To the Editor:
Routine screenings for cancer were paused beginning in March 2020 as the COVID-19 Pandemic emerged in the United States.1 Previous studies reported 80% to 90% declines in breast, cervical, and colorectal cancer screening volumes in March-April of 2020 before rebounding in the summer of 2021, after clinics resumed routine screening.2 However, the pandemic’s impact on lung cancer screening (LCS) rates nationally or by state is not yet known. This is of interest because lung cancer remains the leading cause of cancer death in the United States, and annual LCS with low-dose CT scanning (LDCT) is recommended for a group that is at a high risk of dying of this disease.3 The objective in the current study was to examine annual LCS rates before (2019) and during (2020) the pandemic nationally and according to state.
Methods
The numbers of LCSs performed in 2019 and 2020 were obtained from the American College of Radiology’s Lung Cancer Screening public reports.4 Facilities are required to enter data on all LDCT for LCS, regardless of payor. The primary outcome was LCS rates among eligible adults defined according US Preventive Services Task Force criteria in 2019-2020: people 55 to 80 years old who currently or formerly smoked cigarettes and quit within the past 15 years, with ≥30 pack-year smoking history.3 LCS rates were computed by dividing the number of LDCTs recorded in the registry during 2019 and 2020 by the number of eligible adults, which was estimated with the most contemporary population-based surveys and census data with a method described elsewhere.5 Briefly, the proportion of eligible adults was computed with 2019 Behavioral Risk Factor Surveillance System data, which were used to estimate state-specific former and current smoking prevalence; National Health Interview Survey data were used to estimate the probability that a person who currently or formerly smoked met United States Preventive Services Task Force eligibility as detailed smoking data (eg, pack-years) are not collected uniformly in Behavioral Risk Factor Surveillance System. The proportion of eligible adults were then multiplied by 2019 US Census Bureau population counts to estimate the number of eligible adults (Table 1 ). Screening rate ratios (SSRs) that compared 2020 vs 2019 LCS rates were computed and corresponding 95% CIs were estimated with bootstrap sampling in SAS-version 9.4. The study analyses used deidentified publicly available data, which is considered nonhuman participants research under the US Department of Health and Human Services’ Office for Human Research Protection and does not require institutional review board review or informed consent.
Table 1.
Lung Cancer Screening Rates in the United States by State, 2019 and 2020a
| Variable | 2019 |
2020 |
|---|---|---|
| % (95% CI) | % (95% CI) | |
| US Total | 6.6 (6.5-7.4) | 6.5 (6.4-7.3) |
| State | ||
| Alabama | 7.1 (7.0-8.3) | 6.3 (6.2-7.4) |
| Alaska | 7.1 (7.0-8.8) | 6.8 (6.7-8.5) |
| Arizona | 2.5 (2.4-2.9) | 2.5 (2.4-2.9) |
| Arkansas | 4.3 (4.3-5.0) | 4.2 (4.1-4.8) |
| California | 1.4 (1.4-1.6) | 1.1 (1.1-1.3) |
| Colorado | 3.6 (3.5-4.2) | 3.7 (3.7-4.3) |
| Connecticut | 8.5 (8.4-9.9) | 8.3 (8.2-9.6) |
| Delaware | 9.9 (9.7-11.8) | 9.8 (9.7-12.0) |
| District of Columbia | …b | 4.4 (4.4-5.6) |
| Florida | 3.7 (3.7-4.3) | 3.5 (3.4-4.1) |
| Georgia | 6.4 (6.4-7.5) | 6.3 (6.2-7.3) |
| Hawaii | 4.4 (4.3-5.1) | 3.3 (3.2-3.8) |
| Idaho | 8.9 (8.8-10.6) | 8.8 (8.6-10.5) |
| Illinois | 7.1 (7.1-8.4) | 7.3 (7.2-8.6) |
| Indiana | 8.2 (8.1-9.4) | 7.9 (7.8-9.1) |
| Iowa | 11.7 (11.5-13.4) | 12.2 (12.0-14.1) |
| Kansas | 9.5 (9.4-10.9) | 9.0 (8.9-10.3) |
| Kentucky | 14.6 (14.5-17.2) | 17.7 (17.4-21.1) |
| Louisiana | 3.3 (3.3-3.9) | 3.8 (3.8-4.5) |
| Maine | 11.0 (10.8-12.6) | 13.9 (13.7-16.1) |
| Maryland | 9.2 (9.1-10.6) | 7.1 (7.0-8.1) |
| Massachusetts | 20.5 (20.3-23.8) | 19.7 (19.5-22.8) |
| Michigan | 10.4 (10.3-12.0) | 9.4 (9.3-10.9) |
| Minnesota | 8.9 (8.8-10.2) | 8.0 (7.9-9.2) |
| Mississippi | 6.1 (6.1-7.2) | 6.7 (6.6-7.9) |
| Missouri | 8.2 (8.1-9.5) | 8.8 (8.7-10.3) |
| Montana | 8.2 (8.1-9.6) | 7.4 (7.3-8.6) |
| Nebraska | 6.2 (6.1-7.1) | 5.8 (5.7-6.6) |
| Nevada | 1.2 (1.2-1.5) | 1.7 (1.7-2.1) |
| New Hampshire | 13.2 (13.1-15.5) | 13.4 (13.3-15.7) |
| New Jersey | 3.5 (3.5-4.4) | 3.3 (3.2-4.1) |
| New Mexico | 1.7 (1.7-2.1) | 1.9 (1.9-2.2) |
| New York | 6.5 (6.5-7.5) | 6.6 (6.5-7.6) |
| North Carolina | 8.9 (8.8-10.5) | 9.4 (9.3-11.0) |
| North Dakota | 12.7 (12.5-14.6) | 13.3 (13.1-15.4) |
| Ohio | 8.0 (7.9-9.2) | 8.3 (8.2-9.5) |
| Oklahoma | 2.0 (2.0-2.3) | 2.1 (2.1-2.4) |
| Oregon | 8.5 (8.5-10.1) | 9.1 (9.0-10.8) |
| Pennsylvania | 9.2 (9.1-10.7) | 9.0 (8.9-10.4) |
| Rhode Island | 12.2 (12.0-14.5) | 7.1 (7.0-8.5) |
| South Carolina | 6.3 (6.2-7.3) | 7.2 (7.1-8.3) |
| South Dakota | 11.0 (10.8-13.5) | 11.2 (11.0-13.7) |
| Tennessee | 7.2 (7.1-8.4) | 7.5 (7.4-8.8) |
| Texas | 2.6 (2.6-3.1) | 2.2 (2.1-2.5) |
| Utah | 4.0 (4.0-4.5) | 1.9 (1.9-2.2) |
| Vermont | 14.8 (14.6-17.6) | 11.2 (11.1-13.3) |
| Virginia | 8.5 (8.4-9.7) | 8.7 (8.6-10.2) |
| Washington | 7.0 (7.0-8.2) | 7.6 (7.5-8.9) |
| West Virginia | 3.6 (3.6-4.3) | 5.0 (5.0-5.9) |
| Wisconsin | 11.9 (11.7-14.1) | 11.6 (11.4-13.8) |
| Wyoming | …b | …b |
The following formulas were used to compute lung cancer screening (LCS) rates and are described elsewhere.5 Population-survey and detailed census data for 2020 have not yet been released, so 2019 data were relied on to compute 2019 and 2020 denominators (ie, eligible population). The numerator (number of low-dose CT scans) were based on 2019 and 2020 Lung Cancer Screening Registry data. The 95% CIs were computed with bootstrap sampling with 1,000 replicates and accounted for the variation in smoking behavior.
Formula 1:
Formula 2: EligiblePops,y = CensusPops,y × ((P(Elig/Currentn,2015) × P(Currents,y) + (P(Elig/Formern,2015) × P(Formers,y))Where: LDCT Scan = number of low-dose CT scans from 2019-2020 LCSR data; EligiblePop = population eligible for low-dose CT scanning; s = state (Alabama…Wyoming); n = national; y = year (2019,2020); 2015 = year 2015; p = probability; CensusPop = number of adults 55 to 80 years old in 2019 US Census data; Elig = eligible from 2015 National Health Interview Survey; Current = current smoker from 2019 Behavioral Risk Factor Surveillance System; Former = former smoker from 2019 Behavioral Risk Factor Surveillance System; 2019 = year 2019; 2020 = year 2020;
Lung cancer screening rates not available. Data on the number of low-dose CT scans were suppressed in lung cancer screening registry reports.
Results
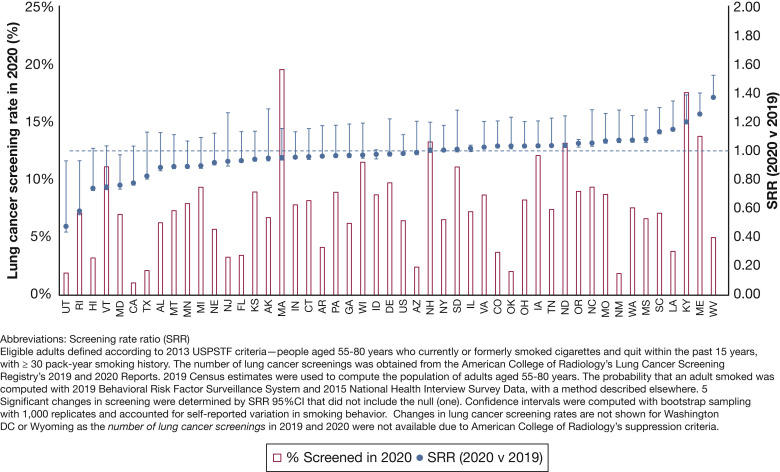
Among 8.51 million eligible adults, 564,164 and 557,795 received LCSs in 2019 and 2020, respectively. National LCS rates were steady between 2019 (6.6%; 95% CI, 6.5-7.4) and 2020 (6.5%; 95% CI, 6.4-7.3; 2020 vs 2019 SRR = 0.99; 95% CI, 0.97-1.01) (Table 1; Fig 1 ) Between 2019 and 2020, SRRs statistically significantly declined by 23% to 52% in five states (Utah, Rhode Island, Vermont, Hawaii, and Maryland; SRRs ranged from 0.77 to 0.48). During the same period, SRRs were unchanged in 25 states and significantly increased in 19 states, by ≥20% (SRRs ≥1.2) in Nevada, West Virginia, Maine, and Kentucky.
Figure 1.
Lung cancer screening rates in 2020 and changes in lung cancer screening rates between 2020 vs 2019 among eligible adults by state. The term “eligible adults” was defined according to 2013 United States Preventive Services Task Force criteria: people who were 55 to 80 years old who currently or formerly smoked cigarettes and quit within the past 15 years, with ≥30 pack-year smoking history. The number of lung cancer screenings was obtained from the American College of Radiology’s Lung Cancer Screening Registry’s 2019 and 2020 Reports. The 2019 Census estimates were used to compute the population of adults who were 55 to 80 years old. The probability that an adult smoked was computed with 2019 Behavioral Risk Factor Surveillance System and 2015 National Health Interview Survey Data, with a method described elsewhere.5 Significant changes in screening were determined by screening rate ratio (95% CI) that did not include the null (one). CIs were computed with bootstrap sampling with 1,000 replicates and accounted for self-reported variation in smoking behavior. Changes in lung cancer screening rates are not shown for Washington DC or Wyoming because the number of lung cancer screenings in 2019 and 2020 were not available due to American College of Radiology’s suppression criteria.
Discussion
In this population-based study, LCS rates remained stable between 2019 and 2020 and just under one in 15 eligible people were screened. The lack of nationwide declines could be due to underutilization of LCS before the pandemic began when only 5% to 6% of adults received screening in 2018,5 which limited the room for further decreases. Rates, however, increased between 2019 and 2020 for 19 states, which suggests that health systems and local and state-level cancer control efforts played a role in improving LCS rates. For example, Kentucky, which has one of the nation’s highest LCS rates, has made concerted efforts to improve LCS rates since 2013.6 There were five states in which LCS rates statistically significantly decreased, including Hawaii and Utah, which had below-average rates before the pandemic began. States’ stay-at-home orders and COVID-19 surges may have influenced short-term screening volumes, although there was not a clear pattern with annual LCS rates. 2 For example, orders were more comprehensive and enduring in the Northeast, but there was a mix of LCS patterns within this region, with annual LCS rates unchanged in New York, which is a state that experienced a substantial surge of COVID-19 infection during the Spring of 2020, but declined in Vermont.7
Limitations include potential under capture of LDCTs in registries and denominators relied on self-reported smoking behavior. Strengths include contemporary national estimates of LCS rates.
In conclusion, although national LCS rates remained low and unchanged, 19 states experienced significant improvements despite the pandemic. Best practices from successful state and local LCS programs could inform ongoing efforts to detect lung cancers early.
Footnotes
FINANCIAL/NONFINANCIAL DISCLOSURES: The authors have reported to CHEST the following: S. A. F., P. B., R. A. S., and A. J. are employed by the American Cancer Society, which receives grants from private and corporate foundations, including foundations associated with companies in the health sector for research outside of the submitted work. The authors are not funded by or key personnel for any of these grants, and their salaries are funded solely through American Cancer Society funds. None declared (G. A. S.).
References
- 1.Mazzone P.J., Gould M.K., Arenberg D.A., et al. Management of lung nodules and lung cancer screening during the COVID-19 pandemic: CHEST expert panel report. Chest. 2020;158(1):406–415. doi: 10.1016/j.chest.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen RC, Haynes K, Du S, Barron J, Katz AJ. Association of Cancer screening deficit in the United States with the COVID-19 pandemic. JAMA Oncol. 2021;7(6):878–884. doi: 10.1001/jamaoncol.2021.0884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moyer V.A., US Preventive Services Task Force Screening for lung cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160(5):330–338. doi: 10.7326/M13-2771. [DOI] [PubMed] [Google Scholar]
- 4.American College of Radiology LCSR Available Reports. 2020. https://nrdrsupport.acr.org/support/solutions/articles/11000039783-lcsr-available-reports?_ga=2.201388568.823086855.1583799862-1358519942.1578412757 Accessed June 1, 2021.
- 5.Fedewa SA, Kazerooni EA, Studts JL, et al. State variation in low-dose CT scanning for lung cancer screening in the United States. J Natl Cancer Inst. 2021;113(8):1044–1052. doi: 10.1093/jnci/djaa170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.University of Kentucky Kentucky LEADS Collaborative. 2020. https://ukmarkey.org/ky-leads-collaborative-led-by-uk-u-of-l/ Accessed February 8, 2021.
- 7.Oster A.M., Kang G.J., Cha A.E., et al. Trends in number and distribution of COVID-19 Hotspot counties - United States, March 8-July 15, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(33):1127–1132. doi: 10.15585/mmwr.mm6933e2. [DOI] [PMC free article] [PubMed] [Google Scholar]