Abstract
Objective
Our objective was to quantify the associations between sleep duration and perceived and chronic stress with ideal cardiovascular health (CVH) among emergency medical services (EMS) personnel from county‐based EMS agencies.
Methods
We conducted a cross‐sectional survey of cardiovascular disease (CVD)‐free EMS personnel from 4 US EMS agencies. The questionnaire consisted of the Pittsburgh Sleep Quality Index (PSQI), Perceived Stress Scale (PSS), Chronic Burden Scale, and the CVH components (smoking, body mass index, physical activity, diet, blood glucose, blood pressure, cholesterol, each scored 0–2 points). The components were summed and ideal CVH considered 11–14 points. Mixed effects logistic regression models with a random intercept for agency were used to estimate the odds of ideal CVH for good sleep quality (PSQI < 5 points), recommended sleep duration (7 to < 9h), low perceived stress (PSS < 26 points), and low chronic stress (0 recent stressful events).
Results
We received 379 responses (response rate = 32%). There was low prevalence of good sleep quality (23%) and recommended sleep duration (25%), but 95% reported low perceived stress, and 33% had low chronic stress. Ideal CVH was reported by 30%. No significant associations between ideal CVH and sleep quality, perceived stress, or chronic stress were found. There was a nearly 2‐fold increase in the odds of ideal CVH with recommended sleep duration (odds ratio: 1.83, 95% confidence interval: 1.08–3.10).
Conclusion
In this sample of EMS personnel, only recommended sleep duration was associated with ideal CVH. Future longitudinal studies are needed to understand the relationship between sleep, stress, and CVD in this understudied occupational group.
Keywords: emergency medical services, emergency medical technician, heart disease risk factors, occupational stress, paramedic, psychological stress, sleep
1. INTRODUCTION
1.1. Background
Personnel working in the emergency services, such as police, fire, and emergency medical services (EMS), appear to be at increased risk of developing cardiovascular disease (CVD). 1 , 2 , 3 One approach to understanding CVD risk, especially on a population level, is the concept of cardiovascular health (CVH). The Life's Simple 7 (LS7) metrics, introduced in 2010 by the American Heart Association, describe ideal, intermediate, and poor criteria for 7 modifiable health behaviors and risk factors for CVD. 4 The approach of LS7 focuses on primordial prevention, or prevention of risk factors instead of prevention of a disease state. 5 The metrics provide a framework for measuring and quantifying the health status of a population, such as the occupational group of EMS personnel.
1.2. Importance
Emergency responders frequently experience physiological and psychological stressors while on duty, including long periods of inactivity with intermittent strenuous activity while responding to an emergency, which may exacerbate poor cardiac health and precipitate a major cardiac event. 1 , 2 , 6 Because of this, substantial work has been done to study the cardiovascular health risks faced by firefighters, specifically. However, not all EMS personnel work in a fire‐based setting, and their CVD risk remains unclear. Previous work has shown that EMS personnel have a high prevalence of poor health for certain LS7 components such as obesity, poor diet, and inadequate physical activity. 7 , 8 , 9 EMS personnel also have a high prevalence of non‐traditional CVD risk factors, such as poor sleep quality, short or long sleep duration, and high stress, 10 , 11 , 12 , 13 which may further increase the risk of developing CVD. No prior studies have examined the relationship between sleep, stress, and CVH within the occupational group of EMS personnel. Establishing a cross‐sectional association between these factors would suggest that future longitudinal studies are needed to understand the relationship between the modifiable risk factors of poor sleep and high stress with chronic disease development.
1.3. Goals of this investigation
The objective of this study was to quantify the associations between sleep quality, sleep duration, perceived stress, and chronic stress with ideal CVH among a sample of EMS personnel working in county‐based EMS agencies.
2. METHODS
2.1. Study design and setting
This study was an electronic survey of a convenience sample of currently working EMS personnel from 4 non‐fire, county‐based EMS agencies in the United States. This type of agency is frequently referred to as “third service,” external to municipal police and fire departments, where employees do not work in a dual firefighter/EMS role. In the United States, there are approximately 3000 governmental, non‐fire EMS agencies, representing about 20% of all EMS agencies. 14 The 4 agencies were purposefully recruited to capture a range of sizes, typical workload or call volume, and rurality. This study was approved by the institutional review board (IRB) at American Institutes for Research (IRB# EX00474), with a waiver of documentation of consent.
2.2. Study population and data collection
The Bottom Line.
The Bottom Line: Emergency medical services (EMS) personnel face a host of psychological and physical risks in their work. This study examines the interrelationship between sleep, stress, and cardiovascular health. A minority of EMS personnel reported good sleep quality and recommended sleep duration and only 30% of respondents had ideal cardiovascular health. The odds of having ideal cardiovascular health increased significantly if respondents reported adequate sleep duration.
We used 4 components of data collection: an agency profile, demographic information for all eligible respondents, the electronic questionnaire, and an abbreviated non‐respondent questionnaire. Each agency representative completed a profile to gather basic information about their EMS operations and provided enumerated lists of all eligible employees from which to recruit participants. Active employees working in a position with EMS duties, including front‐line ambulance personnel and field supervisors, at the time of the survey were eligible to participate (n = 1,199).
Before data collection, we performed a sample size calculation to determine the number of respondents needed. We assumed a 5% margin of error, α = 0.05, and a conservative 50/50 split in responses. We also included a finite population correction, accounting for the target population size (n = 1199). We calculated that we would require 292 respondents under these conditions. Respondents to the main survey were identified as those who completed at least half of the survey items. We excluded from the analysis respondents who reported a history of CVD, because these individuals would be considered to have poor CVH regardless of the health behaviors or factors reported. Recruitment and data collection occurred from April 2019 to June 2019. The initial survey invitation was sent via email, with up to 3 reminder emails sent approximately 1, 2, and 4 weeks later. Respondents were offered an incentive of a random drawing of 20 $50 gift cards. One agency was not offered the incentive because of policies on acceptance of gifts by employees.
2.3. Questionnaires and measurements
2.3.1. Agency profile survey
The agency profile requested information about the agency's location, structure, and annual operations. Items included the types of services provided by the agency (eg, 911 response or medical transport), levels of EMS certifications employed, size of the community served, typical shift duration, and ambulance crew configurations (2 or 3 person). Operation metrics in 2018, such as the number of EMS responses and EMS response units, also were requested. The approximate daily average of responses per EMS unit or EMS transport unit was calculated and used as a measure of typical workload.
2.3.2. Main study survey
The full electronic questionnaire consisted of participant demographics and CVD history; EMS‐related characteristics; and measurement of sleep, stress, and LS7 components. The questionnaire was developed from existing scales and items previously used with EMS personnel. 15 The existing scales included the Patient Health Questionnaire (PHQ‐9), the Pittsburgh Sleep Quality Index (PSQI), 10‐item Perceived Stress Scale (PSS‐10), and Chronic Burden Scale. 16 , 17 , 18 , 19 These scales were selected to allow for comparison with prior work, especially as related to associations with CVH. The PSQI and PSS‐10 have both been validated and used in multiple languages and settings, each with a Cronbach's α > 0.70 and test‐retest reliability of > 0.70 across multiple studies. 20 Similarly, the PHQ‐9 has excellent internal reliability (Cronbach's α > 0.80). 16 The Chronic Burden Scale is an inventory rather than a psychometrically validated scale that is commonly used in longitudinal studies on CVD. 21 , 22 , 23 Before data collection, items were cognitively tested with 9 EMS personnel not included in the study to ensure construct and face validity.
Respondent demographics included age, sex, racial and ethnic identity (dichotomized to non‐Hispanic white or minority owing to the low prevalence of minority EMS personnel), education level, and marital status. Prior history of CVD was defined as reporting any diagnoses of stroke, myocardial infarction, congestive heart failure, coronary heart disease, or angina pectoris. Depressive symptoms were assessed using the PHQ‐9 depression screening tool, with moderately severe to severe depressive symptoms defined as 15–27 points. 16 Recency of the respondent's last physical exam by a healthcare professional (< 6 or ≥6 months ago) was assessed to examine accuracy of self‐reported health factors.
Items for EMS‐related characteristics included questions developed for the Longitudinal EMS Attributes and Demographics Study, 24 using standard definitions of EMS characteristics. 25 EMS‐related variables included primary role, number of EMS jobs, typical shift duration worked, and years of EMS experience. Certification level was dichotomized to basic life support (emergency medical technician [EMT]) and advanced life support (ALS; advanced EMT and paramedic).
2.3.3. Non‐respondent survey
Based on prior work surveying EMS personnel, 7 , 26 the response rate to the full questionnaire was expected to be low; for that reason, a planned non‐respondent survey was also conducted. This additional survey was an abbreviated version of the full questionnaire to allow for comparison of respondents and non‐respondents and to assess for potential response bias. The non‐respondent survey was launched in June 2019 to all eligible participants who did not complete the full questionnaire. Non‐respondents received 1 email invitation to the abbreviated questionnaire.
2.4. Exposures
The primary exposures of interest were sleep quality, sleep duration, perceived stress, and chronic stress. Sleep quality and duration were measured with the PSQI. 17 The global PQSI score was examined as a continuous variable and dichotomized to poor (>5 points) and good sleep quality (≤5 points). 17 Sleep duration was categorized as short (<7 hours), recommended (7 to <9 hours), and long (≥9 hours). 27 Because of evidence that both short and long sleep durations have detrimental health outcomes, 28 , 29 the variable was further dichotomized to recommended (7 to <9 hours) and short or long (<7 or ≥9 hours). Perceived stress, measured by the PSS‐10, 24 was analyzed in 2 ways: as a continuous variable and dichotomized (0–26 points as low, 27–40 points as high). 30 Chronic stress, measured with the Chronic Burden Scale, 25 was categorized as high (reporting 2 or more moderately or very stressful problems over the past 6 months), moderate (1 moderately or very stressful problem), or low (0 moderately or very stressful problems).
2.5. Outcome
The primary outcome of interest was ideal CVH as measured by the LS7 metrics. The 7 components of the LS7—smoking, body mass index (BMI), physical activity, diet, blood pressure, fasting plasma glucose, and cholesterol—were assessed via self‐report. These are scored from 0–2 points based on clinical guidelines or expert opinion (Table S1), with the sum of these points being the CVH score. 4 , 31 , 32 Unlike other commonly used CVD risk models such as the Framingham risk score, 33 higher scores are desired and reflect better CVH. Ideal CVH as measured by LS7 has been shown to be related to reduced risk of developing incident CVD, CVD‐related mortality, cancer, and several other chronic conditions. 34 , 35 , 36 , 37
For the health factors of blood pressure, cholesterol, and fasting plasma glucose, response options were the ranges of values based on the component cut points. 4 For example, cholesterol was asked as 3 categories: < 200 mg/dL, 200–239 mg/dL, and ≥240 mg/dL, with an additional option of “I don't know.” A summary of the LS7 component scoring is included in Table S1. 4 Briefly, the ideal categories were defined as being a non‐smoker or not smoking within the previous 12 months, reporting ≥75 minutes of vigorous or ≥150 minutes of moderate and vigorous physical activity per week, meeting recommendations of 4–5 components of the American Heart Association Healthy Diet score, BMI < 25 kg/m2, untreated blood pressure < 120/80 mmHg, untreated cholesterol < 200 mg/dL, and untreated fasting plasma glucose < 100 mg/dL. Respondents who did not know a health factor were classified as ideal for that component if they reported not taking medication for and had no prior history of the applicable condition. Conversely, if the respondent did not know but reported a prior history of hypertension, hyperlipidemia, or diabetes mellitus, they were classified as poor for that component. The overall CVH score was calculated by summing the points for each of the ideal (2 points), intermediate (1 point), and poor (0 points) components met. Ideal CVH was defined as a score of 11–14 points.
2.6. Analysis
There was minimal item missingness (≤6.5%) in the main survey; therefore, we used available case analysis. Descriptive statistics were calculated overall and stratified by ideal CVH status. Because little difference was found between respondents and non‐respondents, the respondents were treated as a random sample and no survey weights were used in the analyses. Internal consistency of each of the scales was determined using Cronbach's α. To determine associations between ideal CVH and sleep and stress, we estimated the odds of ideal CVH for the following primary predictor variables: sleep quality, sleep duration, perceived stress, and chronic stress. Because of the agency‐level recruiting of participants, potential clustering was accounted for by using mixed effects logistic regression with a random intercept for agency treated as a nuisance variable.
We selected covariates for the adjusted models based on prior literature and substantive reasoning while maintaining 8–10 events per variable to prevent overfitting. 38 We constructed directed acyclic graphs and used their established rules to select covariates to obtain the most parsimonious models possible. 39 The demographic variables included were age, sex, education level (ie, any college or not), and marital status. Linearity of age as a continuous variable was confirmed using fractional polynomials; in the chronic stress model, age was included as quartiles because of model fit. Depressive symptoms also were included in the perceived stress and chronic stress models 40 but not the sleep quality or sleep duration models because of small sample sizes leading to zero cells. The EMS‐related variables included average daily responses per unit, shift length, certification level, and role (ie, providing patient care or not). 7 , 10 , 11 , 26 Calibration and fit of each model were determined using calibration plots.
To assess for potential response bias, statistical comparisons were made between respondents to the full survey, respondents to the abbreviated non‐respondent survey, and demographic information available from all eligible participants. All analyses were completed using Stata IC 15.1 (StataCorp LLC, College Station, TX).
2.7. Sensitivity analyses
Because the questionnaire relied on self‐report, some respondents answered that they did not know their blood pressure, cholesterol, or blood glucose. Timing of the last physical exam by a healthcare professional where those health factors were measured was used to determine if reporting of these components differed by recency of a physical exam and to determine the potential for recall bias or misclassification. An exam < 6 months ago was considered recent to minimize recall bias.
Heterogeneity of effect was assessed in each model by testing interaction terms for the following biologically plausible interactions: primary predictor variable and age, primary predictor variable and sex, and age and sex. 41 , 42 Multiple imputation, using chained equations with 10 iterations, was used to confirm the findings from the available case analysis. 43 , 44 , 45 Finally, misclassification of the health factors was assessed by constructing 2 alternative scenarios. Respondents who did not know their blood pressure, cholesterol, or blood glucose were classified instead as intermediate and then poor for each factor. Models were repeated with these new classifications and results compared to the main analysis. These scenarios represent the range of potentially true outcomes to see the effect of misclassification.
3. RESULTS
3.1. Response rate
A total of 379 EMS personnel responded to the main survey (response rate = 32%), with 8 respondents then excluded from the analysis owing to a history of CVD. An additional 52 participants responded to the abbreviated non‐respondent survey. There were no significant differences between respondents to the main survey and abbreviated survey participants, including among the exposures and selected components of the outcome of interest (Table S2). However, respondents to the main survey were slightly older (mean age 37 vs 35 years, P = 0.002) with a higher proportion of those at the ALS level (85% vs 78%, P = 0.01) compared to non‐respondents overall.
3.2. Agency characteristics
All 4 agencies provided 911 services, and 1 also provided non‐emergency medical transports (Table 1). Agencies were of a variety of sizes, ranging from 115 to 420 employees doing EMS work, with 6500 to 149,680 EMS responses in 2018. Typical workload, measured by the average daily number of EMS responses, also varied by agency with a low of 1.5 responses per unit to a high of 7.2. Notably, the smallest agency, which operated only at the ALS level, used a 3‐person crew configuration as opposed to the more typical dyad.
TABLE 1.
Characteristics of the EMS agencies included in the study
| Characteristic | Agency A | Agency B | Agency C | Agency D |
|---|---|---|---|---|
| Service type | 911 and medical transport | 911 response | 911 response | 911 response |
| Levels of certification employed | EMT, AEMT, Paramedic | EMT, AEMT, Paramedic | AEMT, Paramedic | EMT, AEMT, Paramedic |
| Urbanicity | Large city | Large city | Midsized city | Suburb of large city |
| Annual number of EMS responses, 2018 | 149,680 | 107,432 | 6500 | 68,245 |
| Annual number of EMS transports, 2018 | 114,091 | 71,884 | 3422 | 54,596 |
| Number of employees in EMS roles, 2018 | 415 | 420 | 115 | 243 |
| Average daily number of EMS response unitsa | 101 | 53 | 12 | 26 |
| Average daily responses per EMS unit | 4.1 | 5.6 | 1.5 | 7.2 |
| Average daily number of EMS transport unitsb | 90 | 42 | 10 | 20 |
| Average daily transports per EMS transport unit | 3.5 | 4.7 | 0.9 | 7.5 |
| Shift duration | 12 hours | 12 hours | 24 hours | 24 hours |
| EMS crew configuration | 2 person | 2 person | 3 person | 2 person |
aThe average number of EMS response units (vehicles that may or may not be capable of transporting a patient such as quick response vehicle or ambulance) deployed per day.
bThe average number of EMS transport units (vehicles that can transport a patient, ie, ambulances) deployed per day.
Abbreviations: AEMT, advanced emergency medical technician; EMS, emergency medical services; EMT, emergency medical technician.
3.3. Demographics
The mean age of respondents was 36 years (SD 10.1), with 64% males and 87% identifying as non‐Hispanic white (Table 2). About one‐quarter or fewer of respondents reported a history of hypertension (22%), hyperlipidemia (26%), or diabetes mellitus (7%). Most respondents worked in a primary role providing patient care (81%), were certified at the ALS level (84%) and held only 1 EMS job (83%). One‐quarter of respondents typically worked shifts of ≥24 hours. A total of 106 (30%) respondents met the ideal CVH criteria. These respondents were younger (mean age 33 vs 38 years, P < 0.001), had a lower prevalence of the self‐reported chronic diseases (eg, hypertension, 5% vs 29%, P < 0.001), and fewer years of EMS experience (eg, ≥15 years, 21% vs 41%, P = 0.002) compared to respondents with non‐ideal CVH.
TABLE 2.
Demographic and EMS‐related characteristics of the respondents overall and stratified by CVH status a
| Characteristic | Overall (n = 371) | Ideal CVH (n = 106) | Non‐Ideal CVH (n = 246) | P b |
|---|---|---|---|---|
| Age (years), mean (SD) | 36 (10.1) | 33 (8.7) | 38 (10.2) | <0.001 |
| Missing | 4 | 0 | 2 | |
| Sex, n (%) | ||||
| Female | 130 (36) | 45 (42) | 79 (32) | 0.06 |
| Male | 236 (64) | 61 (58) | 167 (68) | |
| Missing | 5 | 0 | 0 | |
| Race/ethnicity, n (%) | ||||
| Non‐Hispanic white | 301 (87) | 92 (88) | 206 (87) | 0.86 |
| Minority | 46 (13) | 13 (12) | 31 (13) | |
| Missing | 24 | 1 | 9 | |
| Education level, n (%) | ||||
| Some college or less | 133 (37) | 31 (29) | 100 (41) | 0.11 |
| Associate's degree | 89 (25) | 28 (26) | 58 (24) | |
| Bachelor's degree or more | 135 (38) | 47 (44) | 87 (36) | |
| Missing | 14 | 0 | 1 | |
| Marital status, n (%) | ||||
| Married or coupled | 223 (62) | 61 (58) | 159 (65) | 0.09 |
| Single | 89 (25) | 34 (32) | 52 (21) | |
| Widowed, divorced, or separated | 45 (13) | 11 (10) | 34 (14) | |
| Missing | 14 | 0 | 1 | |
| Depressive symptoms c , n (%) | ||||
| Mild to moderate | 314 (90) | 92 (90) | 210 (89) | 0.82 |
| Moderately severe to severe | 35 (10) | 10 (10) | 25 (11) | |
| Missing | 22 | 4 | 11 | |
| Self‐reported medical history, n (%) | ||||
| Hypertension | 78 (22) | 5 (5) | 70 (29) | <0.001 |
| Hyperlipidemia | 97 (26) | 7 (7) | 87 (35) | <0.001 |
| Diabetes mellitus | 25 (7) | 0 (0) | 24 (10) | 0.001 |
| Last physical exam, n (%) | ||||
| < 6 months ago | 211 (58) | 60 (57) | 144 (59) | 0.71 |
| ≥6 months ago | 150 (42) | 46 (43) | 101 (41) | |
| Missing | 10 | 0 | 1 | |
| EMS role, n (%) | ||||
| Patient care | 301 (81) | 87 (82) | 199 (81) | 0.72 |
| Administrator or supervisor | 44 (12) | 11 (10) | 32 (13) | |
| Other | 26 (7) | 8 (8) | 15 (6) | |
| Certification level, n (%) | ||||
| BLS | 58 (16) | 16 (15) | 40 (16) | 0.78 |
| ALS | 313 (84) | 90 (85) | 206 (84) | |
| Number of EMS jobs, n (%) | ||||
| 1 | 308 (83) | 89 (84) | 205 (83) | 0.88 |
| ≥2 | 63 (17) | 17 (16) | 41 (17) | |
| Years of EMS experience, n (%) | ||||
| <3 years | 52 (14) | 18 (17) | 32 (13) | 0.002 |
| 3–7 years | 82 (22) | 32 (30) | 45 (18) | |
| 8–15 years | 108 (29) | 34 (32) | 67 (27) | |
| ≥15 years | 129 (35) | 22 (21) | 102 (41) | |
| Shift length, n (%) | ||||
| Does not work shifts | 3 (1) | 1 (1) | 2 (1) | 0.73 |
| <24 hours | 271 (73) | 80 (75) | 176 (72) | |
| ≥24 hours | 97 (26) | 25 (24) | 68 (28) | |
Abbreviations: ALS, advanced life support; BLS, basic life support; CVH, cardiovascular health; EMS, emergency medical services.
aA total of 19 respondents were missing 1 or more components of the CVH score and were excluded from the stratified analysis.
bP‐values calculated from χ2 tests or t tests as appropriate at the α = 0.05 level.
c Depressive symptoms were determined by the Patient Health Questionnaire‐9 (Cronbach's α = 0.88). Moderately severe to severe symptoms were defined as a score of 15–27 points.
3.4. Prevalence of sleep, stress, and LS7 components
Overall, there was a low prevalence of good sleep quality (23%) and recommended sleep duration (25%; Table 3). The prevalence of low stress was more common, with 95% of respondents reporting low perceived stress; by contrast, 33% reporting low chronic stress. A greater proportion of respondents with ideal CVH, compared to those with non‐ideal CVH, reported recommended sleep durations (36% vs 22%, P = 0.01). For the individual LS7 components (Figure 1), there was a high prevalence of meeting ideal criteria for smoking (87%), blood glucose (76%), and cholesterol (71%). However, fewer respondents had ideal BMI (22%), physical activity (24%), or diet (11%).
TABLE 3.
Prevalence of sleep and stress metrics overall and stratified by CVH status a
| Overall (n = 371) | Ideal CVH (n = 106) | Non‐Ideal CVH (n = 246) | P b | |
|---|---|---|---|---|
| Metric c | n (%) | n (%) | n (%) | |
| Sleep quality | ||||
| Mean global PSQI score (SE) | 8.4 (0.2) | 8.5 (0.4) | 8.3 (0.2) | 0.65 |
| Poor (>5 points) | 280 (77) | 84 (81) | 180 (74) | 0.18 |
| Good (0–5 points) | 85 (23) | 20 (19) | 63 (26) | |
| Missing | 6 | 2 | 3 | |
| Sleep duration | ||||
| Short (<7 hours) | 277 (75) | 68 (64) | 192 (78) | 0.01 |
| Recommended (7 to <9 hours) | 91 (25) | 38 (36) | 52 (22) | |
| Long (≥9 hours) | 3 (1) | 0 (0) | 2 (1) | |
| Missing | 0 | 0 | 0 | |
| Perceived stress | ||||
| Mean stress score (SE) | 16.1 (0.3) | 15.9 (0.7) | 16.0 (0.4) | 0.81 |
| High (27–40 points) | 19 (5) | 7 (7) | 12 (5) | 0.52 |
| Low (0–26 points) | 351 (95) | 99 (93) | 233 (95) | |
| Missing | 1 | 0 | 1 | |
| Chronic stress | ||||
| High (≥2 problems) | 136 (37) | 34 (32) | 95 (39) | 0.22 |
| Moderate (1 problem) | 108 (30) | 38 (36) | 64 (26) | |
| Low (0 problems) | 122 (33) | 33 (31) | 83 (34) | |
| Missing | 5 | 1 | 4 | |
Abbreviations: CVH, cardiovascular health; PSQI, Pittsburgh Sleep Quality Index; PSS, Perceived Stress Scale.
aA total of 19 respondents were missing 1 or more components of the CVH score and were excluded from the stratified analysis.
b P‐values calculated from χ2 tests or t‐tests as appropriate at the α = 0.05 level.
cCronbach's α for PSQI (sleep quality) was 0.78 at the item‐level and 0.69 at the component level; for PSS‐10 (perceived stress) Cronbach's α was 0.89.
FIGURE 1.
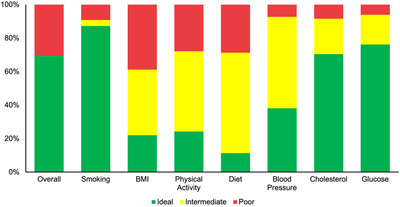
Prevalence of ideal, intermediate, and poor classification for each of the Life's Simple 7 components. Abbreviation: BMI, body mass index.
3.5. Associations between sleep, stress, and ideal cardiovascular health
Recommended sleep duration was the only metric associated with ideal CVH in the unadjusted and adjusted models (Table 4). In the adjusted model, there was a nearly 2‐fold increase in the odds of ideal CVH for the typical respondent with recommended sleep duration compared to a typical respondent with short or long sleep duration (odds ratio 1.83; 95% confidence interval 1.08‐3.10). No significant associations were found between good sleep quality, low perceived stress, and moderate or low chronic stress with ideal CVH (Table 4). Models demonstrated adequate calibration (Figure S1).
TABLE 4.
Estimated odds of ideal CVH for each of the sleep and stress metrics of interest
| Unadjusted | Adjusted a | |
|---|---|---|
| Exposure | OR (95% CI) | OR (95% CI) |
| Sleep quality | ||
| Poor (>5 points) | 1.00 | 1.00 |
| Good (0–5 points) | 0.67 (0.38–1.19) | 0.69 (0.38–1.23) |
| Sleep duration | ||
| Short or long (<7 or ≥9 hours) | 1.00 | 1.00 |
| Recommended (7 to < 9 hours) | 2.10 (1.27–3.48) | 1.85 (1.09–3.15) |
| Perceived stress | ||
| High (27–40 points) | 1.00 | 1.00 |
| Low (0–26 points) | 0.80 (0.29–2.23) | 0.78 (0.23–2.70) |
| Chronic stress | ||
| High (≥2 problems) | 1.00 | 1.00 |
| Moderate (1 problem) | 1.64 (0.92–2.91) | 1.86 (1.00–3.46) |
| Low (0 problems) | 1.10 (0.62–1.96) | 1.17 (0.62–2.19) |
Abbreviations: CI, confidence interval; CVH, cardiovascular health; EMS, emergency medical services; OR, odds ratio.
aSleep models adjusted for age, sex, education level (ie, any college or not), marital status, average daily responses per EMS unit, shift length (ie, 24 hours or not), certification level, and primary EMS role (ie, providing patient care or not). Age was modeled as a continuous variable except in the chronic stress model, where quartiles were used because of model fit. Stress models also adjusted for depressive symptoms.
3.6. Sensitivity analyses
Participants who reported a non‐recent physical exam by a healthcare professional had significantly higher proportions who did not know their blood pressure (eg, systolic, 7% vs 0%, P = 0.001), cholesterol (50% vs 34%, P = 0.003), or blood glucose (33% vs 19%, P = 0.01) compared to those with a recent physical exam (Table S3). However, there was no significant difference in the proportion of respondents classified as meeting the ideal CVH criteria by last exam timing; 31% of respondents with recent physical exams had ideal CVH compared to 29% of those with less recent exams (P = 0.71).
We found no evidence of effect modification by age or sex in any of the models. With multiple imputation, there was little difference in the observed associations except for a significant positive association between moderate chronic stress and higher odds of ideal CVH (Table 5). Finally, the 2 additional scenarios were explored using available cases for handling respondents who reported not knowing their blood pressure, cholesterol, or blood glucose. Little change was noted in the associations when these respondents were classified in the intermediate or poor categories (Table 5). However, for the poor scenario only, the association between recommended sleep duration and ideal CVH was attenuated and no longer statistically significant.
TABLE 5.
Sensitivity analyses estimating odds of ideal CVH under the intermediate and poor scenarios and using multiple imputation
| Multiple Imputation a | Intermediate Scenario a | Poor Scenario a | |
|---|---|---|---|
| Exposure | OR (95% CI) | OR (95% CI) | OR (95% CI) |
| Sleep quality | |||
| Poor (>5 points) | 1.00 | 1.00 | 1.00 |
| Good (0–5 points) | 0.72 (0.40–1.28) | 0.83 (0.43–1.61) | 0.58 (0.28–1.24) |
| Sleep duration | |||
| Short or long (<7 or ≥9 hours) | 1.00 | 1.00 | 1.00 |
| Recommended (7 to< 9 hours) | 1.82 (1.07–3.07) | 1.81 (1.01–3.28) | 1.40 (0.74–2.65) |
| Perceived stress | |||
| High (27–40 points) | 1.00 | 1.00 | 1.00 |
| Low (0–26 points) | 0.70 (0.22–2.19) | 0.75 (0.21–2.77) | 0.62 (0.17–2.34) |
| Chronic stress | |||
| High (≥2 problems) | 1.00 | 1.00 | 1.00 |
| Moderate (1 problem) | 2.01 (1.08–3.72) | 1.62 (0.79–3.34) | 1.28 (0.60–2.75) |
| Low (0 problems) | 1.13 (0.62–2.08) | 1.32 (0.64–2.72) | 0.97 (0.45–2.10) |
Abbreviations: CI, confidence interval; CVH, cardiovascular health; EMS, emergency medical services; OR, odds ratio.
aSleep models adjusted for age, sex, education level eg, any college or not), marital status, average daily responses per EMS unit, shift length (eg, 24 hours or not), certification level, and primary EMS role (eg, patient care or not). Age was modeled as a continuous variable except in the chronic stress model, where quartiles were used because of model fit. Stress models also adjusted for depressive symptoms.
3.7. Limitations
These are several potential limitations to this study. The 32% response rate was low but expected, 7 , 26 and we achieved the required number of respondents according to our sample size calculation. With the 371 included respondents, our calculated margin of error was 4.2%, below the planned 5%. The margin of error for each exposure or outcome of interest ranged from 1.8% for perceived stress to 4.0% for chronic stress. Because of the low response rate, some of the models may have been underpowered to detect a significant association. Further work with larger samples is encouraged.
There was also a potential for misclassification of the primary predictor variables. For example, self‐reported sleep durations tend to be overestimated compared to objectively measured durations with actigraphy. 46 , 47 Using objectively measured sleep data or medical records was not feasible for this work. We would encourage future studies to use actigraphy and medical records to reduce misclassification bias. These data were collected in a cross‐sectional survey, so causal associations cannot be inferred. All variables were assessed at only 1 time point, limiting the assessment of the timing of events, such as that recommended sleep duration preceded ideal CVH. Following participants over time to assess factors such as temporality and biological gradient of the association would provide evidence for a causal relationship between sleep, stress, and ideal CVH.
Finally, the EMS agencies who participated in this study were a convenience sample. We attempted to include a range of characteristics in terms of structure, workload, and rurality, but there is wide variability among EMS agencies. Compared to a recent prior description of the EMS workforce, 48 respondents in this study were more likely to be female and certified at the ALS level; however, the demographics of EMS personnel likely vary by agency type. It is unclear if these results would be generalizable to those working in other EMS agencies, especially those with a different service model (eg, fire based, private).
4. DISCUSSION
In this cross‐sectional survey of EMS personnel from 4 EMS agencies, there was a low prevalence of good sleep quality, recommended sleep duration, low chronic stress, and ideal status for many of the LS7 components, especially BMI, physical activity, and diet. Recommended sleep duration was consistently associated with ideal CVH. Additional work with a larger sample size and objectively measured health behaviors and factors is needed to confirm our findings and better characterize the health risks faced by EMS personnel.
Low response rates have been an increasingly common problem over the past few decades for survey‐based research. 49 Although we did not elicit reasons for non‐response among this sample, national surveys (eg, National Health Interview Survey) have shown that a lack of interest in the topic or lack of time is frequently cited as the reason for non‐response. 49 Common approaches to increase response rates include participation incentives and multiple reminders, both of which were implemented in this study. To account for our low response rate and potential response bias, we conducted a planned abbreviated non‐respondent survey and compared respondents to the demographics of non‐respondents. There were no significant differences between full survey and abbreviated survey respondents for the exposures of interest (eg, sleep duration). We found no evidence that respondents were in some way healthier or not compared to non‐respondents. However, response bias is still possible, and we may have been underpowered to detect a statistically significant association in multivariable models. Future work could benefit from increased incentives to promote participation; data collection in person or via telephone rather than limited to electronic questionnaires; and collection of objective data to minimize self‐reporting bias.
EMS personnel in this sample had worse sleep quality, short and long sleep durations, and high chronic stress compared to the general population. 41 , 50 , 51 , 52 , 53 The high‐stress nature of EMS work, as well as reliance on shift work and long shift durations, may help explain some of these differences. This sample had higher prevalence of poor sleep and stress compared to prior descriptions of EMS personnel. 10 , 11 , 12 , 13 This sample also had worse sleep quality than reported by police officers but lower levels of perceived stress. 54 , 55 Compared to firefighters, this sample also reported worse sleep quality but similar levels of perceived stress. 56 , 57
A larger proportion of the EMS personnel in this study met the criteria for ideal CVH (30%) compared to estimates in the United States and globally (12% and 20%, respectively). 31 , 58 , 59 Compared to estimates of the individual LS7 components in US adults, EMS personnel reported higher levels of ideal criteria for smoking (eg, 87% vs 71% of US adults), diet (11% vs 6%), cholesterol (70% vs 50%), and blood glucose (76% vs 64%). 59 However, a prior study of nationally certified EMS personnel found similar proportions of respondents meeting ideal criteria for the LS7 components. 7 Better CVH in EMS personnel may be because of the “healthy worker” effect 60 and differences in demographics such as age or education level. We also relied on self‐reporting used in this study, and it is likely that some participants in this study overestimated their health behaviors and factors. The use of objectively measured data in a future study would overcome this limitation.
There has been conflicting evidence of an association between sleep quality and duration with ideal CVH. 61 , 62 Notably, prior studies did not examine participants with a shift work schedule, and none examined these associations specifically in the occupational group of EMS personnel. Shift work is a major risk factor for inadequate sleep duration and poor sleep quality. 63 , 64 Psychological stress, also frequently experienced by EMS personnel, 13 is associated with decreased odds of ideal CVH in the general population and other healthcare workers. 65 , 66 , 67 The lack of association observed in this study between perceived stress and ideal CVH may be because the PSS does not adequately measure the common stressors faced in EMS. Further work is needed to determine if other measures of stress that may be more applicable to the EMS setting would be associated with CVH status.
Because meeting ideal CVH criteria based on LS7 is associated with a reduced risk of developing CVD and other chronic conditions, 32 , 34 , 35 , 36 , 37 there is evidence of the potential for negative health outcomes for some EMS personnel. The associations seen in this exploratory study between sleep and stress measures and ideal CVH, though most not statistically significant in this small sample, suggest further work is needed to determine if these additional modifiable risk factors could be targeted for interventions in this population. EMS personnel serve a critical function in the medical care system, and their personal health status likely affects their ability to remain in the workforce and provide these services.
In summary, in this sample of EMS personnel from 4 county‐based, non‐fire EMS agencies, there was a low prevalence of good sleep quality, adequate sleep duration, low chronic stress, and ideal CVH. Only recommended sleep duration of 7 to < 9 hours per night was consistently associated with ideal CVH. There was also a positive, but not significant, association between moderate or low chronic stress and ideal CVH. Further work in larger samples and other EMS settings is needed to verify these findings. Additionally, we encourage future studies to establish if the risk factors of sleep and stress are associated longitudinally with development of incident CVD in this population.
CONFLICT OF INTEREST
The authors have no conflicts to disclose.
AUTHOR CONTRIBUTIONS
REC, SEA, KEL, BL, and ARP conceived and designed the study. REC, MKR, and ARP collected the data. SEA, KEL, BL, CAC, and ARP provided statistical advice. REC analyzed the data. REC drafted the manuscript, and all authors contributed substantially to its revision. REC takes responsibility for the paper as a whole.
Supporting information
Supporting material
Biography
Rebecca E. Cash, PhD, MPH, is an Assistant Professor of Emergency Medicine at Harvard Medical School.

Cash RE, Anderson SE, Lancaster KE, et al. Associations between sleep, stress, and cardiovascular health in emergency medical services personnel. JACEP Open. 2021;2:e12516. 10.1002/emp2.12516
Supervising Editor: Elizabeth Donnelly, PhD, MPH
Funding and support: By JACEP Open policy, all authors are required to disclose any and allcommercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org ). The authors have stated that no such relationships exist.
REFERENCES
- 1. Drew‐Nord DC, Hong O, Froelicher ES. Cardiovascular risk factors among career firefighters. AAOHN J. 2009;57(10):415‐422. [DOI] [PubMed] [Google Scholar]
- 2. Soteriades ES, Smith DL, Tsismenakis AJ, Baur DM, Kales SN. Cardiovascular disease in US firefighters: a systematic review. Cardiol Rev. 2011;19(4):202‐215. [DOI] [PubMed] [Google Scholar]
- 3. Varvarigou V, Farioli A, Korre M, Sato S, Dahabreh IJ, Kales SN. Law enforcement duties and sudden cardiac death among police officers in United States: case distribution study. BMJ. 2014;349:g6534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lloyd‐Jones DM, Hong Y, Labarthe D. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic impact goal through 2020 and beyond. Circulation. 2010;121(4):586‐613. [DOI] [PubMed] [Google Scholar]
- 5. Claas SA, Arnett DK. The role of healthy lifestyle in the primordial prevention of cardiovascular disease. Curr Cardiol Rep. 2016;18(6):56. [DOI] [PubMed] [Google Scholar]
- 6. Hall SJ, Aisbett B, Tait JL, Turner AI, Ferguson SA, Main LC. The acute physiological stress response to an emergency alarm and mobilization during the day and at night. Noise Health. 2016;18(82):150‐156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cash RE, Crowe RP, Bower JK, Foraker RE, Panchal AR. Differences in cardiovascular health metrics in emergency medical technicians compared to paramedics: a national study of emergency medical services professionals. Prehosp Disaster Med. 2019;34(3):288‐296. [DOI] [PubMed] [Google Scholar]
- 8. Brice JH, Cyr JM, Hnat AT. Assessment of key health and wellness indicators among North Carolina emergency medical service providers. Prehosp Emerg Care. 2019;23(2):179‐186. [DOI] [PubMed] [Google Scholar]
- 9. Studnek JR, Bentley M, Mac Crawford J, Fernandez AR. An assessment of key health indicators among emergency medical services professionals. Prehosp Emerg Care. 2010;14(1):14‐20. [DOI] [PubMed] [Google Scholar]
- 10. Patterson PD, Weaver MD, Frank RC. Association between poor sleep, fatigue, and safety outcomes in emergency medical services providers. Prehosp Emerg Care. 2012;16(1):86‐97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Patterson PD, Suffoletto BP, Kupas DF, Weaver MD, Hostler D. Sleep quality and fatigue among prehospital providers. Prehosp Emerg Care. 2010;14(2):187‐193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Guyette FX, Morley JL, Weaver MD, Patterson PD, Hostler D. The effect of shift length on fatigue and cognitive performance in air medical providers. Prehosp Emerg Care. 2013;17(1):23‐28. [DOI] [PubMed] [Google Scholar]
- 13. Cash RE, Anderson SE, Lancaster KE. Comparing the prevalence of poor sleep and stress metrics in basic versus advanced life support emergency medical services personnel. Prehosp Emerg Care. 2020;24(5):644‐656. [DOI] [PubMed] [Google Scholar]
- 14. Federal Interagency Committee on Emergency Medical Services . 2011 National EMS Assessment. Washington, DC: U.S. Department of Transportation, National Highway Traffic Safety Administration; 2011. [Google Scholar]
- 15. Levine R. Longitudinal emergency medical technician attributes and demographic study (leads) design and methodology. Prehosp Disaster Med. 2016;31(S1):S7‐s17. [DOI] [PubMed] [Google Scholar]
- 16. Kroenke K, Spitzer RL, Williams JB. The PHQ‐9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606‐613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Buysse DJ, Reynolds CFI, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193‐213. [DOI] [PubMed] [Google Scholar]
- 18. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385‐396. [PubMed] [Google Scholar]
- 19. Bromberger JT, Matthews KA. A longitudinal study of the effects of pessimism, trait anxiety, and life stress on depressive symptoms in middle‐aged women. Psychol Aging. 1996;11(2):207‐213. [DOI] [PubMed] [Google Scholar]
- 20. Mollayeva T, Thurairajah P, Burton K, Mollayeva S, Shapiro CM, Colantonio A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non‐clinical samples: a systematic review and meta‐analysis. Sleep Med Rev. 2016;25:52‐73. [DOI] [PubMed] [Google Scholar]
- 21. Mujahid MS, Roux AVD, Cooper RC, Shea S, Williams DR. Neighborhood stressors and race/ethnic differences in hypertension prevalence (The Multi‐Ethnic Study of Atherosclerosis). Am J Hypertens. 2011;24(2):187‐193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gallo LC, Roesch SC, Fortmann AL. Associations of chronic stress burden, perceived stress, and traumatic stress with cardiovascular disease prevalence and risk factors in the Hispanic Community Health Study/Study of Latinos Sociocultural Ancillary Study. Psychosom Med. 2014;76(6):468‐475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Whitaker KM, Jacobs DR, Kershaw KN. Racial disparities in cardiovascular health behaviors: the coronary artery risk development in young adults study. Am J Prev Med. 2018;55(1):63‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bentley MA, Shoben A, Levine R. The demographics and education of emergency medical services (EMS) professionals: a national longitudinal investigation. Prehosp Disaster Med. 2016;31(S1):S18‐s29. [DOI] [PubMed] [Google Scholar]
- 25. National Highway Traffic Safety Administration Office of EMS . National Emergency Medical Services Workforce Data Definitions. Washington, DC: U.S. Department of Transportation; 2013. [Google Scholar]
- 26. Crowe RP, Bower JK, Cash RE, Panchal AR, Rodriguez SA, Olivo‐Marston SE. Association of burnout with workforce‐reducing factors among EMS professionals. Prehosp Emerg Care. 2018;22(2):229‐236. [DOI] [PubMed] [Google Scholar]
- 27. Hirshkowitz M, Whiton K, Albert SM. National sleep foundation's updated sleep duration recommendations: final report. Sleep Health. 2015;1(4):233‐243. [DOI] [PubMed] [Google Scholar]
- 28. Jike M, Itani O, Watanabe N, Buysse DJ, Kaneita Y. Long sleep duration and health outcomes: a systematic review, meta‐analysis and meta‐regression. Sleep Med Rev. 2018;39:25‐36. [DOI] [PubMed] [Google Scholar]
- 29. Itani O, Jike M, Watanabe N, Kaneita Y. Short sleep duration and health outcomes: a systematic review, meta‐analysis, and meta‐regression. Sleep Med. 2017;32:246‐256. [DOI] [PubMed] [Google Scholar]
- 30. Gambetta‐Tessini K, Mariño R, Morgan M, Evans W, Anderson V. Stress and health‐promoting attributes in Australian, New Zealand, and Chilean dental students. J Dent Educ. 2013;77(6):801‐809. [PubMed] [Google Scholar]
- 31. Folsom AR, Yatsuya H, Nettleton JA. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57(16):1690‐1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kulshreshtha A, Vaccarino V, Judd SE. Life's simple 7 and risk of incident stroke: the reasons for geographic and racial differences in stroke (regards) study. Stroke. 2013;44(7):1909‐1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lloyd‐Jones DM, Wilson PW, Larson MG. Framingham risk score and prediction of lifetime risk for coronary heart disease. Am J Cardiol. 2004;94(1):20‐24. [DOI] [PubMed] [Google Scholar]
- 34. Foraker RE, Abdel‐Rasoul M, Kuller LH. Cardiovascular health and incident cardiovascular disease and cancer: the women's health initiative. Am J Prev Med. 2016;50(2):236‐240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ramirez‐Velez R, Saavedra JM, Lobelo F, Celis‐Morales CA, BD Pozo‐Cruz, Garcia‐Hermoso A. Ideal cardiovascular health and incident cardiovascular disease among adults: a systematic review and meta‐analysis. Mayo Clin Proc. 2018;93(11):1589‐1599. [DOI] [PubMed] [Google Scholar]
- 36. Joseph JJ, Echouffo‐Tcheugui JB, Carnethon MR. The association of ideal cardiovascular health with incident type 2 diabetes mellitus: the multi‐ethnic study of atherosclerosis. Diabetologia. 2016;59(9):1893‐1903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rasmussen‐Torvik LJ, Shay CM, Abramson JG. Ideal cardiovascular health is inversely associated with incident cancer: the atherosclerosis risk in communities study. Circulation. 2013;127(12):1270‐1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol. 2006;165(6):710‐718. [DOI] [PubMed] [Google Scholar]
- 39. Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 40. Gaye B, Prugger C, Perier MC. High level of depressive symptoms as a barrier to reach an ideal cardiovascular health: the Paris Prospective Study III. Sci Rep. 2016;6:18951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB. Prevalence of healthy sleep duration among adults–United States. MMWR Morb Mortal Wkly Rep. 2014;65(6):137‐141. [DOI] [PubMed] [Google Scholar]
- 42. Cohen S, Janicki‐Deverts D. Who's stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. J Appl Soc Psychol. 2012;42(6):1320‐1334. [Google Scholar]
- 43. StataCorp . Stata Multiple Imputation Reference Manual Release 15. Stata Press; 2017. [Google Scholar]
- 44. Little RJ, Rubin DB. Statistical Analysis With Missing Data. 2014;333. [Google Scholar]
- 45. Rubin DB. Multiple Imputation for Nonresponse in Surveys. John Wiley & Sons; 2004. [Google Scholar]
- 46. Jackson CL, Patel SR, Jackson WB, Lutsey PL, Redline S. Agreement between self‐reported and objectively measured sleep duration among white, black, Hispanic, and Chinese adults in the United States: Multi‐Ethnic Study of Atherosclerosis. Sleep. 2018;41(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self‐reported and measured sleep duration: how similar are they?. Epidemiology. 2008;19(6):838‐845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Rivard MK, Cash RE, Mercer CB, Chrzan K, Panchal AR. Demography of the national emergency medical services workforce: a description of those providing patient care in the prehospital setting. Prehosp Emerg Care. 2021;25(2):213‐220. [DOI] [PubMed] [Google Scholar]
- 49. National Research Council . Nonresponse in Social Science Surveys: A Research Agenda. National Academies Press; 2013. [Google Scholar]
- 50. Chung J. Social support, social strain, sleep quality, and actigraphic sleep characteristics: evidence from a national survey of US adults. Sleep Health. 2017;3(1):22‐27. [DOI] [PubMed] [Google Scholar]
- 51. Buysse DJ, Hall ML, Strollo PJ, Relationships between the Pittsburgh Sleep Quality Index (PSQI) . Epworth Sleepiness Scale (ESS), and clinical/polysomnographic measures in a community sample. J Clin Sleep Med. 2008;4(6):563‐571. [PMC free article] [PubMed] [Google Scholar]
- 52. Krueger PM, Friedman EM. Sleep duration in the United States: a cross‐sectional population‐based study. Am J Epidemiol. 2009;169(9):1052‐1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Meier HCS, Hussein M, Needham B. Cellular response to chronic psychosocial stress: ten‐year longitudinal changes in telomere length in the multi‐ethnic study of atherosclerosis. Psychoneuroendocrino. 2019;107:70‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Garbarino S, Guglielmi O, Puntoni M, Bragazzi NL, Magnavita N. Sleep quality among police officers: implications and insights from a systematic review and meta‐analysis of the literature. Int J Environ Res Public Health. 2019;16(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Charles LE, Slaven JE, Mnatsakanova A. Association of perceived stress with sleep duration and sleep quality in police officers. Int J Emerg Ment Health. 2011;13(4):229‐241. [PMC free article] [PubMed] [Google Scholar]
- 56. Mehrdad R, Haghighi KS, Esfahani AH. Sleep quality of professional firefighters. Int J Prev Med. 2013;4(9):1095‐1100. [PMC free article] [PubMed] [Google Scholar]
- 57. Makara‐Studzińska M, Golonka K, Izydorczyk B. Self‐efficacy as a moderator between stress and professional burnout in firefighters. Int J Environ Res Public Health. 2019;16(2):183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Bambs C, Kip KE, Dinga A, Mulukutla SR, Aiyer AN, Reis SE. Low prevalence of “ideal cardiovascular health” in a community‐based population: the Heart Strategies Concentrating on Risk Evaluation (Heart SCORE) study. Circulation. 2011;123(8):850‐857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Peng Y, Cao S, Yao Z, Wang Z. Prevalence of the cardiovascular health status in adults: a systematic review and meta‐analysis. Nutr Metab Cardiovasc Dis. 2018;28(12):1197‐1207. [DOI] [PubMed] [Google Scholar]
- 60. Chowdhury R, Shah D, Payal AR. Healthy worker effect phenomenon: revisited with emphasis on statistical methods ‐ a review. Indian J Occup Environ Med. 2017;21(1):2‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Makarem N, St‐Onge MP, Liao M, Lloyd‐Jones DM, Aggarwal B. Association of sleep characteristics with cardiovascular health among women and differences by race/ethnicity and menopausal status: findings from the American Heart Association go red for women strategically focused research network. Sleep Health. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Hausler N, Marques‐Vidal P, Heinzer R, Haba‐Rubio J. How are sleep characteristics related to cardiovascular health? Results from the population‐based hypnolaus study. J Am Heart Assoc. 2019;8(7):e011372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Kuhn G. Circadian rhythm, shift work, and emergency medicine. Ann Emerg Med. 2001;37(1):88‐98. [DOI] [PubMed] [Google Scholar]
- 64. Morris CJ, Purvis TE, Hu K, Scheer FAJL. Circadian misalignment increases cardiovascular disease risk factors in humans. Proc Natl Acad Sci USA. 2016;113(10):E1402‐E1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Poirat L, Gaye B, Perier MC. Perceived stress is inversely related to ideal cardiovascular health: The Paris Prospective Study III. Int J Cardiol. 2018;270:312‐318. [DOI] [PubMed] [Google Scholar]
- 66. Brewer LC, Redmond N, Slusser JP. Stress and achievement of cardiovascular health metrics: The American Heart Association life's simple 7 in blacks of the Jackson Heart Study. J Am Heart Assoc. 2018;7(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Burroughs Pena MS, Mbassa RS, Slopen NB, Williams DR, Buring JE, Albert MA. Cumulative psychosocial stress and ideal cardiovascular health in older women. Circulation. 2019;139(17):2012‐2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting material


