Abstract
Background
In December 2019, a global pandemic of Coronavirus 2019 (COVID-19) has invaded entire the world. The virus associated with the COVID-19 infections is SARS-CoV-2; the infections are mainly pulmonary manifesting as severe respiratory complications such as acute respiratory distress syndrome. However, there are some extra-pulmonary manifestations that are reported to be associated with SARS-CoV-2 from the published literature. We aim to report a case manifested as post-COVID-19 optic neuritis, in addition to make a quantitative analysis (meta-analysis) for the published similar case reports around the world.
Methods
We followed CARE guidelines for case reports. Also, we followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Case presentation
A 32-year-old male patient with no previous relevant medical history, presented to the ophthalmology clinic in a tertiary hospital. He complained of a sudden drop of vision in his left eye, throbbing left sided headaches, central scotoma, color depth affection, elevated intra-ocular pressure; two weeks post-COVID-19 infection.
Results
Post-COVID optic neuritis is a possible neurological complication of the novel coronavirus infection. It was shown that females were more affected by optic neuritis and retinal complications, the left eye is more liable to drop of visual acuity post-COVID-19 infection; while there was no significant difference between both eyes regarding accompanied vision loss or blindness.
Conclusions
Optic neuritis either unilateral or bilateral could be one of the possible viral manifestations after COVID-19 infection.
Keywords: COVID-19, Optic neuritis
1. Introduction
In December 2019, a global pandemic invaded the entire world called Coronavirus 2019 (COVID-19). The virus associated with the COVID-19 infections is SARS-CoV-2; the infections are mainly pulmonary, manifesting with severe respiratory complications such as acute respiratory distress syndrome (ARDS). However, extra-pulmonary manifestations were reported to be associated with SARS-CoV-2 from the published literature [1]. Optic neuritis is usually unilateral and associated with an acute painful eye or just periorbital pain, and reaching its maximum presentation within a week [2]. We aim to report a case manifested with optic neuritis post-COVID-19 infection, in addition to presenting a quantitative analysis (meta-analysis) for the published similar case reports around the world. To our knowledge, this is the world's first COVID-19 study reporting a case report accompanied by quantitative analysis for previous case reports of optic neuritis.
2. Methods
We aim to follow CARE guidelines for case reports. We also followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
2.1. Selection of the studies for quantitative analysis
Two authors (MAA, AYA) applied the selection criteria. Eligibility was divided into three steps. The first step is the title screening after database searching using particular keywords (“optic neuritis AND COVID-19” and “optic neuritis AND SARS-CoV-2”) on PubMed/Medline, Scopus and Google Scholar; the second step is abstracts screening, and the third step is a full-text screening for the relevant information for the meta-analysis. Conflicts between authors have been resolved by a third author (HH). Inclusion criteria included, at least one case reported with optic neuritis post COVID-19 infection, while exclusion criteria were regarding articles which didn’t report any clinical data regarding the patients such as editorials and letter to the editor.
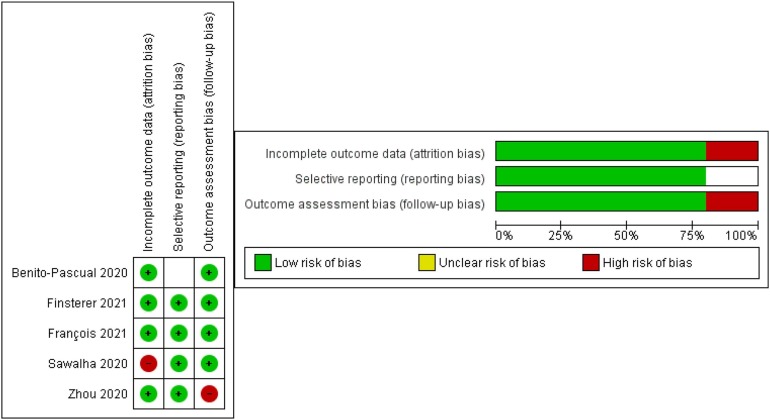
2.2. Risk of bias assessment for quantitative synthesis
Two authors (SFH, HH) assessed the risk of bias among the studies using the Cochrane risk of the bias assessment tool in Review Manager V5.4.0, similar to the Cochrane Handbook of Systematic Reviews Interventions.
2.3. Data analysis for quantitative synthesis
Differentiation between gender affection, visual loss assessment, and visual acuity changes was pooled using the odds ratio (OR). We used RStudio Version 1.2.5033
2.4. Heterogeneity assessment
The forest plots were used to analyze the data by visual inspection and testing using I2 and Chi2 tests. A sensitivity analysis was performed to detect the heterogeneity in the case of significant heterogeneity (Chi2 P < 0.1).
2.5. Publication bias
The funnel plot is one of the standard methods to assess bias among in the included studies if the number of studies is at least ten to consider the funnel plot significant according to Egger 1997 at al. [3]; however, it was not used because the number of included studies in the analysis is lower than ten.
3. Case presentation
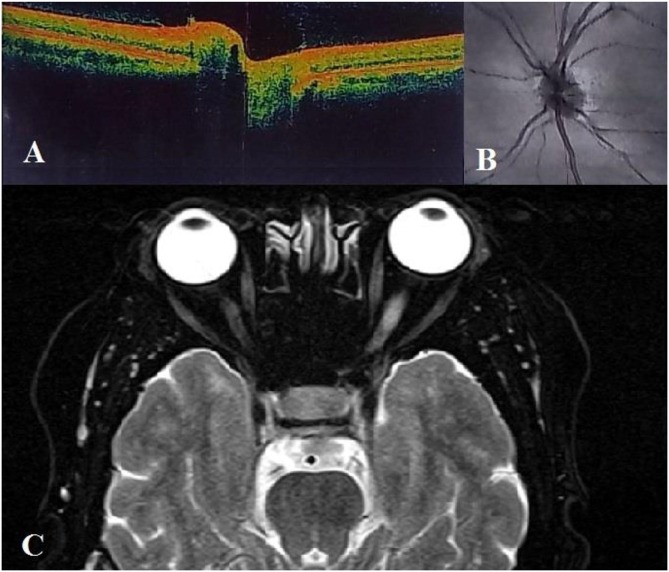
A 32-year-old male patient with no relevant medical history presented to the ophthalmology clinic in a tertiary hospital. He complained of a sudden drop of vision in his left eye, throbbing headaches, central dark points in the visual field, and color depth affection, two weeks post-COVID-19 infection. The patient claimed that he was hospitalized for ten days in the intensive care unit (ICU) due to severe COVID-19 complications; the confirmation of SARS-CoV-2 was done by a nasopharyngeal swab polymerase chain reaction (PCR). No antiviral drugs were prescribed; only paracetamol 500 mg twice per day for a week. A week later, the patient developed a gradual loss of vision. The IOP in the left eye was 23 and in the right eye it was 16, so there is a borderline IOP in the left eye. By slit lamb examination, both the anterior chamber and the vitreous, and the uvea were free of inflammation. Fundus examination revealed only left mild disc swelling while vessels were normal in course and caliber and no lesions, scars, or pigmentary changes in the macula or periphery. General neurological examination was free. Optical coherence tomography (OCT), fundus examination and magnetic resonance imaging (MRI) axial T2 were used by the ophthalmologist Fig. 1 . Visual acuity test was 20/200 best corrected on the affected eye (left eye) with an evident relative afferent pupillary defect (RAPD); the non-affected eye (right eye) visual acuity was 20/30. The final diagnosis of the case is a left optic neuritis. One-gram intravenous methylprednisolone for three days followed by, 60 mg oral prednisone were prescribed for a week with gradual tapering and a proton pump inhibitor in addition to paracetamol 500 mg once per day. The left eye improved and was about 20/40 in the third follow up, but did not regain the visual acuity and color depth perception as before COVID-19 infection. There are several follow-up sessions are to be within neurology and ophthalmology departments aiming at a faster recovery.
Fig. 1.
A) OCT showing retinal nerve papilla mild swelling; B) fundus examination showing mild papilledema; D) Axial T2 MRI showing left optic nerve swelling of the retro-bulbar intra-orbital segment.
4. Results
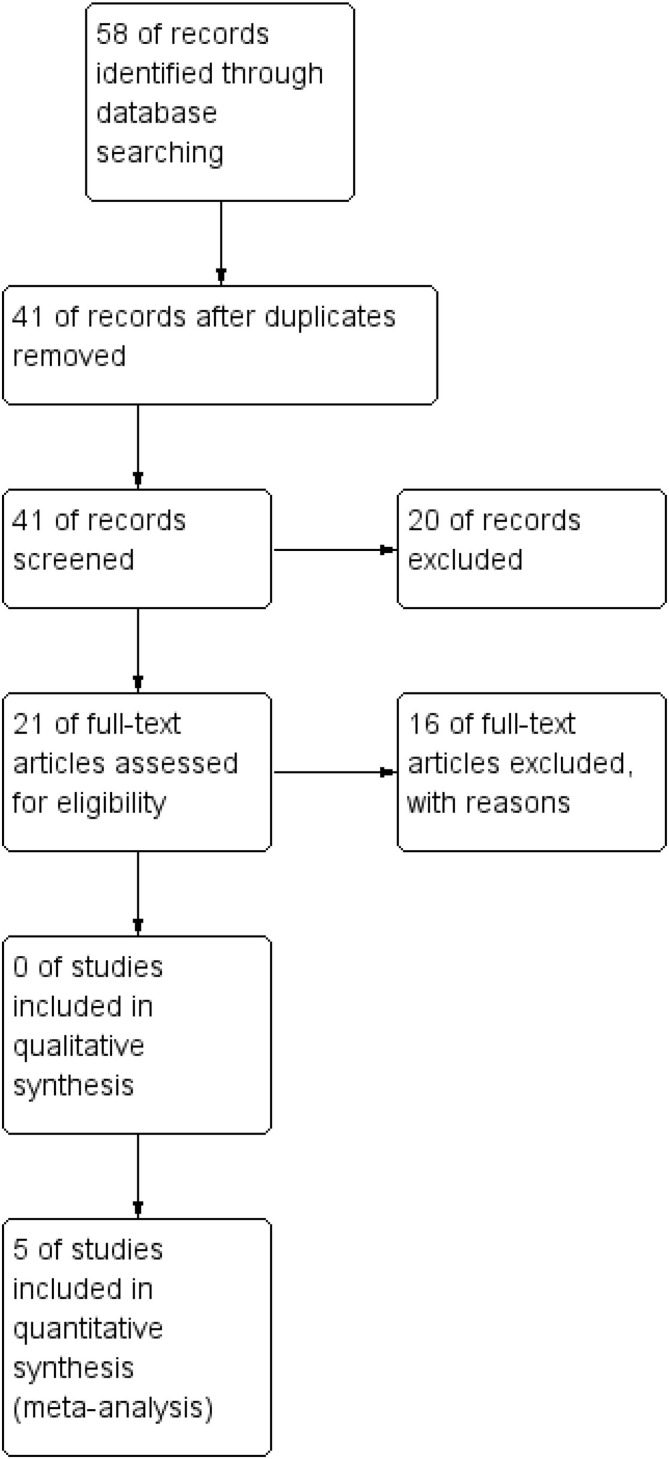
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines to perform all the quantitative synthesis steps. PRISMA flow diagram Fig. 2 was used to report the inclusion and the exclusion of the studies. A summary of the included studies' results is shown in Table 1 . Baseline characteristics of the included studies are listed in Table 2 . The results of the Cochrane risk of bias assessment tool are presented in Fig. 3 .
Fig. 2.
PRISMA flow diagram.
Table 1.
Summary of the previous case reports.
| Study | Country | Design | Intervention | Population | Results and Outcomes |
|---|---|---|---|---|---|
| Zhou 2020 et al. [8] | USA | Case report | One gram intravenous methylprednisolone | Man with optic neuritis and myelitis post-COVID-19 Infection. | Improvement in visual acuity and complete resolution of retinal findings and optic disc edema |
| Sawalha 2020 et al. [9] | USA | Case report | One gram of methylprednisolone every 24 h for five days | Man with bilateral optic neuritis post-COVID-19 infection. | Complete restoration of vision in the left eye, while the right eye did not show complete recovery. |
| Finsterer 2021 et al. [11] | Brazil | Case series | Intravenous methylprednisolone and oral prednisone | Cases with optic neuritis and mimic retinitis post-COVID-19 infection. | Improvement in vision, some patients' had complete resolution while some did not sow complete recovery yet |
| François 2021 et al. [12] | France | Case report | Oral and topical corticosteroids | Woman with ocular neuropathy and pan-uveitis post-COVID. | Permanent visual acuity loss without recovery |
| Benito-Pascual 2020 et al. [10] | Spain | Case report | 60 mg oral prednisone, 400 mg hydroxychloroquine and 400 mg lopinavir for six days | Woman with pan-uveitis and optic neuritis post-COVID-19 infection. | Improvement of visual acuity, but without complete recovery |
Table 2.
Baseline characteristics of the studies.
| Study | Gender | Age | Optic neuritis affected eye | Visual acuity (right eye) | Visual acuity (left eye) |
|---|---|---|---|---|---|
| Zhou 2020 et al. [8] | Male | 26 | Left eye | Hand motion | 20/250 |
| Sawalha 2020 et al. [9] | Male | 44 | Both eyes | 20/200 | 20/30 |
| Benito-Pascual 2020 et al. [10] | Female | 50 | Left eye | 6/6 | 20/200 |
| Finsterer 2021 et al. [11] | Male | 48 | Left eye | N/A | N/A |
| François 2021 et al. [12] | Female | 38 | Right eye | Blindness (non-COVID-19 related) | Hand motion |
Fig. 3.
Cochrane risk of bias assessment.
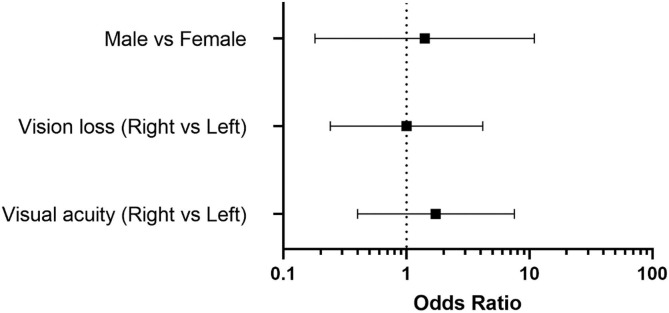
4.1. Gender affection
Forest plot indicates that females were more affected by the optic neuritis and retinal complications after COVID-19 infection (OR = 1.73, 95% CI [0.4, 7.53], P-value < 0.01) Fig. 4 . The results were statistically significant and homogenous.
Fig. 4.
Forest plot for the studies included in quantitative synthesis.
4.2. Vision loss
Forest plot indicates both eyes were almost equal in the rate of vision loss or blindness after COVID-19 infection (OR = 1.00, 95% CI [0.24, 4.18], P-value < 0.01) Fig. 4. The results were statistically significant and homogenous.
4.3. Visual acuity
Forest plot indicates that left eye was more affected in the drop of visual acuity after COVID-19 infection (OR = 1.41, 95% CI [0.18, 10.94], P-value < 0.01) Fig. 4. The results were statistically significant and homogenous.
5. Discussion
Optic neuritis is an autoimmune inflammatory condition that develops a rapid drop of vision accompanied by ocular movement-induced pain; it is usually unilateral and associated with multiple sclerosis (MS) [4]. The progression of optic neuritis is initiated by demyelination and swelling of optic nerve fibers due to systemic T-cell activation leading to immunological antigen-antibody reaction [5]. The diagnosis is mainly dependent on the medical history and examination. The findings in the fundoscopic examination, OCT and MRI are diagnostic in cases of optic neuritis [6]. Upon diagnosis, the treatment plan should be started as soon as possible. The current standard treatment plan for optic neuritis is intravenous methylprednisolone, oral prednisone and the doses are modified according to patients’ age, medical history and interaction with other drugs if present [4]. In our case, we present one of the relatively rare COVID-19 complications. Since presentation with optic neuritis is usually accompanied by MS, we recommend the patient several follow-up sessions with both ophthalmologists and neurologists to rule out any other medical conditions inflicted later. However, this is not the first time that COVID-19 affects the nervous system and causing damage to it; in a recent case report by Azab 2021 et al. [7], it was reported SARS-CoV-2 had caused viral encephalitis with mortality outcome. It has been suggested that SARS-CoV-2 has the potential to develop several neurological complications. To our knowledge, we performed the first meta-analysis for case reports regarding the development of optic neuritis post-COVID-19 infection.
6. Conclusions
Optic neuritis, either unilateral or bilateral, can be one of the possible presentations after the COVID-19 infection. We suggest if any patient starts to develop a sudden drop of vision, unusual headaches to visit the neurology department as soon as possible to rule out any post-viral complications.
Funding
The authors' did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approvals
All necessary approvals have been obtained successfully.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Jiang F., Deng L., Zhang L., Cai Y., Cheung C.W., Xia Z. Review of the clinical characteristics of coronavirus disease 2019 (COVID-19) J. Gen. Intern. Med. 2020;35(5):1545–1549. doi: 10.1007/s11606-020-05762-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de la Cruz J., Kupersmith M.J. Clinical profile of simultaneous bilateral optic neuritis in adults. Br. J. Ophthalmol. 2006;90(5):551–554. doi: 10.1136/bjo.2005.085399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Egger M., Smith G.D., Schneider M., Minder C. bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balcer L.J. Clinical practice. Optic neuritis. N. Engl. J. Med. 2006;354(12):1273–1280. doi: 10.1056/NEJMcp053247. [DOI] [PubMed] [Google Scholar]
- 5.Roed H., Frederiksen J., Langkilde A., Sørensen T.L., Lauritzen M., Sellebjerg F. Systemic T-cell activation in acute clinically isolated optic neuritis. J. Neuroimmunol. 2005;162(1-2):165–172. doi: 10.1016/j.jneuroim.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 6.Jacobs L.D., Kaba S.E., Miller C.M., Priore R.L., Brownscheidle C.M. Correlation of clinical, magnetic resonance imaging, and cerebrospinal fluid findings in optic neuritis. Ann. Neurol. 1997;41(3):392–398. doi: 10.1002/ana.410410315. [DOI] [PubMed] [Google Scholar]
- 7.Azab M.A., Azzam A.Y. SARS-CoV-2 associated viral encephalitis with mortality outcome. Interdiscip. Neurosurg. 2021;25 doi: 10.1016/j.inat.2021.101132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhou S., et al. Myelin oligodendrocyte glycoprotein antibody-associated optic neuritis and myelitis in COVID-19. J. Neuroophthalmol. 2020;40(3):398–402. doi: 10.1097/WNO.0000000000001049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sawalha K., Adeodokun S., Kamoga G.R. COVID-19-induced acute bilateral optic neuritis. J. Invest. Med. High Impact Case Rep. 2020;8 doi: 10.1177/2324709620976018. 2324709620976018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benito-Pascual B., Gegúndez J.A., Díaz-Valle D., Arriola-Villalobos P., Carreño E., Culebras E., Rodríguez-Avial I., Benitez-Del-Castillo J.M. Panuveitis and optic neuritis as a possible initial presentation of the novel coronavirus disease 2019 (COVID-19) Ocul. Immunol. Inflamm. 2020;28(6):922–925. doi: 10.1080/09273948.2020.1792512. [DOI] [PubMed] [Google Scholar]
- 11.Finsterer J., et al. Vascular damage may mimic retinitis and optic neuritis in COVID-19. Curr. Eye Res. 2021;1–2 doi: 10.1080/02713683.2021.1896743. [DOI] [PubMed] [Google Scholar]
- 12.François J., Collery A.S., Hayek G., Sot M., Zaidi M., Lhuillier L., Perone J.M. Coronavirus disease 2019-associated ocular neuropathy with panuveitis: a case report. JAMA Ophthalmol. 2021;139(2):247. doi: 10.1001/jamaophthalmol.2020.5695. [DOI] [PubMed] [Google Scholar]