To the Editor: During the COVID-19 pandemic, cases of acute hair shedding following the infection have been reported. Telogen effluvium (TE), a self-limiting cause of diffuse hair shedding, typically occurs 2 to 3 months after a triggering event, such as febrile state, stress, drugs, or postpartum.1 We aimed to evaluate the onset and duration of acute TE post COVID-19.
Patients were recruited by 4 dermatologists in the United States, Brazil, and Spain, who agreed to provide retrospective data of patients with hair loss after COVID-19 infection, which was confirmed by reverse transcription polymerase chain reaction test for SARS-CoV-2. Only patients with monthly follow-up until recovery of hair loss were eligible. Diagnosis of TE was based on dermatologist evaluation, using mainly trichoscopy (Fig 1 ) and pull test, with 1 patient confirmed by biopsy. Background information gathered included sex, age, country of residence, pertinent medical history, date of reverse transcription polymerase chain reaction, recovery from symptoms, date of TE onset and cessation, patchy alopecia upon resolution, and medications. Patients continued their prescribed medications throughout COVID-19 infection (Supplemental material available via Mendeley at https://doi.org/10.17632/bsn65bztxy.4).
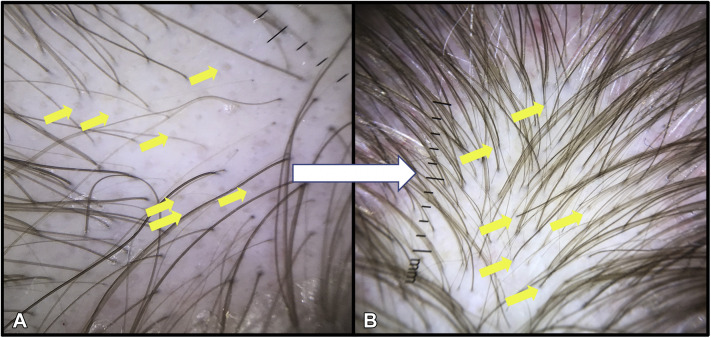
Fig 1.
Acute telogen effluvium post COVID-19 in 1 female patient with androgenetic alopecia background. A, Trichoscopy shows empty follicles (yellow arrows) and hair shaft variability. B, After 4 months, the resolution of empty follicles and the presence of short hair shafts (yellow arrows) growing after TE can be seen.
Among the 30 cases, 9 (30%) were men, and 21 (70%) were women. The median age was 40.5 years (interquartile range = 13). Overall, 26.7% of patients (5 men, 3 women) had a history of androgenetic alopecia. The onset of acute TE occurred at a median of 45 days (interquartile range = 13) after a positive reverse transcription polymerase chain reaction test. The median duration of TE was 47.5 days (interquartile range = 45), ranging from 12 to 100 days. One patient presented with patchy alopecia in the occipital area, diagnosed as pressure alopecia from prolonged intensive care admission. 53.3% of patients reported concomitant medication use. Trichoscopy showed empty hair follicles, as expected for TE (Fig 1, A).
Acute TE post COVID-19 appears to occur sooner than when triggered by usual events, at a median of 1.5 months. In a multicenter study of 214 cases of acute TE post COVID-19, Moreno-Arrones et al2 noted an average of 57.1 days to onset. Trüeb et al3 similarly observed early onset effluvium in 5 consecutive cases of confirmed SARS-CoV-2 infection. Although typical acute TE takes 3 to 6 months to cease, resolution of most of our cases was observed before 2 months.1 Factors such as hypoxia, inflammation, metabolic abnormalities, medications, and the eventual need for mechanical ventilation could play a role in the development and severity of TE. The intensity of the effluvium and earlier onset could be related to the individual severity of COVID-19. As previously studied, elevated levels of interleukin 6 were documented in COVID-19.4 Interleukin 6 inhibits hair shaft elongation and proliferation of matrix cells that express interleukin 6 receptor in cultured hair follicles, suggesting a connection between the pathophysiology of COVID-19 and the manifestation of TE.5 In sum, these cases depict an intense TE with shorter duration, potentially reducing hair density or unmasking previous androgenetic alopecia. Because patients may present with TE sometime after their COVID-19 infection, it is important for clinicians to consider a previous COVID-19 infection as a possible cause for their patient's TE in the context of this pandemic. Limitations of the study include the possibility of other concomitant causes of TE and the small number of cases.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Malkud S. Telogen effluvium: a review. J Clin Diagn Res. 2015;9(9):WE01–WE03. doi: 10.7860/JCDR/2015/15219.6492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moreno-Arrones O.M., Lobato-Berezo A., Gomez-Zubiaur A. SARS-CoV-2-induced telogen effluvium: a multicentric study. J Eur Acad Dermatol Venereol. 2021;35(3):e181–e183. doi: 10.1111/jdv.17045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Trüeb R.M., Rezende H.D., Dias M.F. Comment on alopecia and grey hair associated with COVID-19 Severity. Exp Dermatol. 2020;29(12):1250–1252. doi: 10.1111/exd.14220. [DOI] [PubMed] [Google Scholar]
- 4.Grifoni E., Valoriani A., Cei F. Interleukin-6 as prognosticator in patients with COVID-19. J Infect. 2020;81(3):452–482. doi: 10.1016/j.jinf.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kwack M.H., Ahn J.S., Kim M.K. Dihydrotestosterone-inducible IL-6 inhibits elongation of human hair shafts by suppressing matrix cell proliferation and promotes regression of hair follicles in mice. J Invest Dermatol. 2012;132(1):43–49. doi: 10.1038/jid.2011.274. [DOI] [PubMed] [Google Scholar]