Abstract
Burnout in healthcare workers (HCWs) is costly, consequential, and alarmingly high. Many HCWs report not having enough time or opportunities to engage in self-care. Brief, engaging, evidence-based tools have unique potential to alleviate burnout and improve well-being. Three prospective cohort studies tested the efficacy of web-based interventions: Three Good Things (n = 275), Gratitude Letter (n = 123), and the Looking Forward Tool (n = 123). Metrics were emotional exhaustion, depression, subjective happiness, work-life balance, emotional thriving, and emotional recovery. Across all studies, participants reported improvements in all metrics between baseline and post assessments, with two exceptions in study 1 (emotional thriving and happiness at 6 and 12-month post) and study 3 (optimism and emotional thriving at day 7). The Three Good Things, Gratitude Letter, and Looking Forward tools appear promising interventions for the issue of HCW burnout.
Keywords: Positive psychology interventions, Three Good Things, gratitude, hope, burnout, healthcare
Introduction
Globally, over half a billion people struggle with anxiety, depression or both, and the rates of these and other mental disorders are on the rise (World Health Organization, 2017). A recent study by the World Health Organization found that such disorders cost the global economy $1 trillion in lost productivity each year (World Health Organization, 2017). The U.S. Department of Health and Human Services estimates that annually, one out of five adults have a mental illness, and less than half of them received mental health services (Hedden et al., 2015). The prevalence of suffering is high, and the utilization of resources is not keeping pace. This is particularly pronounced for healthcare workers (HCWs), who put themselves in sufferings’ way at great personal cost to their own well-being (e.g. Mata et al., 2015; Shanafelt et al., 2015).
Roughly a third to a half of HCWs meet the criteria for burnout (Poghosyan et al., 2010; Shanafelt et al., 2019), and rates of burnout continue to climb. We know that HCW burnout is common (Poghosyan et al., 2010; Shanafelt et al., 2015), consequential to patients (i.e. mortality and healthcare acquired infection; Aiken et al., 2002; Cimiotti et al., 2012), interferes with the safe delivery of patient care (Hall et al., 2016), and the ability to engage in quality improvement efforts (Adair et al., 2018). We also know burnout is bad for HCWs, with consequences ranging from marital problems (Kumar, 2016) to shorter lifespan (Ahola et al., 2010). Moreover, recent evidence suggests burnout and problems with work-life balance are socially contagious (Petitta et al., 2017; Schwartz et al., 2019). In other words, eating lunch, taking breaks, and leaving work on time, as well as your burnout level, are variables that are associated with the behavior and well-being of your colleagues.
Positive emotion
Just as depression and anxiety have been linked to lower levels of positive emotions (Fredrickson, 2001; Gloria & Steinhardt, 2016), the same has been found for burnout (Gong, Schooler, Yong, &Mingda, 2018). Research has consistently shown that experiencing positive emotion is a causal link in the chain of feeling greater purpose (Fredrickson et al., 2008) and recovery after emotional upheavals (Fredrickson et al., 2000). Positive emotions, like hope, serve as little engines that effectively recharge our depleted batteries (Fredrickson & Joiner, 2002; Gong & Li, 2017). In controlled experiments, positive emotions demonstrably undo the cardiovascular sequelae of an emotional upheaval relative to negative emotions and control groups (Fredrickson & Levenson, 1998). Improvements in well-being after randomized control trials of meditation (Fredrickson et al., 2008) show that a distinct mechanism at work is the increased access to positive emotion that comes with practice. Similarly, the COMPASS program, designed to facilitate meaningful conversations among HCWs, is thought beneficial due to its ability to elicit positive emotions towards work and foster connections with colleagues (West et al., 2014). The Three Good Things intervention also intentionally elicits moments to reflect on events that generated positive emotion (Seligman et al., 2005; Sexton & Adair, 2018). Thus, across a number of interventions being used to address burnout in healthcare, a common thread is increasing access to positive emotion.
However, as the number of burnout prevalence studies continue to grow (Dugani et al., 2018; Hall et al., 2016), there are still relatively few (e.g. Adair et al., 2020; Profit et al., 2018; Sexton & Adair, 2018) well-documented and scalable interventions that offer relief from burnout. Given the increasing rates of HCW burnout, there is an urgent need for interventions that are simple, brief, effective and help facilitate the restorative effects of positive emotions.
Across three prospective cohort studies, we test the efficacy of web-based interventions designed to improve well-being by enhancing opportunities to experience positive emotions. The first study is a modified Three Good Things intervention for reflecting on ‘what went well today’, the second is a brief gratitude letter intervention for reflecting on your appreciation toward a specific individual, and the third is a novel tool for reflecting on what you are looking forward to in the future.
Study 1: Three Good Things (3GT)
Study 1 tested a modified version of the Three Good Things tool as a way to improve HCW well-being. In this study, the tool was administered via text message and delivered over a 15-day period, instead of the typical 7-day period (Seligman et al., 2005).
Method
Participants
Potential participants learned of the tools and the enrollment link by participating (or through colleagues who participated) in a webinar or continuing education talk given by the first or third authors (all enrollment links are available at https://www.hsq.dukehealth.org/tools/). All HCWs (clinical and non-clinical) 18 and older were eligible to participate. Due to the ease of enrollment, we define initiators as participants that responded to links that were sent to them as part of the study. Participation was initiated (used the day 1 text link) by 275 HCWs (predominately female, 82.5%) and 146 (53%) completed the final day of the intervention (day 15). HCW role information for all studies can be found in Table 1, Additional demographic information can be found in the online supplemental.
Table 1.
Healthcare worker role by study.
| Study 1: Three Good Things (N = 275) n (%) | Study 2: Gratitude Letter (N = 123) n (%) | Study 3: Looking Forward (N = 123) n (%) | |
|---|---|---|---|
| Admin Support | 6 (2.2%) | 2 (1.6%) | 3 (2.4%) |
| Attending/Staff/Fellow/Resident Physician | 74 (26.9%) | 35 (28.5%) | 10 (8.1%) |
| Nurse Manager/Charge Nurse | 40 (14.5) | 20 (16.3%) | 20 (16.3%) |
| Other1 | 56 (20.4%) | 19 (15.4%) | 30 (24.4%) |
| Other Manager (e.g. clinic manager) | 36 (13.1%) | 20 (16.3%) | 19 (15.4%) |
| Pharmacist | 3 (1.1%) | 2 (1.6%) | 7 (5.7%) |
| Physician Assistant/Nurse Practitioner | 18 (6.5%) | 5 (4.1%) | 5 (4.1%) |
| Registered Nurse | 28 (10.2%) | 12 (9.8%) | 23 (18.7%) |
| Therapist (RT, PT, OT, speech) | 6 (2.2) | 3 (2.4%) | 1 (.8%) |
| Technologist/Technician | 3 (1.1) | 2 (1.6%) | 4 (3.2%) |
| Missing | 5 (1.8) | 3 (2.4%) | 1 (.8%) |
This category includes the positions clinical social worker, pharmacist, environmental support, and those who selected ‘other’.
Materials
Burnout (Emotional Exhaustion (EE) Sub-scale): The Maslach Burnout Inventory is considered the gold standard tool in the field of burnout, and has been used extensively with HCWs. A meta-analysis revealed that of the three sub-scales (emotional exhaustion, depersonalization, and personal accomplishment), emotional exhaustion consistently produces the largest and most consistent coefficient alpha estimates (Wheeler et al., 2011). Emotional exhaustion can also be used to discriminate between burned out and non-burned out outpatients suffering from work-related neurasthenia (according to ICD-10 criteria; Schaufeli et al., 2001). We used a 5-item derivative (Adair et al.,2018, 2020; Sexton & Adair, 2019; Sexton et al., 2018) of the original 9-item emotional exhaustion scale. Example items include ‘I feel frustrated by my job’ and ‘Events at work affect my life in an emotionally unhealthy way’. Participants responded using a 5-point scale (1 = disagree strongly; 5 = agree strongly). Each participant’s mean of the 5 items was converted to a 0–100 point scale, with higher scores representative of more severe emotional exhaustion. Internal consistency in the current study was good (α =.85).
Emotional thriving and emotional recovery
Two new positively valanced well-being domains were created as part of our NIH-funded research into measuring and reducing burnout in HCWs. The first is Emotional Thriving, which asks about the level of flourishing of a respondent (e.g. ‘I have a chance to use my strengths every day at work’) and is akin to the opposite of Emotional Exhaustion. The second is Emotional Recovery, which assesses the extent to which one is able to ‘bounce back’ from adversity or emotional upheavals (e.g. ‘My mood reliably recovers after frustrations and setbacks’). Emotional Recovery and Emotional Thriving only share about 10% of their variance so being good at recovery does not ensure thriving, and vice versa.
The psychometric validity of these scales was evaluated on over 5,000 HCWs enrolled in our interventions, and using pre-post data from Randomized Clinical Trials, we have found the scales responsive to interventions. The NHS in the UK has used Emotional Thriving (α = .86), and Emotional Recovery (α = .89), with results from over 16,000 HCWs across 75 trusts. In the current study, we also found these scales to exhibit good internal consistency (Emotional Thriving α = .84, and Emotional Recovery α = .78).
Subjective happiness
The subjective happiness scale (SHS) is a valid, psychometrically sound, and internationally used scale of global happiness (Lin et al., 2010; Lyubomirsky & Lepper, 1999). Example items include ‘In general I consider myself (1 = not a very happy person to 7 = a very happy person)’ and ‘Compared to most of my peers I consider myself (1 = less happy to 7 = more happy)’. All four items of the SHS are answered using a 7-point scale, and each participant’s responses were averaged, with higher scores representative of higher subjective happiness (Lyubomirsky & Lepper, 1999). Internal consistency in the current study was good (α = .84).
Depressive symptoms
The Center for Epidemiological Studies Depression Scale-10-item version (CES-D10) is a psychometrically sound tool for screening respondents for clinical depression (Andresen et al., 1994). All items are prefaced with, ‘during the past week, how often did this occur’ and include items such as ‘I could not “get going”‘ and ‘my sleep was restless’. Responses are answered on a 4 point scale (0 = rarely or none; 3 = all of the time). Participant’s responses are summed together to achieve a 0–30 point scale. Internal consistency in the current study was good (α = .85).
Work-life balance
Work-life balance was assessed with the climate scale (Sexton et al., 2017). Work-life balance items assess behavioral work-life infractions by asking: ‘During the past week, how often did this occur?’ Followed by phrases such as: ‘Skipped a meal; arrived home late from work’. The response scale was: Rarely or none of the time (less than 1 day); Some or a little of the time (1–2 days); Occasionally or a moderate amount of time (3–4 days); All of the time (5–7 days); and Not Applicable. Work–life climate scale scores were computed by taking the mean of the items. Internal consistency in the current study was good (α = .81).
Procedure
This was a repeated measures cohort study of a web-based 3GT intervention conducted in April 2017. Pilot testing revealed that HCWs desired more than 7 days of 3GT, often forgot to do it, and that starting on a Monday led to less attrition overall. Consequently, this modified 3GT intervention was delivered via text-messaged links and doubled the dose to 15 days. In addition, we expanded the well-being metrics previously used in 3GT studies from depression and subjective well-being to include four additional scales, and we extended the follow-up period to 12 months. Assessments were collected on day 15, and 1-month, 6-months, and 12-months post-intervention.
Participants received daily links to submit three responses to the prompts ‘What went well today?’ and ‘What was your role in making it happen?’ To increase savoring, participants could select the positive emotion that best fit how each good thing made them feel. They could also choose to share their Good Things in a daily log visible to other participants, and upon completion, were redirected to the log.
Results and discussion
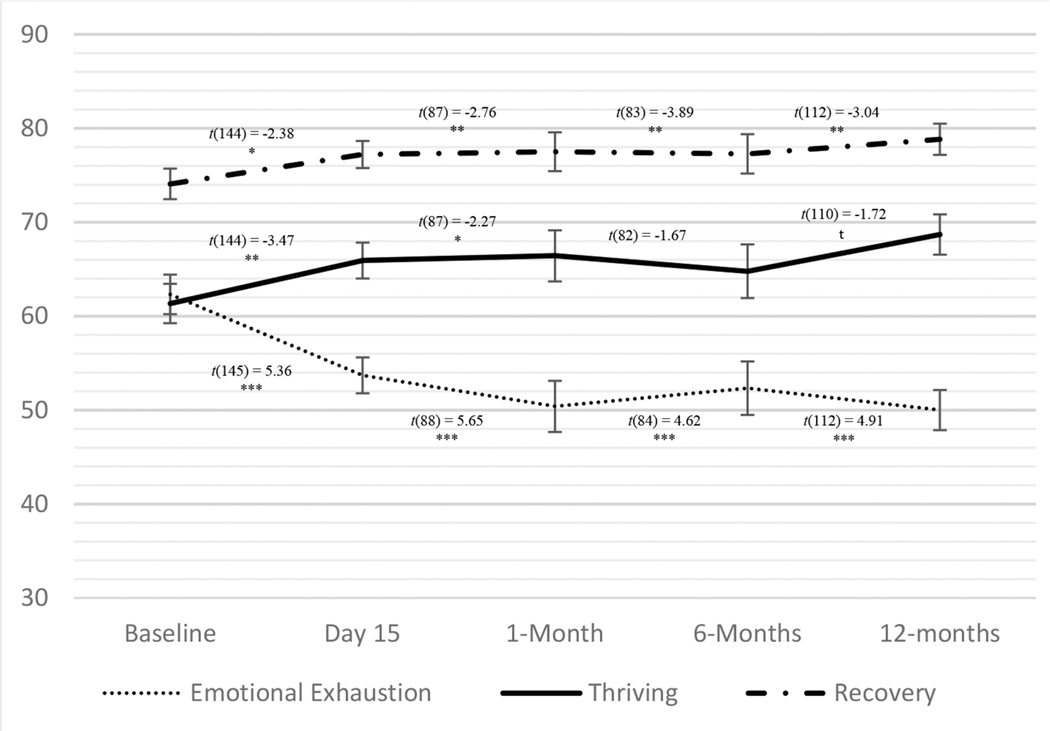
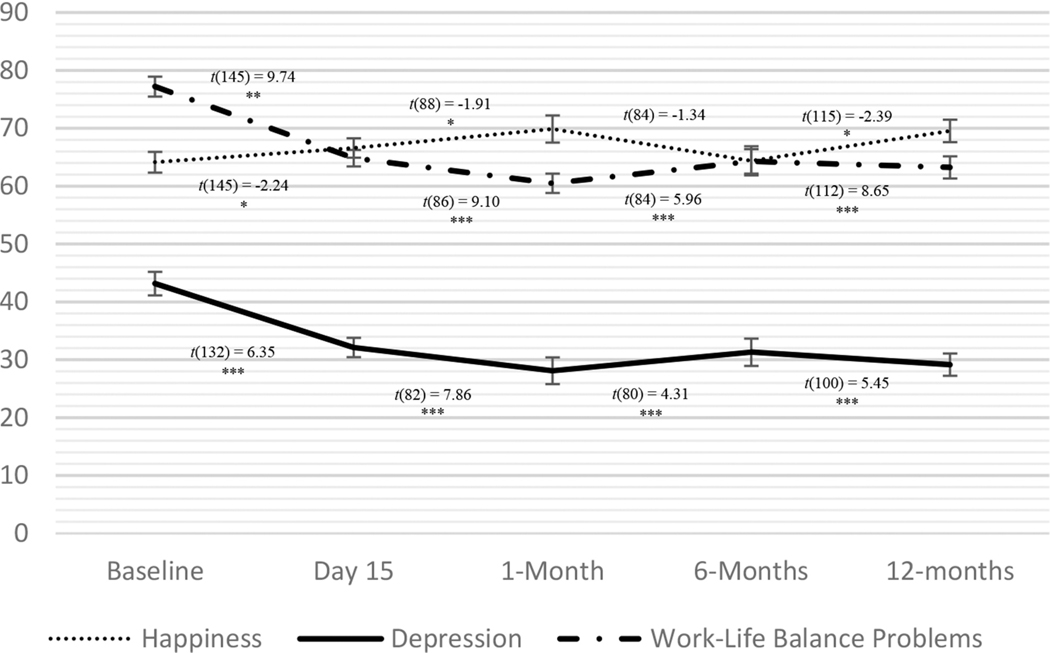
3GT participants exhibited significant improvements from baseline to day 15 across all well-being metrics using paired t-tests (see Table 2 and Figures 1 and 2). Well-being improvements endured at all follow-up time points (1 month, 6 months and 12 months) across all metrics, with two exceptions: emotional thriving did not reach statistical significance at the 6 and 12 month follow-ups (6-mo: t= −1.67, p= .10; 12-mo: t= −1.72, p= .09). Happiness at 6 months was not significantly higher than baseline (t= −1.34, p= .18), but it was at all other follow-ups. Participant evaluations of the tool were positive; see online supplemental).
Table 2.
Changes in well-being metrics across all three studies.
| Time 0 (Baseline) | Time 1 | Time 2 | Time 3 | Time 4 | |
|---|---|---|---|---|---|
| Mean (SD) | Baseline to T1: | Baseline to T2: | Baseline to T3: | Baseline to T4: | |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||
| t, df | t, df | t, df | t, df | ||
| Study 1: Three Good Things | |||||
| Emotional Exhaustion | 62.32 (25.34) | 53.71 (25.52) 5.36, 145*** | 50.40 (27.40) 5.65, 88*** | 52.34 (27.26) 4.62, 84*** | 50.01 (27.91) 4.91, 112*** |
| Subjective Happiness | 64.14 (21.61) | 66.95 (20.22) −2.24, 145* | 69.87 (21.97) −1.91, 88* | 64.39 (23.37) −1.34 84 | 69.54 (20.6) −2.39, 115* |
| Work-life Balance | 2.32 (0.62) | 1.95 (0.51) 9.74,145** | 1.81 (0.47) 9.10, 86*** | 1.93 (0.58) 5.96, 84*** | 1.9 (0.60) 8.65, 112*** |
| Depression Symptoms | 10.79 (5.87) | 8.03 (4.90) 6.35, 132*** | 7.02 (5.26) 7.86, 82*** | 7.83 (5.31) 4.31, 80*** | 7.29 (4.79) 5.45, 100*** |
| Emotional Thriving | 61.35 (25.34) | 65.93 (22.99) −3.47 144** | 66.43 (25.54) −2.27, 87 * | 64.78 (25.93) −1.67, 82 | 68.69 (22.52) −1.72, 110 |
| Emotional Recovery | 74.08 (19.69) | 77.21 (17.29) −2.38, 144* | 77.51 (19.40) −2.76, 87** | 77.28 (19.07) −3.89, 83** | 78.83 (17.64) −3.04, 112** |
| Study 2: Gratitude Letter | |||||
| Emotional Exhaustion | 61.38 (25.28) | 54.14 (26.44) 4.56, 122*** | |||
| Subjective Happiness | 65.71 (17.25) | 68.73 (17.71) −3.05, 122** | |||
| Work-life Balance | 2.33 (0.63) | 2.04 (0.59) 6.21, 121*** | |||
| Study 3: Looking Forward | |||||
| Depression Symptoms | 9.46 (5.56) | 8.31 (5.27) 2.69, 86 ** | 7.06 (6.23) 2.75, 51** | ||
| Optimism | 5.12 (1.36) | 5.11 (1.24) .11, 86 | 5.37 (1.36) −2.49, 51* | ||
| Emotional Thriving | 67.7 (26.33) | 68.90 (26.33) −.75, 85 | 72.84 (27.83) −2.20, 51* | ||
| Emotional Recovery | 72.97 (20.68) | 77.25 (18.91) −2.87, 85** | 76.60 (20.02) −2.37, 51* | ||
p < .001
p < .01
p < .05
p < .10.
Baseline Means, SDs and Ns reported are those used in the baseline to T1 paired T-tests. Assessment timing for each study were as follows: Study 11 (T1 = day 15, T2 = 1 month, T3 = 6 months, T4 = 12 months), Study 2 (T1 = 1 month), Study 3, (T1 = day 7, T2 = day 28).
Figure 1.
Study 1: Three Good Things means and standard errors for emotional exhaustion, thriving, and recovery across assessment points. *** p < .001, ** p < .01, * p < .05, t p < .10. Paired t-tests reflect changes from baseline.Displayed means at baseline reflect those from the baseline to day 15 analyses.
Figure 2.
Study 1: Three Good Things means and standard errors for happiness, depression, and work-life balance across assessment points. *** p < .001, ** p < .01, * p < .05, t p < .10. Paired t-tests reflect changes from baseline.Displayed means at baseline reflect those from the baseline to day 15 analyses.
Study 2: Gratitude letter
Study 2 tested the effects of a spending approximately 7 minutes writing a letter of gratitude on HCW well-being. Participants completed assessments and the gratitude letter intervention at baseline and the post assessment was one month later.
Method
Participants
The same recruitment and eligibility criteria from Study 1 were used in this study. HCWs (N = 123; see Table 1) initiated participation through a website link.1
Materials
Three of the measures from Study 1 were used at each time point: Emotional Exhaustion (current study α = .83; Sexton et al., 2018), Subjective Happiness (current study α = .84; Lyubomirsky & Lepper, 1999), and Work-Life Balance (current study α = .76; Sexton et al., 2017).
Procedure
Study 2 was a prospective gratitude letter intervention conducted between April, 2017 and January, 2018. Participants completed assessments and then the gratitude letter intervention at baseline and again one month later. After completing baseline assessments, participants received gratitude letter writing instructions (accompanied by a 7-minute timer), and open-ended text boxes for completing their letters (see online supplemental for letter instructions). This was repeated again at the 1-month follow-up assessments, which were collected before being presented the instructions for completing a second gratitude letter.
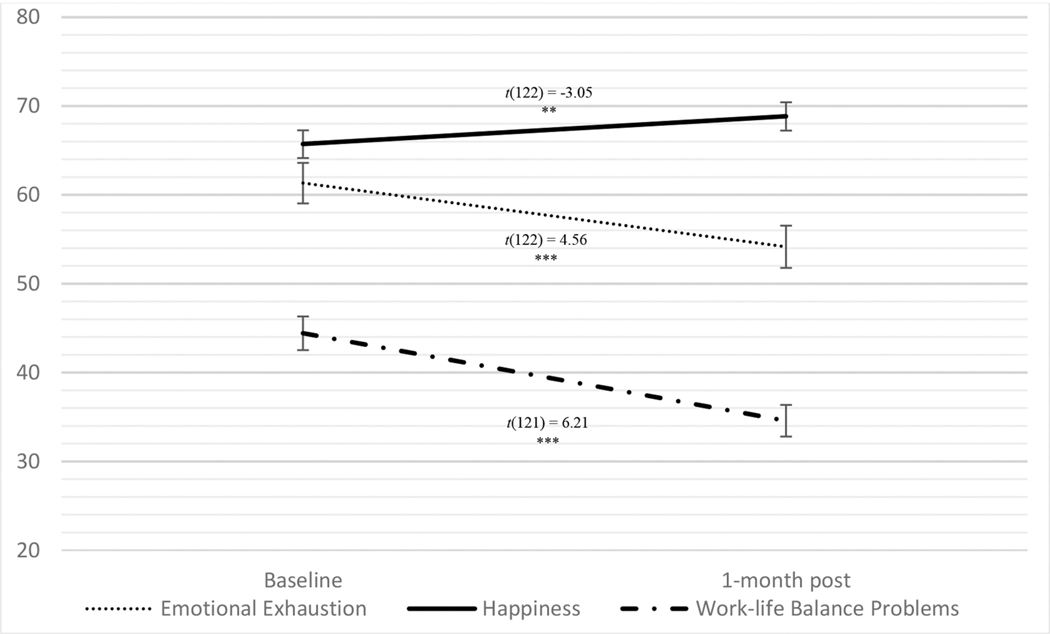
Results and discussion
Table 2 shows the means and t-test results across the sample of participants who completed the one-month follow-up. Paired t-tests demonstrated significant improvement in burnout, subjective happiness, and work-life balance from pre intervention to 1-month post (see Figure 3; see online supplemental for analyses on work-life balance items).
Figure 3.
Study 2: means and standard errors for emotional exhaustion, subjective happiness, and work-life balance across assessment points. *** p < .001, ** p < .01, Work-life Balance Problems was rescaled for the graph by subtracting 1 and multiplying by 33.33.
Study 3: Looking forward tool
Drawing upon hope theory (Snyder, 2002) and learned optimism (Seligman, 1991), Study 3 pilot tested the new ‘Looking Forward’ tool as a reflective practice to enhance well-being. This tool was designed to cultivate optimism by having participants initially reflect on positive future events far into the future, then closer to the present with subsequent exposures.
Method
Participants
The same recruitment and eligibility criteria from Study 1 were used in this study. HCWs enrolled through a website link between February and August, 2018. The sample was predominantly White (84.6%), female (88.6%), and between the ages of 31 and 60 (71.4%).2 Similar to other positive psychology interventions, participation in the Looking Forward tool generally declined over time (Day 1 (enrollment) n = 397; Day 2 (initiators) n = 123; Day 7 n = 87; Day 28 n= 52). Ninty-seven people completed 4 of the 7 activities.
Materials
Well-being metrics were collected at baseline, Day 7 and Day 28. Three metrics from Study 1 were used: Depression symptoms (current study α = .82; CES-D; Andresen et al., 1994), Emotional Thriving (current study α = .86), and Emotional Recovery (current study α = .80). This study used one new measure:
Optimism
The Life Orientation Test-Revised (LOT-R; Scheier et al., 1994) was used to measure optimism. This 10-item scale asks participants questions such as ‘In uncertain times, I usually expect the best’ and ‘I rarely count on good things happening to me’ (reverse scored). Four of the ten items are filler items and were not scored. The 1–5 response scale ranged from ‘Strongly agree’ to ‘strongly disagree’. Internal reliability in the current study was good (α = .83).
Procedure
Participants started the Looking Forward Tool upon enrollment, and then continued via automatically emailed links 1, 3, 7, 14, 21, and 28 days later. Participants were asked to describe something they hoped to experience or were looking forward to either 10, 5, 3, or 1 year(s) away, depending on the day (see online supplemental for tool instructions), and to write about thoughts and feelings associated with what they are looking forward to. Assessments were collected at baseline, day 7, and day 28.
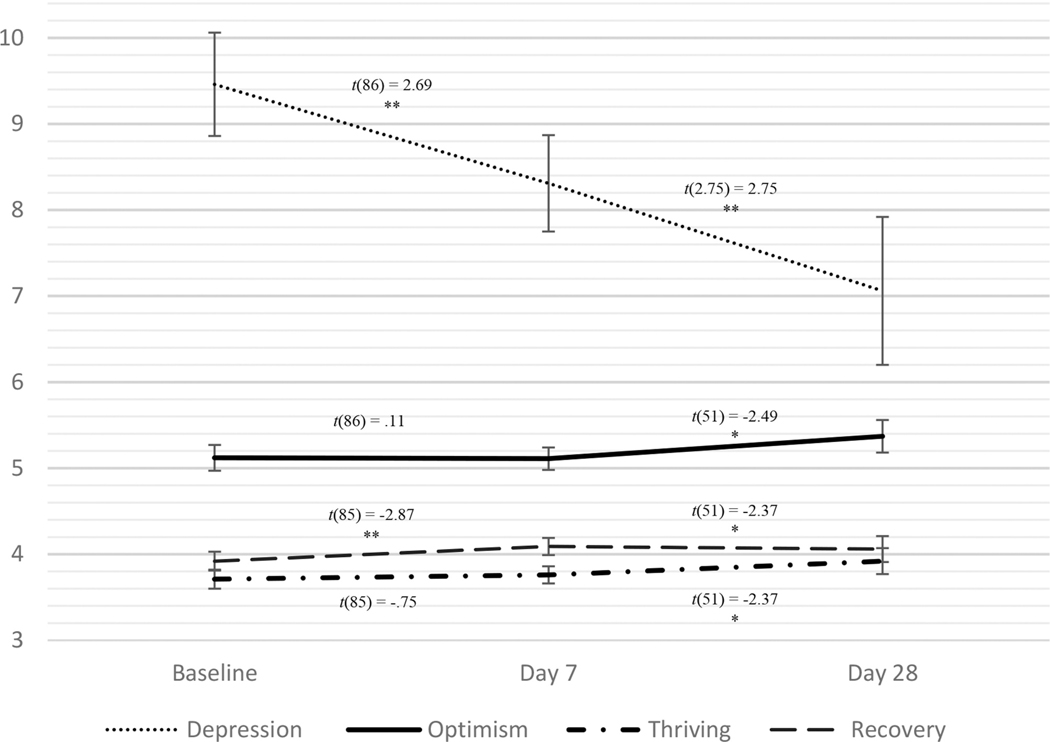
Results and discussion
Paired t-tests revealed significant improvements depression and emotional recovery between baseline and day 7; however, optimism (p = .913) and emotional thriving (p = .457) did not significantly improve between baseline and day 7 (see Table 2 and Figure 4). Participants reported significant improvement across all measures (i.e. depression symptoms, optimism, emotional thriving, and emotional recovery) between baseline and day 28.
Figure 4.
Study 3: looking forward means and standard errors for depression symptoms, optimism, thriving, and recovery across assessment points. ** p < .01, * p < .05, t p < .10. Paired t-tests reflect changes from baseline.Displayed means at baseline reflect those from the baseline to day 7 analyses.
General discussion
Positively reflecting backwards (3GT and gratitude letters) and forwards (Looking Forward Tool) with three positive psychology tools, was associated with significant improvements in a variety of well-being metrics. We found these effects to be longer lasting than previously assessed and reported (Seligman et al., 2005), with 3GT improvements detectable 12 months later. We also found that the dose of the gratitude letter (suggested 7 minutes, single exposure) could be relatively small and still confer benefits. The findings of these studies indicate that simple, brief, and uplifting web-based positive psychology tools hold promise for improving short- and long-term (up to a year later) well-being. Given the ubiquity of mobile phones, the potential to scale these types of low-cost interventions for broader use is quite high.
In all three studies, well-being was assessed with a variety of metrics: Work-Life Balance, Emotional Thriving, Emotional Recovery and Emotional Exhaustion (a key component of burnout). Emotional Thriving and Recovery are important additions to metrics of well-being because scoring below the threshold for burnout does not equate to thriving. In addition, across all three tools, ‘negative’ measures of well-being (e.g. depression) exhibited greater improvement than positive measures of well-being (e.g. subjective happiness). Furthermore, each measure performed well psychometrically and in sensitivity to detect changes over time. The responsiveness of these metrics is encouraging as we endeavor to establish a core set of well-being metrics for use across studies.
The current work has several limitations. A key limitation is the lack of randomized control groups, which would help assess causality and non-intervention related effects such as selection biases. Of note, however, is that 2 of the 3 tools (3GT and gratitude letter) did demonstrate improvements when compared to control groups in prior studies (Seligman et al., 2005). Attrition was an issue across all three tools, but this is a common if not primary barrier to evaluating web-based interventions related to health, with levels often reaching 60–80% (Eysenbach, 2005). We find there is an initial interest in well-being interventions that is often sufficient to get individuals to enroll, but that the best way to capture participation is to identify those who engage with a tool at least once beyond enrollment. Future research will investigate different methods to enhance engagement with the tools, for example, with more follow-up reminders. HCWs are often busy, tired and struggling with work-life balance, so keeping these tools simple, brief and engaging is critical to limiting attrition, and creating a better user experience for participants.
This work offers several new avenues for future research. With an expanding array of tools available, the field would benefit from identifying the best tool(s) for each participant based on their baseline measures or characteristics. An empirically-driven road map of tool use would help users maximally benefit in less time. Studies of person-activity fit indicate that participant characteristics (e.g. extraversion) predispose them to benefit more from certain tools that draw upon that characteristic (e.g. activities that involved regular social contact; Lyubomirsky et al., 2005). Future research examining the efficacy of data-driven tool selection would shed light on how to expedite tool benefits.
Future research should also investigate the most appealing and efficient ways to deliver these tools. Considering the ubiquity of mobile phones, tools delivered either via apps or links sent via text message are more likely to be used than tools delivered via email or paper and pencil workbooks. However, research to identify the best kinds of wording, images, and message-delivery options to engage the most users would be useful. In the current work, we asked some usability and engagement questions for each tool (see online supplemental), and found that participants were generally quite satisfied and engaged with all three tools studied herein. However, these questions were asked after a significant number of enrollees failed to initiate participation, leaving an understanding of why participants fail to engage with the tools unknown. Identifying methods to enhance usability and participation of online well-being tools would be a fruitful line of research for this field.
In short, brief web-based positive psychology tools can improve well-being and reduce burnout in an important population: HCWs. Given the negative downstream consequence of burnout, focusing research efforts on ways to quickly and easily facilitate positive emotional experiences in HCWs’ already busy lives, has the potential to increase their well-being, and in turn improve patient safety.
Supplementary Material
Acknowledgments
We acknowledge and thank Jon Bae, Amy Zaas, and Jochen Profit for their help in piloting the 3GT tool.
Funding
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development [R01 HD084679-01, Co-PI: Sexton and Profit].
Footnotes
Data availability
The authors will share data from the study upon reasonable request to the corresponding author.
Disclosure statement
The authors have no conflicts of interest relevant to this article to disclose.
Initiators N = 123 (reflects 15% of those who wrote an initial gratitude letter). Additional demographic information was not collected.
Race and ethnicity were not collected.
References
- Adair KC, Quow K, Frankel A, Mosca PJ, Profit J, Hadley A, Leonard M, & Bryan Sexton J. (2018). The Improvement Readiness scale of the SCORE survey: A metric to assess capacity for quality improvement in healthcare. BMC Health Services Research, 18(1), 975. 10.1186/s12913-018-3743-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adair KC, Rodriguez-Homs LG, Masoud S, Mosca PJ, & Sexton JB (2020). Gratitude at Work: Prospective Cohort Study of a Web-Based, Single-Exposure Well-Being Intervention for Health Care Workers. Journal of Medical Internet Research, 22(5), e15562. 10.2196/15562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahola K, Väänänen A, Koskinen A, Kouvonen A, & Shirom A. (2010). Burnout as a predictor of all-cause mortality among industrial employees: A 10-year prospective register-linkage study. Journal of Psychosomatic Research, 69(1), 51–57. 10.1016/j.jpsychores.2010.01.002 [DOI] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, & Silber JH (2002). Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA, 288(16), 1987–1993. 10.1001/jama.288.16.1987 [DOI] [PubMed] [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, & Patrick DL (1994). Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for epidemiologic studies depression scale). American Journal of Preventive Medicine, 10(2), 77–84. 10.1016/S0749-3797(18)30622-6 [DOI] [PubMed] [Google Scholar]
- Cimiotti JP, Aiken LH, Sloane DM, & Wu ES (2012). Nurse staffing, burnout, and health care–associated infection. American Journal of Infection Control, 40(6), 486–490. 10.1016/j.ajic.2012.02.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dugani S, Afari H, Hirschhorn LR, Ratcliffe H, Veillard J, Martin G, Lagomarsino G, Basu L, & Bitton A. (2018). Prevalence and factors associated with burnout among front-line primary health care providers in low- and middle-income countries: A systematic review. Gates Open Res. 2018;2:4. Published 2018 Jun 11. doi:10.12688/gatesopenres.12779.310.12688/gatesopenres.12779.3https://doi.org/10.12688/gatesopenres.12779.1https://doi.org/10.12688/gatesopenres.12779.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenbach G. (2005). The law of attrition. Journal of Medical Internet Research, 7(1), e11. 10.2196/jmir.7.1.e11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL (2001). The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist, 56(3), 218. 10.1037/0003-066X.56.3.218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL, Cohn MA, Coffey KA, Pek J, & Finkel SM. (2008). Open hearts build lives: Positive emotions, induced through loving-kindness meditation, build consequential personal resources. Journal of Personality and Social Psychology, 95(5), 1045–1062. 10.1037/a0013262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL, & Joiner T. (2002). Positive emotions trigger upward spirals toward emotional well-being. Psychological Science, 13(2), 172–175. 10.1111/1467-9280.00431 [DOI] [PubMed] [Google Scholar]
- Fredrickson BL, & Levenson RW (1998). Positive emotions speed recovery from the cardiovascular sequelae of negative emotions. Cognition & Emotion, 12(2), 191–220. 10.1080/026999398379718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL, Mancuso RA, Branigan C, & Tugade MM (2000). The undoing effect of positive emotions. Motivation and Emotion, 24(4), 237–258. 10.1023/A:1010796329158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gloria CT, & Steinhardt MA (2016). Relationships among positive emotions, coping, resilience and mental health. Stress and Health : Journal of the International Society for the Investigation of Stress, 32(2), 145–156. 10.1002/smi.2589 [DOI] [PubMed] [Google Scholar]
- Gong S, & Li Q. (2017). Rebuilding self-control after ego depletion: The role of positive emotions. In Proceedings of the Tenth International Conference on Management Science and Engineering Management (pp. 1401–1411). Singapore : Springer. 10.1007/978-981-10-1837-4_113 [DOI] [Google Scholar]
- Gong Z, Schooler JW, Wang Y, & Tao M. (2018). Research on the Relationship between Positive Emotions, Psychological Capital and Job Burnout in Enterprises’ Employees: Based on the Broaden-and-Build Theory of Positive Emotions. Canadian Social Science, 14(5),42–48. doi: 10.3968/10383 [DOI] [Google Scholar]
- Hall LH, Johnson J, Watt I, Tsipa A, & O’Connor DB (2016). Healthcare staff wellbeing, burnout, and patient safety: A systematic review. PloS One, 11(7), 7. 10.1371/journal.pone.0159015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedden SL, Kennet J, Lipari R, Medley G, Tice P, Copello EAP, & Kroutil LA. (2015). Key substance use and mental health indicators in the United States: Results from the 2015 national Survey on Drug Use and Health. 74. [Google Scholar]
- Kumar S. (2016). Burnout and doctors: Prevalence, prevention and intervention. Healthcare, 4(3), 37. 10.3390/healthcare4030037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J-D, Lin P-Y, & Wu C-L (2010). Wellbeing perception of institutional caregivers working for people with disabilities: Use of subjective happiness scale and satisfaction with life scale analyses. Research in Developmental Disabilities, 31(5), 1083–1090. 10.1016/j.ridd.2010.03.009 [DOI] [PubMed] [Google Scholar]
- Lyubomirsky S, & Lepper HS (1999). A measure of subjective happiness: Preliminary reliability and construct validation. Social Indicators Research, 46(2), 137–155. 10.1023/A:1006824100041 [DOI] [Google Scholar]
- Lyubomirsky S, Sheldon KM, & Schkade D. (2005). Pursuing happiness: The architecture of Sustainable change. Review of General Psychology, 9(2), 111–131. 10.1037/1089-2680.9.2.111 [DOI] [Google Scholar]
- Mata DA, Ramos MA, Bansal N, Khan R, Guille C, Angelantonio ED, & Sen S. (2015). Prevalence of depression and depressive symptoms among resident physicians: A systematic review and meta-analysis. JAMA, 314(22), 2373–2383. 10.1001/jama.2015.15845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petitta L, Jiang L, &Härtel, C. E. J. (2017). Emotional contagion and burnout among nurses and doctors: Do joy and anger from different sources of stakeholders matter? Stress and Health, 33(4), 358–369. 10.1002/smi.2724 [DOI] [PubMed] [Google Scholar]
- Poghosyan L, Clarke SP, Finlayson M, & Aiken LH (2010). Nurse burnout and quality of care: Cross-national investigation in six countries. Research in Nursing & Health, 33(4), 288–298. 10.1002/nur.20383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Profit J, Adair KC, Cui X, Mitchell B, Brandon D, Tawfik DS, Rigdon J, Gould JB, Lee HC, & Sexton JB (2018). Randomized controlled trial of the “WISER” program to reduce healthcare worker burnout. Under Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaufeli WB, Bakker AB, Hoogduin K, Schaap C, & Kladler A. (2001). On the clinical validity of the maslach burnout inventory and the burnout measure. Psychology & Health, 16(5), 565–582. 10.1080/08870440108405527 [DOI] [PubMed] [Google Scholar]
- Scheier MF, Carver CS, & Bridges MW (1994). Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the life orientation test. Journal of Personality and Social Psychology, 67(6), 1063–1078. 10.1037/0022-3514.67.6.1063 [DOI] [PubMed] [Google Scholar]
- Schwartz SP, Adair KC, Bae J, Rehder KJ, Shanafelt TD, Profit J, & Sexton JB (2019). Work-life balance behaviours cluster in work settings and relate to burnout and safety culture: A cross-sectional survey analysis. BMJ Quality & Safety, 28(2), 142–150. 10.1136/bmjqs-2018-007933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman MEP (1991). Learned optimism. Knopf [Google Scholar]
- Seligman MEP, Steen TA, Park N, & Peterson C. (2005). Positive psychology progress: Empirical validation of interventions. The American Psychologist, 60(5), 410–421. 10.1037/0003-066X.60.5.410 [DOI] [PubMed] [Google Scholar]
- Sexton JB, & Adair KC (2018). 45 Good things: a prospective pilot study of the three good things well-being intervention in the US for healthcare worker emotional exhaustion, depression, work-life balance, and happiness. BMJ Open, Under Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sexton JB, & Adair KC (2019). Forty-five good things: A prospective pilot study of the Three Good Things well-being intervention in the USA for healthcare worker emotional exhaustion, depression, work–life balance and happiness. BMJ Open, 9(3), e022695. 10.1136/bmjopen-2018-022695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sexton JB, Adair KC, Leonard MW, Frankel TC, Proulx J, Watson SR, Magnus B, Bogan B, Jamal M, Schwendimann R, & Frankel AS (2018). Providing feedback following leadership walkrounds is associated with better patient safety culture, higher employee engagement and lower burnout. BMJ Quality & Safety, 27(4), 261–270. 10.1136/bmjqs-2016-006399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sexton JB, Schwartz SP, Chadwick WA, Rehder KJ, Bae J, Bokovoy J, Doram K, Sotile W, Adair KC, & Profit J. (2017). The associations between work–life balance behaviours, teamwork climate and safety climate: Cross-sectional survey introducing the work–life climate scale, psychometric properties, benchmarking data and future directions. BMJ Quality & Safety, 26(8), 632–640. 10.1136/bmjqs-2016-006032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanafelt TD, Hasan O, Dyrbye LN, Sinsky C, Satele D, Sloan J, & West CP (2015). Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clinic Proceedings, 90(12), 1600–1613. 10.1016/j.mayocp.2015.08.023 [DOI] [PubMed] [Google Scholar]
- Shanafelt TD, West CP, Sinsky C, Trockel M, Tutty M, Satele DV, Carlasare LE, & Dyrbye LN (2019). Changes in burnout and satisfaction with work-life integration in physicians and the general US Working population between 2011 and 2017. Mayo Clinic Proceedings, 94(9), 1681–1694. 10.1016/j.mayocp.2018.10.023 [DOI] [PubMed] [Google Scholar]
- Snyder CR (2002). TARGET ARTICLE: Hope Theory: Rainbows in the Mind. Psychological Inquiry, 13(4),249–275. doi: 10.1207/S15327965PLI1304_01 [DOI] [Google Scholar]
- West CP, Dyrbye LN, Rabatin JT, Call TG, Davidson JH, Multari A, Romanski SA, Hellyer JMH, Sloan JA, & Shanafelt TD (2014). Intervention to promote physician well-being, job satisfaction, and professionalism: A randomized clinical trial. JAMA Internal Medicine, 174(4), 527–533. 10.1001/jamainternmed.2013.14387 [DOI] [PubMed] [Google Scholar]
- Wheeler DL, Vassar M, Worley JA, & Barnes LLB (2011). A reliability generalization meta-analysis of coefficient alpha for the maslach burnout inventory. Educational and Psychological Measurement, 71(1), 231–244. 10.1177/0013164410391579 [DOI] [Google Scholar]
- World Health Organization. (2017). Depression and other common mental disorders: Global health estimates (Licence: CC BY-NC-SA 3.0 IGO). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.