Abstract
From the beginning of the COVID-19 pandemic, the world stands idly by in the face of the virus spreading. The prediction of highly vulnerable population and the implementation of proper actions are very important steps to break the infection chain of any virus. This will, in turn, reduce the economic and social impact of this virus outbreak. In this study, the COVID-19 vulnerability map for the West Bank, Palestine was developed. Analytic Hierarchy Process (AHP) was used to develop the COVID-19 vulnerability map. The Geographic Information system (GIS) in combination with multi-criteria decision analysis (MCDA) was adopted to estimate the COVID-19 vulnerability index (CVI) based on some selected potential criteria including population, population density, elderly population, accommodation and food service activities, school students, chronic diseases, hospital beds, health insurance, and pharmacy. The results of this study show that Nablus, Jerusalem, and Hebron governorates are under very high vulnerability. Tulkarm, Ramallah & Al-Bireh and Jenin governorates are high vulnerable to COVID-19. Additionally, 82 % of the West Bank population are under high to very high COVID-19 vulnerability classes. Moreover, 14% and 4 % are medium and low to very low vulnerable, respectively. The obtained results are of high value to help decision-makers to take proper actions as early as possible mainly in the highly COVID-19 vulnerable governorates to control the risk associated with the potential outbreak of the virus and accordingly to protect social life and to sustain economic conditions.
Keywords: COVID-19, GIS, AHP, Vulnerability mapping, West Bank, Vulnerability index, MCDA
1. Introduction
In early 2020, different countries all over the world have been vulnerable to the speared of Coronavirus (SARS-CoV-2, COVID-19) [1]. Worldwide, the spreading of the COVID-19 virus was uncontrolled and subsequently became a pandemic that has a very serious health issue [[2], [3], [4]]. Thus, the COVID-19 spreading was affecting different aspects of life in many countries of the world [5].
The first case of COVID-19 has been confirmed in China (Wuhan) [6]. However, the virus was quickly spread and within a couple of months, confirmed cases were recorded in most of the world countries [1]. Moreover, on 13 July, COVID-19 extends to different countries and causing 569,128 deaths [7]. COVID-19 is an infectious virus, causes an acute respiratory syndrome that quickly updated into a deadly disease with a mortality rate of about 1.38% [1,8].
In Palestine (West Bank and Gaza Strip), the COVID-19 was firstly recorded in March 2020 in the Bethlehem governorate [9]. The number of infected people was increased and reached 630 cases and 5 deaths on June 2nd, 2020 [10]. However, the number of confirmed cases and the mortality rate were less compared to the other countries in the region until the second outbreak in July 2020 [11]. From the beginning of the pandemic mainly on the March 5, 2020, the Palestinian government announced the state of emergency and implied serious precautions to control the spreading of COVID-19 in Palestine. Additionally, on March 22, the mobility between the different governorates was stopped. Schools, universities, and most business activities were closed and the government asking the people to stay at home for 14 days [12]. Wearing masks and using sterilizers every 15–20 min is essential to reduce the COVID-19 outbreak. Additionally, keep social distance and avoid crowded places is very important to decrease the COVID-19 vulnerable population [[13], [14], [15]].
For any disaster (e.g. the outbreak of COVID-19), local communities are potentially vulnerable to maximum risk [16,17]. The social vulnerability to the influence of any disaster is usually spatially distributed [18,19]. However, social vulnerability is a dynamic process that is highly dependent on the government's actions and mitigation plans [20]. Thus, the improper or slow reaction from the government might turn less vulnerable communities into highly vulnerable ones [20].
Vulnerability is defined as the situation where the risk of exposure to the hazard of a certain community might be increased [21]. For a certain health risk, vulnerability mapping is a commonly used method that implies the use of multiple driving parameters to classify a certain community into different health vulnerability classes [22].
Different studies have discussed the mapping of epidemic prediction depending on multiple criteria analysis [23]. In the vulnerability mapping of COVID-19, the multiple criteria were often considered through the implementation of the multi-criteria decision analysis (MCDA) approach [24]. Driving factors for the mapping of COVID-19 are generally driven by different parameters such as: demographic (e.g., population), epidemiological (e.g., chronic diseases), and ecological/physical (e.g., temperature) [19,[25], [26], [27]]. Analytic Hierarchy Process (AHP) is the most commonly used MCDA approach [28]. The AHP is a well-organized approach for assigning reasonable weights of different influential criteria. The geographic information systems (GIS) based-MCDA is a professional way to map epidemic vulnerability and risk assessment (e.g. COVID-19 vulnerability) [[29], [30], [31], [32], [33]]. In this study, GIS-based MCDA was used to develop the COVID-19 vulnerability index (CVI) which was subsequently utilized to classify the West Bank governorates into different COVID-19 vulnerability classes.
This research aims to develop the COVID-19 vulnerability map for the West Bank. The developed map is of high value to guide decision-makers in the prediction of COVID-19 potential outbreaks and accordingly to develop proper mitigation measures to protect public health mainly in the highly vulnerable governorates.
2. Materials and methods
2.1. Study area
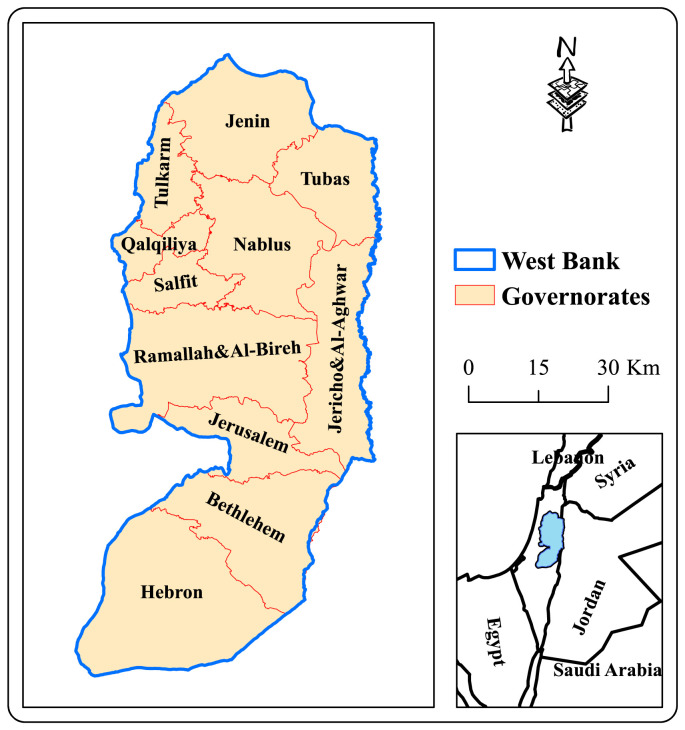
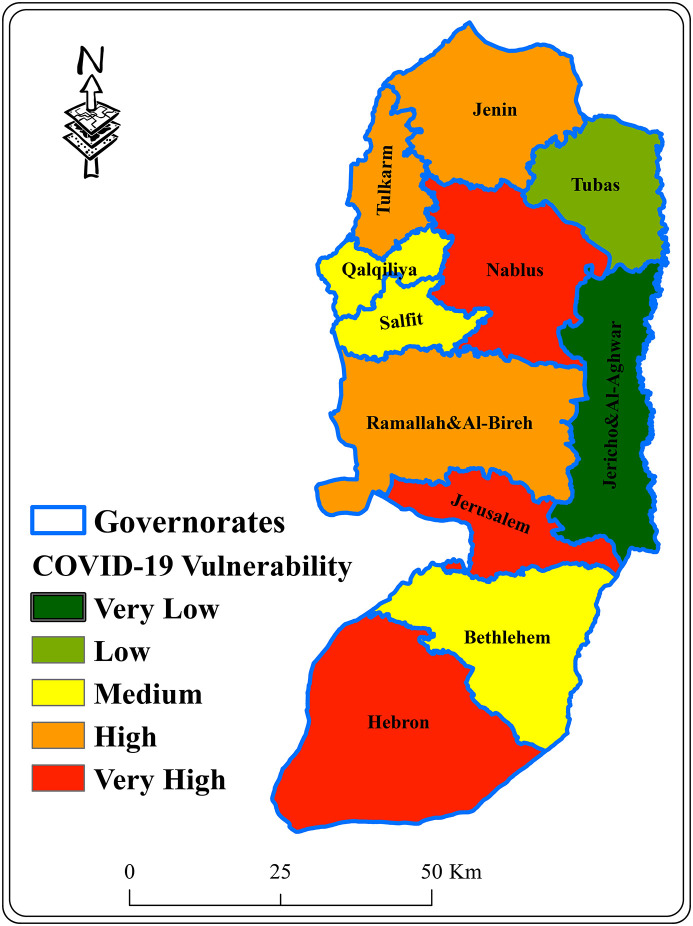
This study was accomplished in the West Bank, Palestine that has a total population of 2.9 million [34]. Administratively, West Bank is divided into 11 governorates. Jerusalem, Jenin, Tubas, Nablus, Tulkarm, Qalqiliya, Salfit, Jericho & Al-Aghwar, Ramallah & Al-Bireh, Bethlehem, and Hebron (see Fig. 1 ). However, Hebron has the highest population number and Jericho & Al-Aghwar has the lowest one. The highest and lowest population densities are in Jerusalem and Jericho & Al-Aghwar governorates, respectively.
Fig. 1.
Location map of the West Bank, Palestine.
Generally, the health system in Palestine is weak and suffers from a lack of resources and financing [35]. In the West Bank, there exist 255 adult intensive care unit (ICU) beds and 175 ventilators in private and government hospitals [12]. The total number of hospitals is 52 (including East Jerusalem), among which 29 are general hospitals [36].
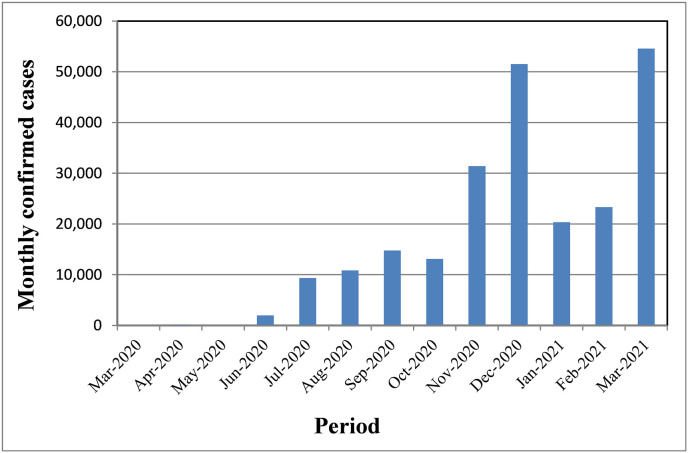
COVID-19 was firstly outbreak in the Bethlehem governorate, in March 2020. The monthly confirmed cases do not exceed 211 until May 2020. In July 2020, the second outbreak started and the confirmed cases reached about 14,000. The third outbreak has been started in December 2020 where the number of monthly confirmed cases exceeded 51,000 [37]. Figure (2) illustrates the distribution of monthly confirmed cases in Palestine (West Bank and Gaza excluding Jerusalem City) since the start of the COVID-19 pandemic. Most confirmed cases (88 %) are due to community transmission [37].
Fig. 2.
Monthly variation of COVID-19 confirmed cases in Palestine.
2.2. Methodology
In this study, the COVID-19 vulnerability map was obtained based on the development of the CVI map. Nine influential criteria were selected in the development of the CVI map (see Table 1 ). These criteria were driven from the data of population, services, health care, and epidemiological.
Table 1.
CVI criteria.
| Criteria | Description | Data Source |
|---|---|---|
| P | Number of the population | [34] |
| PD | Population per kmb | |
| EP | Number of the population more than 65 years old (per 10,000 population) | |
| HI | Number of health insured people (per 10,000 population) a | |
| AF | Number of accommodation and food service activities (per 10,000 population) | [38] |
| SS | Number of school students in the year 2017/2018 (per 10,000 population) b | [39] |
| CD | Number of the population diagnosed with chronic diseases (per 10,000 population) a | [40] |
| HB | Number of hospital beds (per 10,000 population) | [36] |
| Ph | Number of pharmacies (per 10,000 population) |
Data exclude those parts of Jerusalem which were annexed by the Israeli Occupation in 1967.
The data do not include the Israeli Municipality and Culture Committee Schools in Jerusalem.
The selected criteria include population (P), population density (PD), the elderly people (EP), accommodation and food service activities (AF), school students (SS), chronic diseases (CD), hospital beds (HB), health insurance (HI), and pharmacy (Ph). These criteria were selected based on their eligibility to increase (P, PD, EP, AF, SS, and CD) or decrease (HB, HI, and Ph) the COVID-19 vulnerability.
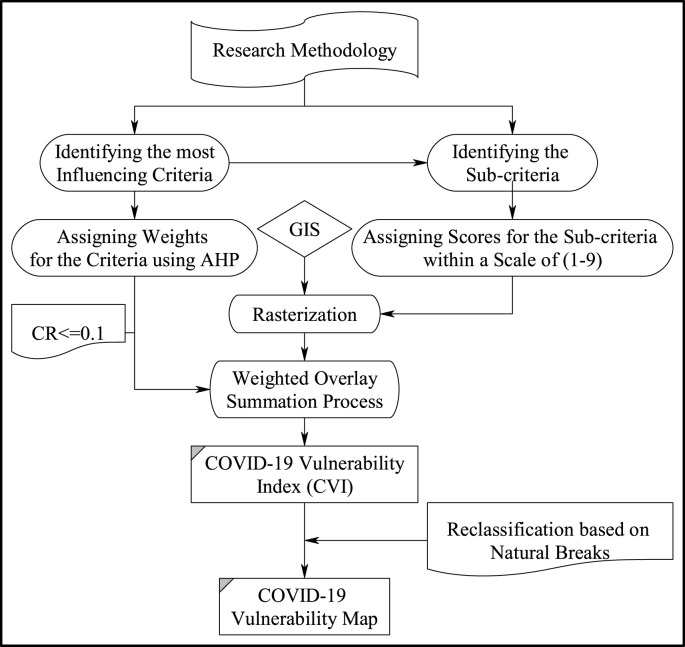
The overall methodological approach for developing of COVID-19 vulnerability map is presented in Fig. 3 .
Fig. 3.
The overall methodological approach.
To assign weights for the different CVI criteria, the AHP pairwise comparison matrix approach as introduced by Ref. [41] was used (see Table 2 ). Subsequently, these assigned weights were tested for consistency by computing a consistency ratio (CR) as follows [41]:
where CI is the consistency index, RI is a random consistency index that depends on the number of criteria, λ is the maximum eigenvector of the matrix, and n is the number of criteria.
Table 2.
AHP pairwise comparison matrix for the CVI of the West Bank.
| Criteria | P | PD | EP | SS | HB | HI | Ph | AF | CD | Weight |
|---|---|---|---|---|---|---|---|---|---|---|
| P | 1.0 | 0.3 | 4.0 | 2.0 | 2.0 | 3.0 | 2.0 | 2.0 | 3.0 | 0.15 |
| PD | 3.0 | 1.0 | 3.0 | 3.0 | 4.0 | 4.0 | 3.0 | 4.0 | 3.0 | 0.22 |
| EP | 0.3 | 0.3 | 1.0 | 0.5 | 2.0 | 3.0 | 3.0 | 2.0 | 2.0 | 0.11 |
| SS | 0.5 | 0.3 | 2.0 | 1.0 | 3.0 | 4.0 | 5.0 | 3.0 | 4.0 | 0.18 |
| HB | 0.5 | 0.3 | 0.5 | 0.3 | 1.0 | 2.0 | 2.0 | 0.2 | 2.0 | 0.07 |
| HI | 0.3 | 0.3 | 0.3 | 0.3 | 0.5 | 1.0 | 2.0 | 0.2 | 0.5 | 0.04 |
| Ph | 0.5 | 0.3 | 0.3 | 0.2 | 0.5 | 0.5 | 1.0 | 0.2 | 0.3 | 0.03 |
| AF | 0.5 | 0.3 | 0.5 | 0.3 | 5.0 | 5.0 | 5.0 | 1.0 | 2.0 | 0.15 |
| CD | 0.3 | 0.3 | 0.5 | 0.3 | 0.5 | 2.0 | 0.5 | 0.5 | 1.0 | 0.05 |
The allowable value of CR should not exceed 0.1 [42]. In this study, a CR value of 0.09 was obtained. This indicates that the CVI criteria matrix is consistent.
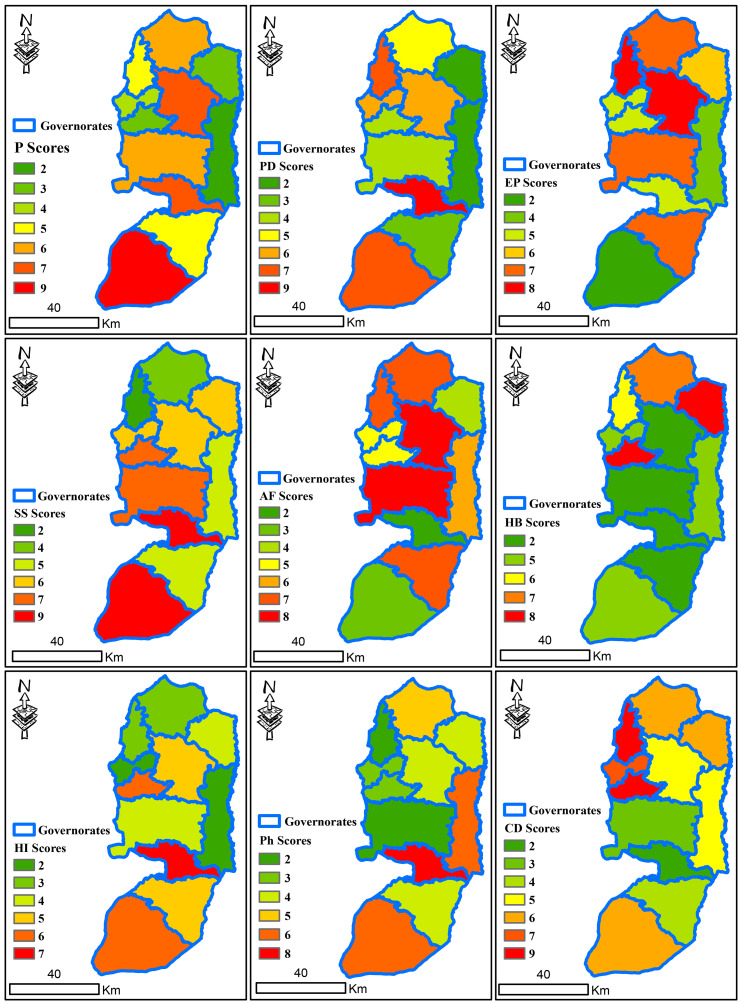
Each criterion used in the CVI map was classified into seven value classes, each of them was assigned a score from 1 (less important) to 9 (high important) (see Table 3 ) [41]. The selected criteria were rasterized and reclassified using different GIS (ArcMap 10.1) tools (See Fig. 4 ).
Table 3.
CVI Scoring for the different Sub-criteria in the West Bank.
| # | Criteria | Sub-criteria | Score |
|---|---|---|---|
| 1 | P | <50,002 | 2 |
| 50,002–75,444 | 3 | ||
| 75,444–112,400 | 4 | ||
| 112,400–217,400 | 5 | ||
| 217,400–328,861 | 6 | ||
| 328,861–435,753 | 7 | ||
| ≥435,753 | 9 | ||
| 2 | PD | <152 | 2 |
| 152–330 | 3 | ||
| 330–384 | 4 | ||
| 384–540 | 5 | ||
| 540–676 | 6 | ||
| 676–759 | 7 | ||
| ≥759 | 9 | ||
| 3 | EP | <256 | 2 |
| 256–315 | 3 | ||
| 315–326 | 4 | ||
| 326–359 | 5 | ||
| 359–372 | 6 | ||
| 372–402 | 7 | ||
| ≥402 | 8 | ||
| 4 | SS | <2466 | 2 |
| 2466–2483 | 3 | ||
| 2483–2491 | 4 | ||
| 2491–2598 | 5 | ||
| 2598–2639 | 6 | ||
| 2639–2747 | 7 | ||
| ≥2747 | 9 | ||
| 5 | AF | <11.4 | 2 |
| 11.4–13.7 | 3 | ||
| 13.7–19.6 | 4 | ||
| 19.6–21.2 | 5 | ||
| 21.2–23.7 | 6 | ||
| 23.7–25.8 | 7 | ||
| ≥25.8 | 8 | ||
| 6 | HB | <6.4 | 9 |
| 6.4–7.0 | 8 | ||
| 7.0–8.8 | 7 | ||
| 8.8–9.3 | 6 | ||
| 9.3–10.5 | 5 | ||
| 10.5–16.1 | 3 | ||
| ≥16.1 | 2 | ||
| 7 | HI | <5753 | 8 |
| 5753–5824 | 7 | ||
| 5824–6132 | 6 | ||
| 6132–6593 | 5 | ||
| 6593–7023 | 4 | ||
| 7023–7494 | 3 | ||
| ≥7494 | 2 | ||
| 8 | Ph | <2.1 | 8 |
| 2.1–3.4 | 7 | ||
| 3.4–3.8 | 6 | ||
| 3.8–4.1 | 5 | ||
| 4.1–4.4 | 4 | ||
| 4.4–4.7 | 3 | ||
| ≥4.7 | 2 | ||
| 9 | CD | <182 | 2 |
| 182–222 | 3 | ||
| 222–242 | 4 | ||
| 242–279 | 5 | ||
| 279–421 | 6 | ||
| 421–463 | 7 | ||
| ≥463 | 9 |
Fig. 4.
The scored grids of the nine criteria for the West Bank.
GIS was employed to estimate the CVI through the use of the weighted overlay summation process [42] for the different selected criteria by aggregating the weighted cell values together. Each input layer (criteria) was multiplied by its assigned weight and the results are summed as:
where CVI is the final cell index, Wi is a normalized weight (∑Wi = 1), Sij is the score of the ith cell for the jth layer, and n is the number of cells in each jth layer.
Finally, the total CVI through natural breaks (Jenks) in GIS was used to develop the COVID-19 vulnerability map for the entire West Bank.
3. Results and discussion
3.1. COVID-19 vulnerability map
Based on the previous approach and depending on the selected CVI criteria, the COVID-19 vulnerability map for the West Bank was developed (see Fig. 5 ). The developed map was classified the West Bank governorates into five different COVID-19 vulnerability classes (very low, low, medium, high, and very high). Furthermore, the total number of population under different COVID-19 vulnerability classes in the West Bank is presented in Table 4 .
Fig. 5.
COVID-19 Vulnerability map for the West Bank.
Table 4.
COVID-19 Vulnerable population in the West Bank.
| COVID-19 vulnerability class | The population may be affected | The percentage from total West Bank population (%) |
|---|---|---|
| Very low | 50,002 | 2 |
| Low | 60,927 | 2 |
| Medium | 405,244 | 14 |
| High | 830,487 | 29 |
| Very high | 1,535,297 | 53 |
| Total | 2,881,957 | 100 |
From Fig. 5 and Table 4, almost 82 % of the total West Bank population are under high (Tulkarm, Ramallah & Al-Bireh and Jenin governorates) to very high (Nablus, Jerusalem, and Hebron governorates) COVID-19 potential vulnerability conditions. Moreover, Tubas and Jericho & Al-Aghwar are under low to very low vulnerability conditions (4 % of the total West Bank population). Additionally, the medium vulnerability class covers nearly 14 % of the total West Bank population in the governorates of Qalqiliya, Salfit, and Bethlehem.
3.2. Validation
The total number of confirmed, recovered, death, and active COVID-19 cases in the different West Bank governorates from the first outbreak in March 2020 to March 28, 2021 are presented in Table 5 [37]. From Table 5, it is clear that the total number of confirmed cases is 202,006 (7 % of the total West Bank population). However, nearly 53 % of these cases are confirmed in Hebron, Jerusalem, and Nablus governorates. This can be attributed to the high population number in Hebron, the high population density in Jerusalem, and the high number of accommodation and food service activities in Nablus. The highest number of active cases is in the Nablus governorate (13 cases per 1000 population). This is because of the high number of AF (26 per 10,000) and EP (403 per 10,000 population). According to the table, the mortality rate of COVID-19 in the West Bank is nearly 1 % (death to confirmed cases). The highest value of mortality rate in the Qalqiliya governorate (15 per 1000 confirmed cases) and the lowest one in the Jerusalem governorate (9 per 1000 confirmed cases). This can be attributed to the relatively high number of the population diagnosed as CD in these governorates. Based on Table (5) and Fig. (5), 81 % of confirmed cases in the West Bank are in the areas that were classified as high to very high vulnerable governorates. Additionally, 82 % and 80 % of active and death cases, respectively are within these areas.
Table 5.
COVID-19 in the West bank.
| Governorate | Cases |
|||
|---|---|---|---|---|
| Confirmed | Recovered | Death | Active | |
| Jenin | 15,083 | 12,809 | 208 | 2066 |
| Tubas | 3856 | 3526 | 43 | 287 |
| Tulkarm | 12,431 | 10,245 | 169 | 2017 |
| Nablus | 27,278 | 21,906 | 313 | 5059 |
| Qalqiliya | 7129 | 6003 | 108 | 1018 |
| Salfit | 6593 | 6158 | 69 | 366 |
| Ramallah & Al-Bireh | 28,808 | 27,008 | 281 | 1519 |
| Jericho & Al-Aghwar | 4092 | 3762 | 43 | 287 |
| Jerusalem | 38,895 | 36,974 | 340 | 1581 |
| Bethlehem | 16,705 | 15,076 | 194 | 1435 |
| Hebron | 41,136 | 37,723 | 467 | 2946 |
| Total | 202,006 | 181,190 | 2235 | 18,581 |
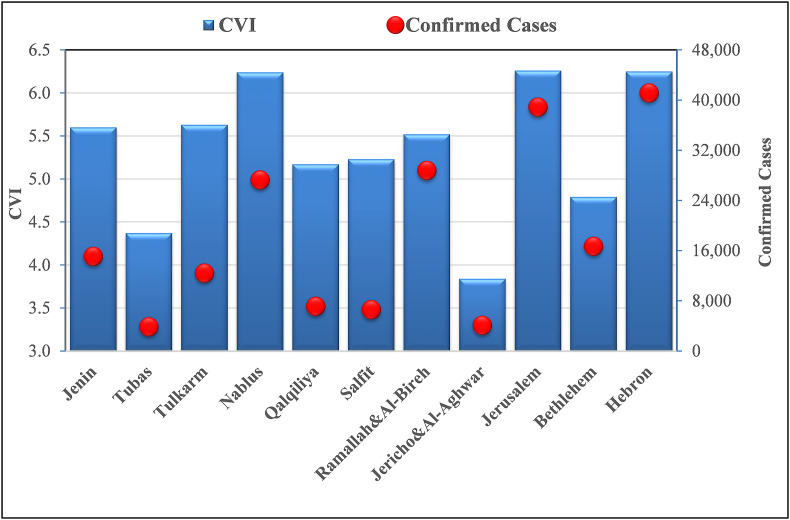
Fig. 6 presents the CVI and confirmed cases in the different West Bank governorates. According to the figure, the governorates with very high CVI values (Nablus, Jerusalem, and Hebron) reported the highest number of confirmed cases. Additionally, Tubas and Jericho & Al-Aghwar governorates have the lowest CVI values. Thus, they reported the lowest number of confirmed cases. The CVI in the Tulkarm governorate (5.63) is high but the number of confirmed cases is relatively low. This can be attributed to the low number of COVID-19 laboratory tests (from March 5, 2020 to March 28, 2021) where the number of tests in Tulkarm governorates is nearly 28 per 100 capita. In comparison, the number of tests is 64 per 100 capita in Ramallah & Al-Bireh. Therefore, the confirmed cases in Ramallah & Al-Bireh are very high whereas the CVI is relatively high. However, the number of confirmed cases is highly related to socio-economic conditions such as poor households [19] employment [43], car ownership [26], and household density [44]. Thus, the obtained CVI values do not reflect the actual number of the confirmed cases in all of the West Bank governorates.
Fig. 6.
CVI and COVID-19 confirmed cases in the different West Bank governorates.
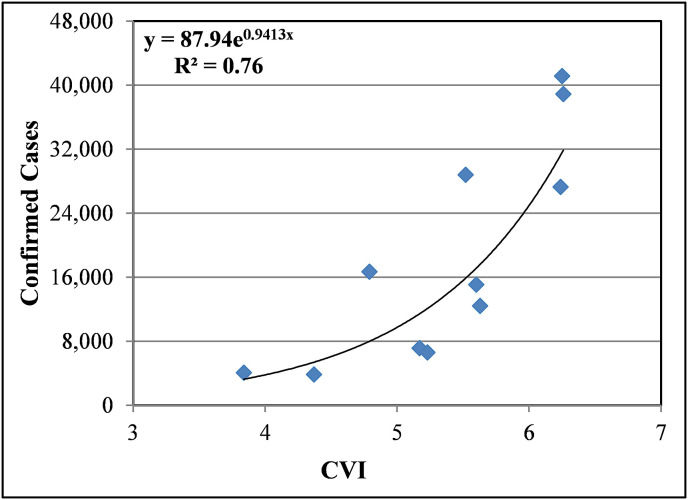
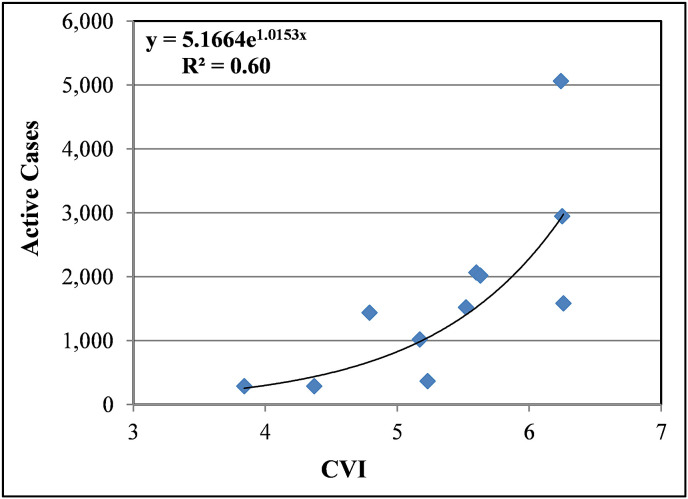
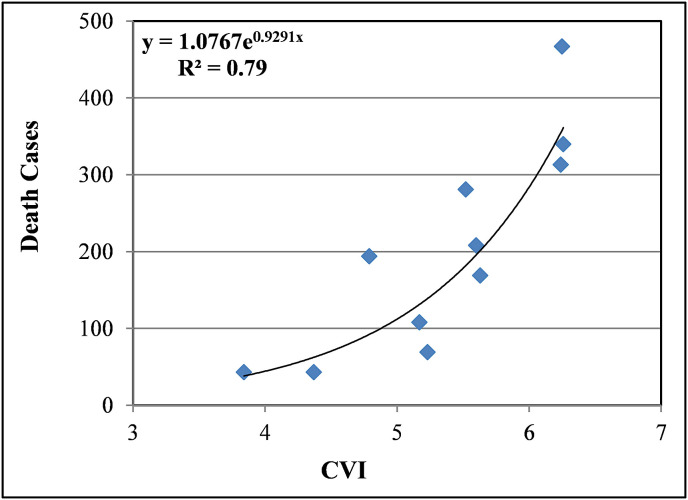
Additionally, the CVI values versus confirmed, active, and death cases were plotted (see Fig. 7, Fig. 8, Fig. 9 ). However, the relations were estimated based on data presented in Table 5. From the figures, it is clear that there is a positive exponential trend between CVI values and the number of confirmed cases, active and death cases with R2 values of 0.76, 0.60, and 0.79, respectively. Accordingly, the number of confirmed, active, and death cases were exponentially increased with the increase of CVI values.
Fig. 7.
Relation between CVI and COVID-19 confirmed cases.
Fig. 8.
Relation between CVI and COVID-19 active cases.
Fig. 9.
Relation between CVI and COVID-19 death cases.
4. Conclusions
In this study, the COVID-19 vulnerability map for the West Bank was developed based on the CVI values that were obtained by utilizing the GIS-based MCDA. Nine influential criteria were selected; population, population density, elderly population, accommodation and food service activities, school students, chronic diseases, hospital beds, health insurance, and pharmacy. AHP pairwise comparison matrix was adopted to assigning weights for these criteria. The GIS was used to classify the CVI values of the West Bank into five COVID-19 vulnerability classes (very low, low, medium, high, and very high). The results of this study concluded that 82 % of the West Bank population are under high to very high COVID-19 vulnerability classes. Therefore, these governorates will suffer from the potential negative consequences of COVID-19 more than other governorates unless the Palestinian government acts early to apply serious precaution measures to protect population in these areas.
The developed map will help the decision-makers in the prediction of COVID-19 potential spreading in the different West Bank governorates. Thus, develop more efficient preparedness plans and mitigation measures to reduce the potential economic, social, and health impacts of the COVID-19 outbreak in the West Bank in the future. Therefore, the number of infected people will be under control, and as such to avoid failure health system in Palestine. Finally, ongoing research might introduce new facts and criteria that have to be considered to improve the developed COVID-19 vulnerability map to successfully predict the future COVID-19 outbreak in Palestine, if any.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.WHO . 2020. Coronavirus Disease 2019 (COVID-19): Situation Report-72. [Google Scholar]
- 2.WHO . 2020. Coronavirus Disease 2019 (COVID-19): Situation Report-91. [Google Scholar]
- 3.WHO . 2020. Coronavirus Disease 2019 (COVID-19): Situation Report-51. [Google Scholar]
- 4.WHO . 2020. Coronavirus Disease 2019 (COVID-19): Situation Report-30. [Google Scholar]
- 5.Gralinski L.E., Menachery V.D. Return of the coronavirus: 2019-nCoV. Viruses. 2020;12:135. doi: 10.3390/v12020135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO . 2019. Novel Coronavirus (2019-nCoV): Situation Report-1. [Google Scholar]
- 7.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real-time. Lancet Infect. Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Verity R., Okell L.C., Dorigatti I., Winskill P., Whittaker C., Imai N., et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect. Dis. 2020;20 doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Muhareb R., Giacaman R. Tracking COVID-19 responsibly. Lancet. 2020;0(0) doi: 10.1016/S0140-6736(20)30693-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.AlKhaldi M., Kaloti R., Shella D., Al Basuoni A., Meghari H. Health system's response to the COVID-19 pandemic in conflict settings: policy reflections from Palestine. Global Publ. Health. 2020;15(8):1244–1256. doi: 10.1080/17441692.2020.1781914. [DOI] [PubMed] [Google Scholar]
- 11.WHO . 2020. Ethical Standards for Research during Public Health Emergencies: Distilling Existing Guidance to Support COVID-19 R&D. [Google Scholar]
- 12.Palestinian Authority . Ramallah, Palestine; 2020. State of Emergency: Palestine’s COVID-19 Response Plan. [Google Scholar]
- 13.Russell C.D., Millar J.E., Baillie J.K. Clinical evidence does not support corticosteroid treatment for 2019-ncov lung injury. Lancet. 2020;395:473–475. doi: 10.1016/S0140-6736(20)30317-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang L.L.Y. Potential interventions for novel coronavirus in China: a systemic review. J. Med. Virol. 2020;92:479–490. doi: 10.1002/jmv.25707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xu X., Wu X., Jiang X., et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan. China: Retrospective case series. BMJ. 2020;368:m606. doi: 10.1136/bmj.m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Palaiologou P., Ager A.A., Nielsen-Pincus M., Evers C.R., Day M.A. Social vulnerability to large wildfires in the western USA. Landsc. Urban Plann. 2019;189:99–116. [Google Scholar]
- 17.Rufat S., Tate E., Burton C.G., Maroof A.S. Social vulnerability to floods: a review of case studies and implications for measurement. Int. J. Disaster Risk Reduct. 2015;14(4):470–486. [Google Scholar]
- 18.Ramchand R., Seelam R., Parks V., Ghosh-Dastidar B., Lee M.R., Finucane M. Exposure to the Deepwater Horizon Oil Spill, associated resource loss, and long-term mental and behavioral outcomes. Disaster Med. Public Health Prep. 2019;13:889–897. doi: 10.1017/dmp.2019.3. [DOI] [PubMed] [Google Scholar]
- 19.Acharya R., Porwal A. A vulnerability index for the management of and response to the COVID-19 epidemic in India: an ecological study. Lancet Glob. Heal. 2020;8:e1142–e1151. doi: 10.1016/S2214-109X(20)30300-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lancet T. Redefining vulnerability in the era of COVID-19. Lancet. 2020;395:1089. doi: 10.1016/S0140-6736(20)30757-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holand I.S., Lujala P., Rod J.K. Social vulnerability assessment for Norway: a quantitative approach. Nor. Geografisk Tidsskr. 2011;65(1):1–17. [Google Scholar]
- 22.Flanagan B.E., Hallisey E.J., Adams E., Lavery A. Measuring community vulnerability to natural and anthropogenic hazards: the centers for disease control and prevention's social vulnerability index. J. Environ. Health. 2018;80:34. [PMC free article] [PubMed] [Google Scholar]
- 23.Chretien J.P., George D., Shaman J., Chitale R.A., McKenzie F.E. Influenza forecasting in human populations: a scoping review. PLoS One. 2014;9(4) doi: 10.1371/journal.pone.0094130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sangiorgio V., Parisi F. A multicriteria approach for risk assessment of Covid-19 in urban district lockdown. Saf. Sci. 2020;130:104862. doi: 10.1016/j.ssci.2020.104862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Meraj G., Farooq M., Singh S.K., Romshoo S.A., Nathawat M.S., Kanga S. Coronavirus pandemic versus temperature in the context of Indian subcontinent: a preliminary statistical analysis. Environ. Dev. Sustain. 2021;23(4):6524–6534. doi: 10.1007/s10668-020-00854-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Macharia P.M., Joseph N.K., Okiro E.A. A vulnerability index for COVID-19: spatial analysis at the subnational level in Kenya. BMJ Public Health. 2020;5 doi: 10.1136/bmjgh-2020-003014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schoeman D., Fielding B.C. Coronavirus envelope protein: current knowledge. Virol. J. 2019;16(1):69. doi: 10.1186/s12985-019-1182-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Saaty T. A scaling method for priorities in hierarchical structures. J. Math. Psychol. 1977;15:234–281. [Google Scholar]
- 29.Cox R., Sanchez J., Revie C.W. Multi-criteria decision analysis tools for prioritizing emerging or re-emerging infectious diseases associated with climate change in Canada. PLoS One. 2013;8 doi: 10.1371/journal.pone.0068338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Paul M.C., Goutard F.L., Roulieau F., Holl D., Thanapongtharm W., Roger F.L., Tran A. Quantitative assessment of a spatial multicriteria model for highly pathogenic avian influenza H5N1in Thailand, and application in Cambodia. Sci. Rep. 2016;6:31096. doi: 10.1038/srep31096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kanga S., Sudhanshu Meraj G., Farooq M., Nathawat M.S., Singh S.K. Reporting the management of COVID-19 threat in India using remote sensing and GIS based approach. Geocarto Int. 2020:1–8. [Google Scholar]
- 32.Ranga V., Pani P., Kanga S., Meraj G., Farooq M., Nathawat M.S., Singh S.K. 2020. National Health-GIS Portal-A Conceptual Framework for Effective Epidemic Management and Control in India. [Google Scholar]
- 33.Kanga S., Meraj G., Farooq M., Nathawat M.S., Singh S.K. Risk Analysis; 2021. Analyzing the Risk to COVID‐19 Infection Using Remote Sensing and GIS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Palestinian Central Bureau of Statistics . 2018. Population, Housing, and Establishments Census 2017: Census Final Results - Summary. Ramallah, Palestine. [Google Scholar]
- 35.AlKhaldi M., Kaloti R., Shella D., Al Basuoni A., Meghari H. Health system's response to the COVID-19 pandemic in conflict settings: policy reflections from Palestine. Global Publ. Health. 2020;15:1–13. doi: 10.1080/17441692.2020.1781914. [DOI] [PubMed] [Google Scholar]
- 36.Ministry of Health . 2020. Annual Health Report, Palestine-2019. Ramallah, Palestine. [Google Scholar]
- 37.Ministry of Health . 2021. CORONAVIRUS-COVID19 Surveillance System. Ramallah, Palestine. [Google Scholar]
- 38.Palestinian Central Bureau of Statistics . 2017. Final Result of Population, Housing, and Establishment Census. Ramallah, Palestine. [Google Scholar]
- 39.Ministry of Education . 2020. Database of Education Survey for the Scholastic Years 2014/2015-2019/2020. Ramallah, Palestine. [Google Scholar]
- 40.Ministry of Health . 2017. Primary Health Care Annual Report. Ramallah, Palestine. [Google Scholar]
- 41.Saaty T.L. McGraw-Hill International Book Co.; New York: 1980. The Analytic Hierarchy Process: Planning, Priority Setting, Resource Allocation. [Google Scholar]
- 42.Malczewski J. Wiley; New York: 1999. GIS and Multi-Criteria Decision Analysis; p. 392. [Google Scholar]
- 43.Snyder B.F., Parks V. Spatial variation in socio-ecological vulnerability to Covid-19 in the contiguous United States. Health Place. 2020;66:102471. doi: 10.1016/j.healthplace.2020.102471. [DOI] [PubMed] [Google Scholar]
- 44.Sarkar A., Chouhan P. COVID-19: district level vulnerability assessment in India. Clin. Epidemiol. Global. Health. 2021;9:204–215. doi: 10.1016/j.cegh.2020.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]