Abstract
Purpose
We examined ideas about how youth would mitigate non-medical use of prescription medications among their peers.
Design/methodology/approach
The National Monitoring of Adolescent Prescription Stimulants Study (N-MAPSS) interviewed 11,048 youth10–18 years of age between 2008 and 2011 from entertainment venues of 10 US urban, suburban, and rural areas. Using a mixed-methods approach, participants completed a survey culminating in open ended questions asking: 1) How should kids your age be told about prescription drugs and their effects?; 2) If you ran the world, how would you stop kids from taking other people’s prescription medicines?; 3)Why do people use prescription stimulants without a prescription? Responses from a random sample of 900 children were analyzed using qualitative thematic analyses.
Findings
The random sample of 900 youth (52% female, 40% white, with a mean age was 15.1 years) believed they should be educated about prescription drugs and their negative effects at schools, at home by parents, through the media, and health professionals. Youth would stop kids from using other people’s prescription drugs through more stringent laws that restricted use, and education about negative consequences of use. Peer pressure was the most common reason youth gave for using other’s pills, though some reported using for curiosity.
Originality/value
This analysis shows the importance of considering youth’s opinions on non-medical use of prescription medications, which are often overlooked. Studies should disseminate this data from youth to stop the illicit use of prescription drugs among teens and youth.
Keywords: Prescription drug use, Adolescents, Mixed-methods, United States
Introduction
Substance use by youth continues to be a public health concern even though rates of substance use among youth have been on a decline over the past 20 years in the United States (US) [1]. Some of the most commonly used substances among youth are alcohol and tobacco, followed by marijuana [2, 3]. Studies report that between 20–35% of youth used alcohol in the past 30 days [4–6], while approximately 25% used tobacco in the past 30 days [7], and nearly 22% of 12th graders used marijuana in the past 30 days [8]. Additionally, the type of substance used differs by age group and gender among youth. Younger teens are more likely to use substances they can inhale compared to older teens who are more likely to non-medically use prescription medications [2]. In addition, even though males are more likely to use prescription medications compared to females overall, females aged 12–17 are more likely to use prescription medications non-medically when compared to males overall [9–11].
Non-medical use is commonly defined as using a prescription drug that was not prescribed for you, taking a medication in a manner or dose other than prescribed, or taking a medication to feel euphoria [12, 13]. The classes of prescription drugs that are typically used non-medically include stimulants, opioids, and sedatives [1]. Youth are sometimes prescribed these medications by a physician, but may also access and use prescriptions non-medically from their family’s medicine cabinet [14]. In the US, the National Survey on Drug Use and Health (NSDUH) reports that 5.9% of youth used a prescription non-medically used a prescription in the past 30 days [15]. Non-medical use of prescription drugs among youth is especially problematic due to the critical period of development in adolescents during this time; youth are at highest risk for experimentation and addiction. Further, youth may perceive prescription medications as less harmful compared to other drugs [16], even though they can cause serious side effects. For example, stimulants can cause paranoia and an irregular heartbeat while opioids can cause drowsiness and nausea; depressants can cause slurred speech and shallow breathing [17]. Non-medical use of prescription medications among youth is not only harmful to the development of the adolescent brain and body, but also has social consequences that may include delinquency [18], school dropout [19], abuse and subsequently dependence [20, 21].
There are many factors contributing to non-medical use of prescription drugs among youth. Established characteristics include being female [19, 22] and Caucasian [19, 23]. Use has been found to increase with age [22]. Individual risk factors such as deviant [24] and sensation seeking behaviors [25], and peer influence [26] are two of the main reasons youth initiate use of prescription drugs non-medically. Other risk factors include previous medical use of prescription drugs [22], availability [27], and urbanicity [28]. In addition to these risk factors, there are protective factors for non-medical use of prescription drug use including parental monitoring [29] and academic achievement [19].
The United States utilizes multiple national surveys to equip researchers to better understand the use of prescription drugs among youth including trends and changes over time, and implementation of interventions. National surveys such as Monitoring the Future (MTF), funded by the National Institute on Drug Abuse (NIDA), have assessed substance use and related attitudes among youth nationwide since 1975. The Youth Risk Behavior Surveillance System (YRBSS) conducted by the Centers for Disease Control and Prevention (CDC) tracks tobacco, alcohol, and other drugs used among youth. Further, the NSDUH, by the Substance Abuse and Mental Health Services Administration (SAMHSA), includes information regarding trends in the use of alcohol, tobacco, and various types of drugs from individuals aged 12 years or older. In addition, school-based programs including the Drug Abuse Resistance Education (DARE) program has been implemented to educate youth on the harms of drug use and to prevent the initiation of drug use. Other national representative studies such as the National Monitoring of Adolescent Prescription Stimulants Study (N-MAPSS) have been used to examine signals for non-medical use of stimulants and other drugs. Results from N-MAPSS show that approximately 4% of youth reported prescription stimulant non-medical use in the past 30 days [30] and 3% used prescription opioids non-medically in the past 30 days [11]. Prevalence of other substance use has also been examined in this dataset. Though many of the national surveys described above assess data that is necessary to understand prescription drug use among youth, N-MAPSS also included open-ended questions to probe youth on their opinions on why people use prescription drugs non-medically, how to educate, and how to stop kids from using prescription drugs non-medically.
Our aims were to: examine perceptions of prescription drugs, their effects, and ideas on how youth would stop non-medical use of prescription medications among their peers. The aims of this study were addressed with the following questions on the survey: 1) How should kids your age be told about prescription drugs and their effects?; 2) If you ran the world, how would you stop kids from taking other people’s prescription medicines?; and 3) Why do people use prescription stimulants without a prescription? We hypothesized that, helpful themes would emerge on how youth of different ages perceived prescription drugs, their effects, and ideas on how to stop non-medical use among them and their peers.
Methods
Study Design
N-MAPSS was a national study conducted between 2008 and 2011 in four waves. The cross-sectional study design assessed medical and non-medical use of prescription drugs (stimulants, opioids, etc.). Participants were eligible for this study if they were between the ages of 10 and 18 years and resided in Seattle, Los Angeles, Denver, St. Louis, Houston, Cincinnati, Tampa, Philadelphia, New York or Boston; these cities and their surrounding areas were representative of urban, suburban, and rural areas. Exclusion criteria included non-English readers, those enrolled in college, and those who could not identify their zip code. Participants were recruited from local entertainment and other venues (i.e., parks, movie theaters, shopping malls, sports and recreation centers) in the 10 sites listed above from across the US. This venue intercept method allowed N-MAPSS to recruit a representative sample of youth with recruitment goals including urban, suburban, and rural areas to ensure participation from youth in all areas. N-MAPSS included a representative sample distribution that was comparable to US Census data. Detailed methodological information including categorization of urban, suburban, and rural areas is published elsewhere [30].
During the four waves, 21,444 youth were approached. Of 16,143 potentially eligible youth who stopped to hear about the study, 3,403 (21%) were ineligible (not between 10 and 18 years old and resided outside of an urban, suburban or rural zip code of one of ten cities). Of the 12,740 eligible youth, 1,272 (10%) who were approached decided they were not interested in hearing more about the study and 420 (3%) did not complete the survey. The total sample size included 11,048 youth who completed the survey. Participants aged 10 to 11 years of age were offered the opportunity to be interviewed with the survey in order to reduce problems with reading and comprehension. This study was approved in 2008 by the Human Research Protection Office at Washington University in St. Louis. Implied assent was obtained. Parental permission was removed as a requirement of the study by Washington University since all survey data were anonymous. The study PI moved to the University of Florida in 2011 and the Humans Studies Office there also approved the study.
Measurements
Youth completed a paper survey, including questions about prescription medications presented with pictures of these medications for ease of identification. At the end of the survey, a mixed methods approach was used to ask youth to respond to three open-ended questions on ideas about how to educate peers about prescription drugs, how to stop people from using prescription drugs, and why people use prescription drugs that don’t belong to them [31–33]. Specifically, we asked three open-ended questions: 1) “How should kids your age be told about prescription drugs and their effects? 2) If you ran the world, how would you stop kids from taking other people’s prescription medicines?; 3) Why do people use prescription stimulants without a prescription?” Responses to these questions were typically between three to five words long.
Demographic characteristics of interest captured through questionnaire items included gender (male or female), age (10 through 18), race and ethnicity (Alaskan Native/Eskimo, American Indian, Asian or Asian-American, Back or African-American, Middle Eastern, Pacific Islander, White/Euro-American/Caucasian, biracial or multiracial), school grade enrolled in currently or most recently completed (grades 3 through 12), and urbanicity. The drug use items reported on in these analyses included prescription stimulant use (past 30 day use, yes/no) and marijuana use (lifetime use, yes/no).
Data analysis
Because a sample of 11,048 youth would be difficult to analyze for this mixed methods effort, we establish emerging trends, themes and categories by generating a sample of 100 youth (300 observations) and coding data using two team members “to think without distraction” [34]. Inconsistencies between coders were discussed and recoded; saturation was met.
Then, a random sample of 900 youth was generated (2,700 observations) from the sample of 11,048 youth, using the proc surveyselect statement in SAS and weighted to fit the age distribution of the larger quantitative study. The full N-MAPSS data set was comprised of 13% 10 to 12 years (n=1,436), 40% 13–15 years (n=4,419), and 47% 16–18 years (n=5,193). The generated sample of 900 youth was weighted as described above to choose 115 10 to 12 year olds, 357 13 to 15 year olds and 428 16 to 18 year olds. Survey responses were coded using the original themes that were identified by the two coders; more than one theme was allowed to be coded per response. Frequencies for demographic characteristics were tabulated in SAS [35].
Results
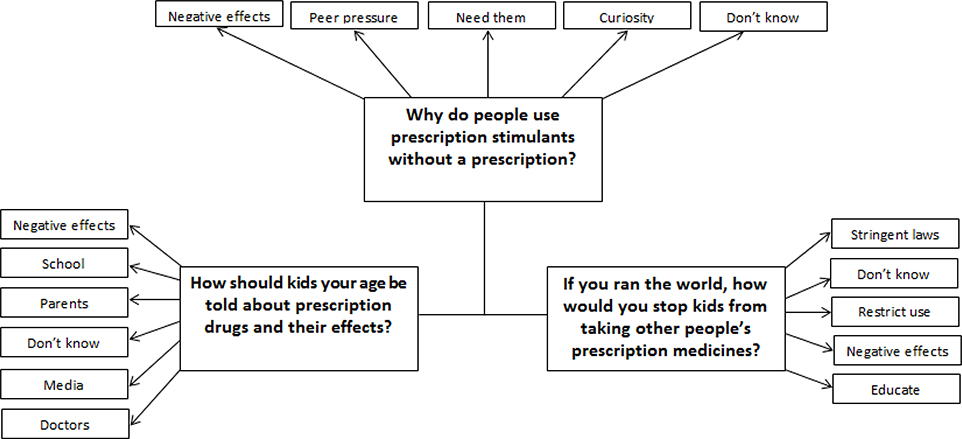
Among the entire N-MAPSS sample (n=11,048), 52% were female, 43% white, 48% resided in urban communities and the mean age was 15.1 years. As expected, demographics for the 900 youth randomized for these qualitative questions were similar with 52% female, 40% white, and 48% residing in urban communities with the same mean age (table 1). The themes that emerged for each qualitative question were determined by the coders and are outlined below (figure 1).
Table 1.
Baseline characteristics of N-MAPSS youth randomized by age group, (n=900)
| Characteristic | Entire sample (n=11,048)N ( %) | Sub-sample (n=900) N ( %) | Group 1(10–12 year olds) (n= 115) N ( %) | Group 2 (13–15 year olds) (n= 357) N ( %) | Group 3(16–18 year olds) (n= 428) N ( %) |
|---|---|---|---|---|---|
| Mean age, years (SD) | 15.2 (2.1) | 15.1 (2.1) | 11.21 (0.8) | 14.11 (0.8) | 16.9 (0.8) |
| Sex, % female | 5,762 (52.2) | 469 (52.1) | 60 (52.2) | 159 (53.0) | 226 (52.8) |
| Race, % white | 4,715 (42.9) | 356 (39.8) | 37 (32.7) | 204 (57.1) | 173 (40.6)) |
|
Education Grade 3– 8 Grade 9–12 |
3,218 (29.2) 7,830 (70.0) |
253(28.1) 647 (71.9) |
115 (100.0) 0 (0.0) |
158 (44.3) 199 (55.7) |
1 (0.2) 427 (99.8) |
| Urbanicity | 5,256 (47.6) | 432 (48.0) | 55 (47.8) | 178 (49.9) | 206 (48.1) |
| Stimulant use (Past 30 days) | 1,371 (12.4) | 99 (11.0) | 12 (10.4) | 38 (10.6) | 63 (14.7) |
| Marijuana use (Lifetime) | 3,320 (29.1) | 263 (29.5) | 4 (3.5) | 69 (19.3) | 196 (45.8) |
Figure 1.
Diagram representing the themes that emerged for each of three qualitative questions
How should kids your age be told about prescription drugs and their effects?
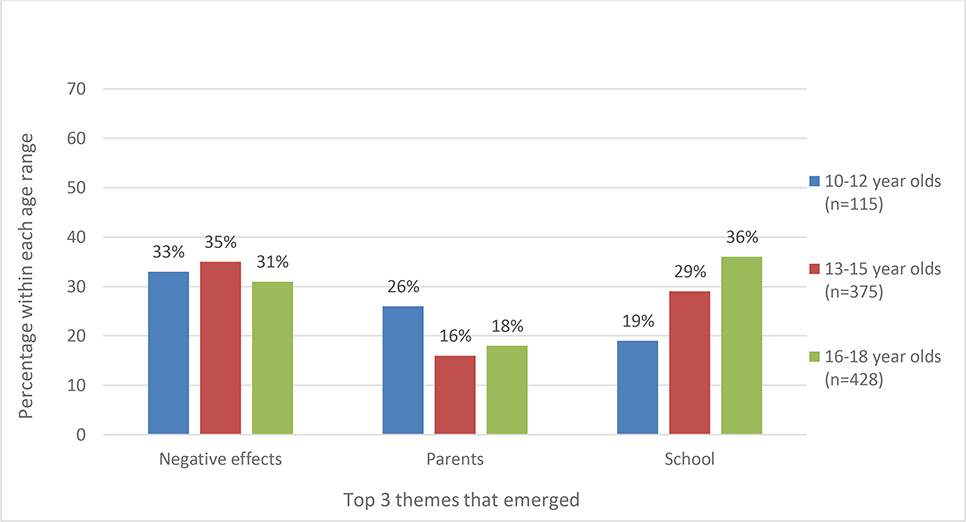
When youth were asked how they should be told about prescription drugs and their effects, the top 3 themes that emerged included negative effects, school, and parents (figure 2). Many youth (n=297; 33%) believed children should be told about the negative effects of prescription drug use, saying “they should be told how bad they are for your health” and “that they are dangerous and taking them with recreational goals can lead to death.” It was also believed that users should tell their personal narratives to educate kids about the negative consequences related to use. For example, one youth suggested, “I think by having speakers come and talk about their personal use is very effective.” The second largest theme to emerge (n= 276; 31%) was school and teacher sources. For example, “teachers in health class” and “school assemblies” were examples of the common responses. After schools, parents/guardians was the third largest medium mentioned (n=165; 18%). Youth believed parents or caretakers should be the ones to educate kids on prescription drugs and their effects. Common responses included “by parents starting from a young age.” School was a more common theme in the older age groups while parents were a more common theme among the younger age group (10–12 year olds).
Figure 2.
How should kids your age be told about prescription drugs and their effects?
The remaining themes that are not included in figure 2 included not knowing how to educate kids on prescription drug use (n=117; 13%) with common responses like “I really don’t know” or simply “just don’t use them.” Another theme that emerged was media advertising (n=101; 11%) such as “a television through commercials” because kids watch and listen to television and radio. The remaining theme was through health professionals (n=87; 10%) such as doctors or prescribers.
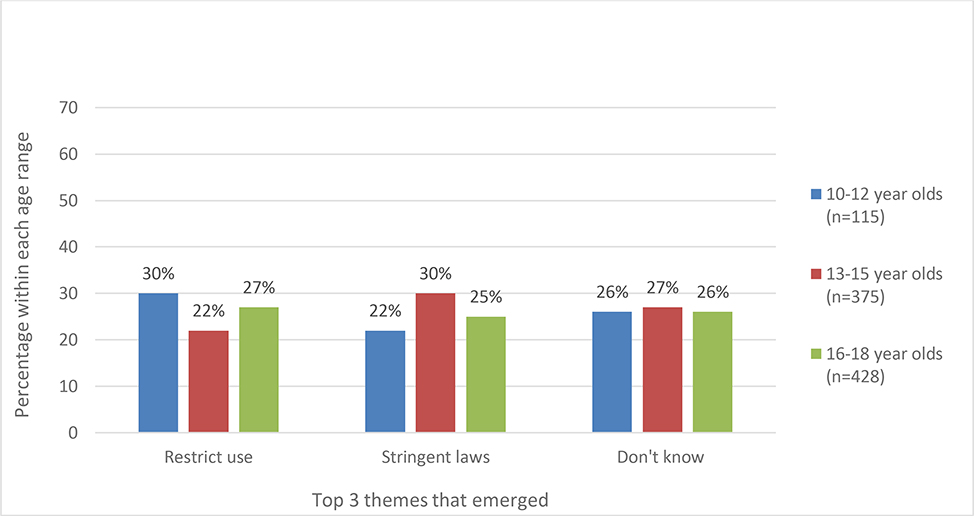
If you ran the world, how would you stop kids from taking other people’s prescription medicines?
When youth were asked this question, the 3 most common themes to emerge included restricting use, enforcing more stringent laws, and not knowing how (figure 3). The most common theme was to implement more stringent laws. These youth (n=240; 27%) believed creating laws and punishments if laws were broken would help stop the use of other people’s prescription drugs. Some suggested examples such as “put them in juvie (detention center or court for juvenile offenders)” and “make a law against it.” Many youth (n= 237; 26%) did not know how to stop kids from taking other’s prescription drug and this was the second most common theme. Responses included “I honestly don’t know” and “I’m not sure. That’d be the least of my worries if I ruled the world.” The third largest theme to emerge was the restriction of prescription drugs (n=228; 25%); youth suggested banning prescription drugs all together: “they wouldn’t exist” and “I would take them away from everyone.” Others also suggested implementing security measures would help reduce prescription drug use. Some of these responses included “put a lock on the bottle with a combo,” “make sure every pill is tracked,” and “make them go to the store and buy 1 for each day.” When youth were stratified by age, restricting use was the most common theme among 10–12 year olds while implementing stringent laws was most common among 13–15 year olds.
Figure 3.
If you ran the world, how would you stop kids from taking other people’s prescription medicines?
After restricting use, discussing negative consequences was the most common theme (not included in figure 3). These youth (n=151; 17%) believed children should be told about the negative consequences related to using prescription drugs that do not belong to them. Responses included stating “how bad the drug is and what it may cause” and stating that they would “show them the long-term mental health effects.” The remaining youth (n=51) believed education was the way to stop kids from using prescription drugs. Responses included “by educating kids on the hazards of these medicines” or “reduce use by increasing awareness throughout the world.”
Why do people use prescription stimulants without a prescription?
Lastly, when youth were asked this question the top responses included, “because of the effects” and “peer pressure”. The “effects” response was the most common theme regardless of age (n=538; 60%); the rate of this response increased with age (figure 4). Youth believed stimulant use without a prescription was due to the good feelings prescription stimulants can cause and common responses included “to get high” and “feel better” and the effects from use would “make them happy and relieve their pain” or help them “forget their problems.” The second largest theme to emerge was use by peer pressure. Youth who mentioned this (n=136; 15%) thought people used prescription stimulants without a prescription in order to fit in with others around them. Common responses included “to look good in front of friends” and “peer pressure.” The peer pressure response decreased with age.
Figure 4.
Why do people use prescription stimulants without a prescription?
The remaining youth (n=111; 12%) believed individuals could not afford prescription stimulants but needed them. Some responded with “they probably can’t afford it but need it,” or “maybe because they don’t have insurance.” Others answered that they did not know why youth used prescription stimulants without prescriptions (n=90; 10%). Finally, some (n=83; 9%) believed that those who used prescription stimulants without a prescription were curious and were experimenting because they never tried it before. These youth commonly responded with “just being curious” or “because they don’t know what it does.”
Discussion
Among a sample of over 11,000 youth, we assessed perceptions of prescription drug use and ways these youth would stop non-medical use of prescription drugs. Youth believed they should be educated about the negative effects related to prescription drug use, that education efforts should be included in their formal education at school or that they should be informed through their parents. Parental education was a more common theme among younger children 10–12 years, while school education was a more common theme among older children 16–18 years of age. These results suggest that education efforts for prescription drugs may need to be delivered through different sources depending on youth age groups. Parents may have a greater influence on younger children, who expect their parents to educate them on prescription drugs, while formal education in schools may have a greater influence on older children and adolescents.
Additionally, if youth ruled the world, they would stop kids from taking other people’s prescription drugs by implementing more stringent laws. Differences emerged by age groups, where restricting use was the most common theme among those aged 10–12 years of age. Implementing stringent laws was more common among 13–15 year olds. This suggests that strategies restricting access to other people’s prescription drugs may have a greater influence on younger children, who believe this would be effective. Conversely, older children and adolescents appear to be more motivated by legal consequences and the threat of punishment.
Interestingly, we found that youth, regardless of age, most commonly believed the main motivation for non-medical use of prescription stimulants was for their psychoactive effects. It was a most common belief among 16 to 18 year olds (67%) compared to every other answer they gave, as well as the younger cohorts. This may be potentially related to the increasing pressure to perform academically. Previous studies have found an association between prescription stimulant use and cognitive enhancement among college students [36–38]. In our study, the motivation of peer pressure decreased with age. The youth who were the youngest (10–12 year olds) believed non-medical use was due to peer pressure more frequently compared to older youth. Other studies have found substance use is often influenced by social networks and factors such as peer pressure [39–42]. These findings suggest that motivations for non-medical use of prescription stimulants may change as adolescents mature.
The sampling technique used in N-MAPSS resulted in prevalence rates of prescription drug use among youth that were similar to those found by traditional national surveys. In the last few decades, national surveys have examined prescription drug use among youth using quantitative surveys. In addition, some qualitative studies have used a focus group approach to gain a better understanding of attitudes and perceptions on substance use [43,44]. Uniquely, N-MAPSS not only surveyed youth about their own use, but also used a mixed methods approach to assess perspectives of youth on how to stop non-medical use of prescription drugs. Though surveys such as these are an integral part of monitoring prescription drug use among youth, supplementing measures with qualitative data can help to understand opinions and concerns of youth regarding prescription drugs. Results from studies like N-MAPSS, that include both quantitative and qualitative measures, can be used to better understand the non-medical use of prescription drugs among youth and to find possible interventions to reduce such use [31–33].
We had the opportunity to analyze qualitative questions embedded in a larger quantitative study to get a better understanding of prescription drug use among youth. Results from this study are most relevant in today’s epidemic. Previous nation-wide prevention programs such as the D.A.R.E. program have been shown not to be effective in the long-term. In fact, the literature has shown that D.A.R.E. was minimally effective [45, 46] and during five year follow-up periods no significant differences were observed between intervention and comparison schools [47]. More recently, D.A.R.E. has revised their curriculum to include decision making skills and social competence. Preliminary results from the revised curriculum have shown higher efficacy in preventing substance use [48]. Integrating perspectives from youth, such as the results from this current study, and teaching youth social skills into future prevention programs that target the prevention of drug use among youth may be a more effective prevention strategy. Assumptions by adults about non-medical use among youth can be avoided with this approach and resources can be directed to the most appropriate settings. For instance, integrated education efforts from multiple outlets including the media and doctor visits may be more effective than efforts delivered solely within a school setting. Using parental based education efforts in younger children and then gradually increasing school based efforts as children get older may also be an effective approach, based on our results.
Some limitations of the data include the cross-sectional nature of the study, meaning that cohort changes over time cannot be examined. Data were also self-reported, which could lead to under-reporting of comments on the questions to begin with. In addition, age differences were not empirically tested. However, these preliminary analyses examined through a mixed methods approach have highlighted thematic differences by age among youth that need to be further examined. Gender differences and thematic differences that may emerge between youth who use and don’t use prescription drugs non-medically should also be further examined. It should be noted that the data collected covers a broad time period (2008–2011) and may not reflect current prescription drug practices. However, the qualitative information ascertained from the youth can be translated for interventional purposes regarding the mitigation of non-medical use of prescription medications among their peers and these ideas transcend time.
This study had many strengths in addition to using mixed methods to better understand youth and their perspectives on prescription drug use. The questions analyzed were open-ended and responses were clear and unambiguous allowing easy identification of themes. This entertainment venue methodology was successful, with only 10% of participants declining to participate, allowing recruitment of a large data set of youth in a short period. Age, sex, race and composition of urban and rural areas of this sample in N-MAPSS were also comparable to the 2010 US Census data.
Overall, the themes we observed in this study varied and identify some useful clues for moving forward. For example, younger children appear to have different views and suggestions to those of older adolescents. This suggests that different targeted approaches by age group would be useful to consider, considering the themes identified when asking about education, prevention and motivation. Strategies may be more effective if designed based on the opinions of the youth themselves, rather than the preconceived ideas of adults about the opinions of youth.
Conclusion
Though many national surveys quantify trends and changes in prevalence of prescription drug use among youth, no study thus far has asked youth about their perceptions directly from youth regarding their ideas on prescription drugs and how they would prevent non-medical use. This current analysis uses qualitative methods to examine prescription drug use among youth and obtain their insight on future prevention strategies of non-medical use. These results suggest that further research among this age population should focus on prevention strategies more central to the youth, without making assumptions about drug use behavior.
Funding
Shire Development LLC and Noven Therapeutics and University of Florida Substance Abuse Training Center in Public Health T32DA035167
Contributor Information
Mirsada Serdarevic, Center for Outcomes Research, JPS Health Network, Texas, United States.
Vicki Osborne, Drug Safety Research Unit, Southampton, Southampton, United Kingdom of Great Britain and Northern Ireland.
Amy Elliott, University of Florida, Gainesville, Florida, United States.
Catherine W Striley, University of Florida, Gainesville, Florida, United States.
Linda B Cottler, University of Florida, Gainesville, Florida, United States.
References
- 1.National Institute on Drug Abuse. Summary [Internet]. 2017. [cited 2017 May 23]. Available from: https://www.drugabuse.gov/publications/research-reports/misuse-prescription-drugs/summary
- 2.National Institute on Drug Abuse. What drugs are most frequently used by adolescents? [Internet]. 2017. [cited 2017 May 23]. Available from: https://www.drugabuse.gov/publications/principles-adolescent-substance-use-disorder-treatment-research-based-guide/frequently-asked-questions/what-drugs-are-most-frequently-used-by-adolescents
- 3.Office of the Surgeon General (US), National Institute on Alcohol Abuse and Alcoholism (US), Substance Abuse and Mental Health Services Administration (US). The Surgeon General’s Call to Action To Prevent and Reduce Underage Drinking [Internet]. Rockville (MD): Office of the Surgeon General (US); 2007. [cited 2017 May 23]. (Publications and Reports of the Surgeon General). Available from: http://www.ncbi.nlm.nih.gov/books/NBK44360/ [PubMed] [Google Scholar]
- 4.NSDUH. Population Data [Internet]. 2017. [cited 2017 May 23]. Available from: data/population-data-nsduh/reports
- 5.Kann L Youth Risk Behavior Surveillance — United States, 2015. MMWR Surveill Summ [Internet]. 2016. [cited 2017 May 23];65. Available from: http://www.cdc.gov/mmwr/volumes/65/ss/ss6506a1.htm [DOI] [PubMed] [Google Scholar]
- 6.Johnston L, O’Malley P, Miech R, Bachman J, Schulenberg je. Monitoring the future national survey results on drug use, 1975–2015: 2015 Overview- Key findings on adolescent drug use. 2015; Available from: http://www.monitoringthefuture.org/pubs/monographs/mtf-overview2015.pdf
- 7.Centers for Disease Control and Prevention. Smoking and Tobacco Use; Fact Sheet; Youth and Tobacco Use [Internet]. Smoking and Tobacco Use. 2018. [cited 2017 May 23]. Available from: http://www.cdc.gov/tobacco/data_statistics/fact_sheets/youth_data/tobacco_use/
- 8.Centers for Disease Control and Prevention. Cigarette, Cigar, and Marijuana Use Among High School Students — United States, 1997–2013 [Internet]. 2015. [cited 2018 Jul 19]. Available from: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6440a2.htm
- 9.Nakawaki B, Crano WD. Predicting adolescents’ persistence, non-persistence, and recent onset of nonmedical use of opioids and stimulants. Addict Behav. 2012. June 1;37(6):716–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Institute on Drug Abuse. Gender differences [Internet]. 2017. [cited 2017 May 23]. Available from: https://www.drugabuse.gov/publications/research-reports/prescription-drugs/trends-in-prescription-drug-abuse/gender-differences
- 11.Osborne V, Serdarevic M, Crooke H, Striley C, Cottler LB. Non-medical opioid use in youth: Gender differences in risk factors and prevalence. Addict Behav. 2017. September;72:114–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zacny J, Bigelow G, Compton P, Foley K, Iguchi M, Sannerud C. College on Problems of Drug Dependence taskforce on prescription opioid non-medical use and abuse: position statement. Drug Alcohol Depend. 2003. April 1;69(3):215–32. [DOI] [PubMed] [Google Scholar]
- 13.National Institute on Drug Abuse. Summary of Misuse of Prescription Drugs [Internet]. 2018. [cited 2018 Mar 6]. Available from: https://www.drugabuse.gov/publications/research-reports/misuse-prescription-drugs/summary
- 14.Cottler LB, Kwiatkowski E, Striley CW. What’s in your medicine cabinet? Gender differences. Drug and Alcohol Dependence. 2017;100(171):e46–7. [Google Scholar]
- 15.National Institute on Drug Abuse. Adolescents and young adults [Internet]. 2017. [cited 2017 May 23]. Available from: https://www.drugabuse.gov/publications/research-reports/prescription-drugs/trends-in-prescription-drug-abuse/adolescents-young-adults
- 16.Quintero G, Peterson J, Young B. An Exploratory Study of Socio-Cultural Factors Contributing to Prescription Drug Misuse among College Students. J Drug Issues. 2006. October 1;36(4):903–31. [Google Scholar]
- 17.SAMHSA. Teen Prescription Drug Misuse and Abuse [Internet]. 2016. [cited 2017 May 23]. Available from: https://www.samhsa.gov/homelessness-programs-resources/hpr-resources/teen-prescription-drug-misuse-abuse
- 18.Catalano RF, White HR, Fleming CB, Haggerty KP. Is nonmedical prescription opiate use a unique form of illicit drug use? Addict Behav. 2011. January;36(1–2):79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ford JA. Nonmedical Prescription Drug Use Among Adolescents: The Influence of Bonds to Family and School. Youth Soc. 2009. March 1;40(3):336–52. [Google Scholar]
- 20.McCabe SE, West BT, Teter CJ, Boyd CJ. Trends in medical use, diversion, and nonmedical use of prescription medications among college students from 2003 to 2013: Connecting the dots . Addict Behav. 2014. July;39(7):1176–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Institute on Drug Abuse. Prescription Drug Abuse [Internet]. 2010. [cited 2017 May 23]. Available from: https://www.drugabuse.gov/about-nida/legislative-activities/testimony-to-congress/2010/09/prescription-drug-abuse
- 22.Boyd CJ, Esteban McCabe S, Teter CJ. Medical and nonmedical use of prescription pain medication by youth in a Detroit-area public school district. Drug Alcohol Depend. 2006. January 4;81(1):37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Simoni-Wastila L, Yang H-WK, Lawler J. Correlates of prescription drug nonmedical use and problem use by adolescents. J Addict Med. 2008. March;2(1):31–9. [DOI] [PubMed] [Google Scholar]
- 24.Harrell ZAT, Broman CL. Racial/ethnic differences in correlates of prescription drug misuse among young adults. Drug Alcohol Depend. 2009. October 1;104(3):268–71. [DOI] [PubMed] [Google Scholar]
- 25.Herman-Stahl MA, Krebs CP, Kroutil LA, Heller DC. Risk and protective factors for nonmedical use of prescription stimulants and methamphetamine among adolescents. J Adolesc Health Off Publ Soc Adolesc Med. 2006. September;39(3):374–80. [DOI] [PubMed] [Google Scholar]
- 26.Peters RJ, Meshack AF, Kelder SH, Webb P, Smith D, Garner K. Alprazolam (Xanax) use among southern youth: beliefs and social norms concerning dangerous rides on “handlebars.” J Drug Educ. 2007;37(4):417–28. [DOI] [PubMed] [Google Scholar]
- 27.Office of National Drug Control Policy. (ONDCP) Teens and prescription drugs: An analysis of recent trends on the emerging drug threat. 2007. Retrieved from: 2007; Available from: http://www.mediacampaign.org/teens/brochure.pdf.
- 28.Hall MT, Howard MO, Mccabe SE. Prescription Drug Misuse Among Antisocial Youths. J Stud Alcohol Drugs. 2010. November 1;71(6):917–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beyers JM, Toumbourou JW, Catalano RF, Arthur MW, Hawkins JD. A cross-national comparison of risk and protective factors for adolescent substance use: the United States and Australia. J Adolesc Health. 2004. July;35(1):3–16. [DOI] [PubMed] [Google Scholar]
- 30.Cottler LB, Striley CW, Lasopa SO. Assessing prescription stimulant use, misuse, and diversion among youth 10–18 years of age. Curr Opin Psychiatry. 2013. September;26(5):511–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schram AB. A Mixed Methods Content Analysis of the Research Literature in Science Education. Int J Sci Educ. 2014. October 13;36(15):2619–38. [Google Scholar]
- 32.Creswell J, Klassen A, Plano Clark V, Smith K. Best practices for mixed methods research in the health sciences. 2013.
- 33.Creswell JW, Plano Clark VL (Lynn). Designing and Conducting Mixed Methods Research (2nd International Edition). SAGE Publications, Inc; 2011. [Google Scholar]
- 34.Richards L, Morse JM. README FIRST for a User’s Guide to Qualitative Methods. 3rd ed. SAGE Publications, Inc; 2013. 336 p. [Google Scholar]
- 35.SAS Institute Inc., 9.4, Cary, NC: SAS Institute Inc., 2011. [Google Scholar]
- 36.McCabe SE, Knight JR, Teter CJ, Wechsler H. Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addict Abingdon Engl. 2005. January;100(1):96–106. [DOI] [PubMed] [Google Scholar]
- 37.Franke AG, Bonertz C, Christmann M, Huss M, Fellgiebel A, Hildt E, et al. Non-medical use of prescription stimulants and illicit use of stimulants for cognitive enhancement in pupils and students in Germany. Pharmacopsychiatry. 2011. March;44(2):60–6. [DOI] [PubMed] [Google Scholar]
- 38.Hall KM, Irwin MM, Bowman KA, Frankenberger W, Jewett DC. Illicit use of prescribed stimulant medication among college students. J Am Coll Health J ACH. 2005. February;53(4):167–74. [DOI] [PubMed] [Google Scholar]
- 39.McDonough MH, Jose PE, Stuart J. Bi-directional Effects of Peer Relationships and Adolescent Substance Use: A Longitudinal Study. J Youth Adolesc. 2016. August;45(8):1652–63. [DOI] [PubMed] [Google Scholar]
- 40.Mayberry ML, Espelage DL, Koenig B. Multilevel modeling of direct effects and interactions of peers, parents, school, and community influences on adolescent substance use. J Youth Adolesc. 2009. September;38(8):1038–49. [DOI] [PubMed] [Google Scholar]
- 41.Kristjansson AL, Sigfusdottir ID, Allegrante JP. Adolescent substance use and peer use: a multilevel analysis of cross-sectional population data. Subst Abuse Treat Prev Policy. 2013. July 31;8:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chan GCK, Kelly AB, Carroll A, Williams JW. Peer drug use and adolescent polysubstance use: Do parenting and school factors moderate this association? Addict Behav. 2017. January;64:78–81. [DOI] [PubMed] [Google Scholar]
- 43.Alhyas L, Al Ozaibi N, Elarabi H, El-Kashef A, Wanigaratne S, Almarzouqi A, et al. Adolescents’ perception of substance use and factors influencing its use: a qualitative study in Abu Dhabi. JRSM Open. 2015. February 1;6(2):2054270414567167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Menghrajani P, Klaue K, Dubois-Arber F, Michaud P-A. Swiss adolescents’ and adults’ perceptions of cannabis use: a qualitative study. Health Educ Res. 2005. August 1;20(4):476–84. [DOI] [PubMed] [Google Scholar]
- 45.West SL, O’Neal KK. Project D.A.R.E. Outcome Effectiveness Revisited. Am J Public Health. 2004. June 1;94(6):1027–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pan W, Bai H. A Multivariate Approach to a Meta-Analytic Review of the Effectiveness of the D.A.R.E. Program. Int J Environ Res Public Health. 2009. January 13;6(1):267–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Clayton RR, Cattarello AM, Johnstone BM. The Effectiveness of Drug Abuse Resistance Education (Project DARE): 5-Year Follow-Up Results. Prev Med. 1996. May 1;25(3):307–18. [DOI] [PubMed] [Google Scholar]
- 48.Day LE, Miller-Day M, Hecht ML, Fehmie D. Coming to the new DARE: A prelim inary . . test of the officer-taught elementary keepin’it REAL curriculum. Addictive behaviors. 2017. . . .November 1;74:67–73. [DOI] [PubMed] [Google Scholar]