Abstract
This study investigated the role of breast cancer survivors in a computer-mediated social support (CMSS) group for women with breast cancer. Applying a computer-aided content analytic method, the present study examined the differences in support provision between survivors and newly diagnosed patients. This study further investigated the impacts of survivor-provided social support on psychosocial adjustment of newly diagnosed patients. The results revealed that, compared with newly diagnosed patients, breast cancer survivors provided more emotional and informational support. Receiving emotional support from survivors contributed to an improvement in the quality of life and the depression of patients. The effects of survivor-provided informational support were not significant.
Keywords: breast cancer survivor, social support, CMSS groups, psychosocial adjustment
Breast cancer is a global public health problem, with an estimated 1.7 million cases and 521,900 deaths in 2012 (Torre et al., 2015). Moreover, the incidence rate and mortality of breast cancer are rapidly increasing in the less-developed countries of Asia, Latin America, and Africa (Global Burden of Disease Cancer Collaboration, 2015). Although the mortality of breast cancer has decreased in the United States for the past decade due to early diagnosis and advanced treatment, it is still the most frequently diagnosed cancer and leading cause of death for women aged 20 to 59 years in the United States as of 2015 (Siegel, Miller, & Jemal, 2015).
Once diagnosed with breast cancer, patients often find themselves in need of information about treatment, medication, and side effects (Leydon et al., 2000; Rutten, Arora, Bakos, Aziz, & Rowland, 2005; Vogel, Bengel, & Helmes, 2008). They are also confronted with psychological discomforts such as low quality of life, depression, and concerns about treatment (Burgess et al., 2005; Meyerowitz, 1980; Reich, Lesur, & Perdrizet-Chevallier, 2008). Providing adequate social support, therefore, becomes important in buffering breast cancer patients’ stress from the cancer experience, thereby contributing to better psychosocial adjustment (Butler, Koopman, Classen, & Spiegel, 1999; Gremore et al., 2011; Kornblith et al., 2001). In particular, with advances in communication technologies, a growing body of literature has addressed the therapeutic benefits of participating in computer-mediated social support (CMSS) groups: alleviating depressive symptoms (E. Kim et al., 2012; Winzelberg et al., 2003), enhancing quality of life (Lieberman & Goldstein, 2006), increasing information competence (Gustafson et al., 2001; Han et al., 2008), and helping patients to be better-informed about treatment (Høybye, Johansen, & Tjornhoj-Thomsen, 2005; Owen, Klapow, Roth, & Tucker, 2004).
Some studies have suggested that breast cancer survivors can play an important role in providing cancer patients with useful information and emotional support (Falzon, Radel, Cantor, & d’Arripe-Longueville, 2015; Kreuter et al., 2008; Macvean, White, & Sanson-Fisher, 2008; Pérez et al., 2014). After undergoing cancer treatment, survivors can have a better understanding of treatments and related psychological difficulties and often report posttraumatic growth, which may assist them in sharing their experience and knowledge (Campbell, Phaneuf, & Deane, 2004; Frazier et al., 2013). In addition, as cancer patients consider survivors as more trustworthy (Falzon et al., 2015; McQueen & Kreuter, 2010) and similar to them (Pérez et al., 2014; Wood, Taylor, & Lichtman, 1985), survivors’ participation in social support groups may have positive impacts on the psychosocial adjustment of other patients.
However, little is known about how breast cancer survivor’s participation in support groups contributes to the psychological adjustment of other cancer patients. Even the few studies involving the supportive behavior of breast cancer survivors (e.g., Ashbury, Cameron, Mercer, Fitch, & Nielsen, 1998; Gray, Fitch, Davis, & Phillips, 1997; Sutton & Erlen, 2006) have mostly focused on dyadic peer relationships in a face-to-face context. Given the growing popularity of CMSS groups in cancer care (Walther & Boyd, 2002; Wright, 2016), it is important to understand the role of breast cancer survivors in CMSS groups and the impacts of social support provided by survivors in terms of psychological adjustment of other new patients. This study, therefore, will examine what types of social support are provided by breast cancer survivors and how they are different from the social support provided by newly diagnosed patients. The present study will further investigate how the survivors’ support contributes to psychosocial adjustment of newly diagnosed patients. Specifically, to analyze supportive expressions in a CMSS group, this study will adopt a computer-assisted content analysis which combines an inductive approach with a conventional deductive content coding approach.
Peer-to-Peer Support Groups in Breast Cancer Treatment
Social support refers to the emotional (e.g., empathy, reassurance, and encouragement), informational (e.g., advice and direction), or instrumental (e.g., financial and physical) resources provided by one’s social networks that help her or him to cope with stressful events (Cohen, 2004; Gottlieb & Bergen, 2010). In particular, studies have reported the benefits of peer-to-peer social support groups—either supervised by professionals or not—where patients can communicate with other people experiencing the same disease or similar health condition (e.g., Dennis, 2003; Dunn, Steginga, Rosoman, & Millichap, 2003; Ussher, Kirsten, Butow, & Sandoval, 2006). Supportive interaction with peers having common experiences may decrease feelings of isolation and may increase a sense of belonging (Cohen, Underwood, & Gottlieb, 2000; Ussher et al., 2006). Based on a shared identity and perceived similarity among peers, patients in peer support groups tend to perceive information provided by peers as more credible (Petosa & Smith, 2014) and are more likely to engage in empathic communication (Helgeson & Gottlieb, 2000).
In the context of breast cancer treatment, the benefits of participating in peer-to-peer support groups have been well-documented. Women with breast cancer feel more comfortable about sharing their emotions and concerns with those who have been through the same experience (Silverman-Dresner, 1990). Therefore, breast cancer patients have reported peer-to-peer support as beneficial in receiving emotional support such as connecting with other patients, feeling understood, and sharing important information and knowledge (Gray et al., 1997), which in turn contributes to a better quality of life (Ashbury et al., 1998) and lower psychological distress (Silverman-Dresner, 1990).
Over the past two decades, a growing number of studies have investigated the benefits of peer-to-peer support groups in breast cancer treatment in the context of computer-mediated communication. Grounded in the buffering hypothesis (Cohen & Wills, 1985), previous studies have found that social support in CMSS groups could buffer the harmful physiological consequences of stress from breast cancer (Barak, Boniel-Nissim, & Suler, 2008; Rubenstein, 2015). For example, depressive symptoms such as feelings of isolation, hopelessness, anxiety, and a lack of interest were found to be decreased in patients who received emotional support, such as empathy and encouragement, from peers in CMSS groups (Batenburg & Das, 2014; E. Kim et al., 2012; Winzelberg et al., 2003). Consequently, women with breast cancer reported a higher quality of life after participating in CMSS groups (Lieberman & Goldstein, 2006). In addition, information exchange within CMSS groups contributed to an improvement in information competence (Gustafson et al., 2001; Han et al., 2008) and knowledge of breast cancer and its treatment among patients (Høybye et al., 2005; Owen et al., 2004), thereby helping patients feel more in control.
The Potential of Survivors as Support Providers
Cancer survivors refer to women who have been diagnosed with cancer, who have finished a set of treatment procedure (e.g., surgery, radiation therapy, chemotherapy), and who are alive without a recurrence (Howard-Anderson, Ganz, Bower, & Stanton, 2012; Vivar & McQueen, 2005). As a former patient who has undergone the process from diagnosis to survivorship, breast cancer survivors may have a greater potential to be support providers because they have a better understanding of treatments and show better psychological adjustment after primary treatment. Campbell et al. (2004), for example, claimed that “those who have survived the disease have an understanding and first-hand experience of the disease and its treatment that facilitates shared experiences” (p. 4). In a similar vein, Meyer, Coroiu, and Korner (2015) pointed out that cancer survivors can be ideal support providers because they have “authentic knowledge of what it is like to live with cancer, and as such, they are able to bring a unique perspective to the support process” (p. 300). Moreover, cancer survivors generally present better physical functioning and emotional well-being than newly diagnosed patients (Baker, Denniston, Haffer, & Liberatos, 2009). Survivors, therefore, may possess more resources to provide informational and emotional support to other patients (Cameron, Ashbury, & Iverson, 1997; Gray et al., 1997). Consequently, as more experienced members, breast cancer survivors can take a leading role in social support groups by providing information and their experiences of coping (Meier, Lyons, Frydman, Forlenza, & Rimer, 2007).
Another important mechanism that assists survivors in sharing information and providing emotional support is posttraumatic growth. Coined by Calhoun and Tedeschi (1990), this concept refers to positive cognitive changes, such as the reframing of life goals, appreciation of life, and increased spirituality, as a result of struggling with a traumatic event. Many breast cancer survivors have reported posttraumatic growth such as a better sense of connectedness with others, deepened spirituality, and reappraising life’s meaning in the aftermath of breast cancer treatment (Bellizzi & Blank, 2006; Cordova, Cunningham, Carlson, & Andrykowski, 2001; Manne et al., 2004; Weiss, 2004). As Staub and Vollhardt (2008) noted, such psychological growth leads people to have a greater awareness of others’ suffering; increased perspective-taking, empathy, and sympathy; and a greater sense of responsibility for others’ welfare, which can prompt people to be engaged in altruistic behavior, such as helping others and providing support. Supporting this, some studies have found the relationship between posttraumatic growth of breast cancer survivors and their prosocial behavior such as helping others in need and providing emotional support (Frazier et al., 2013; Hannah & Midlarsky, 2005).
In contrast to survivors, newly diagnosed breast cancer patients experience greater physical, emotional, and social distress resulting from a diagnosis of breast cancer and its ensuing treatments (Hanson Frost et al., 2000; Tighe, Molassiotis, Morris, & Richardson, 2011). In addition, because of the uncertainty of their treatment and fear of death, women who are newly diagnosed with breast cancer need more emotional support to manage their psychological distress such as common feelings of sadness and vulnerability to depression, anxiety, and social isolation (Vivar & McQueen, 2005); moreover, they have greater needs for treatment-related information (Rutten et al., 2005). Previous research on newly diagnosed breast cancer patients has found high levels of unmet needs across a range of support domains, including psychological and physical/daily living and informational support (Griesser et al., 2011; Harrison, Young, Price, Butow, & Solomon, 2009; Sanson-Fisher et al., 2000). Newly diagnosed breast cancer patients, therefore, tend to receive support from others (Davis, Williams, Parle, Redman, & Turner, 2004).
Given these differences in the psychosocial status between survivors and newly diagnosed patients in their potential to be support providers, this study predicts that survivors will provide more emotional support (H1a) and more informational support (H1b) than newly diagnosed patients.
Effects of Social Support Provided by Survivors
Some studies have provided anecdotal evidence showing that new patients could benefit more from survivors. For example, studies from the Reach to Recovery program (see, for a detailed description, Rinehart, 1994), which offered matched one-to-one peer support between newly diagnosed cancer patients and survivors, reported that the quality of life of newly diagnosed patients had improved as a result of the supportive communication with their survivor partners (Ashbury et al., 1998; Cameron et al., 1997). Similarly, in a study of a peer-to-peer support program for breast cancer patients, it was found that newly diagnosed patients (i.e., “sojourners”) perceived their survivor peers (i.e., “navigators”) as being informative and empowering, thus contributing to the psychological improvement of new patients, such as enhancing their emotional well-being and self-efficacy (Giese-Davis et al., 2006).
Although it has not been clearly explained why newly diagnosed patients benefit from emotional and informational support provided by survivors in the literature, social comparison may affect the outcomes of interactions between new patients and survivors. Grounded in social comparison theory (Festinger, 1954), Taylor and Lobel (1989) proposed that people use either upward or downward comparison to cope with stressful events. Upward comparison includes seeking affiliation with and information from those who are in a better condition, whereas downward comparison refers to self-evaluation against others in a worse situation (Taylor & Lobel, 1989). Buunk, Collins, Taylor, VanYperen, and Dakof (1990) later distinguished positive upward comparison, in which individuals become optimistic to see others in a better situation (i.e., upward identification), from negative upward comparison by which people become pessimistic to see others in a better situation (i.e., upward contrast).
In the context of cancer care, a few studies have shown that (positive) upward comparison is related to the self-improvement of cancer patients, such as developing coping strategies, finding hope, and learning useful information (Taylor & Lobel, 1989). Furthermore, women with breast cancer tend to have a greater desire for upward comparison, thereby seeking information and emotional support from better-adjusted patients versus poorly adjusted patients (Stanton et al., 1999). Although the previous literature on social comparison in cancer care has not specified the role of cancer survivors, given a better understanding of cancer treatment and psychological adjustment of survivors (Baker et al., 2009; Meyer et al., 2015), positive upward comparison may occur when newly diagnosed patients receive social support from survivors, which in turn contributes to the psychological adjustment of new patients.
As discussed above, receiving social support within CMSS groups could contribute to improvements in the psychosocial status of patients, receiving emotional support was related to fewer depressive symptoms (Batenburg & Das, 2014; E. Kim et al., 2012; Winzelberg et al., 2003) and a greater quality of life (Lieberman & Goldstein, 2006), and receiving informational support contributed to information competence (Gustafson et al., 2001; Han et al., 2008) and cancer knowledge (Høybye et al., 2005; Owen et al., 2004). However, based on a discussion on the potential impact of survivor-provided social support over that of social support provided by newly diagnosed patients, this study predicts that survivor-provided social support will be more strongly related to improving psychosocial status of newly diagnosed patients than social support provided by newly diagnosed patients. Specifically, the present study hypothesizes that survivor-provided emotional support will be more strongly related to improving quality of life (H2a) and reducing depression (H2b) than new patient–provided emotional support; survivor-provided informational support will be more strongly related to improving of cancer information competence (H3a) and cancer knowledge (H3b) than new patient–provided informational support.
Method
Sample
The sample of this study is collected from the Comprehensive Health Enhancement Support System (CHESS) intervention study which investigated the effects of online-based support system for women with breast cancer. From April 2004 to April 2006, a total of 661 newly diagnosed breast cancer patients were recruited from three cancer institutions in Connecticut, Texas, and Wisconsin. They were within 2 months of diagnosis and were literate in English. Doctors and nurses provided brief information about this study to potential and eligible patients. If the patients agreed to participate, research staffs contacted them to explain the purpose and procedures of the study in detail. Participants were provided a laptop to use during the 6 months of intervention, or they were allowed to use their own computers. All computers were equipped with a CHESS browser, which was installed to record the action log data of system use that tracked every click and keystroke made by the participants. The study also supported Internet access fees up to US$30.00/month for the 6 months of the study intervention when it was requested.
These newly diagnosed breast cancer patients were randomly assigned to one of six experimental conditions: (1) Internet only (n = 112), (2) CHESS information service only (n = 118), (3) CHESS information and communication services only (n = 109), (4) full CHESS (n = 111), (5) mentor only (n = 106), and (6) mentor and full CHESS (n = 105). The CHESS system consists of information services (e.g., treatments, medications, and medical system information), collaboration services (e.g., action plans and easing distress), and communication services (e.g., discussion group and ask-an-expert services). Among these, the discussion group is a CMSS group with an asynchronous bulletin board on which patients can share experiences and provide informational or emotional support.
As the present research aims to investigate the impact of participating in CMSS, only 236 participants, who could access the discussion group (i.e., Conditions 3, 4, and 6), visited the discussion group at least twice during their 6 months of intervention, and those who finished both the pretest and posttest were selected for the analysis. The sample consists of 76 participants from the CHESS information and communication services only group, 81 from the full CHESS group (n = 81), and 79 from the mentor and full CHESS group. The newly diagnosed patients in this study had a mean age of 51 years, and more than half of them reported having at least a bachelor’s degree (4-year college). Regarding race, the sample included 90.1% Caucasian and 9.9% minority women. Only 29 newly diagnosed patients reported that they lived alone (12.3%), whereas the majority lived with family or friends (n = 204, 86.4%). Detailed characteristics of the patients are presented in Table 1. Among the 236 study participants, 76 patients belonged to information and communication services group, whereas 160 participants were either the full CHESS or the mentor and full CHESS conditions.
Table 1.
Sample Characteristics.
| n | % | |
|---|---|---|
| Race | ||
| Caucasian | 210 | 88.98 |
| Minority | 23 | 9.75 |
| NA | 3 | 1.30 |
| Education | ||
| Some junior high | 2 | 0.85 |
| Some high school | 4 | 1.69 |
| High school degree | 36 | 15.25 |
| Some college courses | 39 | 16.53 |
| Associate degree | 21 | 8.90 |
| Bachelor’s degree | 62 | 26.27 |
| Some graduate courses | 18 | 7.63 |
| Graduate degree | 51 | 21.61 |
| NA | 2 | 0.85 |
| Annual household income | ||
| less than US$20,000 | 12 | 5.08 |
| US$20,001–US$40,000 | 31 | 13.14 |
| US$40,001–US$60,000 | 38 | 16.10 |
| US$60,001–US$80,000 | 37 | 15.68 |
| US$80,001–US$100,000 | 43 | 18.22 |
| more than US$100,000 | 56 | 23.73 |
| NA | 19 | 8.05 |
| Living alone | ||
| No | 204 | 86.44 |
| Yes | 29 | 12.29 |
| NA | 3 | 1.27 |
Note. NA = not applicable.
Prior research from the CHESS has provided a vast amount of empirical evidence on the therapeutic benefits of social support within breast cancer CMSS groups: positive reframing (Han et al., 2008), increased self-efficacy (Namkoong et al., 2010), enhanced emotional well-being (J. Kim, Han, Shaw, McTavish, & Gustafson, 2010), and greater information competence (Gustafson et al., 2001). However, previous studies from the CHESS have paid less attention to the role of breast cancer survivors in CMSS groups, and thus could not distinguish survivor-provided social support from social support provided by new patients. As an initial study to examine the role of breast cancer survivors in a CMSS group, this study allowed a total of 56 breast cancer survivors, who had participated in earlier CHESS studies, to participate in the discussion group as volunteers. The researchers investigated how these survivors provided social support to other newly diagnosed patients. The survivors in this study had been diagnosed with breast cancer, had experienced a set of primary treatments, and were alive without any sign of recurrence.
Between April 1, 2005, and May 31, 2007, 18,263 messages were posted in the discussion group. Of these, a total of 7,841 (42.9%) messages were posted by new patients, whereas 8,986 (49.2%) messages were written by survivors.
Data Construction
The data in the analysis consist of data from a survey (pretest and posttest), outcomes of computer-assisted content coding, usage log data, and message database files. The study participants (i.e., newly diagnosed patients) were asked to complete the pretest before they participated in the CHESS system and the posttest after 6 months of intervention. Information regarding the demographics, psychological status, and health condition of the participants was obtained from the pretest and posttest surveys. To analyze the content of expressions in the discussion group, this study conducted a systematic computer-aided content analysis using the InfoTrend system. The outcomes from the content coding were combined with the action log data and message database files, which allows the researchers to identify which messages were retrieved (i.e., clicked message page and stayed at least 1 s on the page) and written by each participant. The log data recorded users’ activities in the discussion group, including what messages were requested by which users and when each request happened. The message database recorded the posted messages, the user ID of the posters, and when the messages were posted.
A Systematic Computer-Assisted Content Analysis
In particular, this study conducted a systematic computer-assisted content analysis using the InfoTrend system. The major obstacles to describing and analyzing the expressions from CMSS groups were the massive amounts of information, difficulties in interpreting the contextual meanings in content, and the nonstandard nature of the language used (e.g., typos, slangs, abbreviations). The InfoTrend system (Fan, 1990, 1994) is a computer software program for advanced content analyses, which allows users to more precisely capture the semantic properties of content by applying dynamic rules. Specifically, using the dynamic rule structure, researchers can capture the complex meaning of expressions composed of multiple concepts and ideas.
The content-coding procedure in this analysis combined a conventional deductive processing, where prespecified analytic frameworks were examined by applying a pre-established dictionary to the content, with an inductive process that could be more inclusive to new patterns of expressions and could enable a more comprehensive description of expressions. In the deductive process, this study first defined emotional support and informational support and identified the main categories for them based on the previous literature (e.g., Braithwaite, Waldron, & Finn, 1999; Coulson, Buchanan, & Aubeeluck, 2007; Cutrona & Suhr, 1994). Emotional support was defined as a type of social support that contributes tofeelings of being cared for and loved, which consists of four subcategories: (a) empathy/sympathy, (b) encouragement/reassurance, (c) care/physical affection, and (d) universality/relationship. Similarly, informational support was defined as a type of support that provides information and advice regarding the following eight subjects: (a) secondary treatment, (b) side effects, (c) surgery, (d) diagnostic/symptoms, (e) psychosocial aspects, (f) general breast cancer information, (g) other information, and (h) health system navigation. From the prior literature (e.g., Alpers et al., 2005; Braithwaite et al., 1999; Coulson et al., 2007; Cutrona & Suhr, 1994; Tausczik & Pennebaker, 2010), keywords relevant to each emotional and informational support category were selected. Table 2 presents the selected examples of expressions for each category.
Table 2.
Examples of Keywords of Emotional and Informational Support Expressions.
| Category | Examples |
|---|---|
| Emotional support | |
| Empathy/sympathy | sorry (to hear that), afraid (that you), empathy, sympathy, understand, worry, concern, etc. |
| Encouragement/reassurance | hope, wish, trust, congratulation, cheer, hang in there, stay strong, keep marching, keep your heads up, don’t give up etc. |
| Care/physical affection | take care, hugs, kisses, love, with love, etc. |
| Universality/relationship | (I’m or we are) here for you, same boat, common, army of CHESSling, sisterhood, not alone, together, buddy, friend(s), etc. |
| Informational support | |
| Secondary treatment | chemo, hormone replacement, radiation, external beam, Anastrozole, Tamoxifen, Fulvestrant, Taxotere, etc. |
| Side effects | pain, sore, vomit, nausea, acid reflux, bloating, bone pain, excessive bleeding, heart burn, rupture, etc. |
| Surgical information | dissection, anesthesia, mastectomy, lumpectomy, lymphadenectomy, etc. |
| Diagnostic/symptoms | biopsy, bone scan, mammogram, MRI, lymph, tumor, etc. |
| Psychosocial | antidepress, Celexa, Elavil, Luvox, wig, overweight, hair, plastic surgeon, etc. |
| General breast cancer information | brac1, brac2, endoscopy, estrogen, gland, injection, oncology, stage, etc. |
| Health system navigation | insurance, Medicare, GHC, UnitedHealth, medical bill, etc. |
| Other information | about CHESS, resource directory, resource guide, etc. |
Note. CHESS = Comprehensive Health Enhancement Support System; MRI = magnetic resonance imaging; GHC = Group Health Cooperative.
The inductive process was conducted following a deductive process. This process consisted of five steps, including (a) a keyword search, (b) a grounded examination, (c) natural language processing, (d) rule creation, and (e) rule testing. InfoTrend generated a data set containing specific keywords or concepts that were suggested by previous studies (keyword search), and the data was examined in an inductive manner to understand the usage patterns of keywords in context (grounded examination). The next step (natural language processing) included lemmatizing and extraction: The former denotes the process in which variations of words in different tenses or forms (e.g., went, goes, going, and gone) are integrated into their original forms (e.g., go); the latter refers to the process by which a target word (e.g., hear) is distinguished from other words that may have the same alphabet characters, yet have different meanings (e.g., sphere, rehearsal). Based on the sentence-level analysis, coding rules were then created by formulating a relationship between terms, phrases, or concepts (rule creation). For example, this study captured providing empathetic support, such as “I am sorry for your loss” by combining two meaning categories (e.g., “emotional expression: sorry” and “reasons for emotion: others’ grief”), thereby distinguishing empathy from general apologies, such as “I am sorry for my absence” or “Sorry for the late response.”
Once the rules were established, they were tested on a random selection of data to assess their performance in capturing the intended concept (rule testing). To reach a high level of precision and consistency of rules and content analysis, the rules were tested repeatedly by applying them to new message posts. After achieving a high level of consistency in the rules, this study conducted a reliability test between human- and computer-coding results of a randomly selected set of 200 discussion posts in a breast cancer discussion group. The results generated an estimate of 91.0% agreement across the four emotional support expression categories (empathy: 90.9%; encouragement: 88.4%; care: 92.0%; universality: 95.0%), and 85.4% agreement across the eight subcategories of informational support (surgical: 91.8%; side effects: 75.2%; adjuvant treatment/pharmaceutical: 91.5%; diagnostic/symptoms; 85.7%; general breast cancer information: 75.9%; health system navigation: 100.0%; psychosocial information: 80.0%; other information: 73.3%). Krippendorff’s alpha was also calculated to assess agreement between the human coder and the computer on each of the categories. The results indicated that the coding schemes for emotional support (Krippendorff’s α = .80) and informational support (Krippendorff’s α = .70) were reliable (Hayes & Krippendorff, 2007).
Measures
Independent variables.
Receiving emotional support was measured by counting the total number of messages containing emotional support expressions that were retrieved by each newly diagnosed patient. Two different measures were separately calculated, according to the message posters: receiving survivor-provided emotional support (M = 100.90, SD = 241.27) and receiving new patient–provided emotional support (M = 246.65, SD = 481.87).
Receiving informational support was calculated by counting the total number of messages containing informational support that were requested by each newly diagnosed patient. After identifying the message posters, receiving survivor-provided informational support (M = 72.08, SD = 162.93) and receiving new patient–provided informational support (M = 247.88, SD = 241.27) were calculated separately for each new patient.
Dependent variables.
The primary dependent variables for H1a and H1b were providing emotional support and providing informational support. Providing emotional support by newly diagnosed patients was calculated by averaging the number of expressions that included any of the four types of emotional support in the messages posted by newly diagnosed patients (M = 1.23, SD = 1.82). In the same manner, providing emotional support by survivors was also calculated separately (M = 2.87, SD = 2.32). Similarly, providing informational support was measured by calculating the average of the number of expressions, including any of the eight types of informational support within the messages posted by newly diagnosed patients (i.e., providing informational support by newly diagnosed patients, M = 1.83, SD = 2.17) and survivors (i.e., providing informational support by survivors, M = 3.16, SD = 2.16), respectively.
The primary outcomes of H2a, H2b, H3a, and H3b included gain scores (i.e., improvement) in psychosocial conditions, such as the quality of life, depression, cancer information competence, and breast cancer knowledge, respectively. As this study focused on the impact of support provided by survivors and newly diagnosed patients on improvements in the psychological status of patients, each outcome variable was constructed by calculating the differences between the pretest and posttest scores. Quality of life was measured by the abbreviated version of the World Health Organization Quality of Life (WHOQOL-BREF) instrument, which consists of 26 items to measure physical health, psychological health, the environment, and social relationships of individuals (pretest α = .91, posttest α = .93). The difference in the quality of life between pretest and posttest was used in the analysis (M = 0.05, SD = 0.44). To assess current levels of depressive symptomatology, a short eight-item Center for Epidemiologic Studies Depression (CES-D) scale (Radloff, 1977) was used (pretest α = .88, posttest α = .86). A gain score between the pre- and posttest was used as the outcome depression variable (M = −0.37, SD = 0.68). The measure for cancer information competence consisted of five items (5 points), assessing the participant’s comfort level in dealing with cancer information (pretest α = .81, posttest α = .83). Similar to the other outcome variables, a gain score between the posttest and pretest was used as the outcome cancer information competence variable (M = 0.27, SD = 0.75). Breast cancer knowledge was measured with a six-item measure (5 points) that evaluated the level of understanding of breast cancer and treatment (pretest α = .88, posttest α = .90). The difference between posttest and pretest was used as the final primary outcome of this study (M = 0.54, SD = 0.76).
Control Variables
To examine the contribution of receiving social support from survivors and other new patients with respect to the psychological adjustment of new patients, the present study controlled for demographics (e.g., age, race, education level, annual household income), living condition (living alone or not), and study condition (access to the full CHESS or not). In addition, the total volume of messages posted by each patient (M = 21.46, SD = 54.54) and the total volume of messages read by each patient (M = 466.23, SD = 934.67) were also included in the control variables to rule out potential confounding effects of overall reading and posting messages. Table 3 presents descriptive statistics for the variables in the analyses.
Table 3.
Description of Variables.
| n | M | SD | Minimum | Maximum | |
|---|---|---|---|---|---|
| Age | 234 | 51.18 | 9.05 | 26 | 78 |
| Education | 235 | 5.52 | 1.84 | 1 | 8 |
| Income | 217 | 4.09 | 1.57 | 1 | 6 |
| Total volume of writing | 236 | 21.46 | 54.54 | 0 | 426 |
| Total volume of reading | 236 | 466.23 | 934.67 | 0 | 7,121 |
| Receiving emotional support | |||||
| From newly diagnosed patients | 236 | 241.43 | 478.04 | 0 | 3,237 |
| From survivors | 236 | 73.11 | 210.12 | 0 | 1,590 |
| Receiving informational support | |||||
| From newly diagnosed patients | 236 | 242.63 | 478.49 | 0 | 3,091 |
| From survivors | 236 | 52.23 | 142.28 | 0 | 1,135 |
| Δ Quality of lifea | 202 | 0.05 | 0.44 | − 0.96 | 1.50 |
| Δ CES-Da | 201 | − 0.37 | 0.68 | − 2.50 | 2.25 |
| Δ Cancer information competencea | 202 | 0.27 | 0.75 | − 2.00 | 2.20 |
| Δ Cancer knowledgea | 194 | 0.54 | 0.76 | − 2.00 | 2.88 |
Note. CES-D = Center for Epidemiologic Studies Depression scale.
Values represent differences between the posttest and pretest.
Analysis
To test H1a and H1b, this study first conducted a t test comparing the differences in providing supportive messages between survivors and newly diagnosed patients (Analysis 1). The present study further tested H2a, H2b, H3a, and H3b by using ordinary least squares (OLS) regression (Analysis 2). For OLS regression, this study entered control variables in the first block. The main predictors such as receiving emotional support which was provided by survivors and newly diagnosed patients, respectively, were included in the second block for the models to test H2a (Model 1) and H2b (Model 2). Similarly, receiving of informational support provided by survivors and newly diagnosed patients were included in the second block to test H3a (Model 3) and H3b (Model 4). The statistical significance of the models was validated by an F test for an ANOVA at the 95% confidence level.
To evaluate the H2a, H2b, H3a, and H3b more precisely, this study further tested whether standardized beta coefficients of survivor-provided support were statistically larger than those of social support provided by new patients based on Cumming’s (2009) approach of statistical inference from confidence intervals. For this purpose, the corresponding 95% confidence intervals for the standardized beta coefficients of main predictors (i.e., receiving emotional and informational support provided by survivors and new patients) were estimated via bias-corrected bootstrapping (1,000 resamples) for each model, and then the overlaps between confidence intervals were calculated. The beta coefficients were considered statistically significantly different from each other if the overlaps between confidence intervals were smaller than 80% (one-tailed, p < .05; Cumming, 2009).
Results
Differences in Providing Social Support Between Survivors and New Patients
To test the differences in supportive behavior between survivors and newly diagnosed patients, t tests were conducted. H1a predicted that survivors would provide more emotional support than newly diagnosed patients. Confirming this, the average amount of emotional support expressions in the messages posted by breast cancer survivors was significantly greater than that in the messages written by newly diagnosed patients (t = 6.23, df = 62.15, p < .001). The difference in providing emotional support between survivors and newly diagnosed patients was found to be significant across all four subcategories of emotional support (see Table 4): empathy/sympathy (t = 3.63, df = 56.23, p < .001), encouragement/reassurance (t = 5.25, df = 63.35, p < .001), care/physical affection (t = 4.48, df = 63.86, p < .001), and universality/relationship (t = 3.74, df = 56.73, p < .001).
Table 4.
Differences in Providing Informational and Emotional Support Between Newly Diagnosed Patients and Survivors.
| Newly diagnosed patients (n = 236) | Survivors (n = 56) | ||
|---|---|---|---|
| M (SD) | M (SD) | t (df) | |
| Emotional support | 0.40 (0.55) | 1.31 (1.06) | 6.23*** (62.15)a |
| Empathy/sympathy | 0.02 (0.04) | 0.12 (.20) | 3.63*** (56.23)a |
| Encouragement/reassurance | 0.16 (0.27) | 0.52 (0.49) | 5.25*** (63.35)a |
| Care/physical affection | 0.19 (0.32) | 0.54 (0.56) | 4.48*** (63.86)a |
| Universality/relationship | 0.02 (0.06) | 0.13 (0.22) | 3.74*** (56.73)a |
| Informational expression | 1.42 (1.91) | 2.19 (2.40) | 2.57** (290) |
| Secondary treatment | 0.60 (0.87) | 0.89 (1.20) | 2.06* (290) |
| Side effects | 0.19 (0.35) | 0.44 (0.54) | 3.32*** (66.61)a |
| Surgical information | 0.24 (0.46) | 0.27 (0.36) | 0.44 (290) |
| Diagnostic/symptoms | 0.16 (0.33) | 0.33 (0.58) | 2.10*** (63.54)a |
| Psychosocial | 0.10 (0.26) | 0.08 (0.13) | 0.60 (290) |
| Breast cancer | 0.07 (0.16) | 0.10 (0.21) | 1.15 (290) |
| Health system navigation | 0.03 (0.11) | 0.04 (0.15) | 0.76 (290) |
| Other information | 0.05 (0.11) | 0.06 (0.10) | 0.71 (290) |
Equal variances are not assumed because Levene’s test for equality of variances was statistically significant.
p < .05.
p < .01.
p < .001 (all p values are one-tailed).
As H1b predicted, breast cancer survivors provided more informational support than newly diagnosed patients (t = 2.57, df = 290, p < .01). Specifically, as Table 4 presents, this difference was driven by differences in providing information about secondary treatment (t = 2.06, df = 290, p < .05), side effects (t = 3.32, df = 66.61, p < .001), and diagnostic/symptoms (t = 2.10, df = 63.54, p < .001). However, there were no significant differences found in providing informational support between survivors and newly diagnosed patients regarding information on surgery, psychosocial problems, general breast cancer, health system navigation, and other information.
Effects of Receiving Social Support
H2a predicted that the impact of survivor-provided emotional support on the improvement of the quality of life would be stronger than that of emotional support provided by new patients. Table 5 presents a summary of the OLS regression model (Model 1) for H2a. The results showed that, after controlling for age, gender, education, study conditions, the total volume of messages posted, and the total volume of messages read, only receiving survivor-provided emotional support was positively related to an improvement in the quality of life (b = .01, SE = .00, β = .25, p < .05). However, the relationship between receiving emotional support provided by other new patients and an improvement in the quality of life was not statistically significant (b = .00, SE = .00, β = .10, p = .96). The result of the F test indicated that the final model was statistically significant, explaining 11.8% of the variance in an improvement in the quality of life, R2 = .118, F(10, 175) = 2.40, p < .05. Although it was relatively small in magnitude, including predictors (i.e., receiving of emotional support from survivors and other new patients) improved the model fit significantly, ΔR2 = .04, ΔF(2, 175) = 3.61, p < .05.
Table 5.
Summary of Hierarchical Regression Analysis for Variables Predicting Changes in Quality of Life and Depression.
| Model 1: Quality of life change (n = 186) | Model 2: CES-D change (n = 186) | |||||
|---|---|---|---|---|---|---|
| B | SE | β | B | SE | β | |
| Block 1: Control variables | ||||||
| Age | .00 | .00 | −.06 | .01 | .01 | .11 |
| Race (minority = 1) | .13 | .13 | .07 | .12 | .21 | .04 |
| Education | − .03 | .02 | − .12 | .01 | .03 | .03 |
| Income | − .03 | .02 | − .10 | .02 | .04 | .04 |
| Living alonga | − .08 | .10 | − .06 | .05 | .16 | .02 |
| Study conditionb | − .04 | .04 | − .08 | .04 | .06 | .04 |
| Total volume of writingc | − .08** | .04 | − .29** | .08 | .06 | .17 |
| Total volume of readingc | .04 | .02 | .21 | − .03 | .03 | − .11 |
| Δ R2 (F change) | .08 (1.96) | .04 (0.08) | ||||
| Block 2: Receiving ES | ||||||
| From new patientsc | .00 | .00 | .01 | .00 | .00 | .01 |
| From survivorsc | .01* | .00 | .24* | − .00*** | 0 | − .32*** |
| Δ R2 (F change) | .04* (3.61) | .07** (6.47) | ||||
| Total R2 (F) | .118* (2.34) | .102* (1.99) | ||||
Note. CES-D = Center for Epidemiologic Studies Depression scale; ES = emotional support; CHESS = Comprehensive Health Enhancement Support System.
Living alone is coded as (0) no and (1) yes.
Study condition is coded as (0) CHESS information and communication services only group and (1) full CHESS and mentor group and full CHESS group.
Values were log transformed.
p < .05.
p < .01.
p < .001.
To test H2a more precisely, this study tested whether the standardized beta of survivor-provided emotional support was significantly larger than that of new patient–provided emotional support. For this purpose, the corresponding 95% confidence intervals of standardized coefficients of main predictors were first estimated via bias-corrected bootstrapping (1,000 resamples). As illustrated in Figure 1, half of the 80% (one-tailed) of the overlapping confidence intervals was calculated (.158) and added to the lower bound estimate of the standardized beta weight for the survivor-provided emotional support (.050), which yielded .208. As the upper bound estimate of emotional support provided by new patients (.205) did not exceed .208, the standardized coefficient of survivor-provided emotional support (.245) was considered statistically significantly larger than that of emotional support provided by new patients (.006; one-tailed, p < .05), thereby supporting H2a. This result indicates that receiving emotional support provided by survivor was more strongly related to improving patients’ quality of life than receiving emotional support provided by other newly diagnosed patients.
Figure 1.
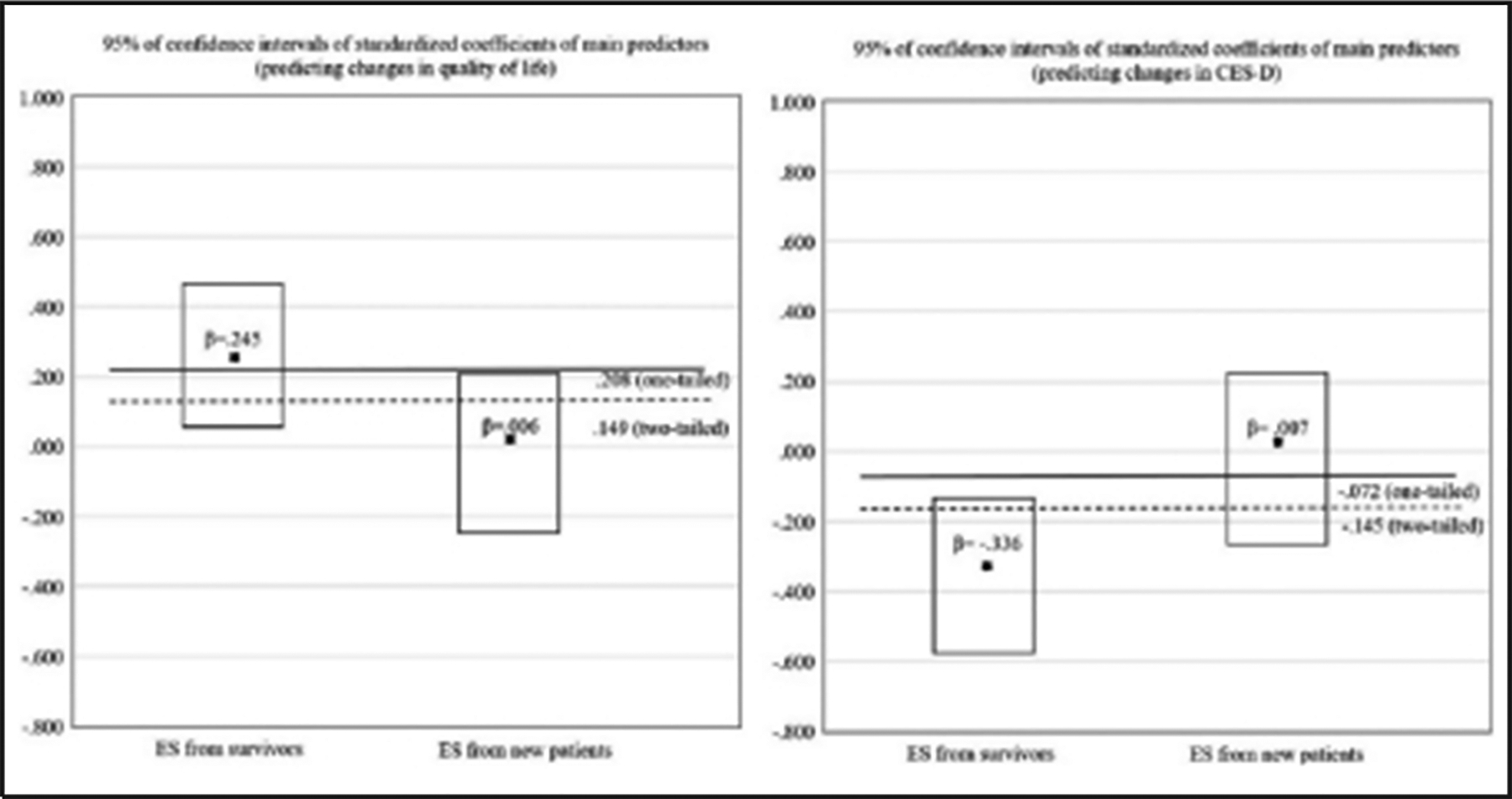
Plots for 95% confidence intervals of the standardized coefficients of the main predictors: Receiving ES.
Note. ES = emotional support; CES-D = Center for Epidemiologic Studies Depression scale.
H2b predicted that emotional support provided by survivors would be more strongly associated with the reduction of depression. As Table 5 shows (Model 2), receiving survivor-provided emotional support was positively related to a reduction in the level of depression (b = −.00, SE = .00, β = −.32, p < .001). However, there was not a significant relationship between receiving emotional support provided by other new patients and the reduction of depression. The final model (Model 2) was found to be statistically significant, explaining 10.2% of the variance in the reduction in newly diagnosed patients’ depression, R2 = .102, F(10, 175) = 1.99, p < .05. In addition, the inclusion of the predictors (i.e., receiving of emotional support from survivors and other new patients) improved the model fit significantly, ΔR2 = .07, ΔF(2, 127) = 6.47, p < .01.
As can be seen in Figure 1, the standardized coefficient of survivor-provided emotional support (−.322) was statistically significantly smaller (i.e., a larger negative association) than that of emotional support provided by new patients (.007) because the upper bound estimate of beta weight of survivor-provided emotional support (−.108) did not exceed −.072, the 80% overlap threshold (one-tailed, p < .05). H2b therefore was supported, suggesting that receiving survivor-provided emotional support contributed to a greater amount of reduction in depressive symptoms among patients than did receiving emotional support from the other newly diagnosed patients.
H3a predicted that the impact of survivor-provided informational support on improving cancer information competence would be stronger than that of informational support provided by new patients. As shown in Table 6, receiving of survivor-provided informational support was not significantly related to improving cancer information competence (b = .00, SE = .00, β = .17, p = .08), whereas receiving informational support offered by other newly diagnosed patients was found to have a positive relationship with improved cancer information competence (b = .00, SE = .00, β = .26, p < .05). In contrast to H3b, only informational support provided by new patients was positively related to increased cancer information competence of patients. Therefore, H3a was rejected. It was found that the final model (Model 3) was statistically significant, explaining 11.1% of the variance in improved cancer information competence among patients, R2 = .111, F(10, 175) = 2.19, p < .05. Although the magnitude was small, the contribution of including informational support receptions to this model was found to be significant, ΔR2 = .06, ΔF(2, 175) = 6.10, p < .01. As Table 7 and Figure 2 show, the difference in magnitude of the standardized betas of main predictors was found to be not statistically significant (p < .05, one-tailed) because the upper bound estimate of the beta coefficient of the survivor-provided informational support (.445) exceeded the threshold of an 80% overlap (.247).
Table 6.
Summary of Hierarchical Regression Analysis for Variables Predicting Changes in Cancer Information Competence and Cancer Knowledge.
| Model 3: Cancer information competence change (n = 186) | Model 4: Breast cancer knowledge change (n = 181) | |||||
|---|---|---|---|---|---|---|
| B | SE | β | B | SE | β | |
| Block 1: Control variables | ||||||
| Age | .00 | .01 | − .05 | − .01 | .01 | − .13 |
| Race (minority = 1) | .03 | .23 | .01 | − .14 | .22 | − .05 |
| Education | − .05 | .03 | − .11 | .04 | .03 | .10 |
| Income | − .04 | .04 | − .08 | − .01 | .04 | − .02 |
| Living alonea | − .37* | .17 | − .16* | .24 | .18 | .10 |
| Study conditionb | − .05 | .07 | − .05 | − .04 | .07 | − .04 |
| Total volume of writingc | − .08 | .06 | − .16 | − .07 | .06 | − .14 |
| Total volume of readingc | − .03 | .04 | − .11 | − .05 | .04 | .16 |
| Δ R2 (F change) | .05 (1.15) | .08† (1.81) | ||||
| Block 2: Receiving IS | ||||||
| From new patientsc | .00* | .00 | .26* | .00 | .00 | .21 |
| From survivorsc | .00 | .00 | .17 | .00 | .00 | − .11 |
| Δ R2 (F change) | .06** (6.10) | .02 (1.54) | ||||
| Total R2 (F) | .111* (2.19) | .09† (1.76) | ||||
Note. IS = informational support; CHESS = Comprehensive Health Enhancement Support System.
Living alone is coded as (0) no and (1) yes.
Study condition is coded as (0) CHESS information and communication services only group and (1) Full CHESS and Mentor group and Full CHESS group.
Values were log transformed.
p < .10.
p < .05.
p < .01.
p < .001.
Table 7.
Estimated CIs of Standardized Betas of Main Predictors.
| CIb (95%) | 50% overlap (two-tailed)c | 80% overlap (one-tailed)d | ||||
|---|---|---|---|---|---|---|
| DVsa | Main predictors | β | Lower | Upper | ||
| Δ QoL | ES from survivors | .245 | .009 | .468 | .181 | .273* |
| ES from new patients | .006 | − .214 | .204 | |||
| Δ CES-D | ES from survivors | − .322 | − .571 | − .108 | − .145 | .072* |
| ES from new patients | .007 | − .267 | .221 | |||
| Δ CIC | IS from survivors | .173 | − .092 | .445 | .176 | .247 |
| IS from new patients | .260 | .057 | .441 | |||
| Δ BCK | IS from survivors | − .114 | − .420 | .180 | .066 | .154 |
| IS from new patients | .211 | − .081 | .536 | |||
Note. DV = dependent variables; CI = confidence interval; QoL = quality of life; ES = emotional support; CES-D = Center for Epidemiologic Studies Depression scale (depression); CIC = cancer information competence; IS = informational support; BCK = breast cancer knowledge.
DVs are the gain scores of variables between the pre- and posttest.
CIs were estimated via a bias-corrected bootstrap (1,000 resamples).
The values were calculated by adding half of 50% of the overlapping CIs to the lower bound estimates of the variables with the greater standardized betas. In the event that the upper bound estimates of the variables with the smaller standardized betas are smaller than these values, the overlapping CIs are smaller than 50%, confirming that the betas are statistically different from each other (p < .05, two-tailed).
The values were calculated by adding half of 80% of the overlapping CIs to the lower bound estimates of the variables with the greater standardized betas. In the event that the upper bound estimates of the variables with the smaller standardized betas are smaller than these values, the overlapping CIs are smaller than 80%, confirming that the betas are statistically different from each other (p < .05, one-tailed).
p < .05.
Figure 2.
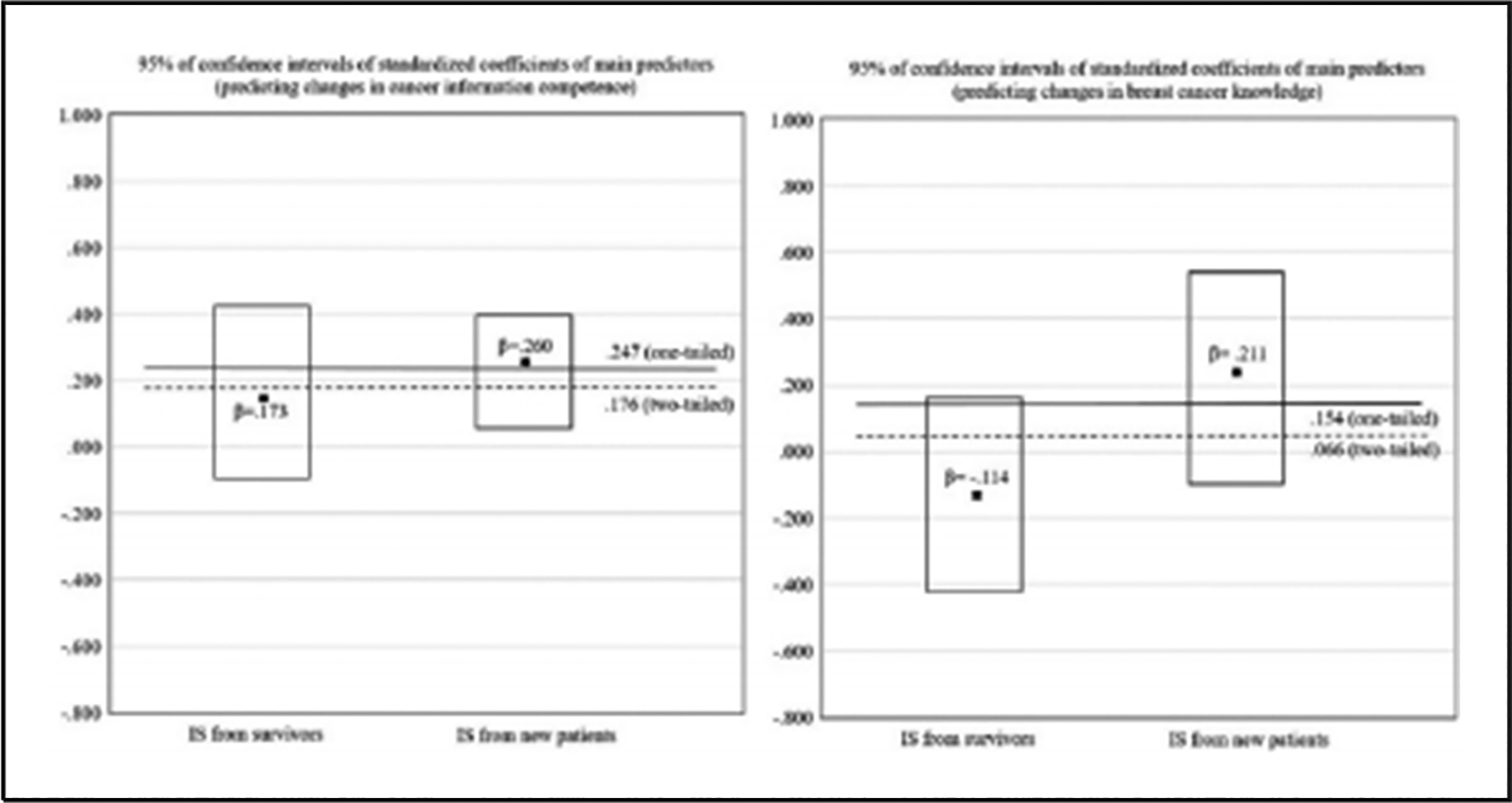
Plots for 95% confidence intervals of the standardized coefficients of the main predictors: Receiving IS.
Note. IS = informational support
H3b predicted that the effect of informational support provided by survivors on cancer information competence would be statistically larger than that provided by new patients. The result showed that neither informational support provided by survivors (b = −.00, SE = .00, β = −.11, p = .25) nor by newly diagnosed patient (b = .00, SE = .00, β = .21, p = .09) was not related to changes in breast cancer knowledge among patients (see Table 6). Thus, H4b was rejected. The final model for breast cancer knowledge improvement (Model 4) was not significant, R2 = .091, F(10, 170) = 1.76, p = .71.
Table 7 presents 95% confidence intervals of the standardized coefficients of the main predictors for each model and the thresholds of 50% (two-tailed, p < .05) and 80% (one-tailed, p < .05) overlaps.
Discussion
This study sought to investigate whether social support provided by breast cancer survivors differs from that provided by new patients, and how social support of survivors contributes to the psychosocial adjustment of newly diagnosed patients in a peer-to-peer CMSS group. It was predicted that breast cancer survivors would provide more emotional (H1a) and informational support (H1b) than newly diagnosed patients. The present study further hypothesized that receiving emotional support provided by survivors would have stronger positive relationships with the improvement of quality of life (H2a) and the reduction of depression (H2b) than receiving emotional support from other newly diagnosed patients. Similarly, this study predicted that receiving informational support provided by survivors would have a stronger positive impact on improving cancer information competence (H3a) and enhancing breast cancer knowledge (H3b) than did receiving informational support provided by other newly diagnosed patients.
The findings supported H1a and H1b. Messages provided by breast cancer survivors included more emotional and informational support than those by newly diagnosed breast cancer patients. Although the number of survivors was much smaller than that of new patients, the results show that survivors accounted for nearly half of the messages posted (n = 8,986, 49.2%), and their messages contained more emotional and information support. The differences in providing emotional support between survivors and newly diagnosed patients were evident across all four types of emotional support. However, the differences in providing information support were significant only in providing information about secondary treatment, side effects, and diagnostic/symptoms. Although the current study cannot provide conclusive evidence for this, it seems that the survivors focused more on information which could be connected with their own experiences than on general information such as health system navigation and general breast cancer information.
The findings from the analyses of the impact of receiving emotional support affirmed H2a and H2b. The results showed that the contributions of emotional support provided by survivors to an improved quality of life and reduced depression among patients were greater than those of emotional support provided by new patients. However, emotional support offered by newly diagnosed patients was found to have no impact on the psychological adjustment of patients. Although it could not be fully confirmed by an empirical test due to a lack of information, the results can be explained by upward identification. As Stanton et al. (1999) explained, patients might want to find hope and learn coping strategies from those who are in a better situation. Emotional support from other newly diagnosed patients, who were likely to be in a similar situation, could be perceived as less attractive and helpful to patients.
Another unexpected finding was that survivor-provided informational support did not contribute to improvement in either cancer information competence or breast cancer knowledge of new patients. Consistent with previous studies (Chen, 2012; Sullivan, 2003), informational support was frequently provided by both survivors and newly diagnosed patients in this study. However, neither survivor-provided nor patient-provided informational support was related to improved breast cancer knowledge. Only informational support provided by other new patients was positively related to enhanced cancer information competence. These findings were intriguing; although the overall results seem to be consistent with some of the previous studies that have shown the limited educational benefits of informational support in peer-led support groups (e.g., Helgeson, Cohen, Schulz, & Yasko, 2000), the positive effect of informational support provided by other newly diagnosed patients cannot be easily explained. Further research needs to be performed to examine whether this difference resulted from qualitative differences (e.g., relevance, novelty) between patient- and survivor-provided information and how patients evaluate and perceive informational support provided by patients and survivors differently.
Limitations
As a secondary analysis, this study had some limitations. First, the current study could not explain the underlying psychological mechanism through which newly diagnosed patients benefited from emotional support provided by survivors. Because of the limited information about the patient’s motivations and perceptions toward survivors or other patients, this study could not provide conclusive evidence of the psychological process such as upward comparisons to survivors or downward contrasts to other patients. Future research may enrich the findings of this study by examining a detailed process of the social comparisons that newly diagnosed patients may experience.
Second, the lack of detailed information about survivors in this study prevented further investigation of the topics, such as posttraumatic growth and helping behavior, motivations of providing support, and survivors’ perceived benefits from participating in peer-to-peer CMSS groups. Previous studies have indicated that survivors derive benefits such as self-empowerment and a better quality of life by sharing their experiences and providing emotional support to others (Barak et al., 2008; Sharf, 1997; Sutton & Erlen, 2006; van Uden-Kraan et al., 2008). Further study will need to be performed on which motivations spur survivors to participate in CMSS group and how survivors can benefit from participating in CMSS groups.
Finally, although this study found that survivor-provided emotional support contributed to an improved quality of life, the average change in quality of life was very small (M = 0.05, SD = 0.44). This may be due to the large variance among patients, that is, the quality of life of some patients improved a great deal, whereas that of others declined quite a bit. This result may alternately suggest that some patients can benefit more from receiving emotional support than other patients. Future research will need to investigate who can benefit more from participating in CMSS groups and why some patients cannot benefit from it.
Implications
Despite these limitations, the present study contributes to providing empirical evidence regarding the impact of social support provided by breast cancer survivors. This study shows that the impact of social support can differ according to who provided it and that survivor-provided emotional support in particular is more effective in improving quality of life and alleviating depression of patients. Although some studies have found that reading survivors’ personal stories is related to better cognitive and behavioral outcomes in new patients (Kreuter et al., 2008; McQueen & Kreuter, 2010), the role of survivors in these studies was relatively limited because they could not directly interact with other patients. Moreover, the few studies that allowed survivors to communicate with other patients (e.g., Lieberman & Russo, 2002; Sharf, 1997) did not explain how survivors interacted with new patients or how survivors’ support affected the cognitive and behavioral adjustment of new patients. Given the paucity of research on survivors’ behavior and role in CMSS groups, the findings of this study can serve as a starting point for further research regarding the role of cancer survivors in CMSS groups.
Another contribution of this study is its advanced methodology. The present study introduced a novel methodology to capture the contextual meaning of expressions more precisely and to analyze a massive amount of content from CMSS groups. The combination of deductive and inductive processes allowed researchers to match concepts with actual usage in the content and to revise the coding rules accordingly. In addition, with these dynamic rules, it was possible to capture the contextual meanings of expressions more precisely, beyond merely counting the number of specific words. This methodology can be used to analyze content from many computer-mediated or mobile communications, which is usually characterized by its massiveness of amount and nonstandard nature of language usage.
A further important contribution of this study is that the findings of this study provide helpful insights for health care providers who will develop peer-to-peer support programs for breast cancer patients. On one hand, given the importance of survivors in providing support and the impact of their emotional support on new patients, health care providers will be able to develop more effective social support programs by encouraging survivors’ participation. On the other hand, based on the limited evidence regarding the impact of peer-provided informational support, health care providers may need to consider how to provide adequate informational support to patients in addition to peer support groups.
Although this study was conducted in the United States, it also has practical implications for other countries especially where social support for breast cancer patients is not sufficient. For example, breast cancer incidence and mortality are higher in Japan, Singapore, and Hong Kong than in the other Asian countries (Curado, 2011). Studies have found that cultural characteristics in these countries, such as stigmatization, strong family bond, and interpersonal responsibility, may hinder patients from receiving adequate social support beyond their family members, thereby contributing to poor prognosis (Ikeda et al., 2013; Makabe & Hull, 2000; Ng et al., 2016). Given the limited social support and cultural barriers in these countries, CMSS groups in which patients can communicate with survivors can be more valuable sources of social support.
Finally, the findings of this study are particularly pertinent to the less-developed countries of South Asia, Latin America, and Africa. Given the limited resources and social support available to patients in these countries (Chib, 2013), survivor-provided social support in CMSS groups can be indispensable for psychosocial adjustment of patients. Although it is difficult to use CMSS groups based on laptops or desktops in these countries due to the low Internet penetration rate, mobile technologies have become more available in underdeveloped countries. A growing number of studies have shown that mobile technologies offer cost-effective tools for prevention, management, and treatment of various diseases in developing countries (e.g., Chib, van Velthoven, & Car, 2015; Déglise, Suggs, & Odermatt, 2012; Gurman, Rubin, & Roess, 2012). Furthermore, mobile technologies allow patients to receive social support in a more timely and convenient manner because they provide a wide variety of communication tools including text messages, instant messaging, and phone calls (Gustafson et al., 2011; Kahn, Yang, & Kahn, 2010). CMSS groups based on mobile technologies, therefore, can be effective tools for providing social support to patients in developing countries. Extending the findings of this study, future research needs to examine the feasibility of CMSS groups based on mobile technologies and the survivors’ role therein.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was funded by P50 CA095817-05 from the National Cancer Institute.
Author Biographies
Tae-Joon Moon is a PhD candidate in the School of Journalism and Mass Communication at University of Wisconsin–Madison. His research topics include analysis of use patterns and the feasibility of computer-mediated and/or smartphone-based health management system for people with chronic diseases.
Ming-Yuan Chih (PhD, University of Wisconsin–Madison, 2013; MPH, University of Missouri–Columbia) is an assistant professor in the College of Health Sciences at University of Kentucky, Lexington. His research focused on developing and implementing interventions that enable patients and their families to play a central role in the management and improvement of the patient’s health.
Dhavan V. Shah (PhD, University of Minnesota–Twin Cities, 1999) is Maier-Bascom Professor at the University of Wisconsin–Madison, Director of the Mass Communication Research Center (MCRC), and Scientific Director in the Center for Health Enhancement System Studies (CHESS). His work concerns framing and cueing effects on social judgments, digital media influence on civic and political engagement, and the impact of ICTs on chronic disease management. Across these domains of work, he has increasingly applied computational techniques to tackle social science questions.
Woohyun Yoo (PhD, University of Wisconsin–Madison, 2014) is an assistant professor in the Survey and Health Policy Research Center at Dongguk University. His research is grounded at the intersections of emerging media technologies, health communication, and message effects.
David H. Gustafson (PhD in industrial engineering, University of Michigan–Ann Arbor, 1966). He is director of the Center for Health Enhancement systems studies at University of Wisconsin–Madison. His research interests include applications of systems engineering to address organizational and individual change in health.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Alpers GW, Winzelberg AJ, Classen C, Roberts H, Dev P, Koopman C, & Barr Taylor C (2005). Evaluation of computerized text analysis in an Internet breast cancer support group. Computers in Human Behavior, 21, 361–376. doi: 10.1016/j.chb.2004.02.008 [DOI] [Google Scholar]
- Ashbury FD, Cameron C, Mercer SL, Fitch M, & Nielsen E (1998). One-on-one peer support and quality of life for breast cancer patients. Patient Education and Counseling, 35, 89–100. doi: 10.1016/s0738-3991(98)00035-4 [DOI] [PubMed] [Google Scholar]
- Baker F, Denniston M, Haffer SC, & Liberatos P (2009). Change in health-related quality of life of newly diagnosed cancer patients, cancer survivors, and controls. Cancer, 115, 3024–3033. doi: 10.1002/cncr.24330 [DOI] [PubMed] [Google Scholar]
- Barak A, Boniel-Nissim M, & Suler J (2008). Fostering empowerment in online support groups. Computers in Human Behavior, 24, 1867–1883. doi: 10.1016/j.chb.2008.02.004 [DOI] [Google Scholar]
- Batenburg A, & Das E (2014). Emotional coping differences among breast cancer patients from an online support group: A cross-sectional study. Journal of Medical Internet Research, 16(2), e28. doi: 10.2196/jmir.2831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellizzi KM, & Blank TO (2006). Predicting posttraumatic growth in breast cancer survivors. Health Psychology, 25, 47–56. doi: 10.1037/0278-6133.25.1.47 [DOI] [PubMed] [Google Scholar]
- Braithwaite DO, Waldron VR, & Finn J (1999). Communication of social support in computer-mediated groups for people with disabilities. Health Communication, 11, 123–151. doi: 10.1207/s15327027hc1102_2 [DOI] [PubMed] [Google Scholar]
- Burgess C, Cornelius V, Love S, Graham J, Richards M, & Ramirez A (2005). Depression and anxiety in women with early breast cancer: Five year observational cohort study. British Medical Journal, 330, 702–705. doi: 10.1136/bmj.38343.670868.D3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler LD, Koopman C, Classen C, & Spiegel D (1999). Traumatic stress, life events, and emotional support in women with metastatic breast cancer: Cancer-related traumatic stress symptoms associated with past and current stressors. Health Psychology, 18, 555–560. doi: 10.1037/0278-6133.18.6.555 [DOI] [PubMed] [Google Scholar]
- Buunk BP, Collins RL, Taylor SE, VanYperen NW, & Dakof GA (1990). The affective consequences of social comparison: Either direction has its ups and downs. Journal of Personality and Social Psychology, 59, 1238–1249. doi: 10.1037/0022-3514.59.6.1238 [DOI] [PubMed] [Google Scholar]
- Calhoun LG, & Tedeschi RG (1990). Positive aspects of critical life problems: Recollections of grief. OMEGA: Journal of Death and Dying, 20, 265–272. doi: 10.2190/qdy6-6pqc-kqwv-5u7k [DOI] [Google Scholar]
- Cameron C, Ashbury FD, & Iverson DC (1997). Perspectives on reach to recovery and CanSurmount: Informing the evaluation model. Cancer Prevention Control, 1, 102–107. Available from http://europepmc.org/ [PubMed] [Google Scholar]
- Campbell HS, Phaneuf MR, & Deane K (2004). Cancer peer support programs—Do they work? Patient Education and Counseling, 55, 3–15. doi: 10.1016/j.pec.2003.10.001 [DOI] [PubMed] [Google Scholar]
- Chen AT (2012). Exploring online support spaces: Using cluster analysis to examine breast cancer, diabetes and fibromyalgia support groups. Patient Education and Counseling, 87, 250–257. doi: 10.1016/j.pec.2011.08.017 [DOI] [PubMed] [Google Scholar]
- Chib A (2013). The promise and peril of mHealth in developing countries. Mobile Media & Communication, 1, 69–75. doi: 10.1177/2050157912459502 [DOI] [Google Scholar]
- Chib A, van Velthoven MH, & Car J (2015). mHealth adoption in low-resource environments: A review of the use of mobile healthcare in developing countries. Journal of Health Communication, 20, 4–34. doi: 10.1080/10810730.2013.864735 [DOI] [PubMed] [Google Scholar]
- Cohen S (2004). Social relationships and health. American Psychologist, 59, 676–684. doi: 10.1037/0003-066X.59.8.676 [DOI] [PubMed] [Google Scholar]
- Cohen S, Underwood LG, & Gottlieb BH (2000). Social support measurement and intervention: A guide for health and social scientists. New York, NY: Oxford University Press. [Google Scholar]
- Cohen S, & Wills TA (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98, 310–357. doi: 10.1037/0033-2909.98.2.310 [DOI] [PubMed] [Google Scholar]
- Cordova MJ, Cunningham LLC, Carlson CR, & Andrykowski MA (2001). Posttraumatic growth following breast cancer: A controlled comparison study. Health Psychology, 20, 176–185. doi: 10.1037/0278-6133.20.3.176 [DOI] [PubMed] [Google Scholar]
- Coulson NS, Buchanan H, & Aubeeluck A (2007). Social support in cyberspace: A content analysis of communication within a Huntington’s disease online support group. Patient Education and Counseling, 68, 173–178. doi: 10.1016/j.pec.2007.06.002 [DOI] [PubMed] [Google Scholar]
- Cumming G (2009). Inference by eye: Reading the overlap of independent confidence intervals. Statistics in Medicine, 28, 205–220. doi: 10.1002/sim.3471 [DOI] [PubMed] [Google Scholar]
- Curado MP (2011). Breast cancer in the world: Incidence and mortality [Cáncer de mama en el mundo: incidencia y mortalidad]. Salud Pública de México, 53, 372–384. Available from http://www.scielosp.org/ [PubMed] [Google Scholar]
- Cutrona CE, & Suhr JA (1994). Social support communication in the context of marriage: An analysis of couples’ supportive interactions. In Burleson BR, Albrecht TL, & Sarason IG(Eds.), Communication of social support (pp. 113–135). Thousand Oaks, CA: SAGE. [Google Scholar]
- Davis C, Williams P, Parle M, Redman S, & Turner J (2004). Assessing the support needs of women with early breast cancer in Australia. Cancer Nursing, 27, 169–174. [DOI] [PubMed] [Google Scholar]
- Déglise C, Suggs LS, & Odermatt P (2012). SMS for disease control in developing countries: A systematic review of mobile health applications. Journal of Telemedicine and Telecare, 18, 273–281. doi: 10.1258/jtt.2012.110810 [DOI] [PubMed] [Google Scholar]
- Dennis C-L (2003). Peer support within a health care context: A concept analysis. International Journal of Nursing Studies, 40, 321–332. doi: 10.1016/S0020-7489(02)00092-5 [DOI] [PubMed] [Google Scholar]
- Dunn J, Steginga SK, Rosoman N, & Millichap D (2003). A review of peer support in the context of cancer. Journal of Psychosocial Oncology, 21(2), 55–67. doi: 10.1300/J077v21n02_04 [DOI] [Google Scholar]
- Falzon C, Radel R, Cantor A, & d’Arripe-Longueville F (2015). Understanding narrative effects in physical activity promotion: The influence of breast cancer survivor testimony on exercise beliefs, self-efficacy, and intention in breast cancer patients. Supportive Care in Cancer, 23, 761–768. doi: 10.1007/s00520-014-2422-x [DOI] [PubMed] [Google Scholar]
- Fan DP (1990). Information processing expert system for text analysis and predicting public opinion based information available to the public (U.S. Patents 4,930,077). Retrieved from http://patft.uspto.gov/netacgi/nph-Parser?Sect2=PTO1&Sect2=HITOFF&p=1&u=/netahtml/PTO/search-bool.html&r=1&f=G&l=50&d=PALL&RefSrch=yes&Query=PN/4930077
- Fan DP (1994). Information processing analysis system for sorting and scoring text (U.S. Patents 5,371,673). Retrieved from http://patft.uspto.gov/netacgi/nph-Parser?Sect2=PTO1&Sect2=HITOFF&p=1&u=/netahtml/PTO/search-bool.html&r=1&f=G&l=50&d=PALL&RefSrch=yes&Query=PN/5371673
- Festinger L (1954). A theory of social comparison processes. Human Relations, 7, 117–140. doi: 10.1177/001872675400700202 [DOI] [Google Scholar]
- Frazier P, Greer C, Gabrielsen S, Tennen H, Park C, & Tomich P (2013). The relation between trauma exposure and prosocial behavior. Psychological Trauma, 5, 286–294. doi: 10.1037/a0027255 [DOI] [Google Scholar]
- Giese-Davis J, Bliss-Isberg C, Carson K, Star P, Donaghy J, Cordova MJ, … Spiegel D (2006). The effect of peer counseling on quality of life following diagnosis of breast cancer: An observational study. Psycho-Oncology, 15, 1014–1022. doi: 10.1002/pon.1037 [DOI] [PubMed] [Google Scholar]
- Global Burden of Disease Cancer Collaboration. (2015). The global burden of cancer 2013. JAMA Oncology, 1, 505–527. doi: 10.1001/jamaoncol.2015.0735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb BH, & Bergen AE (2010). Social support concepts and measures. Journal of Psychosomatic Research, 69, 511–520. doi: 10.1016/j.jpsychores.2009.10.001 [DOI] [PubMed] [Google Scholar]
- Gray R, Fitch M, Davis C, & Phillips C (1997). A qualitative study of breast cancer self-help groups. Psycho-Oncology, 6, 279–289. doi: [DOI] [PubMed] [Google Scholar]
- Gremore TM, Baucom DH, Porter LS, Kirby JS, Atkins DC, & Keefe FJ (2011). Stress buffering effects of daily spousal support on women’s daily emotional and physical experiences in the context of breast cancer concerns. Health Psychology, 30, 20–30. doi: 10.1037/a0021798 [DOI] [PubMed] [Google Scholar]
- Griesser AC, Vlastos G, Morel L, Beaume C, Sappino AP, & Haller G (2011). Socio-demographic predictors of high support needs in newly diagnosed breast cancer patients. European Journal of Cancer Care, 20, 466–474. doi: 10.1111/j.1365-2354.2010.01190.x [DOI] [PubMed] [Google Scholar]
- Gurman TA, Rubin SE, & Roess AA (2012). Effectiveness of mHealth behavior change communication interventions in developing countries: A systematic review of the literature. Journal of Health Communication, 17, 82–104. doi: 10.1080/10810730.2011.649160 [DOI] [Google Scholar]
- Gustafson DH, Hawkins R, Pingree S, McTavish F, Arora NK, Mendenhall J, & Salner A (2001). Effect of computer support on younger women with breast cancer. Journal of General Internal Medicine, 16, 435–445. doi: 10.1046/j.1525-1497.2001.016007435.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson DH, Shaw BR, Isham A, Baker T, Boyle MG, & Levy M (2011). Explicating an evidence-based, theoretically informed, mobile technology-based system to improve outcomes for people in recovery for alcohol dependence. Substance Use & Misuse, 46, 96–111. doi: 10.3109/10826084.2011.521413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han JY, Shaw BR, Hawkins RP, Pingree S, Mctavish F, & Gustafson DH (2008). Expressing positive emotions within online support groups by women with breast cancer. Journal of Health Psychology, 13, 1002–1007. doi: 10.1177/1359105308097963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannah ME, & Midlarsky E (2005). Helping by siblings of children with mental retardation. American Journal on Mental Retardation, 110, 87–99. doi: [DOI] [PubMed] [Google Scholar]
- Hanson Frost H, Suman VJ, Rummans TA, Dose AM, Taylor M, Novotny P, … Evans R (2000). Physical, psychological and social well-being of women with breast cancer: The influence of disease phase. Psycho-Oncology, 9, 221–231. [DOI] [PubMed] [Google Scholar]
- Harrison JD, Young JM, Price MA, Butow PN, & Solomon MJ (2009). What are the unmet supportive care needs of people with cancer? A systematic review. Supportive Care in Cancer, 17, 1117–1128. doi: 10.1007/s00520-009-0615-5 [DOI] [PubMed] [Google Scholar]
- Hayes AF, & Krippendorff K (2007). Answering the call for a standard reliability measure for coding data. Communication Methods and Measures, 1, 77–89. doi: 10.1080/19312450709336664 [DOI] [Google Scholar]
- Helgeson VS, Cohen S, Schulz R, & Yasko J (2000). Group support interventions for women with breast cancer: Who benefits from what? Health Psychology, 19, 107–114. doi: 10.1037/0278-6133.19.2.107 [DOI] [PubMed] [Google Scholar]
- Helgeson VS, & Gottlieb BH (2000). Social support. In Cohen S, Underwood LG, & Gottlieb BH (Eds.), Social support measurement and intervention: A guide for health and social scientists (pp. 221–245). New York, NY: Oxford University Press. [Google Scholar]
- Howard-Anderson J, Ganz PA, Bower JE, & Stanton AL (2012). Quality of life, fertility concerns, and behavioral health outcomes in younger breast cancer survivors: A systematic review. Journal of the National Cancer Institute, 104, 386–405. doi: 10.1093/jnci/djr541 [DOI] [PubMed] [Google Scholar]
- Høybye MT, Johansen C, & Tjornhoj-Thomsen T (2005). Online interaction: Effects of storytelling in an Internet breast cancer support group. Psycho-Oncology, 14, 211–220. doi: 10.1002/pon.837 [DOI] [PubMed] [Google Scholar]
- Ikeda A, Kawachi I, Iso H, Iwasaki M, Inoue M, & Tsugane S (2013). Social support and cancer incidence and mortality: The JPHC study cohort II. Cancer Causes & Control, 24, 847–860. doi: 10.1007/s10552-013-0147-7 [DOI] [PubMed] [Google Scholar]
- Kahn JG, Yang JS, & Kahn JS (2010). “Mobile” health needs and opportunities in developing countries. Health Affairs, 29, 252–258. doi: 10.1377/hlthaff.2009.0965 [DOI] [PubMed] [Google Scholar]
- Kim E, Han JY, Moon TJ, Shaw BR, Shah DV, McTavish FM, & Gustafson DH (2012). The process and effect of supportive message expression and reception in online breast cancer support groups. Psycho-Oncology, 21, 531–540. doi: 10.1002/pon.1942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, Han JY, Shaw B, McTavish F, & Gustafson D (2010). The roles of social support and coping strategies in predicting breast cancer patients’ emotional well-being: Testing mediation and moderation models. Journal of Health Psychology, 15, 543–552. doi: 10.1177/1359105309355338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kornblith AB, Herndon JE, Zuckerman E, Viscoli CM, Horwitz RI, Cooper MR, & Leukemia Group B (2001). Social support as a buffer to the psychological impact of stressful life events in women with breast cancer. Cancer, 91, 443–454. doi: [DOI] [PubMed] [Google Scholar]
- Kreuter M, Buskirk T, Holmes K, Clark E, Robinson L, Si X, & Mathews K (2008). What makes cancer survivor stories work? An empirical study among African American women. Journal of Cancer Survivorship, 2, 33–44. doi: 10.1007/s11764-007-0041-y [DOI] [PubMed] [Google Scholar]
- Leydon GM, Boulton M, Moynihan C, Jones A, Mossman J, Boudioni M, & McPherson K (2000). Cancer patients’ information needs and information seeking behaviour: In depth interview study. British Medical Journal, 320, 909–913. doi: 10.1136/bmj.320.7239.909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman MA, & Goldstein BA (2006). Not all negative emotions are equal: The role of emotional expression in online support groups for women with breast cancer. Psycho-Oncology, 15, 160–168. doi: 10.1002/pon.932 [DOI] [PubMed] [Google Scholar]
- Lieberman MA, & Russo S (2002). Self help groups and the Internet: Breast cancer news-groups. International Journal of Self Help and Self Care, 1, 323–344. [Google Scholar]
- Macvean ML, White VM, & Sanson-Fisher R (2008). One-to-one volunteer support programs for people with cancer: A review of the literature. Patient Education and Counseling, 70, 10–24. doi: 10.1016/j.pec.2007.08.005 [DOI] [PubMed] [Google Scholar]
- Makabe R, & Hull MM (2000). Components of social support among Japanese women with breast cancer. Oncology Nursing Forum, 27, 1381–1390. Available from http://europepmc.org/ [PubMed] [Google Scholar]
- Manne S, Ostroff J, Winkel G, Goldstein L, Fox K, & Grana G (2004). Posttraumatic growth after breast cancer: Patient, partner, and couple perspectives. Psychosomatic Medicine, 66, 442–454. doi: 10.1097/01.psy.0000127689.38525.7d [DOI] [PubMed] [Google Scholar]
- McQueen A, & Kreuter MW (2010). Women’s cognitive and affective reactions to breast cancer survivor stories: A structural equation analysis. Patient Education and Counseling, 81(Suppl. 1), S15–S21. doi: 10.1016/j.pec.2010.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier A, Lyons EJ, Frydman G, Forlenza M, & Rimer BK (2007). How cancer survivors provide support on cancer-related Internet mailing lists. Journal of Medical Internet Research, 9(2), e12. doi: 10.2196/jmir.9.2.e12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer A, Coroiu A, & Korner A (2015). One-to-one peer support in cancer care: A review of scholarship published between 2007 and 2014. European Journal of Cancer Care, 24, 299–312. doi: 10.1111/ecc.12273 [DOI] [PubMed] [Google Scholar]
- Meyerowitz BE (1980). Psychosocial correlates of breast cancer and its treatments. Psychological Bulletin, 87, 108–131. doi: 10.1037/0033-2909.87.1.108 [DOI] [PubMed] [Google Scholar]
- Namkoong K, Shah DV, Han JY, Kim SC, Yoo W, Fan D, & Gustafson DH (2010). Expression and reception of treatment information in breast cancer support groups: How health self-efficacy moderates effects on emotional well-being. Patient Education and Counseling, 81(Suppl.), S41–S47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng HY, Griva K, Lim HA, Tan JY, Mahendran R, Griva K, & Block A (2016). The burden of filial piety: A qualitative study on caregiving motivations amongst family caregivers of patients with cancer in Singapore. Psychology & Health, 31, 1293–1310. doi: 10.1080/08870446.2016.1204450 [DOI] [PubMed] [Google Scholar]
- Owen JE, Klapow JC, Roth DL, & Tucker DC (2004). Use of the Internet for information and support: Disclosure among persons with breast and prostate cancer. Journal of Behavioral Medicine, 27, 491–505. doi: 10.1023/B:JOBM.0000047612.81370.f7 [DOI] [PubMed] [Google Scholar]
- Pérez M, Sefko JA, Ksiazek D, Golla B, Casey C, Margenthaler JA, … Jeffe DB (2014). A novel intervention using interactive technology and personal narratives to reduce cancer disparities: African American breast cancer survivor stories. Journal of Cancer Survivorship, 8, 21–30. doi: 10.1007/s11764-013-0308-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petosa RL, & Smith LH (2014). Peer mentoring for health behavior change: A systematic review. American Journal of Health Education, 45, 351–357. doi: 10.1080/19325037.2014.945670 [DOI] [Google Scholar]
- Radloff LS (1977). The CES-D scale. Applied Psychological Measurement, 1, 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Reich M, Lesur A, & Perdrizet-Chevallier C (2008). Depression, quality of life and breast cancer: A review of the literature. Breast Cancer Research and Treatment, 110, 9–17. doi: 10.1007/s10549-007-9706-5 [DOI] [PubMed] [Google Scholar]
- Rinehart ME (1994). The reach to recovery program. Cancer, 74(Suppl. 1), 372–375. doi: 10.1002/cncr.2820741324 [DOI] [PubMed] [Google Scholar]
- Rubenstein EL (2015). “They are always there for me”: The convergence of social support and information in an online breast cancer community. Journal of the Association for Information Science and Technology, 66, 1418–1430. doi: 10.1002/asi.23263 [DOI] [Google Scholar]
- Rutten LJF, Arora NK, Bakos AD, Aziz N, & Rowland J (2005). Information needs and sources of information among cancer patients: A systematic review of research (1980–2003). Patient Education and Counseling, 57, 250–261. doi: 10.1016/j.pec.2004.06.006 [DOI] [PubMed] [Google Scholar]
- Sanson-Fisher R, Girgis A, Boyes A, Bonevski B, Burton L, Cook P, & Supportive Care Review G (2000). The unmet supportive care needs of patients with cancer. Cancer, 88, 226–237. doi: [DOI] [PubMed] [Google Scholar]
- Sharf BF (1997). Communicating breast cancer on-line: Support and empowerment on the Internet. Women & Health, 26, 65–84. doi: 10.1300/J013v26n01_05 [DOI] [PubMed] [Google Scholar]
- Siegel RL, Miller KD, & Jemal A (2015). Cancer statistics, 2015. CA: A Cancer Journal for Clinicians, 65, 5–29. doi: 10.3322/caac.21254 [DOI] [PubMed] [Google Scholar]
- Silverman-Dresner T (1990). Self-help groups for women who have had breast cancer. Imagination, Cognition and Personality, 9, 237–243. doi: 10.2190/14gd-87a3-g7w6-7jre [DOI] [Google Scholar]
- Stanton AL, Danoff-Burg S, Cameron CL, Cameron CL, Snider PR, & Kirk SB (1999). Social comparison and adjustment to breast cancer: An experimental examination of upward affiliation and downward evaluation. Health Psychology, 18, 151–158. doi: 10.1037/0278-6133.18.2.151 [DOI] [PubMed] [Google Scholar]
- Staub E, & Vollhardt J (2008). Altruism born of suffering: The roots of caring and helping after victimization and other trauma. American Journal of Orthopsychiatry, 78, 267–280. doi: 10.1037/a0014223 [DOI] [PubMed] [Google Scholar]
- Sullivan CF (2003). Gendered cybersupport: A thematic analysis of two online cancer support groups. Journal of Health Psychology, 8, 83–103. doi: 10.1177/1359105303008001446 [DOI] [PubMed] [Google Scholar]
- Sutton LB, & Erlen JA (2006). Effects of mutual dyad support on quality of life in women with breast cancer. Cancer Nursing, 29, 488–498. [DOI] [PubMed] [Google Scholar]
- Tausczik YR, & Pennebaker JW (2010). The psychological meaning of words: LIWC and computerized text analysis methods. Journal of Language and Social Psychology, 29, 24–54. doi: 10.1177/0261927x09351676 [DOI] [Google Scholar]
- Taylor SE, & Lobel M (1989). Social comparison activity under threat: Downward evaluation and upward contacts. Psychological Review, 96, 569–575. doi: 10.1037/0033-295X.96.4.569 [DOI] [PubMed] [Google Scholar]
- Tighe M, Molassiotis A, Morris J, & Richardson J (2011). Coping, meaning and symptom experience: A narrative approach to the overwhelming impacts of breast cancer in the first year following diagnosis. European Journal of Oncology Nursing, 15, 226–232. doi: 10.1016/j.ejon.2011.03.004 [DOI] [PubMed] [Google Scholar]
- Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, & Jemal A (2015). Global cancer statistics, 2012. CA: A Cancer Journal for Clinicians, 65, 87–108. doi: 10.3322/caac.21262 [DOI] [PubMed] [Google Scholar]
- Ussher J, Kirsten L, Butow P, & Sandoval M (2006). What do cancer support groups provide which other supportive relationships do not? The experience of peer support groups for people with cancer. Social Science & Medicine, 62, 2565–2576. doi: 10.1016/j.socs-cimed.2005.10.034 [DOI] [PubMed] [Google Scholar]
- van Uden-Kraan CF, Drossaert CH, Taal E, Shaw BR, Seydel ER, & van de Laar MA (2008). Empowering processes and outcomes of participation in online support groups for patients with breast cancer, arthritis, or fibromyalgia. Qualitative Health Research, 18, 405–417. doi: 10.1177/1049732307313429 [DOI] [PubMed] [Google Scholar]
- Vivar CG, & McQueen A (2005). Informational and emotional needs of long-term survivors of breast cancer. Journal of Advanced Nursing, 51, 520–528. [DOI] [PubMed] [Google Scholar]
- Vogel BA, Bengel J, & Helmes AW (2008). Information and decision making: Patients’ needs and experiences in the course of breast cancer treatment. Patient Education and Counseling, 71, 79–85. doi: 10.1016/j.pec.2007.11.023 [DOI] [PubMed] [Google Scholar]
- Walther J, & Boyd S (2002). Attraction to computer-mediated social support. In Lin CA & Atkin D (Eds.), Communication technology and society: Audience adoption and uses (pp. 153–188). Cresskill, NJ: Hampton Press. [Google Scholar]
- Weiss T (2004). Correlates of posttraumatic growth in married breast cancer survivors. Journal of Social and Clinical Psychology, 23, 733–746. doi: 10.1521/jscp.23.5.733.50750 [DOI] [Google Scholar]
- Winzelberg AJ, Classen C, Alpers GW, Roberts H, Koopman C, Adams RE, … Taylor CB (2003). Evaluation of an Internet support group for women with primary breast cancer. Cancer, 97, 1164–1173. doi: 10.1002/cncr.11174 [DOI] [PubMed] [Google Scholar]
- Wood JV, Taylor SE, & Lichtman RR (1985). Social comparison in adjustment to breast cancer. Journal of Personality and Social Psychology, 49, 1169–1183. doi: 10.1037/0022-3514.49.5.1169 [DOI] [PubMed] [Google Scholar]
- Wright KB (2016). Communication in health-related online social support groups/communities: A review of research on predictors of participation, applications of social support theory, and health outcomes. Review of Communication Research, 4, 65–87. doi: 10.12840/issn.2255-4165.2016.04.01.010 [DOI] [Google Scholar]


