Abstract
The $1 trillion industry of acute hospital care in the United States is shifting from inside the walls of the hospital to patient homes. To tackle the limitations of current hospital care in the United States, on November 25, 2020, the Center for Medicare & Medicaid Services announced that the acute hospital care at home waiver would reimburse for “home hospital” services. A “home hospital” is the home‐based provision of acute services usually associated with the traditional inpatient hospital setting. Prior work suggests that home hospital care can reduce costs, maintain quality and safety, and improve patient experiences for select acutely ill adults who require hospital‐level care. However, most emergency physicians are unfamiliar with the evidence of benefits demonstrated by home hospital services, especially for older adults. Therefore, the lead author solicited narrative inputs on this topic from selected experts in emergency medicine and home hospital services with clinical experience, publications, and funding on home hospital care. Then we sought to identify information most relevant to the practice of emergency medicine. We outline the proven and potential benefits of home hospital services specific to older adults compared to traditional acute care hospitalization with a focus on the emergency department.
Keywords: disposition, Geriatrics, healthcare delivery, home hospital, palliative care, patient‐centered care
1. INTRODUCTION
The $1 trillion industry of acute hospital care in the United States is shifting from inside the walls of the hospital to patient homes. 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 Admission to the hospital is the standard of care for the management of acute illness in the United States, but hospital care is expensive and often unsafe, particularly for older adults. 12 While admitted, up to 35% of patients develop delirium, 13 , 14 >5% contract hospital‐acquired infections, 15 and many lose functional status that is never regained. 16 Timely access to inpatient care is often poor: many hospitals are >100% of inpatient capacity, which can result in patients boarding in the emergency department (ED) for prolonged periods of time waiting for an inpatient bed. Moreover, hospital care is increasingly costly, accounting for about one third of total medical expenditures, and is a leading cause of patient debt. 17
The novel coronavirus disease 2019 (COVID‐19) pandemic further demonstrated the limited ability of hospitals to increase inpatient capacity to accommodate a surge in patient hospitalizations and acuity. To tackle the limitations of current hospital care in the United States, on November 25, 2020, the Center for Medicare & Medicaid Services (CMS) announced the acute hospital care at home waiver to reimburse for “home hospital” services. A “home hospital” is defined as home‐based provision of acute services usually associated with the traditional inpatient hospital setting. 2 Prior work suggests that home hospital care can reduce cost, maintain quality and safety, and improve patient experience for select acutely ill adults who require traditional hospital‐level care. 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 Although home hospital care is familiar in several developed countries, 18 only 2 randomized clinical trials have been conducted in the United States. 19 , 20 The CMS's unprecedented announcement recognizes the benefits of home hospital services and has the potential to rapidly expand hospital capacity in the midst of the COVID‐19 pandemic. More than 96 hospitals in the past 2 months have already been granted waivers. This announcement will likely trigger a wave of health systems investing to provide hospital‐level care in patient homes in the next year.
However, given the dearth of institutions currently offering this service from the ED, most emergency physicians are unfamiliar with the existing evidence in support of using home hospital services as a disposition option. With the anticipated rapid increase in dissemination of home hospital services across the United States, the urgent need exists to delineate the proven and potential benefits and future opportunities for research specific to emergency medicine.
In this concept article, we discuss the benefits of home hospital care compared with traditional acute care, describe additional potential benefits specifically for older adults, and delineate important areas for emergency medicine–focused research. As one of the institutions that provided evidence for the CMS to develop the “home hospital” waiver with experience caring for >1000 patients on the home hospital service, the lead author solicited narrative inputs on this topic from our experts in emergency medicine and home hospital services with clinical experience, publications, and funding on home hospital care. Then, we sought to highlight information most relevant to the practice of emergency medicine.
2. WHAT IS HOME HOSPITAL?
Variations within home hospital exist (Figure 1). A recent systematic review revealed that home hospital service can have 3 subtypes: admission from the ED, from the hospital floor, and from patient homes, avoiding the hospital altogether. 21 Recognizing these variations, we highlight our program to describe what the service typically entails. In our home hospital team, we have a physician, 2 nurses, a mobile integrated health paramedic, and a program associate delivering care for 8 to 10 patients per team. Patients are evaluated for home hospitalization by an emergency physician (in person) and home hospital physician (in person or remotely) in the ED and transferred from the ED to their homes. The home hospital physician makes 1 visit per day (in person or remotely) and nurses/paramedics make 2 visits per day in person. Remote patient monitoring devices transmit patient vital signs, posture (eg, upright/recumbent), steps, and falls in real time to the team's phones/computers, which are monitored 24 hours/day by the clinical team. Using Health Insurance Portability and Accountability–secure video and text services, the enrolled patients or families can contact the team all hours of the day as well. Continuous or intermittent intravenous infusions, oxygen delivery, meal service, home health aide service, and other key personnel such as physical therapists are available. Electrocardiograms, portable ultrasound, at‐home radiology services, and remote specialist consultations are available. Computed tomography and magnetic resonance imaging scans also can be accomplished during home hospitalization via a round‐trip transfer. Predominant contraindications to home hospital care include requiring an imminent inpatient procedure, requiring critical care, being undomiciled, or having unreliable cognition and judgment attributed to psychiatric or substance use disorders. In partnership with the home hospital team, emergency physicians’ clinical expertise 22 allows them to select appropriate patients for home hospitalization. These unique benefits allow patients, especially older adults, to have specific benefits unattainable in the traditional hospital settings.
FIGURE 1.
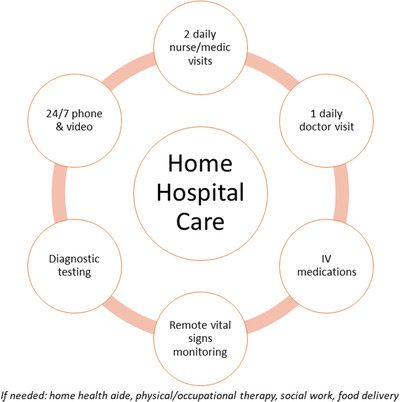
Components of home hospital services. IV, intravenous
2.1. Reduced cost of care
In a recent randomized controlled trial, home hospital reduced the cost of care by up to 40% when compared with traditional hospitalization. Patients at home received fewer laboratory tests, fewer consults, and less imaging. Although safety was not the primary outcome of the study, adverse events during the hospitalization were similar in both home hospital and traditional hospital patients. 19 , 20 In prior non‐randomized studies, similar cost savings were seen from home hospital services. 4 , 23
Indirect cost savings from reduced ED boarding may also be achieved with home hospital dissemination. Association exists between ED boarding times and inpatient hospital costs, 24 and cost‐savings occur by decreasing ED boarding times. 25 , 26 Boarding times were ≈1 hour for both home hospital and usual care arms in recent home hospital trials, 19 , 20 which were substantially shorter than the national average. Home hospital transfers are not reliant on hospital resources. The frequently rapid transfer out of the ED to home hospital, compared with traditional hospitalization, could have a substantial economic effect in busier EDs with longer boarding times. Some regions may experience similarly long wait times for home hospital care, although this has not been the authors’ experience. Among all non‐ICU hospitalization cases, home hospital service dedicates in‐hospital beds to patients who require them by creating spaces outside of the hospital for patients who can receive hospital‐level care at home.
2.2. Improved experience of care
The experience of care is substantially better with home hospital service compared with traditional hospitalization. Qualitative results demonstrated the contributing reasons for better care experience: better environment to promote activity and sleep (eg, patient's own room with own bed, reduced ambient noise), better availability and ease of contact with the clinical team, more contact to family and friends (if desired), and more familiar and comfortable food for nutrition and psychological well‐being. 27 In addition, patients randomized to home hospital service felt that the admissions process was a better experience compared with those who stayed in the traditional hospital.
Home hospital service also improves the experience of care for patients transitioning to hospice care. For patients at the end of life, a structured approach to transition to hospice care in the ED is possible but remains difficult given the complexity of steps required. 28 Although emergency physicians are becoming more experienced with goals‐of‐care conversations, 29 , 30 most patients requiring hospice initiation are admitted to the hospital to facilitate this process. With our home hospital service, we can serve as a bridge to home hospice if it cannot be deployed quickly enough or after a trial of acute care can transition to a home hospice agency.
2.3. How will home hospital service change what emergency physicians do?
There will be little change to the emergency physician's workflow. No restrictions on diagnosis exist for the CMS waiver. To provide examples, the CMS identified >60 diagnoses as appropriate for home hospitalization; common diagnoses include heart failure exacerbation, pneumonia, chronic obstructive pulmonary disease exacerbation, and cellulitis. Patients with COVID‐19 infection may be safely cared for at home 31 , 32 ; thus, home hospital effectively expands the hospital capacity during this and future pandemics.
The initial evaluation and treatment in the ED will remain the same; emergency physicians will evaluate and treat patients and determine an appropriate disposition. When considering hospital admission, emergency physicians will consider the appropriateness of home hospitalization as an alternative in collaboration with the home hospital team.
2.4. Potential challenges of home hospital service
Given the relative novelty of the home hospital service, no standardized, clinician training currently exists to provide this service. The clinical scope of a home hospital physician is different from what a typical inpatient, internal medicine–trained physician would provide. For example, not all diagnostic testing and consultation services are as readily available at home. Therefore, home hospital physicians must rely on their overall clinical judgment more often and make decisions based on available pieces of evidence. Similar to in‐hospital clinical service, specific reporting outcomes will need to be measured to standardize quality of care.
The in‐person nature of home hospital service may also pose a challenge in rural settings where a scarcity of clinicians exists. Because home hospital service relies on trained medical professionals to deliver care at home, the physical distance to each patient's home may make it difficult to provide the same service in rural areas where the travel time may be excessive. This could pose a challenge for more remote areas of the country; however, this must be balanced with the potentially significant benefit from improved access to care in rural areas. Emerging evidence suggests the highly perceived need, optimism, and potential feasibility in rural areas to implement home hospital services. 33 , 34
Although home hospital programs are mostly in the early phases of development, it is important to focus on solutions that will allow equitable access to these services. For example, regional variations may exist in timely disposition transfer to home hospital services from the ED. Although certain patient eligibility constraints (such as geographic requirements) may be attributed to the relatively small scale of many of these nascent programs, other constraints may require creative solutions to ensure broader access (eg, providing a Wi‐Fi hotspot to the individual patient). Similarly, progressive home hospital teams have addressed barriers to care by helping to manage the patient's home environment to make it safe and comfortable for home hospital care. This may include providing portable air conditioning or heat and may eventually include more permanent solutions for problems at home.
2.5. Opportunities for future research
The COVID‐19 pandemic has highlighted the limits of hospital capacity across the country. Home hospital programs have demonstrated the capacity to expand hospital capacity in a safe, efficient, and patient‐centered manner while reducing the cost of care. 35 Future areas of research remain despite the robust current evidence base.
2.5.1. Opportunity 1: Decrease in delirium
Delirium is a life‐threatening condition, characterized by an acute change in mental status and inattention, disorganized thinking, and/or altered level of arousal. 36 Although 8% to 17% of community‐dwelling older adults in the ED have delirium, delirium occurs in 18% to 35% of hospitalized older adults. 14 , 37 , 38 Up to 50% of delirium in hospitalized older adults can be prevented through multicomponent prevention programs. 39 , 40 Some elements of these programs theoretically may be more successfully implemented in the home hospital setting. For instance, maintaining circadian rhythms through non‐pharmacologic approaches to improve sleep quality is a key component of delirium prevention. Qualitative evidence demonstrates that sleep disruptions are reduced in a home hospital program. 27 Another important component of delirium prevention is enhanced and safe mobility practices, accomplished through minimizing physical tethers such as foley catheters, physical restraints, and bed alarms and ensuring that patients are ambulated at least 3 times a day. 14 As being in one's own home results in increased physical mobility compared with inpatient hospitalizations, 19 , 20 it stands to reason that this aspect of delirium prevention would also be enhanced by a home hospital program. As a physical change in environment, such as hospitalization, can be a trigger for delirium in at‐risk individuals, 14 avoiding hospitalization entirely may be even more successful in preventing delirium than non‐pharmacologic delirium prevention strategies in the hospital. The evidence is mixed to date regarding the efficacy of home hospital programs to prevent delirium. 3 , 20 However, one study of an in‐home rehabilitation program demonstrated reduced delirium compared to inpatient rehabilitation program. 10 Furthermore, home hospital care for patients with delirium may be associated with reduced length of stay compared with usual inpatient care, with no impact on mortality. 41 It is critical that future studies of home hospital programs use validated tools to assess for delirium to better understand the impact of the programs on this important geriatric syndrome.
2.5.2. Opportunity 2: Avoid hospital‐associated, increased fall risk and novel home falls evaluation
For older adults requiring acute hospitalization, home hospital would potentially provide multiple benefits in regard to their physical function and risk of fall: (1) patients would avoid the increased risk of falls associated with inpatient hospitalizations, (2) patients would avoid potential physical decline associated with inpatient hospitalizations, and (3) multicomponent fall prevention programs could be implemented in the patients’ native environment. Although more research is needed, patients who are hospitalized at home theoretically may be less likely to fall if they were at home because they are in a familiar environment, 42 which increases their overall mobility relative to those in traditional hospitalization potentially leading to less deconditioning. Low mobilization is common during hospitalization, leading to functional decline 43 , 44 (eg, hospitalized patient's quote, “I couldn't get to the toilet when I wanted. You just have to rely on the nurses, there's nothing else you can do. I once had to call three times, and by the third time, I had wet my bed.”). 45 In a non‐randomized study, patients in home hospital were associated with improvements in instrumental activity of daily living compared with acute hospitalization. 46 Less ambient noise at home (eg, machine beeping) may also decrease sleep deprivation and delirium, leading to accidental falls. 47 , 48 , 49 Finally, the visitor restrictions in the hospital attributed to the COVID‐19 pandemic prevent families from supporting their loved ones while patients are in the hospital.
Beyond a potential decrease in fall risk with home hospital service, older adults who present to the ED with falls could be excellent candidates for home hospital observation with multifactorial fall evaluation and possible rehabilitation placement, if needed. After the acute injuries are managed, these patients are often admitted to the observation unit for physical therapy and case management evaluation where multifactorial fall evaluations are not conducted routinely, resulting in missed opportunities to prevent recurrent falls. 50 A multifactorial fall protocol in a home hospital can overcome this hurdle: (1) home‐based physical therapy and nutritional intervention can improve nutritional and frailty status 51 ; (2) occupational therapy evaluation can complete a home safety evaluation via telemedicine, 52 resulting in handrails and other assistive devices shown to decrease future fall‐related injuries by 26% 53 ; (3) case manager evaluations via telemedicine can also assess patients’ needs and home/family resources; and (4) pharmacists via telemedicine can review patient medications and adjust them as necessary while observing the home environment, often resulting in the clearing of unused/dangerous medications. Such a home hospital fall protocol would minimize time in the ED and ensure that the clinical team gets a comprehensive picture of the patient's life leading to the falls.
2.5.3. Opportunity 3: Expand clinical indications for home hospital
Access to home hospitalization remains limited to certain disease pathways. This limits the scope of practice and excludes many patients who may otherwise benefit from home hospital. We need to invest in research to better understand other conditions that may benefit from home hospital. For example, a recent trial found decreased cost and healthcare use among patients with cancer hospitalized at home. 54 , 55 Studies published 2 decades ago demonstrated that patients with neutropenic fever may be treated at home with antibiotics and close monitoring and thus may be great candidates for home hospitalization. 56 Furthermore, other illnesses may be amenable to home hospital care by further exploring the literature and innovating care protocols. For example, home hospital is currently available for selected postoperative surgical patients, and this could be further expanded to include surgical re‐admissions for ileus, small bowel obstruction, or other patients admitted by a surgical service from the ED who do not require immediate surgical intervention. 57
2.5.4. Opportunity 4: Automation of patient selection for home hospital
Currently, the identification of patients for home hospital is time intensive to ensure the best possible match. The home hospital team must first review individual patient charts for numerous clinical and environmental factors to help determine which patient may be an ideal candidate. Using artificial intelligence, predictive models can be developed to help identify potentially suitable admissions. Given that machine‐learning models have been shown to predict mortality in the ED, similar models could be developed to automatically risk‐stratify patients and quickly identify the best candidates for home hospital. This model could also incorporate predictors of patient refusal for home hospital admission. 58 An automated process would help optimize the clinical and administrative process for patient selection. A relatively simple research design would be to first retrospectively and then prospectively compare the results of the current manual selection of patients for home hospital with an automated machine‐learning model to select patients. Predefining specific patient‐centered and caregiver‐centered outcomes (eg, caregiver burden) becomes essential to rigorously study the effect of such an automated algorithm.
2.5.5. Opportunity 5: Protocols to bypass ED evaluations before hospitalization
As telehealth technology, wearable medical devices, and point‐of‐care testing become more widespread, the remote evaluation of patients with acute illness is becoming more sophisticated (Figure 2). In the near future and depending on the condition, physicians may be able to determine if a patient requires hospitalization through a remote or paramedic‐facilitated visit with point‐of‐care testing only. 59 This could change the admission process, which currently requires an in‐person evaluation. If such a bypass of ED evaluation is possible, this may reduce caregiver burden further during an acute illness, which is also an important outcome to consider throughout the evaluation of home hospital service. More research is needed to demonstrate the safety and efficacy of such an ED bypass protocol. The future “upstream” possibility exists that a patient may be evaluated by a physician, admitted, and discharged without ever leaving his or her home. With the right protocols in place, such a model may help bring home hospital to rural areas, where nearly 1 in 5 Americans lives. 33 , 34
FIGURE 2.
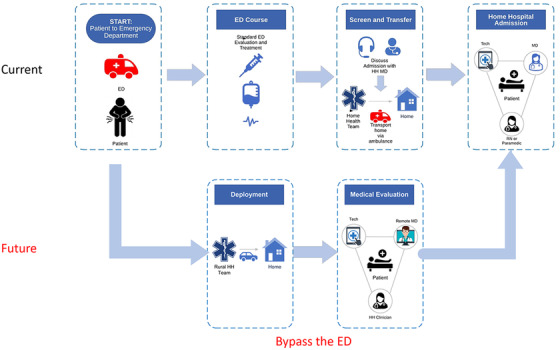
Current and future of home hospital admission workflows. ED, emergency department; HH, home hospital; MD, physician; RN, registered nurse
2.5.6. Opportunity 6: Technology for remote patient monitoring
Home hospital is reliant on accurate, reliable remote patient monitoring to provide a safe, effective, and scalable home‐based hospitalization environment. This need has spawned significant interest in health technology companies and venture capital to rapidly produce new devices, including wearable biosensors and peripheral monitoring devices. The current technologies provide the clinical team with near real‐time monitoring of patients’ vital signs and physical activity level, allowing the care team to intervene early if a problem should arise. A primary opportunity for research and care improvement is predictive algorithms based on vital sign data and activity level to predict clinical decline. This would provide clinicians the opportunity to make medication adjustments, perform further diagnostic testing, or perform therapeutic interventions earlier in the clinical course. Ample opportunities exist to enhance the current remote monitoring so that clinicians can monitor the well‐being (eg, physical, psychological stress, hydration status) of their patients beyond basic vital signs and physical activities. 60
3. CONCLUSIONS
Home hospital is a safe, effective, and cost‐efficient acute care service, which could be especially beneficial for older adults presenting to the ED. Home hospital will rapidly disseminate to become the standard of care in the United States but requires the buy‐in and expertise of emergency physicians to facilitate this paradigm change. Opportunities exist to further improve this line of clinical service in the near future.
CONFLICTS OF INTEREST
Dr. Levine reports grant funding and codevelopment with Biofourmis and grant funding from IBM that is separate from the present work.
ACKNOWLEDGMENT
Dr. Ouchi is supported by National Institute on Aging (K76AG064434) and the Cambia Health Foundation.
Ouchi K, Liu S, Tonellato D, Keschner YG, Kennedy M, Levine DM. Home hospital as a disposition for older adults from the emergency department: benefits and opportunities. JACEP Open. 2021;2:e12517. 10.1002/emp2.12517
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: Yiju Teresa Liu, MD
REFERENCES
- 1. CMS Announces Comprehensive Strategy to Enhance Hospital Capacity Amid COVID‐19 Surge. https://www.cms.gov/newsroom/press-releases/cms-announces-comprehensive-strategy-enhance-hospital-capacity-amid-covid-19-surge. Published 2020. Accessed January 27, 2021.
- 2. Leff B. Defining and disseminating the hospital‐at‐home model. CMAJ. 2009;180(2):156‐157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Leff B, Burton L, Mader SL, et al. Hospital at home: feasibility and outcomes of a program to provide hospital‐level care at home for acutely ill older patients. Ann Intern Med. 2005;143(11):798‐808. [DOI] [PubMed] [Google Scholar]
- 4. Cryer L, Shannon SB, Van Amsterdam M, Leff B. Costs for ‘hospital at home’ patients were 19 percent lower, with equal or better outcomes compared to similar inpatients. Health Aff (Millwood). 2012;31(6):1237‐1243. [DOI] [PubMed] [Google Scholar]
- 5. Tibaldi V, Isaia G, Scarafiotti C, et al. Hospital at home for elderly patients with acute decompensation of chronic heart failure: a prospective randomized controlled trial. Arch Intern Med. 2009;169(17):1569‐1575. [DOI] [PubMed] [Google Scholar]
- 6. Caplan GA, Sulaiman NS, Mangin DA, Aimonino Ricauda N, Wilson AD, Barclay L. A meta‐analysis of “hospital in the home”. Med J Aust. 2012;197(9):512‐519. [DOI] [PubMed] [Google Scholar]
- 7. Shepperd S, Doll H, Angus RM, et al. Avoiding hospital admission through provision of hospital care at home: a systematic review and meta‐analysis of individual patient data. CMAJ. 2009;180(2):175‐182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shepperd S, Iliffe S, Doll HA, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9:CD007491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Board N, Brennan N, Caplan GA. A randomised controlled trial of the costs of hospital as compared with hospital in the home for acute medical patients. Aust N Z J Public Health. 2000;24(3):305‐311. [DOI] [PubMed] [Google Scholar]
- 10. Caplan GA, Coconis J, Board N, Sayers A, Woods J. Does home treatment affect delirium? A randomised controlled trial of rehabilitation of elderly and care at home or usual treatment (The REACH‐OUT trial). Age Ageing. 2006;35(1):53‐60. [DOI] [PubMed] [Google Scholar]
- 11. Caplan GA, Coconis J, Woods J. Effect of hospital in the home treatment on physical and cognitive function: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2005;60(8):1035‐1038. [DOI] [PubMed] [Google Scholar]
- 12. Hung WW, Ross JS, Farber J, Siu AL. Evaluation of the Mobile Acute Care of the Elderly (MACE) service. JAMA Intern Med. 2013;173(11):990‐996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fong TG, Tulebaev SR, Inouye SK. Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol. 2009;5(4):210‐220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911‐922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. National and State Healthcare‐Associated Infections Progress Report. 2016. https://www.cdc.gov/hai/data/portal/progress-report.html#2018. Accessed July 14, 2021.
- 16. Counsell SR, Holder CM, Liebenauer LL, et al. Effects of a multicomponent intervention on functional outcomes and process of care in hospitalized older patients: a randomized controlled trial of Acute Care for Elders (ACE) in a community hospital. J Am Geriatr Soc. 2000;48(12):1572‐1581. [DOI] [PubMed] [Google Scholar]
- 17. National Center for Health Statistics (US). Health, United States, 2015 : With Special Feature on Racial and Ethnic Health Disparities. Hyattsville (MD): National Center for Health Statistics (US); 2016 May. Report No.: 2016‐1232. PMID: 27308685. [PubMed] [Google Scholar]
- 18. Montalto M. The 500‐bed hospital that isn't there: the victorian department of health review of the hospital in the home program. Med J Aust. 2010;193(10):598‐601. [DOI] [PubMed] [Google Scholar]
- 19. Levine DM, Ouchi K, Blanchfield B, et al. Hospital‐level care at home for acutely ill adults: a pilot randomized controlled trial. J Gen Intern Med. 2018;33(5):729‐736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Levine DM, Ouchi K, Blanchfield B, et al. Hospital‐level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020;172(2):77‐85. [DOI] [PubMed] [Google Scholar]
- 21. Leong MQ, Lim CW, Lai YF. Comparison of hospital‐at‐home models: a systematic review of reviews. BMJ Open. 2021;11(1):e043285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Calis M, Sener K, Kaya A, Sari S, Polat M, Yolcu S. The prediction levels of emergency clinicians about the outcome of the ambulance patients and outpatients. Am J Emerg Med. 2020;38(7):1463‐1465. [DOI] [PubMed] [Google Scholar]
- 23. Conley J, O'Brien CW, Leff BA, Bolen S, Zulman D. Alternative strategies to inpatient hospitalization for acute medical conditions: a systematic review. JAMA Intern Med. 2016;176(11):1693‐1702. [DOI] [PubMed] [Google Scholar]
- 24. Baloescu C, Kinsman J, Ravi S, et al. The cost of waiting: Association of ED boarding with hospitalization costs. Am J Emerg Med. 2021;40:169‐172. [DOI] [PubMed] [Google Scholar]
- 25. Schreyer KE, Martin R. The economics of an admissions holding unit. West J Emerg Med. 2017;18(4):553‐558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hrycko A, Tiwari V, Vemula M, et al. A hospitalist‐led team to manage patient boarding in the emergency department: impact on hospital length of stay and cost. South Med J. 2019;112(12):599‐603. [DOI] [PubMed] [Google Scholar]
- 27. Levine DM, Pian J, Mahendrakumar K, Patel A, Saenz A, Schnipper JL. Hospital‐level care at home for acutely ill adults: a qualitative evaluation of a randomized controlled trial. J Gen Intern Med. 2021. 10.1007/s11606-020-06416-7. Epub ahead of print. PMID: 33479931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Liberman T, Kozikowski A, Kwon N, Emmert B, Akerman M, Pekmezaris R. Identifying advanced illness patients in the emergency department and having goals‐of‐care discussions to assist with early hospice referral. J Emerg Med. 2018;54(2):191‐197. [DOI] [PubMed] [Google Scholar]
- 29. Ouchi K, George N, Schuur JD, et al. Goals‐of‐care conversations for older adults with serious illness in the emergency department: challenges and opportunities. Ann Emerg Med. 2019;74(2):276‐284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ouchi K, Lawton AJ, Bowman J, Bernacki R, George N. Managing code status conversations for seriously ill older adults in respiratory failure. Ann Emerg Med. 2020;76(6):751‐756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lwin N, Burgess J, Johnston C, Johnson N, Chung S. Hospital‐in‐the‐Home experience of first 23 COVID‐19 patients at a regional NSW hospital. Intern Med J. 2020;50(10):1271‐1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Coloma E, Nicolás D. Hospital at home units in the post‐COVID 19 era. Eur J Clin Invest. 2020;50(11):e13390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Levine DM, Desai MP, Ross J, Como N, Anne Gill E. Rural perceptions of acute care at home: a qualitative analysis. J Rural Health. 2021. [DOI] [PubMed] [Google Scholar]
- 34. Levine DM, Ross J, Como N, Holley S. Scoping and testing rural acute care at home: a simulation analysis. BMJ Innov. 2021:1‐9. press. [Google Scholar]
- 35. Nogués X, Sánchez‐Martinez F, Castells X, et al. Hospital‐at‐home expands hospital capacity during COVID‐19 pandemic. J Post‐Acute Long‐Term Care Med. 2021;22(5):939‐942. Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Diagnostic and Statistical Manual of Mental Disorders: DSM‐5. 5th ed. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 37. LaMantia MA, Messina FC, Hobgood CD, Miller DK. Screening for delirium in the emergency department: a systematic review. Ann Emerg Med. 2014;63(5):551‐560. [DOI] [PubMed] [Google Scholar]
- 38. Vasilevskis EE, Han JH, Hughes CG, Ely EW. Epidemiology and risk factors for delirium across hospital settings. Best Pract Res Clin Anaesthesiol. 2012;26(3):277‐287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Siddiqi N, Harrison JK, Clegg A, et al. Interventions for preventing delirium in hospitalised non‐ICU patients. Cochrane Database Syst Rev. 2016;3:CD005563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hshieh TT, Yue J, Oh E, et al. Effectiveness of multicomponent nonpharmacological delirium interventions: a meta‐analysis. JAMA Intern Med. 2015;175(4):512‐520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Chia J, Eeles EM, Tattam K, Yerkovich S. Outcomes for patients with delirium receiving hospital‐in‐the‐home treatment: an Australian perspective. Australas J Ageing. 2020;39(2):e215‐e219. [DOI] [PubMed] [Google Scholar]
- 42. Adams CM, Tancredi DJ, Bell JF, Catz SL, Romano PS. Associations between home injury falls and prior hospitalizations in community dwelling older adults: a population case‐crossover study. Injury. 2020;51(2):260‐266. [DOI] [PubMed] [Google Scholar]
- 43. Lazarus BA, Murphy JB, Coletta EM, McQuade WH, Culpepper L. The provision of physical activity to hospitalized elderly patients. Arch Intern Med. 1991;151(12):2452‐2456. [PubMed] [Google Scholar]
- 44. Gill TM, Allore HG, Holford TR, Guo Z. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004;292(17):2115‐2124. [DOI] [PubMed] [Google Scholar]
- 45. Wilson A, Wynn A, Parker H. Patient and carer satisfaction with ‘hospital at home’: quantitative and qualitative results from a randomised controlled trial. Br J Gen Pract. 2002;52(474):9‐13. [PMC free article] [PubMed] [Google Scholar]
- 46. Leff B, Burton L, Mader SL, et al. Comparison of functional outcomes associated with hospital at home care and traditional acute hospital care. J Am Geriatr Soc. 2009;57(2):273‐278. [DOI] [PubMed] [Google Scholar]
- 47. Kamdar BB, Needham DM, Collop NA. Sleep deprivation in critical illness: its role in physical and psychological recovery. J Intensive Care Med. 2012;27(2):97‐111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Mazur K, Wilczynski K, Szewieczek J. Geriatric falls in the context of a hospital fall prevention program: delirium, low body mass index, and other risk factors. Clin Interv Aging. 2016;11:1253‐1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. McCusker J, Cole M, Abrahamowicz M, Han L, Podoba JE, Ramman‐Haddad L. Environmental risk factors for delirium in hospitalized older people. J Am Geriatr Soc. 2001;49(10):1327‐1334. [DOI] [PubMed] [Google Scholar]
- 50. Davenport K, Alazemi M, Sri‐On J, Liu S. Missed opportunities to diagnose and intervene in modifiable risk factors for older emergency department patients presenting after a fall. Ann Emerg Med. 2020;76(6):730‐738. [DOI] [PubMed] [Google Scholar]
- 51. Luger E, Dorner TE, Haider S, Kapan A, Lackinger C, Schindler K. Effects of a home‐based and volunteer‐administered physical training, nutritional, and social support program on malnutrition and frailty in older persons: a randomized controlled trial. J Am Med Dir Assoc. 2016;17(7):e679‐671. [DOI] [PubMed] [Google Scholar]
- 52. Gately ME, Trudeau SA, Moo LR. Feasibility of telehealth‐delivered home safety evaluations for caregivers of clients with dementia. OTJR (Thorofare N J). 2020;40(1):42‐49. [DOI] [PubMed] [Google Scholar]
- 53. Keall MD, Pierse N, Howden‐Chapman P, et al. Home modifications to reduce injuries from falls in the home injury prevention intervention (HIPI) study: a cluster‐randomised controlled trial. Lancet. 2015;385(9964):231‐238. [DOI] [PubMed] [Google Scholar]
- 54. Mooney K, Titchener K, Haaland B, et al. Evaluation of oncology hospital at home: unplanned health care utilization and costs in the huntsman at home real‐world trial. J Clin Oncol. 2021:JCO2003609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Mooney K, Titchener K, Haaland B, et al. The oncology hospital at home: health care utilization outcomes from the huntsman at home trial. J Clin Oncol. 2020;38:7000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Talcott JA, Yeap BY, Clark JA, et al. Safety of early discharge for low‐risk patients with febrile neutropenia: a multicenter randomized controlled trial. J Clin Oncol. 2011;29(30):3977‐3983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Bryan AF, Levine DM, Tsai TC. Home hospital for surgery [published online ahead of print April 28, 2021]. JAMA Surg. 10.1001/jamasurg.2021.0597 [DOI] [PubMed] [Google Scholar]
- 58. Levine DM, Paz M, Burke K, Schnipper JL. Predictors and reasons why patients decline to participate in home hospital: a mixed methods analysis of a randomized controlled trial. J Gen Intern Med. 2021. 10.1007/s11606-021-06833-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Kant RE, Vejar M, Parnes B, et al. Outcomes and provider perspectives on geriatric care by a nurse practitioner‐led community paramedicine program. Geriatr Nurs. 2018;39(5):574‐579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Peake JM, Kerr G, Sullivan JP. A critical review of consumer wearables, mobile applications, and equipment for providing biofeedback, monitoring stress, and sleep in physically active populations. Front Physiol. 2018;9:743. [DOI] [PMC free article] [PubMed] [Google Scholar]


