of the spleen.
Supplemental Material
Supplemental material, sj-pdf-1-imr-10.1177_03000605211031736 for Mesothelial cyst of the spleen mimicking a metastasis: a case report by Mihyeon Park, Jisun Lee, Yook Kim, Chi-Hoon Choi and Kil Sun Park in Journal of International Medical Research
Supplemental material, sj-pdf-2-imr-10.1177_03000605211031736 for Mesothelial cyst of the spleen mimicking a metastasis: a case report by Mihyeon Park, Jisun Lee, Yook Kim, Chi-Hoon Choi and Kil Sun Park in Journal of International Medical Research
Footnotes
Author contributions: M.P. and J.L.: study design and implementation, data collection/validation, data interpretation and major contributions to writing, editing and revising the manuscript; M.P., J.L., Y.K., C.H.C. and K.S.P.: project conceptualization, critical revision of the article, final approval of the version to be submitted. All authors have read and approved the manuscript.
Declaration of conflicting interest: The authors declare that there are no conflicts of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iDs: Jisun Lee https://orcid.org/0000-0002-6264-7171
References
- 1.Kuwabara S, Hohjoh H, Nakano M, et al. Mesothelial splenic cyst. Intern Med 1993; 32: 672–674. [DOI] [PubMed] [Google Scholar]
- 2.Esparza Estaun J, Gonzalez Alfageme A, Saenz Banuelos J. . Radiological appearance of diaphragmatic mesothelial cysts. Pediatr Radiol 2003; 33: 855–858. [DOI] [PubMed] [Google Scholar]
- 3.Carboni F, Valle M, Camperchioli I, et al. Mesothelial cyst of the round ligament of the liver. J Minim Access Surg 2016; 12: 83–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Swilem H, Albuni MK, Alkhateeb M, et al. Mesothelial cyst of the greater omentum as an uncommon cause of gastrointestinal bleeding: a case report. Clin Surg 2019; 4: 1–2. [Google Scholar]
- 5.Parihar A, Singh UR, Rathi V, et al. Multilocular Mesothelial Cyst of the Spleen Mimicking Hydatid Cyst on Imaging. J Clin Diagn Res 2016; 10: EJ01–EJ02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vijayaraghavan R, Chandrashekar R, Aithal S, et al. Mesothelial cyst of the spleen in an adult: a case report. BMJ Case Rep 2010; 2010: bcr0320102810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gagnier JJ, Kienle G, Altman DG, et al. The CARE guidelines: consensus-based clinical case reporting guideline development. Headache 2013; 53: 1541–1547. [DOI] [PubMed] [Google Scholar]
- 8.Ingle SB, Hinge Ingle CR, Patrike S. Epithelial cysts of the spleen: a minireview. World J Gastroenterol 2014; 20: 13899–13903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daga G, Mittal V, Singh R, et al. Epithelial cyst of the spleen. J Indian Assoc Pediatr Surg 2011; 16: 18–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elosua González A, Nantes Castillejo O, Tarifa Castilla A, et al. Primary mesothelial cyst of the spleen as an uncommon cause of dyspepsia: A case report. Rev Gastroenterol Mex (Engl Ed) 2018; 83: 463–465. [DOI] [PubMed] [Google Scholar]
- 11.Zvizdic Z, Karavdic K. Spleen-preserving surgery in treatment of large mesothelial splenic cyst in children: a case report and review of the literature. Bosn J Basic Med Sci 2013; 13: 126–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Trompetas V, Panagopoulos E, Priovolou-Papaevangelou M, et al. Giant benign true cyst of the spleen with high serum level of CA 19-9. Eur J Gastroenterol Hepatol 2002; 14: 85–88. [DOI] [PubMed] [Google Scholar]
- 13.Lucandri G, Felicioni F, Monsellato I, et al. Robotic splenectomy for mesothelial cyst: a case report. Surg Laparosc Endosc Percutan Tech 2011; 21: e93–e96. [DOI] [PubMed] [Google Scholar]
- 14.Robertson F, Leander P, Ekberg O. Radiology of the spleen. Eur Radiol 2001; 11: 80–95. [DOI] [PubMed] [Google Scholar]
- 15.Manoj MG, Misra P, Kakkar S. Multilocular epithelial cyst of spleen: a rare occurrence. Indian J Pathol Microbiol 2012; 55: 602–604. [DOI] [PubMed] [Google Scholar]
- 16.Kala PS, Azad S, Sharma T, et al. Primary epithelial splenic cyst: A rare encounter. Indian J Pathol Microbiol 2019; 62: 605–607. [DOI] [PubMed] [Google Scholar]
- 17.Reddi VR, Reddy MK, Srinivas B, et al. Mesothelial splenic cyst: a case report. Ann Acad Med Singap 1998; 27: 880–882. [PubMed] [Google Scholar]
- 18.Karlo CA, Stolzmann P, Do RK, et al. Computed tomography of the spleen: how to interpret the hypodense lesion. Insights Imaging 2013; 4: 65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thipphavong S, Duigenan S, Schindera ST, et al. Nonneoplastic, benign, and malignant splenic diseases: cross-sectional imaging findings and rare disease entities. AJR Am J Roentgenol 2014; 203: 315–322. [DOI] [PubMed] [Google Scholar]
- 20.Jang S, Kim JH, Hur BY, et al. Role of CT in differentiating malignant focal splenic lesions. Korean J Radiol 2018; 19: 930–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Compérat E, Bardier-Dupas A, Camparo P, et al. Splenic metastases: clinicopathologic presentation, differential diagnosis, and pathogenesis. Arch Pathol Lab Med 2007; 131: 965–969. [DOI] [PubMed] [Google Scholar]
- 22.Abdou J, Omor Y, Boutayeb S, et al. Isolated splenic metastasis from colon cancer: case report. World J Gastroenterol 2016; 22: 4610–4614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rabushka LS, Kawashima A, Fishman EK. Imaging of the spleen: CT with supplemental MR examination. Radiographics 1994; 14: 307–332. [DOI] [PubMed] [Google Scholar]
- 24.Soon DS, Shilton H, Andrabi A. Mesothelial inclusion cyst: a rare occurrence. J Surg Case Rep 2016; 2016: rjw213. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-imr-10.1177_03000605211031736 for Mesothelial cyst of the spleen mimicking a metastasis: a case report by Mihyeon Park, Jisun Lee, Yook Kim, Chi-Hoon Choi and Kil Sun Park in Journal of International Medical Research
Supplemental material, sj-pdf-2-imr-10.1177_03000605211031736 for Mesothelial cyst of the spleen mimicking a metastasis: a case report by Mihyeon Park, Jisun Lee, Yook Kim, Chi-Hoon Choi and Kil Sun Park in Journal of International Medical Research