Abstract
The current study is a randomized controlled trial comparing HOPE (Helping to Overcome PTSD through Empowerment) to an adapted version of present-centered therapy (PCT+) in residents of domestic violence shelters with posttraumatic stress disorder from intimate partner violence. HOPE is a cognitive-behavioral treatment that adopts an empowerment approach. PCT is an attention-matched control condition frequently used in posttraumatic stress disorder treatment research. PCT+ was adapted to include safety planning. We collected data from 172 women from one of six shelters, randomizing participants to receive either HOPE or PCT+. Participants in both treatments received up to 16 sessions during shelter and the first three months post-shelter. Follow-up assessments occurred at post-shelter, post-treatment, and 6- and 12-months post-treatment. Results of multivariate models found that both HOPE and PCT+ were associated with significant and large reductions in intimate partner violence-related posttraumatic stress disorder symptoms. Further, both treatments resulted in significant small to medium effects on intimate partner violence, depression, empowerment, posttraumatic cognitions, and health-related quality of life. Results suggest that both HOPE and PCT+ are viable and efficacious treatments of intimate partner violence-related posttraumatic stress disorder in women residing in shelters. As PCT+ has the potential to be delivered by paraprofessionals and individuals without mental health expertise, PCT+ may be the preferred treatment model for shelters.
Keywords: intimate partner violence, empowerment, randomized clinical trial, cognitive behavioral therapy
Intimate partner violence (IPV) is a serious and preventable public health problem for women. The National Intimate Partner and Sexual Violence Survey found that one in three (36.4%) women experience sexual violence, physical violence, and/or stalking and over 1/3 of women (36.4%) experience psychological aggression by an intimate partner during their lifetime (Smith et al., 2018). IPV is associated with significant loss of personal and social resources (Johnson et al., 2008) and substantial economic burden and health-care costs (Bonomi et al., 2009; Peterson et al. 2018). Although the mental health sequelae of IPV are many (e.g., Hien & Ruglass, 2009; Spencer et al., 2019), posttraumatic stress disorder (PTSD) is one of the most prevalent disorders among IPV survivors with research documenting a strong association between IPV and PTSD (Hien & Ruglass, 2009; Spencer et al., 2019).
Domestic violence shelters are an important resource for IPV survivors and their children, providing safety, case management, and advocacy for residents. Over 1,800 domestic violence programs exist in the United States, with approximately 77% of those agencies providing emergency shelter to adult and child victims of IPV (National Network to End Domestic Violence [NNEDV], 2018). A 2017 survey of IPV programs found that 40,470 adult and child survivors received emergency shelter or transitional housing in a single day (NNEDV, 2018). IPV survivors who seek shelter tend to report more severe abuse histories and present with higher rates of PTSD relative to IPV survivors who do not seek shelter (Jones et al., 2001). Consistently, more recent research finds trauma symptoms like PTSD to be a significant predictor of domestic violence shelter residence (Galano, et al., 2013), and research finds an extremely high rate of IPV-related PTSD in women in shelters (66%; Perez et al., 2012). Furthermore, research suggests that the impairment associated with both IPV and PTSD can interfere with IPV survivors’ ability to effectively access and use shelter and other community resources necessary to establish safety (Johnson et al., 2008). Given these findings, therapy during the shelter should focus on maximizing use of available shelter and community resources that might be important for IPV survivors, especially those with IPV-related PTSD. Consistently, research finds that interventions offered both during and after shelter can be beneficial to women (Jonker et al., 2014). However, only 52% of the domestic violence agencies in the United States provide therapy or counseling services for survivors (NNEDV, 2018) and there are no research-supported treatments designed specifically for IPV-related PTSD in women residing in shelter.
Helping to Overcome PTSD through Empowerment (HOPE; 2009; Johnson et al., 2011, 2016) was developed to address the unique needs of IPV survivors who seek shelter. Although there are numerous research-supported treatments for PTSD (e.g., Foa et al., 2018; Forbes et al., 2012; Lang et al., 2017), none of these treatments have been evaluated in IPV survivors, generally, or in IPV survivors who seek shelter, specifically. Residents of domestic violence shelters are unique relative to other trauma survivors, in that they often face multiple safety risks and a high likelihood of re-victimization, are currently homeless and in a state of crisis, and face distinct challenges such as co-parenting with their abuser. Existing interventions for IPV survivors are in early stages of development (e.g., Kelly & Pich, 2014), do not specifically address IPV-related PTSD (e.g., Rhodes et al., 2015; Rizo et al., 2018; Santos et al., 2017), or are designed for survivors who no longer have safety concerns and have permanently left their abuser (e.g., Kubany et al., 2004). Residents of domestic violence shelters may return to their abuser, or even if they have left, still face ongoing safety concerns. Thus, treatments that assume safety do not appropriately target the needs of shelter residents.
HOPE was designed to fill this gap in the IPV treatment literature. HOPE is a short-term, present-centered, cognitive-behavioral treatment that adopts an empowerment approach. HOPE is considered a first stage treatment in that it focuses on safety, self-care, and empowerment rather than recall and processing of the trauma-related memories (Herman, 1992). A first stage treatment is well-suited to the needs of IPV survivors in shelter, as they are in a state of crisis with high risk for re-victimization. HOPE’s empowerment approach is based in multicultural feminist theory (Worell & Remer, 2002) and thus emphasizes choice, individualized goals, and self-efficacy throughout treatment. Further, HOPE provides space to investigate how the client’s cultural background and socialization as a woman influences her experience of abuse. Finally, HOPE adopts a cognitive-behavioral approach, addressing the five schematic areas hypothesized by McCann et al. (1988) to be influenced by trauma (i.e., safety, trust, power, intimacy, esteem).
HOPE was developed through a series of pilot studies that included focus groups with current and former shelter residents, an open trial (Johnson & Zlotnick, 2006), and two pilot randomized controlled trials evaluating the benefit of adding HOPE to standard shelter services (Johnson et. al., 2011, 2016). A pilot randomized clinical trial (N = 70) of an initial version of HOPE that consisted of 9–12 sessions of individual treatment during the shelter stay found that HOPE, relative to standard shelter services alone, was associated with reduced emotional numbing, effortful avoidance, and arousal symptoms of IPV-related PTSD; depression symptoms; rates of IPV re-victimization; and increased empowerment and social support (Johnson et al., 2011). Notably, most HOPE participants left shelter prior to completing HOPE and reported ongoing clinically significant PTSD symptoms, life-stressors, and IPV after leaving shelter (Johnson et al., 2011). Building on these findings, HOPE was expanded to a 16-session intervention that continued for three months after residents left shelter (Johnson et al., 2016). A pilot randomized controlled trial (N = 60) of this expanded version of HOPE found HOPE to be associated with reduced IPV-related PTSD and depression severity, as well as increased empowerment and resource gain relative to standard shelter services alone (Johnson et al., 2016).
Since these findings of HOPE were promising but preliminary, the current study evaluated the efficacy of the expanded version of HOPE (Johnson et al., 2016) relative to a time- and attention-matched control condition, over a longer period (i.e., a 12-month follow-up period), and within six diverse shelter settings rather than only one shelter. Our attention-matched control condition was present-centered therapy (PCT), a problem-focused, supportive therapy that has been frequently used as an attention-matched control condition in clinical trials of PTSD (e.g., Foa et al., 2018; Lang et al., 2017; Schnurr et al., 2007). Unlike the two pilot RCTs of HOPE that used doctoral-level psychologists to deliver HOPE, both HOPE and the attention-matched control, PCT were delivered by masters-level community-based therapists. We initially hypothesized that HOPE, relative to control, would be associated with greater reductions in IPV-related PTSD severity and degree of IPV re-victimization across the 12-month follow-up. However, given the research supporting the efficacy of PCT in the treatment of PTSD that were published after we designed and started this study (e.g., Foa et al., 2018; Lang et al., 2017) and the fact that the Society for Clinical Psychology now lists PCT on their website describing research-supported treatments for PTSD (Society for Clinical Psychology, 2020), we are now less certain of this prediction. We also assessed several secondary outcomes including depression severity, empowerment, posttraumatic cognitions, and health-related quality of life. Satisfaction with treatment, treatment attendance, and treatment drop-out rates were also evaluated.
Method
Participants
Participants were residents of one of six shelters in five counties in the midwest. To be eligible, participants had to experience an incident of IPV in the month prior to entering shelter, as defined by endorsing at least one item on either the Severity of Violence against Women Scale (SVAW; Marshall, 1992) or the short-form of the Psychological Maltreatment of Women Inventory (PMWI; Tolman, 1999). Participants also had to meet Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM-IV-TR; American Psychiatric Association [APA], 2000) diagnostic criteria for IPV-related PTSD according to the Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995). Participants were excluded from the study if they: (a) endorsed suicidal ideation with intent and plan determined to be severe risk on the Modified Scale for Suicidal Ideation (MSSI; Miller et al., 1986); (b) endorsed current psychotic symptoms on the psychotic screen of the Structured Clinical Interview for Axis I disorders (SCID-I/P; First et al., 2002); (c) met DSM-IV-TR (APA, 2000) diagnostic criteria for alcohol or drug dependence within the last three months on the SCID-I/P (First et al., 2002); (d) met DSM-IV-TR (APA, 2000) diagnostic criteria for lifetime Bipolar Disorder on the SCID-I/P (First et al., 2002); or (e) were in concurrent individual psychotherapy or counseling.
Procedure
Design
This study was a randomized double-blind clinical trial evaluating the efficacy of HOPE (n = 83) compared to present-centered therapy plus safety planning (PCT+; n = 89; discussed below) in shelter residents with IPV-related PTSD. All participants received the standard shelter services (e.g., case management, therapeutic milieu environment, educational groups) offered through their respective shelter and were randomly assigned to either HOPE or PCT+ using urn randomization (Stout et al., 1994), stratifying participants according to substance use diagnosis and medication status. For blinding purposes, all treatment offered was referred to as “HOPE.” Additionally, participants in both conditions received a “HOPE Workbook” that included all handouts for their specific treatment condition. Participants were discouraged from sharing their HOPE materials with other residents or research staff.
Data were collected between February of 2013 and February of 2017. An a priori power analysis was conducted via Optimal Design 2.0 Software (Raudenbush & Liu, 2000) with an alpha level of .05; a conservative medium effect size (delta = .60); an effect size variability of .07 across the six shelters; and a desired power of .80. Power analysis results indicated a required N of 150. All research procedures were approved by the University of Akron Institutional Review Board (IRB) and all participants provided informed consent. A Certificate of Confidentiality was also received from the National Institute of Mental Health (NIMH). Participants were recruited via several methods at each shelter, including study brochures, posted flyers, shelter-based recruitment sessions, and staff referrals. All participants who expressed interest in the study participated in a brief screen, either in person or by phone. This screen provided more details about the requirements of the study and an initial screen of inclusion criteria (e.g., whether current resident was in a participating shelter, experienced IPV in month prior to shelter, screened for substance dependence with items from the Mini-International Neuropsychiatric Interview (MINI; Sheehan et al., 1998) and screened for PTSD with brief 4-item screen for PTSD in primary care (PC-PTSD; Prin et al., 2003)).
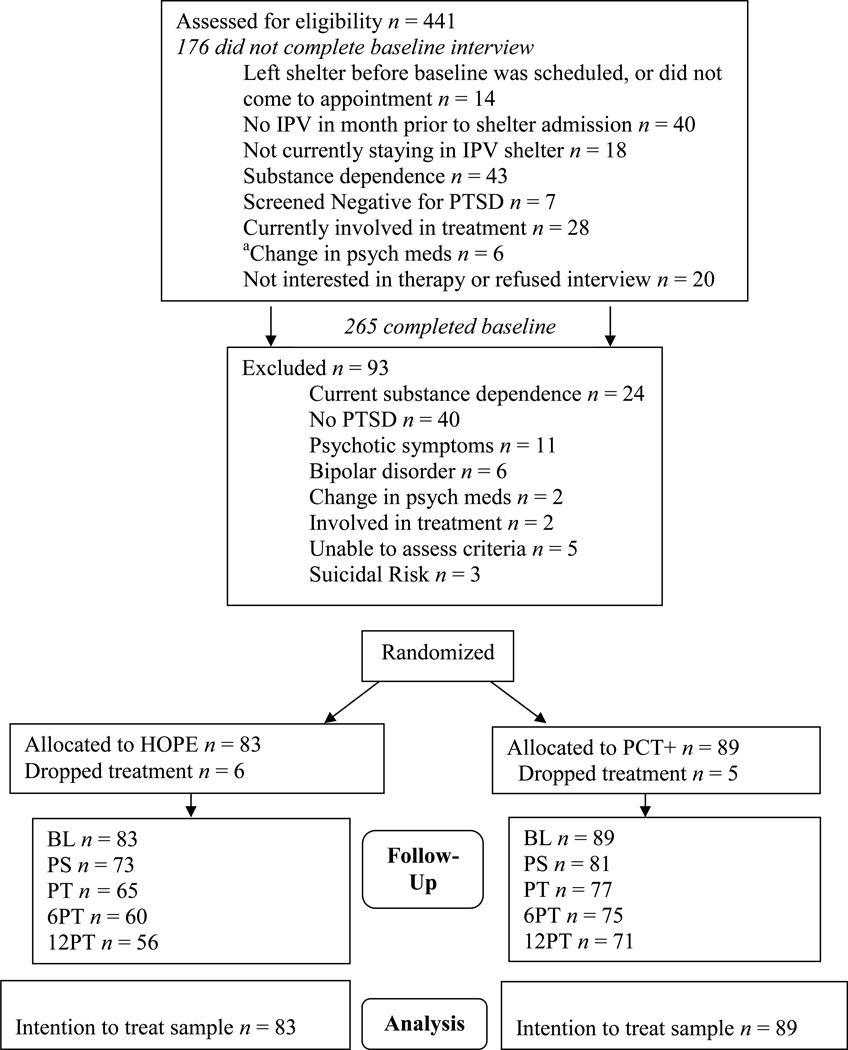
Participants who were still eligible and consented were scheduled a baseline assessment at shelter (see Figure 1). The baseline and follow-up assessments lasted approximately 2–3 hours and were conducted by advanced graduate assistants (GAs) in psychology. Interview training included standard training on interview procedures, practice with a trained interviewer, and observation of experienced staff conducting interviews. All GAs were supervised by the first author and attended weekly group supervision in which they received feedback about proper administration of assessments to minimize coder drift. To assess treatment effects, participants were reassessed by GAs, who were masked to participants’ treatment condition, within one week of leaving shelter (post-shelter; PS), within one week of completing treatment (post-treatment; PT), 6- and 12-months post-treatment (6PT and 12PT, respectively). Baseline assessments occurred in shelter; follow-up assessments occurred at the participants’ home when safe or another safe location convenient to the participant (e.g., library, coffee shop). Participants were reimbursed $40 for the baseline assessment and $50 for each follow-up assessment. Participants who completed at least 75% of study assessments were eligible for a drawing for one of two $250 gift cards. Childcare and bus passes were provided when needed. Measures suggested by Sullivan and Cain (2004) to maximize safety when conducting research with IPV survivors were used throughout the research (e.g., safety planning during interviews, providing limited details regarding participation on phone calls in case abuser is listening).
Figure 1.
CONSORT Diagram of Participant Flow through the Protocol
Note. BL = baseline; PS = post-shelter; PT=-post treatment; 6PT = 6 months post-treatment; 12PT = 12 months post-treatment.
aChange in psychotropic medications in the last month was initially an exclusion criterion. Given the high rates of medication changes observed this criterion was eliminated to maximize recruitment and generalizability.
Measures
Descriptive Variables
Table 1 provides participant descriptive information. For all measures, item-level missing data was addressed using available item analysis (Parent, 2013) providing that at least 80% of the items were completed on a given measure (Downey & King, 1998). Accordingly, total scores were created by multiplying the mean using all available items by the number of items.
Table 1.
Sample Characteristics by Treatment Group (N = 172)
| Variable | HOPE (n =83) | PCT+ (n = 89) | |||
|---|---|---|---|---|---|
| M/n | SD/% | M/n | SD/% | χ2/t(df) | |
| Age | 34.34 | 9.46 | 35.87 | 8.78 | −1.10(170)a |
| Sexual Orientation | .22(1)b | ||||
| Straight/Heterosexual | 78 | 94.0 | 82 | 92.1 | |
| Bisexual | 5 | 6.0 | 7 | 7.9 | |
| Race | 1.15(2)b | ||||
| Black/African American | 33 | 39.8% | 43 | 48.3% | |
| White | 41 | 49.4% | 39 | 43.8% | |
| Multiracial | 8 | 9.6% | 7 | 7.9% | |
| Ethnicity | .01(1)b | ||||
| Hispanic/Latina | 3 | 3.6% | 3 | 3.4% | |
| Not Hispanic/Latina | 79 | 95.2% | 86 | 96.6% | |
| Highest Education Obtained | 3.65(4)b | ||||
| Completed Junior High School | 3 | 3.6% | 3 | 3.4% | |
| Completed some High School | 21 | 25.3% | 21 | 23.6% | |
| Completed High school/GED | 24 | 28.9% | 25 | 28.1% | |
| Completed some college | 32 | 38.6% | 30 | 33.7% | |
| Graduated from college | 3 | 3.6% | 10 | 11.2% | |
| Receiving public assistance | 74 | 89.2% | 68 | 76.4% | 4.85(1)b |
| Employed | 13 | 15.7% | 11 | 12.4% | .39(1)b |
| Have children | 75 | 90.4% | 83 | 93.3% | .48(1)b |
| Cohabitated with abusive partner | 68 | 81.9% | 78 | 87.6% | 1.09(1)b |
| Have restraining order | 28 | 33.7% | 28 | 31.5% | .10(1)b |
| Current Comorbid Psychiatric Disorders | |||||
| Major Depression | 48 | 57.8% | 49 | 55.1% | .14(1)b |
| Anxiety Disorder other than PTSD | 20 | 24.1% | 24 | 27.0% | .19(1)b |
| Borderline Personality Disorder | 14 | 16.9% | 10 | 11.2% | 1.13(1)b |
| Lifetime psychotropic medication use | 45 | 54.2% | 44 | 50.0% | .30(1)b |
| IPV in month prior to shelter | |||||
| Psychological | 80 | 96.4% | 88 | 98.9% | 1.17(1)b |
| Physical | 77 | 92.8% | 82 | 92.1% | .03(1)b |
| Sexual | 53 | 63.8% | 55 | 62.5% | .03(1)b |
| Prior lifetime IPV | 55 | 66.3% | 61 | 68.5% | .10(1)b |
| Number of types of prior lifetime trauma other than index IPV | 3.48 | 2.06 | 3.61 | 2.24 | −.40(169)a |
| Days in shelter at baseline | 18.69 | 25.85 | 19.01 | 19.59 | −.09(170)a |
| Length of shelter stay (days) | 68.92 | 49.84 | 76.39 | 75.22 | −.73(138.20)a |
Note. Values are either reported as M, SD, with differences assessed using t-test (denoted by a, with denominator degrees of freedom in parentheses), or n, %, with differences assessed using χ2 (denoted by b, with numerator degrees of freedom in parentheses).
There were no significant differences by treatment condition at the p < .01 level, chosen to address the potential for family-wise error.
Major Depression and Anxiety Disorder other than PTSD were measured with the SCID-I/P. Borderline Personality was assessed with the SCID II. Psychological IPV was measured with the PMWI. Physical and sexual IPV were measured with the SVAW. Number of types of prior lifetime trauma other than index IPV was measured with the TSS.
Demographic Interview.
A semi-structured interview was conducted to acquire participant demographic and other descriptive information.
Treatment Utilization.
A modified version of the Longitudinal Interval Follow-up Evaluation (LIFE; Keller et al., 1987) was used to assess treatment utilization across the lifetime, as well as the six months prior to baseline interview.
Trauma History.
The Traumatic Stress Schedule (TSS; Norris, 1990) was utilized to assess participants’ lifetime history of traumatic events distinct from their experience of IPV. The TSS includes 10 items of traumatic events (e.g., being attacked, sexual violence,). Participants endorse whether a traumatic event occurred or not for each item. In the present study, a count variable was created to represent the number of types of traumatic events participants had experienced, with possible scores ranging from 0–10.
Comorbidity.
The mood, anxiety (excluding PTSD), substance and psychotic screen modules of the Structured Clinical Interview for DSM-IV-TR (APA, 2000) Axis I (SCID-I/P; First et al., 2002) and the Borderline Personality Disorder module of the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II, First et al., 1997) were utilized to assess for diagnostic comorbidity with PTSD. The SCID-I/P and SCID-II are the gold standard semi-structured clinical interviews for disorders based on DSM-IV-TR symptom criteria. Inter-rater reliability was calculated for 13 randomly selected interviews for MDD (κ = 1).
Primary Outcomes
PTSD.
The Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995) is a structured interview that assesses the DSM-IV-TR (APA, 2000) criteria for PTSD and PTSD symptom severity over the last month. The frequency and intensity of each symptom was assessed on a 5-point Likert scale (0 = never to 4 = daily or almost every day; 0 = absent to 4 = extreme, respectively) for IPV-related PTSD symptoms in the past month. The present study summed frequency and severity items across the 17 symptoms to reflect IPV-related PTSD severity in the last month. Total CAPS scores can be classified as asymptomatic/few symptoms (0–19), mild/subthreshold PTSD (20–39), moderate PTSD/threshold (40–59), severe PTSD (60–79), and extreme PTSD symptoms (≥ 80; Weathers et al., 2001). We also used the CAPS to determine if participants met DSM-IV-TR (APA, 2000) criteria for IPV-related PTSD at baseline and follow-up. A PTSD symptom was considered present if the frequency was rated “1” or higher and the intensity was rated “2” or higher (Weathers et al., 1999). Sample CAPS items include, “In the last week, have you had unwanted memories of the abuse?” and “Have you ever tried to avoid thoughts or feelings about the abuse?” The CAPS has demonstrated internal consistency reliability coefficients ranging from .73–.85 and concurrent validity with other measures of PTSD (Blake et al., 1995), as well as convergent and discriminant validity across 10 years of research (Weathers et al., 2001). Total CAPS scores for this study demonstrated internal consistency of .91. Inter-rater reliability for IPV-related PTSD diagnosis from the CAPS was also calculated for 20 randomly selected interviews (κ = 1).
IPV Severity.
The Severity of Violence Against Women Scale (SVAW; Marshall, 1992) and the Psychological Maltreatment of Women Inventory-Short Version (PMWI-SF; Tolman, 1999) were utilized to assess for IPV. The SVAW is a 46-item self-report measure that assesses for the frequency of serious threats of violence; mild, minor, moderate, and serious violence; and sexual aggression. In the present study, the SVAW was used to assess IPV at baseline (i.e., IPV in the month prior to shelter admission) and as a primary outcome variable (i.e., past month IPV severity). Sample items include: “acted like a bully towards you” and “threatened to kill you.” The SVAW is scored on a 4-item Likert scale ranging from 0 (never) to 3 (4 or more times) and items were summed to reflect an overall severity score. Marshall (1992) report internal consistency reliability α’s between .89-.96 and the present study was similar (α = .96).
The PMWI-SF is a 14-item self-report measure assessing for psychological violence. The PMWI-SF was used to assess IPV inclusion criteria (i.e., IPV in the month prior to shelter admission) and as a primary outcome variable (i.e., past month IPV severity). Sample items include: “My partner called me names” and “My partner treated me like an inferior.” It is scored on a 6-point Likert scale (0 = never to 4 = very frequently) and the items were summed to compute a severity score. Tolman (1999) reported internal consistency reliability for the PMWI-SF ranging from.88-.92, and this study found the similar reliability (α = .90).
Secondary Outcomes
Depression Severity.
The Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977) was used to assess severity of depression symptoms. The CES-D is a 20-item self-report measure of depression symptoms in the past week. Sample items include: “I was bothered by things that usually don’t bother me” and “I did not feel like eating; my appetite was poor.” It is scored on a 4-point Likert scale ranging from 0 (rarely or none of the time [less than 1 day]) to 3 (most of the time [5 – 7 days]). Items were summed to calculate a total severity score. A CES-D cutoff score of 16 is suggestive of significant depression symptoms and has been found to have good sensitivity and specificity (Lewinsohn et al., 1997). The CES-D has demonstrated internal consistency reliability coefficient alphas between .85 and .90 in community and patient samples (Radloff, 1977), as well as in the current study (α = .90).
Empowerment.
The Personal Progress Scale-Revised (PPS-R; Johnson et al., 2005) was utilized to measure empowerment. The PPS-R is a 28-item self-report measure and sample items include: “I feel I give as much as I get in relationships with important others in my life” and “I feel prepared to deal with the discrimination I experience in today’s society.” The PPS-R is scored on a 7-point Likert scale ranging from 1 (almost never) to 7 (almost always). The items were summed to calculate a total score. Reliability (α = .88), validity (r’s ranging from .65-.81 with measures of wellbeing), and discriminant validity (with significant differences in PPS-R total scores found in IPV survivors with and without PTSD symptoms) have been supported in previous research with the PPS-R (Johnson et al., 2005). The present study found internal consistency reliability of .86.
Posttraumatic Cognitions.
The Posttraumatic Cognitions Inventory (PTCI; Foa et al., 1999) was utilized to assess posttraumatic thoughts and beliefs about the world and self. The PTCI is a 33-item self-report measure. Sample items include: “I can’t trust that I will do the right thing” and “People can’t be trusted.” The PTCI is scored on a Likert scale ranging from 1 (totally disagree) to 7 (totally agree). In the present study, items were summed to calculate a total score. Foa et al. (1999) found an internal consistency reliability of .97), and demonstrated convergent validity relative to two other scales that measured trauma cognitions, as well as, discriminant validity. In the present study, internal consistency of .95 was identified.
Health-Related Quality of Life.
The mental component score (MCS) from the Veteran’s Rand 12-item Health Survey (VR-12; Kazis et al., 2004) was used to assess health-related quality of life. The VR-12 is a modification of the Medical Outcomes Study Short Form Health Survey (SF-12) and assesses role limitations from mental or physical health, physical functioning, bodily pain, energy/fatigue, mental health, social functioning, and general health. The MCS uses a T-score metric, with responses to all 12 items used in the calculation of the MCS and item weights accounting for the relative strength of items. Ware et al. (1996) demonstrated 2-week test-retest reliability for the MCS (r = .76) and validity when compared to the MCS from the original 36-item version of the scale. Change of 1–2 units or greater in MCS scores are considered clinically significant (Kazis et al., 2004).
Satisfaction with Treatment.
The Client Satisfaction Questionnaire (CSQ-8; Attkisson & Greenfield, 2004) is an 8-item self-report measure of level of satisfaction with care (e.g., quality of service, convenience) The CSQ-8 is scored on a Likert scale ranging from 1 (low satisfaction) to 4 (high satisfaction). Scores are summed to calculate a total treatment satisfaction score. The CSQ-8 has previously demonstrated internal consistency in a variety of studies with alphas ranging from .83 to .93. Predictive validity has been supported by service completers demonstrating higher satisfaction scores compared to non-service completers. The present study found an internal consistency of .85.
Treatment Protocols, Integrity, and Training
Therapists, Therapist Training, and Supervision.
Both HOPE and PCT+ were delivered by four masters-level therapists, each of whom was trained in both therapy protocols. Training for both HOPE and PCT+ each included a two-day workshop led by the first author and developer of HOPE. The training for PCT+ was adapted from an existing training program for PCT with the assistance of a consultant who has supervised delivery of PCT in prior research (Schnurr et al., 2007). Each therapist had two practice clients (i.e., one HOPE, one PCT+) under weekly supervision with the first author and was assigned therapy clients in the RCT after they were rated as adherent and competent in both protocols. Throughout the RCT, therapists received both individual and group supervision by the first author. Therapists were regularly provided feedback on adherent and competent delivery of both protocols. Individual supervision was titrated, in that as therapists gained more experience with both protocols, less supervision was provided. Group supervision occurred weekly and focused on oversight of research procedures and documentation (i.e., notes, adverse events, and scheduling of assessments), although time was allotted for discussion of client concerns if needed.
Session Delivery Model for HOPE and PCT+.
Delivery of both HOPE and PCT+ was consistent with the model of HOPE (Johnson et al., 2016), where PCT+ was adapted to mirror HOPE’s delivery model. This model attempts to standardize the treatment procedures given the unpredictability and diversity of participants’ length of shelter stay. Participants could receive up to 16 sessions of therapy, some of which occurred in shelter and the remainder of which took place in the first three months after leaving shelter. Specifically, participants could receive up to 10 sessions while residing in shelter, over a 10-week period. In this case, the remaining six sessions would occur in the three months after leaving shelter. However, the specific breakdown of sessions received in shelter and post-shelter was determined by participants’ length of shelter stay. If participants stayed in shelter longer than the 10-week treatment period, they were offered monthly shelter booster sessions until they left shelter. We felt it unethical to discontinue therapy during this time, given that study participants were not permitted to receive other therapy or counseling during the study. These booster sessions did not provide any new information and were designed primarily as check-ins, to assure participant safety, and to work through any ongoing concerns. Only a small minority of participants (n = 11) received any booster sessions while in shelter. All sessions were 50–60 minutes in length. Sessions during shelter were offered at least weekly and sessions post-shelter were offered at least bi-weekly. Sessions occurred in private rooms in shelter or in a private, safe location chosen by the participant (e.g., participant’s home, community room in public library) when conducted post shelter.
HOPE.
The protocol of HOPE has been detailed elsewhere (Johnson et al., 2017), including two case examples (Johnson & Ceroni, 2020; Johnson et al., 2020). HOPE is a flexible module-based treatment where the ordering of the modules and the emphasis placed on each module are determined by client goals and needs. HOPE is trauma-focused in that clients relate their current symptoms and traumas to their experience of IPV but there is no processing of trauma-related memories. Treatment modules focus on (a) establishing safety and providing information and skills that enhance empowerment; (b) CBT skills, including cognitive restructuring, managing triggers, sleep hygiene, and self-soothing and relaxation; (c) improving relationships, assertiveness, and anger management; and (d) post-shelter concerns, such as goal setting and safety planning. There are also several optional modules that can be integrated into the treatment plan based on client need (e.g., crisis management, comorbid substance use).
To assess adherent and competent delivery of HOPE, 34 randomly selected sessions were rated by one of two external experts trained in HOPE. All sessions were rated on the HOPE Adherence and Competence Scale used in prior research (Johnson et al., 2016). On 5-point scales, mean overall adherence was rated as 4.32 (SD = 0.84) and overall competence was rated as 4.18 (SD = 0.94) reflecting “very good” adherence and competence.
PCT+.
PCT was designed to control for the non-specific factors of therapy (e.g., therapeutic relationship) and mirror traditional supportive therapy. The critical difference between HOPE and PCT is the focus on trauma. PCT does not include disclosure, discussion, or exposure of individual traumatic events. Further, PCT does not include any of the hypothesized active ingredients of HOPE (e.g., cognitive-restructuring, acquisition of new behavioral skills, including skills that enhance empowerment). The PCT manual used in prior research (Schnurr et al., 2007) was adapted for our target population to include safety-planning strategies when participants brought up safety concerns to their therapist (i.e., PCT+). Session 1 of PCT+ focused on collecting the client’s history and providing an overview of the therapy. Session 2 focused on psychoeducation about common reactions to trauma and PTSD and introduced participants to the daily monitoring log participants were asked to complete regarding activities or events that were stressful. Sessions 3–15 focused on problem-solving around current difficulties identified in the daily log. Participants prioritized and chose what events they wished to work on each session. Participants who referred to past trauma or IPV were validated and redirected to focus on current concerns. Session 16 focused on reviewing the participant’s progress and termination.
To assess adherent and competent delivery of PCT+, 24 randomly selected sessions were rated by one of two external experts trained in PCT+. Sessions were rated on an adapted version of the PCT adherence scales (Schnurr et al., 2007). On 7-point scales, mean overall adherence of PCT+ essential elements was 5.78 (SD = 0.75) and overall competence was rated as 5.80 (SD = 0.72) reflecting “good” to “very good” adherence and competence.
Statistical Methods
Our primary question regarding the extent to which the HOPE and PCT+ groups differed in improvement after baseline was addressed using group to predict the five occasions (BL, PS, PT, 6PT, and 12 PT) simultaneously; each outcome was predicted in a separate model. Although conceptually similar to a split-plot analysis of variance (i.e., with between-groups treatment and within-subjects occasions), these multivariate models reflect an intent-to-treat approach by using all available cases assuming missing at random. Because marginal main effects of group and occasion were not of interest, we report only planned contrasts regarding group-specific change.
Additional model modifications were needed to account for heterogeneity of variance and the different types of outcomes. For the five outcomes with plausibly normal residuals (PTSD, depression, empowerment, posttraumatic cognitions, and health-related quality of life), residual maximum likelihood in SAS GLIMMIX was used to estimate models with a multivariate normal distribution; all variances and covariances were estimated separately by group and occasion (due to worse fit for homogeneous-variance models; see Hoffman, 2015). For the two symptom-count IPV outcomes with positive skewness, the models specified a log link function to ensure positive predicted outcomes along with a negative binomial conditional distribution. To be able to include separate scale factors for over-dispersion by group and occasion (as also found necessary by comparisons of fit), these models were estimated in Mplus v. 8.4. A random intercept captured covariance among the five occasions (whose variance was constrained to be equal across groups given nonconvergence otherwise), requiring marginal maximum likelihood estimation. Attempts to also include zero-inflation components resulted in non-positive-definite models, indicating the model adequately captured the zero-inflation. Robust standard errors were used in all models to protect the fixed effect standard errors against distribution misfit. For comparability across model type, denominator degrees of freedom were approximated with the number of subjects for all comparisons. Given the number of comparisons to be examined, an alpha < .01 was used. Additional details and annotated model syntax are available in the online supplement.
In preliminary analyses, we first examined the possibility of dependency arising from shelter or therapist. No omnibus main effects, interactions with time, or interactions with group were significant, and thus, effects of shelter or therapist were not retained. The results reported below are organized as follows. We first report bivariate associations involving treatment group, followed by the multivariate model results. We then report Pearson chi-square tests to evaluate significant differences between treatment groups in PTSD diagnostic status at each follow-up occasion. Finally, we used Jacobson and Truax’s (1991) approach to determine the change in CAPS score required for clinically reliable change in PTSD symptoms. Pearson chi-square tests were used to assess differences between treatment groups in the percentage of participants who experienced clinically reliable change at each follow-up occasion.
Results
Study Sample
A total of 172 women met study criteria, consented to treatment, and were randomized into the study. The majority identified as either White (46.5%) or Black/African American (44.2%) and ranged in age from 19 to 59 (M = 35.13, SD = 9.12). For sample demographics by treatment group, see Table 1. The women were sampled from a total of six shelters, with the majority of women recruited from the four larger shelters (i.e., two urban [n = 95] and two rural [n = 57] shelters) and the remaining women recruited from two smaller, rural shelters (n = 20).
Treatment Attendance and Study Retention
Participants in HOPE attended 0–16 sessions (M = 8.86, SD = 6.17). Most sessions were attended post-shelter (M = 5.36, SD = 5.44) rather than during shelter (M = 3.49, SD = 2.94), with 92.8% of participants attending at least one session of therapy and 44.2% receiving at least eight sessions (i.e., 50% of available sessions). Similarly, participants in PCT+ attended 0–16 sessions (M = 10.06, SD = 5.82). Most sessions were attended post-shelter (M = 6.51, SD = 5.08) rather than during shelter (M = 3.54, SD = 3.11), with 92.1% attending at least one session and 55.8% attending at least eight sessions of therapy. No significant differences were found between the number of total sessions, shelter sessions, or post-shelter sessions or in the percentage of participants who received at least eight sessions as a function of treatment condition (all p’s > .05). A total of 11 participants dropped out of treatment, six (7.2%) in HOPE and five (5.6%) in PCT. No significant difference was found between HOPE and PCT+ in the number of participants who dropped treatment, X2 (1) = 0.19, p = .666.
Figure 1 depicts the flow of participants throughout the study. Retention rates for study participants at each occasion are as follows (see Figure 1 for retention for each time-point by treatment): 89.5% at PS (n = 154), 82.6% at PT (n = 142), 78.5% at 6PT (n = 135) and 73.8% at 12PT (n = 127). No significant differences were found between participants who completed all assessments relative to those who missed at least one assessment on demographic variables (all p’s > .05), with the exception of race where a greater proportion of Black participants (81.6%) completed all assessments than their White counterparts (62.5%), X2(1) = 7.01, p = .008.
Client Satisfaction, Participant Safety, and Removal from Treatment
Average satisfaction scores on the CSQ-8 were calculated post-treatment for HOPE participants (n = 65) and PCT+ participants (n = 77). Average ratings for both HOPE (M = 3.67, SD = 0.40) and PCT+ (M = 3.60, SD = 0.52) were high, reflecting overall satisfaction as good to excellent for both treatments. No significant differences were found in HOPE and PCT+ satisfaction ratings, t(140) = 0.94, p = .351.
There were no study-related serious adverse events. Ten participants (6 HOPE and 4 PCT+) were removed from treatment because they were determined to need a higher level of care or different treatment. Consistent with our intent-to-treatment analytic strategy, participants removed from treatment were invited to complete all follow-up assessments. The number of participants removed from treatment in HOPE and PCT+ did not significantly differ, X2 (1) = 0.59, p = .444.
Multivariate Modeling Results
Table 2 provides the model-estimated means per group and occasion (a derivation of how these were obtained from each model is given in the online supplement, along with program syntax). These model-estimated means reflect the values most likely to have been obtained had the sample been complete; actual sample sizes are also provided. The two IPV outcome means are unit-specific (i.e., specific to a participant with a random intercept = 0). Full results for all model parameters are available in the online supplement. Table 3 provides standardized mean differences between occasions in traditional d-units, although given the heterogeneous variance, these d-values were calculated using the model t-value and degrees of freedom (DF) as follows: d = 2t / SQRT[DF] (Friedman, 1982). The limits of the 95% confidence interval (CI) for each d-value were then calculated by replacing the point estimate for the mean difference with the lower and upper bounds of its 95% CI and using the corresponding t-values to compute d-values.
Table 2.
Model-Estimated Means, Standard Error of the Mean (SEM), and Actual Sample Size (n) for Primary and Secondary Outcomes by Occasion and Treatment Group.
| Outcome | Group | Baseline | Post-Shelter | Post-Treatment | 6mo Post-Treatment | 12mo Post-Treatment | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SEM | n | Mean | SEM | n | Mean | SEM | n | Mean | SEM | n | Mean | SEM | n | ||
| Posttraumatic Stress Disorder | PCT+ | 77.82 | 2.23 | 89 | 52.82 | 3.07 | 81 | 34.37 | 3.22 | 77 | 31.84 | 3.00 | 75 | 29.05 | 3.22 | 71 |
| HOPE | 72.11 | 2.28 | 83 | 49.69 | 3.13 | 73 | 31.58 | 2.75 | 65 | 31.07 | 3.52 | 60 | 27.70 | 3.07 | 56 | |
| Severity of Violence Against Women ^ | PCT+ | 65.42 | 3.58 | 89 | 12.48 | 3.02 | 80 | 1.17 | 0.44 | 76 | 2.65 | 0.94 | 75 | 3.75 | 1.50 | 71 |
| HOPE | 64.83 | 3.76 | 83 | 8.04 | 2.20 | 72 | 3.06 | 1.01 | 65 | 4.70 | 2.11 | 60 | 2.27 | 1.17 | 56 | |
| Psychological Maltreatment of Women ^ | PCT+ | 42.01 | 1.48 | 89 | 11.87 | 1.92 | 80 | 4.26 | 1.11 | 77 | 5.08 | 1.19 | 75 | 6.57 | 1.45 | 71 |
| HOPE | 42.82 | 1.50 | 83 | 10.50 | 1.80 | 72 | 6.79 | 1.42 | 65 | 6.15 | 1.62 | 60 | 5.61 | 1.69 | 56 | |
| Depression | PCT+ | 31.01 | 1.31 | 86 | 23.78 | 1.36 | 80 | 18.63 | 1.45 | 76 | 17.91 | 1.44 | 74 | 16.79 | 1.52 | 70 |
| HOPE | 31.52 | 1.38 | 81 | 21.31 | 1.53 | 70 | 18.19 | 1.58 | 65 | 19.38 | 1.66 | 59 | 18.28 | 1.69 | 56 | |
| Empowerment | PCT+ | 129.26 | 2.80 | 87 | 136.95 | 2.85 | 79 | 142.18 | 3.07 | 77 | 140.96 | 3.08 | 75 | 145.27 | 3.14 | 70 |
| HOPE | 130.66 | 2.99 | 80 | 140.46 | 2.89 | 70 | 143.92 | 3.16 | 65 | 143.96 | 3.43 | 59 | 139.61 | 3.41 | 55 | |
| Posttraumatic Cognitions | PCT+ | 110.05 | 4.16 | 87 | 93.43 | 4.34 | 80 | 85.77 | 3.91 | 77 | 93.29 | 4.89 | 75 | 85.89 | 4.71 | 70 |
| HOPE | 112.13 | 4.66 | 83 | 92.86 | 4.80 | 71 | 78.12 | 5.08 | 65 | 83.85 | 5.46 | 60 | 83.59 | 5.38 | 56 | |
| Health-Related Quality of Life | PCT+ | 34.61 | 0.86 | 84 | 37.95 | 1.06 | 78 | 39.90 | 1.04 | 76 | 40.84 | 1.20 | 75 | 41.94 | 1.08 | 70 |
| HOPE | 34.56 | 1.03 | 77 | 41.06 | 1.06 | 72 | 42.35 | 1.14 | 64 | 42.78 | 1.31 | 60 | 39.64 | 1.36 | 56 | |
Note.
Indicates data-scale predicted unit-specific outcomes using an inverse log link function. For Empowerment and Health-Related Quality of Life, higher scores indicate better outcomes; otherwise, lower scores indicate better outcomes.
Table 3.
Model-Derived Standardized Mean Difference Effect Sizes for the Changes over Time for Primary and Secondary Outcomes by Treatment Group.
| Outcome | Group | Baseline to Post-Shelter | Baseline to Post-Treatment | Baseline to 6mo Post-Treatment | Baseline to 12mo Post-Treatment | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Est | LCL | UCL | Est | LCL | UCL | Est | LCL | UCL | Est | LCL | UCL | ||
| Posttraumatic Stress Disorder | PCT+ | −1.50 | −1.80 | −1.20 | −2.03 | −2.33 | −1.74 | −2.41 | −2.71 | −2.11 | −2.27 | −2.57 | −1.97 |
| HOPE | −1.15 | −1.45 | −0.85 | −2.06 | −2.36 | −1.76 | −1.73 | −2.03 | −1.43 | −2.11 | −2.41 | −1.81 | |
| Severity of Violence Against Women | PCT+ | −1.07 | −1.37 | −0.77 | −1.62 | −1.92 | −1.32 | −1.34 | −1.64 | −1.04 | −1.08 | −1.38 | −0.78 |
| HOPE | −1.19 | −1.49 | −0.89 | −1.38 | −1.68 | −1.08 | −0.90 | −1.20 | −0.60 | −0.98 | −1.28 | −0.68 | |
| Psychological Maltreatment of Women | PCT+ | −1.20 | −1.49 | −0.90 | −1.33 | −1.63 | −1.03 | −1.35 | −1.65 | −1.05 | −1.27 | −1.57 | −0.98 |
| HOPE | −1.24 | −1.54 | −0.94 | −1.32 | −1.62 | −1.02 | −1.12 | −1.42 | −0.83 | −1.02 | −1.32 | −0.72 | |
| Depression | PCT+ | −0.89 | −1.19 | −0.59 | −1.25 | −1.55 | −0.95 | −1.26 | −1.56 | −0.96 | −1.25 | −1.55 | −0.95 |
| HOPE | −0.94 | −1.24 | −0.64 | −1.14 | −1.44 | −0.84 | −0.97 | −1.27 | −0.68 | −1.06 | −1.36 | −0.76 | |
| Empowerment | PCT+ | 0.65 | 0.35 | 0.95 | 0.66 | 0.36 | 0.96 | 0.61 | 0.31 | 0.91 | 0.73 | 0.43 | 1.03 |
| HOPE | 0.50 | 0.20 | 0.80 | 0.64 | 0.35 | 0.94 | 0.60 | 0.30 | 0.90 | 0.40 | 0.10 | 0.70 | |
| Posttraumatic Cognitions | PCT+ | −0.61 | −0.91 | −0.31 | −0.87 | −1.17 | −0.57 | −0.55 | −0.85 | −0.25 | −0.73 | −1.03 | −0.43 |
| HOPE | −0.72 | −1.02 | −0.42 | −0.97 | −1.27 | −0.67 | −0.71 | −1.01 | −0.41 | −0.78 | −1.08 | −0.48 | |
| Health-Related Quality of Life | PCT+ | 0.46 | 0.16 | 0.76 | 0.68 | 0.38 | 0.98 | 0.70 | 0.40 | 1.00 | 0.93 | 0.63 | 1.23 |
| HOPE | 0.85 | 0.55 | 1.15 | 0.95 | 0.65 | 1.25 | 0.81 | 0.51 | 1.11 | 0.48 | 0.18 | 0.78 | |
Note. Est = Estimate, LCL = Lower 95% Confidence Limit, UCL = Upper 95% Confidence Limit. All comparisons were significant at p < .01. For Empowerment and Health-Related Quality of Life, higher scores indicate better outcomes; otherwise, lower scores indicate better outcomes.
As shown in Table 3, both treatment groups improved significantly (p < .01) in all outcomes from baseline to each subsequent assessment. However, no significant group differences were found at any occasion (all d-values within ± 0.32) or in changes from baseline to any subsequent occasion (all d-values within ± 0.30) due to relatively small effect sizes. Finally, we also examined potential moderation of change from baseline by process-related variables (i.e., length of shelter stay before baseline, number of sessions during or post-shelter, patterns of attrition), but no consistent findings emerged.
Additional Analyses
In addition to PTSD severity, we also evaluated whether participants met diagnostic criteria for IPV-related PTSD on the CAPS at each follow-up occasion (see Table 4). Pearson chi-square tests revealed no significant group differences (all ps > .05). Finally, using Jacobson and Truax’s (1991) approach, the degree of change required for reliable change was calculated at PT for all outcomes except the health-related quality of life (the Cronbach’s alpha required for the formula could not be computed given the weighted scoring procedure for the MCS). Instead, we report the percentage of participants who improved by 2 units, which is considered clinically relevant (Kazis et al., 2004). The percentage of HOPE participants who achieved clinically significant change at PT was as follows: 83.1% (n = 54) for PTSD symptom severity, 87.7% (n = 57) for IPV severity (SVAW), 83.1% (n = 54) for psychological maltreatment severity (PMWI), 50.8% (n = 32) for depression severity, 23.8% (n = 15) for empowerment, 47.7% (n = 31) for posttraumatic cognitions, and 76.7% (n = 46) for health-related quality of life. The percentage of PCT+ participants who achieved clinically significant change at PT was as follows: 76.6% (n = 59) for PTSD symptom severity, 88.2% (n = 67 ) for IPV severity (SVAW), 93.5% (n = 72) for psychological maltreatment severity (PMWI), 54.8% (n = 40) for depression severity, 25.0% (n = 19) for empowerment, 39.5% (n = 30) for posttraumatic cognitions, and 68.1% (n = 49) for health-related quality of life. No statistically significant difference in rate of reliable improvement by treatment condition was found (all p’s > .05).
Table 4.
Percentage of Participants Meeting Criteria for IPV-Related PTSD at Each Follow-Up Point
| HOPE | PCT+ | |
|---|---|---|
| Time Point | % (n) | % (n) |
| Post-Shelter | 56.2% (41) | 60.5% (49) |
| Post-Treatment | 30.8% (20) | 32.5% (25) |
| 6-Months Post-Treatment | 26.7% (16) | 32.0% (24) |
| 12-Months Post-Treatment | 16.1% (9) | 26.8% (19) |
Note. No values significantly differ by treatment group.
Discussion
Residents of domestic violence shelters randomized to HOPE or PCT+ demonstrated significant and large reductions in IPV-related PTSD and significant small to medium reductions in degree of IPV, and these effects were maintained across the 12-month follow-up period. Significant improvements in our secondary outcomes, including depression, empowerment, posttraumatic cognitions, and health-related quality of life (effect sizes ranging from small to medium; see Table 3) were found in both treatments, which were maintained across follow-up. Both treatments were also associated with loss of IPV-related PTSD diagnosis in most participants (see Table 4). Although rates of IPV-related PTSD diagnosis at each follow-up time-point (see Table 4) favored the direction of HOPE, none of these effects were significant. Further, effect sizes and rates of clinically significant change for PTSD and other outcomes were similar across treatments (see Table 3) and did not significantly differ. Both treatments also had similar and low drop-out rates (7.2% for HOPE and 5.6% for PCT+) and attendance rates (average of 8.86 sessions in HOPE and 10.06 in PCT+). Notably, treatment drop-out rates in both groups are lower than those found for trauma-specific treatments of PTSD (36%; Imel et al., 2013). Further, master’s level therapists effectively delivered both treatments across diverse shelter settings, and both treatments had high fidelity ratings and no consistent therapist effects.
Importantly, both HOPE and PCT+ were associated with reduced rates of IPV and improved health-related quality of life across follow-up. However, most participants did not achieve clinically significant improvement in degree of empowerment or posttraumatic cognitions. Additionally, mean scores in Table 2 suggest that participants were still experiencing mild to subthreshold symptoms of PTSD (CAPS scores of 20–39; Weathers et al., 2001) and clinically significant levels of depressive symptoms (i.e., clinical cut-off for CES-D is 16; Lewinsohn et al., 1997). This is not entirely surprising as mean scores in Table 2 also suggest that many participants continued to experience some abuse across follow-up. However, some participants may benefit from additional treatment targeting their depression symptoms.
Results of the current study are consistent with prior findings that HOPE is an efficacious treatment for IPV-related PTSD and associated with reductions in IPV in residents of domestic violence shelters (Johnson et al., 2011, 2016). Our findings extend prior research by demonstrating that HOPE is associated with significant treatment gains in a variety of shelter settings and that these treatment gains are relatively durable. Findings also suggest that HOPE can be competently and effectively delivered by community-based masters-level therapists.
Findings from the current study are also consistent with a growing body of research that supports PCT in the treatment of PTSD (e.g., Society for Clinical Psychology, 2020). Our experience with PCT+ might help explain how an intervention initially designed as a control condition can be efficacious in IPV survivors residing in shelter. PCT+ provides an opportunity for women to take control of the content of their therapy sessions; women choose what they include on their daily log and then choose what they prioritize to discuss in session. Considering the context of shelter residents’ lives (e.g., no control over curfew, when to eat or go to bed, or the noise level of shelter) and the well-documented loss of control IPV survivors experience in general (Walker, 2009), an opportunity to have control over anything for an average of one-hour per week could prove to be incredibly powerful. This is consistent with Sullivan and Goodman’s (2019) advocacy model for IPV survivors that emphasizes a survivor-driven and trauma-informed approach focusing on “what matters most to survivors and a concomitant view of survivors as competent adults capable of making their own decisions about their lives” (p. 25). Future research is needed to determine the specific mechanism through which PCT+ effects PTSD and related outcomes.
Practice Implications
As both HOPE and PCT+ were similarly efficacious, results of this study highlight that therapy in general can be helpful to IPV survivors residing in shelter. Although more shelters provide therapy than have in the past, almost half (48%) of shelters still do not provide therapy or counseling (NNEDV, 2018) and research finds that more than half of shelter residents do not seek therapy (Johnson & Zlotnick, 2007). Findings from this study suggest that a trauma-informed approach to therapy in shelter can have a significant impact on IPV survivors’ mental health symptoms and quality of life. Consistent with recommendations for individuals in the first stage of trauma recovery (Herman, 1992), therapists delivering PCT+ were well-educated on trauma and PCT+ included information on common reactions to trauma and active safety planning when necessary. In addition, since both PCT+ and HOPE were similarly efficacious, the therapeutic relationship might play an important role in the healing of trauma, as suggested in the literature (Norcross & Wampold, 2019).
In support of the dissemination of both treatments, study findings suggest that trained masters-level community-based therapists can deliver both HOPE and PCT+ with good fidelity. PCT+ is a less complex approach than HOPE with fewer treatment strategies and thus potentially requires less training than HOPE. Although training in this study was similar in duration for both treatments, PCT+ cases required less oversight and feedback during the training phase. Further, it is relatively easy to adapt PCT+ to be delivered by paraprofessionals, which could reduce implementation cost and make PCT+ more accessible to shelter residents. PCT+ includes safety planning, which can and has been delivered by paraprofessionals (e.g., community advocates) and by individuals without mental health expertise (e.g., Sullivan & Bybee, 1999). Given this, PCT+ may be preferable to HOPE as a treatment model for residents of domestic violence shelters with IPV-related PTSD.
Limitations and Conclusions
This study represents the first randomized controlled study of HOPE and PCT+ in women residing in shelter. Thus, results are preliminary and require replication for any firm conclusions. Strengths of the current study include the RCT design, large sample size, use of standardized measures with strong reliability and validity, use of masters-level therapists to deliver both interventions, and a long (i.e., 12-months) follow-up period. Additionally, the retention rates across follow-up were respectable (> 70% at 12-month follow-up), especially given the transient nature of our sample (i.e., homeless at the time of recruitment). This study is also high in external validity given treatment was delivered in a community setting.
Weaknesses of this study include the lack of a no-treatment control group (such as the standard services offered in shelter), and our inability to experimentally control many variables that may influence treatment outcome (e.g., length of shelter stay). Additionally, changes to the design made in this study relative to prior research on HOPE (e.g., use of community therapists) may have diluted treatment effects, contributing to our lack of significant findings. Also, as we offered both PCT+ and HOPE in all six shelters, we cannot rule out the possibility of contamination effects. Given our exclusion of residents with severe mental illness (i.e., bipolar disorder, psychotic symptoms, recent substance use disorder, and suicide risk), findings may not generalize to shelter residents with these comorbidities. Further, study findings may not generalize to other IPV populations that do not seek shelter. It is unknown whether HOPE or PCT+ reduces alcohol or drug use, and substance use disorders are often comorbid with PTSD (Hien et al., 2010). However, research suggests that once PTSD symptoms improve, substance use is often reduced (Hien et al., 2010). Future research is needed evaluating the effects of both HOPE and PCT+ on substance use and severe mental health in other settings.
This study’s findings and other research on PCT (e.g., Society for Research on Clinical Psychology, 2020) highlight the need to investigate PCT and other present-centered (rather than trauma-focused) approaches to the treatment of PTSD. Further, study findings emphasize that treatment can be successfully and effectively offered to residents of domestic violence shelters both during and after shelter. Although the current research did not include a no-treatment control group, our prior research (Johnson et al., 2011, 2016) suggests that HOPE is associated with significant treatment gains relative to standard shelter services alone. Thus, agencies that fund shelters are encouraged to prioritize funding to train staff to deliver trauma-informed interventions in shelter settings.
Supplementary Material
Acknowledgments
This work was supported by NIMH grant 1R01MH095767–02. ClinicalTrials.gov Identifier: NCT02398227. Work on this paper by the sixth author was supported by NIH grant T32 DA019426. This material is also the result of work supported with resources and the use of facilities at the Southeast Louisiana Veterans Health Care System in New Orleans, Louisiana (7th author). The contents do not represent the views of VA or the United States Government. We would like to thank Kathleen Alto, RaeAnn Anderson, Brittany Baker, April Barnes, Angela Burton, Jenifer Caldwell, Alexis DaFonseca, Larisa-Jayne Edwards, Vanessa Facemire, Katherine Fedele, Barbara Foster, Paige Giammusso, Mitzi Hutchins, Myriam Kadeba, Caitlin Martin-Wagar, Heike Mitchell, Laura Pappa, Sara Perez, Elsa Rojas-Ashe, Sarah Sanders, Lynn Shaffer, Yulia Shteynberg, Kristin Silver, Heather Sperry, Kristen Thornton, and the staff and residents of the Battered Women’s Shelter of Summit and Medina Counties, Someplace Safe, One Eighty, and Genesis House for their assistance in data collection and/or provision of therapy. We also thank our co-investigators, Doug Delahanty and Ted Miller, who assisted on other aspects of this project not described within this manuscript and consultant M. Tracie Shea for her assistance in adapting and delivering PCT. Finally, we thank Mary Ann Dutton, Michael Suvak, and Lisa Doane for serving on our Data and Safety Monitoring Board.
Contributor Information
Dawn M. Johnson, University of Akron
Patrick A. Palmieri, Summa Health System
Caron Zlotnick, Butler Hospital and Warren Alpert Medical School at Brown University.
Nicole L. Johnson, Lehigh University
Lesa Hoffman, University of Iowa.
Samantha C. Holmes, Yale University
Taylor L. Ceroni, Southeast Louisiana Veterans Health Care System
References
- American Psychiatric Association (APA, 2000). Diagnostic and statistical manual of mental disorders, 4th edition, text revision (DSM-IV-TR). Author. [Google Scholar]
- Attkisson CC, & Greenfield TK (2004). The UCSF Client Satisfaction Scales: I. The Client Satisfaction Questionnaire-8. In Maruish M. (Ed.), The use of psychological testing for treatment planning and outcome assessment (3rd ed.). Lawrence Erlbaum Associates. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, & Keane TM (1995). The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress, 8(1), 75–90. 10.1002/jts.2490080106 [DOI] [PubMed] [Google Scholar]
- Bonomi AE, Anderson ML, Reid RJ, Rivara FP, Carrell D, & Thompson RS (2009). Medical and psychosocial diagnoses in women with a history of intimate partner violence. Archives of Internal Medicine, 169(18), 1692–1697. 10.1001/archinternmed.2009.292 [DOI] [PubMed] [Google Scholar]
- Downey RG, & King CV (1998). Missing data in Likert ratings: A comparison of replacement methods. Journal of General Psychology, 125(2), 175–191. 10.1080/00221309809595542 [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS (1997). Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II). American Psychiatric Association Press. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (2002). Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research version, patient edition (SCID-I/P). Biometrics Research, New York State Psychiatric Institute. [Google Scholar]
- Foa EB, Ehlers A, Clark DM, Tolin DF, & Orsillo SM (1999). The Posttraumatic Cognitions Inventory (PTCI): Development and validation. Psychological Assessment, 11(3), 303–314. 10.1037/1040-3590.11.3.303 [DOI] [Google Scholar]
- Foa EB, McLean CP, Zang Y, Rosenfield D, Yadin E, Yarvis JS, Mintz J, Young-McCaughan S, Borah EV, Dondanville KA, Fina BA, Hall-Clark BN, Lichner T, Litz BT, Roache J, Wright EC, & Peterson A. (2018). Effect of prolonged exposure therapy delivered over 2 weeks vs 8 weeks vs present-centered therapy on PTSD symptom severity in military personnel: A randomized clinical trial. Journal of the American Medical Association, 319(4), 354–364. 10.1001/jama.2017.21242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes D, Lloyd D, Nixon RDV, Elliott P, Varker T, Perry D, Bryant RA, & Creamer M. (2012). A multisite randomized controlled effectiveness trial of cognitive processing therapy for military-related posttraumatic stress disorder. Journal of Anxiety Disorders, 26(3), 442–452. 10.1016/j.janxdis.2012.01.006 [DOI] [PubMed] [Google Scholar]
- Friedman H. (1982).. Educational and Psychological Measurement, 42(2), 521–526. 10.1177/001316448204200214 [DOI] [Google Scholar]
- Galano MM, Hunter EC, Howell KH, Miller LE, & Graham-Bermann SA (2013). Predicting shelter residence in women experiencing recent intimate partner violence. Violence Against Women, 19(4), 518–535. 10.1177/1077801213487056 [DOI] [PubMed] [Google Scholar]
- Herman JL (1992). Trauma and recovery. Basic Books. [Google Scholar]
- Hien DA, Jiang H, Campbell ANC, Hu M, Miele GM, Cohen LR, Brigham GS, Capstick C, Kulaga A, Robinson J, Suarexz-Morales L, & Nunes EV (2010). Do treatment improvements in PTSD severity affect substance use outcomes? A secondary analysis from a randomized clinical trial in NIDA’s Clinical Trials Network. American Journal of Psychiatry, 167)1, 95–101. 10.1176/appi.ajp.2009.09091261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien DA, & Ruglass L. (2009). Interpersonal partner violence and women in the United States: An overview of prevalence rates, psychiatric correlates and consequences and barriers to help seeking. International Journal of Law and Psychiatry, 32(1), 48. 10.1016/j.ijlp.2008.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman L. (2015). Longitudinal analysis: Modeling within-person fluctuation and change. Routledge. [Google Scholar]
- Imel ZE, Laska K, Jakcupcak M, & Simpson TL (2013). Meta-analysis of dropout in treatments for post-traumatic stress disorder. Journal of Consulting and Clinical Psychology, 31(3), 394–404. 10.1037/a0031474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, & Truax P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. 10.1037/10109-042 [DOI] [PubMed] [Google Scholar]
- Johnson DM, & Ceroni T. (2020). Cognitive Behavior Therapy for PTSD. In Bufka LF, Wright CV, & Halfond R. (Eds). PTSD Casebook. Washington DC: American Psychological Association. [Google Scholar]
- Johnson DM, Worell J, & Chandler RK (2005). Assessing psychological health and empowerment in women: The Personal Progress Scale Revised. Women & Health, 41(1), 109–129. 10.1300/J013v41n01_07 [DOI] [PubMed] [Google Scholar]
- Johnson DM, & Zlotnick C. (2006). A cognitive-behavioral treatment for battered women with PTSD in shelters: Findings from a pilot study. Journal of Traumatic Stress, 19(4), 559–564. 10.1002/jts.20148 [DOI] [PubMed] [Google Scholar]
- Johnson DM, & Zlotnick C. (2007). Utilization of mental health treatment and other services by battered women in shelters. Psychiatric Services, 58(12), 1595–1597. 10.1176/appi.ps.58.12.1595 [DOI] [PubMed] [Google Scholar]
- Johnson DM, & Zlotnick C. (2009). HOPE for battered women with PTSD in domestic violence shelters, Professional Psychology: Research and Practice, 40(3), 234–241. 10.1037/a0012519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson DM, Zlotnick C, & Gonzalez A. (2020). Treatment of PTSD in Survivors of Intimate Partner Violence. In Geffner R, Vieth V. Vaughan-Eden V, Rosenbaum A, Hamberger L, & White J. (Eds). Handbook of Interpersonal Violence across the Lifespan. Springer: Cham, Switzerland. [Google Scholar]
- Johnson DM, Zlotnick C, & Perez S. (2008). The relative contribution of abuse severity and PTSD severity on the psychiatric and social morbidity of battered women in shelters. Behavior Therapy, 39(3), 232–241. 10.1016/j.beth.2007.08.003 [DOI] [PubMed] [Google Scholar]
- Johnson DM, Zlotnick C, Perez S, Johnson P, N. L, & Palmieri P. (2016). Comparison of adding treatment of PTSD during and after shelter stay to standard care in residents of battered women’s shelters: Results of a randomized clinical trial. Journal of Traumatic Stress, 29(4), 365–373. 10.1002/jts.22117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson DM, Zlotnick C, & Perez S. (2011). Cognitive-behavioral treatment of PTSD in residents of battered women’s shelters: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology, 79(4), 542–551. 10.1037/a0023822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones L, Hughes M, & Unterstaller U. (2001). Post-traumatic stress disorder (PTSD) in victims of domestic violence: A review of the research. Trauma, Violence, & Abuse, 2(2), 99–119. 10.1177/1524838001002002001 [DOI] [Google Scholar]
- Jonker IE, Sijbrandij M, Van Luijtelaar MJ, Cuijpers P, & Wolf JR (2014). The effectiveness of interventions during and after residence in women’s shelters: A meta-analysis. The European Journal of Public Health, 25(1), 15–19. 10.1093/eurpub/cku092 [DOI] [PubMed] [Google Scholar]
- Kazis LE, Miller DR, Skinner KM, Lee A, Ren XS, Clark JA, Rogers WH, Spiro A, Selim A, Linzer M, Payne SM, Mansell D, & Fincke RG (2004). Patient-reported measures of health: The Veterans Health Study. Journal of Ambulatory Care Management, 27(1), 70–83. 10.1007/s11136-017-1638-x [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, & Andreasen NC (1987). The Longitudinal Interval Follow-up Evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry, 44(6), 540–548. 10.1001/archpsyc.1987.01800180050009 [DOI] [PubMed] [Google Scholar]
- Kelly UA, & Pich K. (2014). Community-based PTSD treatment for ethnically diverse women who experienced intimate partner violence: A feasibility study. Issues in Mental Health Nursing, 35(12), 906–913. 10.3109/01612840.2014.931496 [DOI] [PubMed] [Google Scholar]
- Kubany ES, Hill EE, Owens JA, Iannce-Spencer C, McCaig MA, Tremayne KJ, & Williams PL (2004). Cognitive trauma therapy for battered women with PTSD (CTT-BW). Journal of Consulting and Clinical Psychology, 72(1), 3–18. 10.1037/0022-006X.72.1.3 [DOI] [PubMed] [Google Scholar]
- Lang AJ, Schnurr PP, Jain S, He F, Walser RD, Bolton E, Benedek DM, Norman SB, Sylvers P. Flashman L, Strauss J, Raman R. & Chard KM (2017). Randomized controlled trial of acceptance and commitment therapy for distress and impairment in OEF/OIF/OND veterans. Psychological Trauma: Theory, Research, Practice, and Policy, 9(S1), 74–84. 10.1037/tra0000127 [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Seely JR, Roberts RE, & Allen NB (1997). Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology and Aging, 12(2), 277–287. 10.1037/0882-7974.12.2.277 [DOI] [PubMed] [Google Scholar]
- Marshall LL (1992). Development of the Severity of Violence Against Women Scales. Journal of Family Violence, 7(2), 103–121. 10.1007/BF00978700 [DOI] [Google Scholar]
- McCann IL, Sakheim DK, & Abrahamson DJ (1988). Trauma and victimization: A model of psychological adaptation. The Counseling Psychologist, 16(4), 531–594. 10.1177/0011000088164002 [DOI] [Google Scholar]
- Miller IW, Norman WH, Bishop SB, & Dow MG (1986). The Modified Scale for Suicidal Ideation: Reliability and validity. Journal of Consulting and Clinical Psychology, 54(5), 724. 10.1037/0022-006X.54.5.724 [DOI] [PubMed] [Google Scholar]
- National Network to End Domestic Violence (2018). 13th Annual domestic violence counts report. https://nnedv.org/wp-content/uploads/2019/10/Census_2018_handout_report.pdf.
- Norcross JC, & Wampold BE (2019). Relationships and responsiveness in the psychological treatment of trauma: The tragedy of the APA Clinical Practice Guideline. Psychotherapy, 56(3), 391–399. 10.1037/pst0000228 [DOI] [PubMed] [Google Scholar]
- Norris FH (1990). Screening for traumatic stress: A scale for use in the general population. Journal of Applied Social Psychology, 20(20), 1704–1715. 10.1111/j.1559-1816.1990.tb01505.x [DOI] [Google Scholar]
- Parent MC (2013). Handling item-level missing data: Simpler is just as good. The Counseling Psychologist, 41(4), 568–600. 10.1177/0011000012445176 [DOI] [Google Scholar]
- Perez S, Johnson DM, Walter KH, & Johnson N. (2012). The role of PTSD and length of shelter stay in battered women’s severity of reabuse after leaving shelter. Journal of Aggression, Maltreatment, & Trauma, 21(7), 776–792. 10.1080/10926771.2012.702712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson C, Kearns MC, McIntosh WL, Estefan LF, Nicolaiidis C, McCollister KE, Gordon A, & Florence C. (2018). Lifetime economic burden of intimate partner violence among U.S. Adults . American Journal of Preventative Medicine, 55(4), 433–444. 10.1016/j.amepre.2018.04.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A, Ouimette P, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, Thrailkill A, Gusman FD, & Sheikh JI (2003). The primary care PTSD screen (PC-PTSD): Development and operating characteristics. Primary Care Psychiatry, 9(1), 9–14. 10.1185/135525703125002360 [DOI] [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Raudenbush SW, & Liu X. (2000). Statistical power and optimal design for multisite randomized trials. Psychological Methods, 5(2), 199–213. 10.1037/1082-989X.5.2.199 [DOI] [PubMed] [Google Scholar]
- Rhodes KV, Rodgers M, Sommers M, Hanlon A, Chittams J, Doyle A, Datner E. & Crits- Christoph P. (2015). Brief motivational intervention for intimate partner violence and heavy drinking in the emergency department: A randomized clinical trial. Journal of the American Medical Association, 314(5), 466–477. 10.1001/jama.2015.8369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizo CF, Wretman CJ, Macy RJ, Guo S, & Ermentrout DM. (2018). A novel intervention for system-involved female intimate partner violence survivors: Changes in mental health. American Journal of Orthopsychiatry, 88(6), 681–690. 10.1037/ort0000332 [DOI] [PubMed] [Google Scholar]
- Santos A, Matos M, & Machado A. (2017). Effectiveness of a group intervention program for female victims of intimate partner violence. Small Group Research, 48(1), 34–61. 10.1177/1046496416675226 [DOI] [Google Scholar]
- Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Chow BK, Resick PA, Thurston V, Orsillo SM, Haug R, Turner C. & Bernardy N. (2007). Cognitive behavioral therapy for posttraumatic stress disorder in women: A randomized controlled trial. Journal of the American Medical Association, 297(8), 820–830. 10.1177/1046496416675226 [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T. Baker R, & Dunbar GC (1998). The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59(s20), 22–33. 10.1016/S0924-9338(97)83296-8 [DOI] [PubMed] [Google Scholar]
- Smith SG, Zhang X, Basile KC, Merrick MT, Wang J, Kresnow MJ, & Chen J. (2018). The National Intimate Partner and Sexual Violence Survey: 2015 data brief–updated release. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. https://www.cdc.gov/violenceprevention/pdf/2015data-brief508.pdf [Google Scholar]
- Society for Clinical Psychology. (2020). Present-centered therapy for post-traumatic stress disorder. https://www.div12.org/treatment/present-centered-therapy-for-post-traumatic-stress-disorder/
- Spencer C, Mallory AB, Cafferky BM, Kimmes GG, Beck AR, & Stith SM (2019). Mental health factors and intimate partner violence perpetration and victimization: A meta-analysis. Psychology of Violence, 9(1), 1–17. 10.1037/vio0000156 [DOI] [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, & Del Boca FK (1994). Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol, Supplement, (s12), 70–75. 10.15288/jsas.1994.s12.70 [DOI] [PubMed] [Google Scholar]
- Sullivan CM, & Bybee DI (1999). Reducing violence using community-based advocacy for women with abusive partners. Journal of Consulting and Clinical Psychology, 67(1), 43–53. 10.1037/0022-006X.67.1.43 [DOI] [PubMed] [Google Scholar]
- Sullivan CM, & Cain D. (2004). Ethical and safety considerations when obtaining information from or about battered women for research purposes. Journal of Interpersonal Violence, 19(5), 603–618. 10.1177/0886260504263249 [DOI] [PubMed] [Google Scholar]
- Sullivan CM, & Goodman LA (2019). Advocacy with survivors of intimate partner violence: What it is, what it isn’t, and why it’s critically important. Violence Against Women, 25(16), 2007–2023. 10.1177/1077801219875826 [DOI] [PubMed] [Google Scholar]
- Tolman RM (1999). The validation of the Psychological Maltreatment of Women Inventory. Violence and Victims, 14(1), 25–37. [PubMed] [Google Scholar]
- Walker LEA (2009). The battered woman syndrome (3rd ed.). Springer. [Google Scholar]
- Ware JE, Kosinski M, & Keller SD (1995). How to score the SF-12 physical & mental health summary scales. The Health Institute, New England Medical Center. [Google Scholar]
- Ware JE, Kosinski M, & Keller SD (1996). A 12-item Short Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34(3), 220–233. 10.1097/00005650-199603000-00003 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, & Davidson JR (2001). Clinician Administered PTSD Scale: A review of the first ten years of research. Depression and Anxiety, 13(3), 132–156. 10.1002/da.1029 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Ruscio AM, & Keane TM (1999). Psychometric properties of nine scoring rules for the Clinician Administered Posttraumatic Stress Disorder Scale. Psychological Assessment, 11(2), 123–133. 10.1037/1040-3590.11.2.124 [DOI] [Google Scholar]
- Worell J, & Remer P. (2002). Feminist perspectives in therapy: Empowering diverse women. John Wiley & Sons. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.