In the case of hospitalised COVID-19 patients, especially aging people and those with severe symptoms who require a ventilator, corticosteroids are given in an attempt to alleviate some of the symptoms. However, steroids are known to lower immunity and raise blood sugar levels, and they tend to increase clotting factors and fibrinogen concentrations in patients. This situation provides an opportunity for pathogens to evade the human immune system and infect the host. According to a recent study, the number of cases of mucormycosis (also known as zygomycosis, black fungus) have increased in COVID-19 patients who are either hospitalised or have recovered [1]. Mucormycosis affects the nose, eyes, and brain [2] and is a potentially fatal intrusive fungal infection that frequently affects immunodeficient individuals. People with type-2 diabetes with blood sugar levels higher than 220 mg/dL, autoimmune disorders, iatrogenic immunosuppression, or hematological cancers, and organ transplant recipients are especially vulnerable to mucormycosis [3]. Mucormycosis invades sinus tissues within 3 to 4 weeks [4], and rhinocerebral mucormycosis can manifest with unusual signs and symptoms comparable to severe sinusitis, such as nasal blockage, crusting, proptosis, facial oedema, ptosis, chemosis, ophthalmoplegia, in addition to headache, fever, and other neurological symptoms [5]. Black eschar is common in the nasal cavity or over the hard palate region and penetration of blood vessels, vasculitis with thrombosis, tissue infarction, haemorrhage, and acute neutrophilic infiltrates are histopathological characteristics [6]. Without early identification and treatment, the condition may proceed rapidly, with reported fatality rates from intra-orbital and cerebral complications of 50–80%. Even with quick diagnosis, treatment of underlying conditions, and vigorous medical and surgical interventions, therapy is frequently non-effective, resulting in spread and eventual death [7]. There are several hypotheses as to what else may contribute to mucormycosis infections. Some are unlikely, such as the use of industrial oxygen or ventilation systems, age-related immune complications and non-sterile water, whilst others believe that steam inhalation may play a role by impacting the mucosa, in addition to zinc supplementation being a fungal growth promoter [8].
A complicated interaction of variables such as type-2 diabetes with or without diabetic ketoacidosis (DKA), chronic kidney disease, prior pulmonary issues, use of immunosuppressive medications, nosocomial infection sources, and immune system modifications caused by COVID-19 itself may result in secondary infections, which are becoming more recognised due to their influence on morbidity and death. COVID-19 patients admitted to an ICU, and those requiring a ventilator, or those with prolonged hospital admission (up to 50 days) are more likely to present with fungal co-infections [9]. In addition, use of coritcosteroids during COVID-19 treatment may further reduce immune responses, allowing opportunistic fungal infections. It is therefore vital to be aware that COVID-19 patients, particularly those who are critically ill, may acquire secondary fungal infections and early detection is critical [10]. Other contributing factors which increase susceptibility to secondary infections include increase interleukin (IL)-1 and IL-6 along with tumor necrosis factor-alfa, while decreased levels of CD4 and CD8 T cells and persistent lymphopenia are also contributors [11]. The conclusion is made based on the 13 cross-sectional studies conducted in the China enrolling 20 to 200 confirmed cases of COVID-19 [12]. Patients with ketoacidosis present with low cytosolic pH which aids in the growth of mucor spores and corticosteroid usage further decreases the immune response to the fungus [13]. In addition, high blood glucose levels lead to transferrin and ferritin to glycosylate, which lowers iron coupling and allows for more free iron, which ultimately causes tissue damage due to generation of large amounts of reactive oxygen species [14].
Mucormycosis is rare, accounting for 1.8 cases per 1 million per year worldwide; however, during the COVID-19 pandemic more cases have been reported (Table 1 ). With the emergence of the second COVID-19 wave in India in particular, a significant rise in the number of mucormycosis cases has been reported, with over 40,854 reported cases and 3129 deaths thus far [13,[15], [16], [17]]. Of these reported cases, 86% were COVID-19 positive, of whom 64.1% were comorbid diabetic whilst 32% were aged 18-45 and 68% aged above 45, accounting for 27,546 cases [17]. The cases were reported in the 28 states of India with the highest numbers of cases reported in Gujarat (5486) and Maharashtra (6339) [18]. In a retrospective study, it was noted that patients with uncontrolled type-2 diabetes were more prone to such opportunistic infections following prolonged ventilator use in hospital [19].
Table 1.
Global picture of mucormycosis as a post-COVID-19 complication.
In another study analysis of 101 mucormycosis patients with COVID-19, 80% were diabetic and 78.9% were male [13]. In addition, a case report described a 33-year-old woman with mucormycosis and orbital compartment syndrome who had recovered from COVID-19 and who had a history of asthma and hypertension and upon presentation in hospital had very high blood glucose levels [20]. Similarly, in a retrospective analysis of six male COVID-19 patients in India who developed rhino-orbital mucormycosis, all were diabetic and their mean age was 60.5 ± 12 [19]. A middle-aged diabetic women with non-diabetic ketoacidosis having left eye complete ptosis and facial pain with no signs of rhinitis or sinusitis was also positive for mucormycosis [21]. In a post-mortem prospective study, 10 patients with a confirmed diagnosis of SARS-CoV-2 showed a number of clinical manifestations, including thrombosis, acute tubular injury, lung damage, CD8+ T cell depletion, as well as unexpected findings, including inflammation around the heart, pancreas, and brain, and one of the 10 had disseminated mucormycosis [22]. The median age of this cohort was 73 years. These findings demonstrate the importance of early diagnosis of clinical damage due to COVID-19. Furthermore, a report of 10 cases of mucormycosis in India noted five cases of DKA, with three of them developing DKA during their hospital stay [16]. A case report in Iran described a 44-year-old diabetic woman with a 5‐day history of fever, facial swelling, malaise, toothache, dry cough and partial dyspnoea who was diagnosed with mucormycosis and treated with liposomal amphotericin B [23]. Currently, there is one active clinical trial [NCT04368221], at Rennes University Hospital in France, evaluating the pervasiveness of fungal co-infections in patients with COVID-19 who are immunocompromised and on oxygen for ventilation in ICU.
Once diagnosis of mucormycosis is confirmed, surgical intervention in the affected area is required to enhance survival, but it is not a cure (Fig. 1 ) [31]. To begin, amphotericin-B deoxycholate, an anti-fungal treatment, is favoured due to lower toxic effects to the kidneys [32]; patients with infections tolerant to amphotericin are usually prescribed posaconazole. Even with rigorous surgery and intravenous anti-fungal treatments, the prognosis remains dismal, with documented fatality rates of 33–80%, rising to 100% in disseminated infections [5].
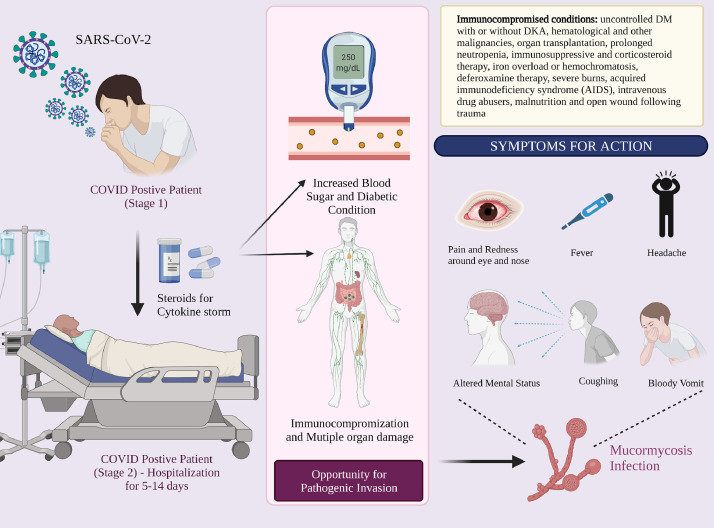
Fig. 1.
Mucormycosis – an opportunistic infection in the immunocompromised individual.
The cause of the outburst of mucormycosis remains a mystery. It is imperative for health professionals to be on the lookout for mucormycosis in COVID-19 patients, particularly those with type-2 diabetes, aging people, and those with facial or orbital pain or black or blood-stained sinus drainage [33]. India has contributed to almost 70% of the global cases of mucormycosis since the emergence of COVID-19 [34]. The rise in mucormycosis in India reflects the triumvirate of type-2 diabetes, widespread corticosteroid use, and SARS-CoV-2 infection; the rate increases considerably in those above 45 years of age. More recently, in India new threats have surfaced, including white and yellow fungus, bacterial infections, and a number of opportunistic respiratory co-infections in patients with severe COVID-19 admitted to ICU [35]. All steps should be taken cautiously in order to maintain optimal blood glucose levels, and with sensible assessment-based corticosteroid usage.
Contributors
Both authors contributed to the conceptualization, design, writing, and editing of the article and the final approval of this editorial.
Conflict of interest
The authors declare that they have no conflicts of interest.
Funding
No funding was received for the preparation of this editorial.
Provenance and peer review
This editorial was commissioned and was not externally peer reviewed.
Acknowledgments
V.A. and her team are supported by philanthropic funds from Greek Orthodox Archdiocese of Australia, The Pappas Family, and, donors to VU vaccine appeal. V.A would also like to thank the Immunology and Translational Research Group, Institute for Health and Sport, Victoria University for helpful discussions. V.P.C. is grateful to the L.M. College of Pharmacy, Ahmedabad, India, for providing necessary support in carrying out the literature search. The figure in the manuscript was created using Biorender.com.
References
- 1.Čolović N., Arsić-Arsenijević V., Barać A., Suvajdžić N., Leković D., Tomin D. Mucormycosis of the paranasal sinuses in a patient with acute myeloid leukemia. Srp. Arh. Celok. Lek. 2016;144:657–660. [PubMed] [Google Scholar]
- 2.Sharma S., Grover M., Bhargava S., Samdani S., Kataria T. Post coronavirus disease mucormycosis: a deadly addition to the pandemic spectrum. J. Laryngol. Otol. 2021:1–6. doi: 10.1017/S0022215121000992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.deShazo R.D. Fungal sinusitis. Am. J. Med. Sci. 1998;316:39–45. doi: 10.1097/00000441-199807000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Ferguson B.J. Definitions of fungal rhinosinusitis. Otolaryngol. Clin. North Am. 2000;33:227–235. doi: 10.1016/s0030-6665(00)80002-x. [DOI] [PubMed] [Google Scholar]
- 5.Scheckenbach K., Cornely O., Hoffmann T.K., Engers R., Bier H., Chaker A., Greve J., Schipper J., Wagenmann M. Emerging therapeutic options in fulminant invasive rhinocerebral mucormycosis. Auris. Nasus. Larynx. 2010;37:322–328. doi: 10.1016/j.anl.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 6.deShazo R.D., Chapin K., Swain R.E. Fungal sinusitis. N. Engl. J. Med. 1997;337:254–259. doi: 10.1056/NEJM199707243370407. [DOI] [PubMed] [Google Scholar]
- 7.González Ballester D., González-García R., Moreno García C., Ruiz-Laza L., Monje Gil F. Mucormycosis of the head and neck: report of five cases with different presentations. J. Cranio-Maxillo-Facial Surg. Off. Publ. Eur. Assoc. Cranio-Maxillo-Facial Surg. 2012;40:584–591. doi: 10.1016/j.jcms.2011.10.015. [DOI] [PubMed] [Google Scholar]
- 8.Gilada Ishwar. Can spurt in black fungus cases be blamed on industrial oxygen cylinders, dirty water in humidifiers? India Today. 2021 UPDATED: May 27, 2021. https://www.indiatoday.in/coronavirus-outbreak/story/black-fungus-cases-industrial-oxygen-cylinders-humidifiers-covid-19-1807099-2021-05-26 (accessed June 24, 2021) [Google Scholar]
- 9.Maes M., Higginson E., Pereira-Dias J., Curran M.D., Parmar S., Khokhar F., Cuchet-Lourenço D., Lux J., Sharma-Hajela S., Ravenhill B., Hamed I., Heales L., Mahroof R., Soderholm A., Forrest S., Sridhar S., Brown N.M., Baker S., Navapurkar V., Dougan G., Bartholdson Scott J., Conway Morris A. Ventilator-associated pneumonia in critically ill patients with COVID-19. Crit. Care. 2021;25:25. doi: 10.1186/s13054-021-03460-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gangneux J.-P., Bougnoux M.-E., Dannaoui E., Cornet M., Zahar J.R. Invasive fungal diseases during COVID-19: we should be prepared. J. Mycol. Med. 2020;30 doi: 10.1016/j.mycmed.2020.100971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bhatt K., Agolli A., Patel M.H., Garimella R., Devi M., Garcia E., Amin H., Domingue C., Guerra Del Castillo R., Sanchez-Gonzalez M. High mortality co-infections of COVID-19 patients: mucormycosis and other fungal infections. Discov. 2021;9:e126. doi: 10.15190/d.2021.5. Craiova, Rom. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lai C.-C., Wang C.-Y., Hsueh P.-R. Co-infections among patients with COVID-19: the need for combination therapy with non-anti-SARS-CoV-2 agents? J. Microbiol. Immunol. Infect. 2020;53:505–512. doi: 10.1016/j.jmii.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singh A.K., Singh R., Joshi S.R., Misra A. Mucormycosis in COVID-19: A systematic review of cases reported worldwide and in India. Diabetes Metab. Syndr. Clin. Res. Rev. 2021 doi: 10.1016/j.dsx.2021.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baldin C., Ibrahim A.S. Molecular mechanisms of mucormycosis - the bitter and the sweet. PLoS Pathog. 2017;13 doi: 10.1371/journal.ppat.1006408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mehta S., Pandey A. Rhino-orbital mucormycosis associated with COVID-19. Cureus. 2020;12:e10726. doi: 10.7759/cureus.10726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sarkar S., Gokhale T., Choudhury S.S., Deb A.K. COVID-19 and orbital mucormycosis. Indian J. Ophthalmol. 2021;69:1002–1004. doi: 10.4103/ijo.IJO_3763_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.N.C. Sharma, India reports 40,854 cases of black fungus so far, MINT. (2021) Updated: 28 Jun 2021. https://www.livemint.com/news/india-records-over-40k-cases-of-mucormycosis-11624875874985.html (accessed July 2, 2021).
- 18.M. Sen, Black fungus, live mint. (2021) Updated: 07 Jun 2021. https://www.livemint.com/news/india/black-fungus-28-states-see-28-252-mucormycosis-cases-maharashtra-gujarat-among-worst-hit-states-11623069135171.html (accessed June 24, 2021).
- 19.Sen M., Lahane S., Lahane T.P., Parekh R., Honavar S.G. Mucor in a viral land: a tale of two pathogens. Indian J. Ophthalmol. 2021;69:244–252. doi: 10.4103/ijo.IJO_3774_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Werthman-Ehrenreich A. Mucormycosis with orbital compartment syndrome in a patient with COVID-19. Am. J. Emerg. Med. 2021;42:264.e5–264.e8. doi: 10.1016/j.ajem.2020.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Revannavar S.M., Supriya P.S., Samaga L., Vineeth V.K. COVID-19 triggering mucormycosis in a susceptible patient: a new phenomenon in the developing world? BMJ Case Rep. 2021;14 doi: 10.1136/bcr-2021-241663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hanley B., Naresh K.N., Roufosse C., Nicholson A.G., Weir J., Cooke G.S., Thursz M., Manousou P., Corbett R., Goldin R., Al-Sarraj S., Abdolrasouli A., Swann O.C., Baillon L., Penn R., Barclay W.S., Viola P., Osborn M. Histopathological findings and viral tropism in UK patients with severe fatal COVID-19: a post-mortem study. Lancet. Microbe. 2020;1:e245–e253. doi: 10.1016/S2666-5247(20)30115-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahmadikia K., Hashemi S.J., Khodavaisy S., Getso M.I., Alijani N., Badali H., Mirhendi H., Salehi M., Tabari A., Mohammadi Ardehali M., Kord M., Roilides E., Rezaie S. The double-edged sword of systemic corticosteroid therapy in viral pneumonia: a case report and comparative review of influenza-associated mucormycosis versus COVID-19 associated mucormycosis. Mycoses. 2021 doi: 10.1111/myc.13256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Skiada A., Pavleas I., Drogari-Apiranthitou M. Epidemiology and diagnosis of mucormycosis: an update. J. Fungi (Basel, Switzerland) 2020;6:265. doi: 10.3390/jof6040265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Szarpak L., Chirico F., Pruc M., Szarpak L., Dzieciatkowski T., Rafique Z. Mucormycosis - a serious threat in the COVID-19 pandemic? J. Infect. 2021 doi: 10.1016/j.jinf.2021.05.015. S0163-4453(21)00257–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Highlights: UK Records 2, 829 New Covid-19 Cases, 9 More Deaths, Hindustan Times. (2021) UPDATED ON MAY 22, 2021. https://www.hindustantimes.com/india-news/covid19-coronavirus-latest-updates-death-toll-india-world-may-21-2021-101621559755794.html (accessed June 28, 2021).
- 27.Prakash H., Chakrabarti A. Global epidemiology of mucormycosis. J. Fungi (Basel, Switzerland) 2019;5:26. doi: 10.3390/jof5010026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reliefweb; 2021. Epidemiological Alert: COVID-19 Associated Mucormycosis.https://reliefweb.int/report/brazil/epidemiological-alert-covid-19-associated-mucormycosis Originally published: 11 Jun 2021. accessed June 28, 2021. [Google Scholar]
- 29.Kamruzzaman Md. Anadolu Agency; 2021. Bangladesh Detects 2 Cases of Black Fungus in Capital.https://www.aa.com.tr/en/asia-pacific/bangladesh-detects-2-cases-of-black-fungus-in-capital/2253078 25.05.2021. (accessed June 28, 2021) [Google Scholar]
- 30.Times of India; 2021. 2 Dead and 11 Suffering from Black Fungus in Nepal. Jun 8, 2021https://timesofindia.indiatimes.com/world/south-asia/2-dead-and-11-suffering-from-black-fungus-in-nepal/articleshow/83334621.cms#:~:text=Mucormycosis affects the brain%2C sinuses,in Nepal and neighbouring India. (accessed June 28, 2021) [Google Scholar]
- 31.Elinav H., Zimhony O., Cohen M.J., Marcovich A.L., Benenson S. Rhinocerebral mucormycosis in patients without predisposing medical conditions: a review of the literature. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2009;15:693–697. doi: 10.1111/j.1469-0691.2009.02884.x. [DOI] [PubMed] [Google Scholar]
- 32.Spellberg B., Walsh T.J., Kontoyiannis D.P., Edwards J.J., Ibrahim A.S. Recent advances in the management of mucormycosis: from bench to bedside. Clin. Infect. Dis. an Off. Publ. Infect. Dis. Soc. Am. 2009;48:1743–1751. doi: 10.1086/599105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patel A, Agarwal R, Rudramurthy SM, Shevkani M, Xess I, Sharma R, et al. Emerg Infect Dis. 2021 Sep. MucoCovi network. Multicenter epidemiologic study of coronavirus disease–associated mucormycosis, India. [date cited](n.d.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Raut A., Huy N.T. Rising incidence of mucormycosis in patients with COVID-19: another challenge for India amidst the second wave? Lancet Respir. Med. 2021 doi: 10.1016/S2213-2600(21)00265-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yang S., Hua M., Liu X., Du C., Pu L., Xiang P., Wang L., Liu J. Bacterial and fungal co-infections among COVID-19 patients in intensive care unit. Microbes Infect. 2021;23 doi: 10.1016/j.micinf.2021.104806. [DOI] [PMC free article] [PubMed] [Google Scholar]