Abstract
BACKGROUND
Frailty predisposes patients to poor postoperative outcomes. We evaluated whether using local rather than general anesthesia for hernia repair could mitigate effects of frailty.
METHODS
We used the Risk Analysis Index(RAI) to identify 8,038 frail patients in the 1998–2018 Veterans Affairs Surgical Quality Improvement Program database who underwent elective, open unilateral inguinal hernia repair under local or general anesthesia. Our outcome of interest was the incidence of postoperative complications.
RESULTS
In total, 5,188(65%) patients received general anesthesia and 2,850(35%) received local. Local anesthesia was associated with a 48% reduction in complications (OR 0.52, 95%CI 0.38–0.72). Among the frailest patients (RAI≥70), predicted probability of a postoperative complication ranged from 22–33% with general anesthesia, compared to 13–21% with local.
CONCLUSIONS
Local anesthesia was associated with a ~50% reduction in postoperative complications in frail Veterans. Given the paucity of interventions for frail patients, there is an urgent need for a randomized trial comparing effects of anesthesia modality on postoperative complications in this vulnerable population.
Keywords: Frailty, Inguinal hernia repair, Veterans, Outcomes, Local anesthesia
INTRODUCTION
Frailty is characterized by a decrease in physiologic reserve and is associated with significant postoperative morbidity and mortality even for otherwise low-risk procedures.1 There are few interventions that improve postoperative outcomes for frail patients, which is particularly troubling because the number of frail older adults is expected to dramatically increase over the next 20 years.2,3 Consequently, there is an urgent need to either develop new interventions to reduce postoperative risk for frail patients, or to leverage existing techniques that reduce morbidity and mortality for this vulnerable population.4
Inguinal hernia repair is the most common general surgery procedure performed in the US, with 800,000 operations annually.5 The operation can be performed under local or general anesthesia, with several studies suggesting that local anesthesia is associated with better postoperative recovery.5–8 However, prior randomized trials and observational studies have focused on relatively healthy patients with limited comorbidity burdens.8,9 Although many surgeons would argue that local anesthesia is beneficial for frail patients, the potential benefits of local compared to general anesthesia for frail patients having inguinal hernia repair has not previously been evaluated.
The aim of this study was to determine the benefits of using local as opposed to general anesthesia for frail patients having inguinal hernia repair. We hypothesized that using local anesthesia for inguinal hernia repair in frail patients would be associated with a significant decrease in postoperative complications. We also hypothesized that local anesthesia would be associated with reduced operative time and more rapid postoperative recovery.
MATERIALS AND METHODS
Data source and patient selection
After approval by the Institutional Review Board of the VA North Texas Health Care System, we screened the Veterans Association Surgical Quality Improvement Program (VASQIP) database to identify Veterans having elective, unilateral, open inguinal hernia repair (Common Procedure Terminology code 49505) from 1998–2018. (Figure 1).
Figure 1.
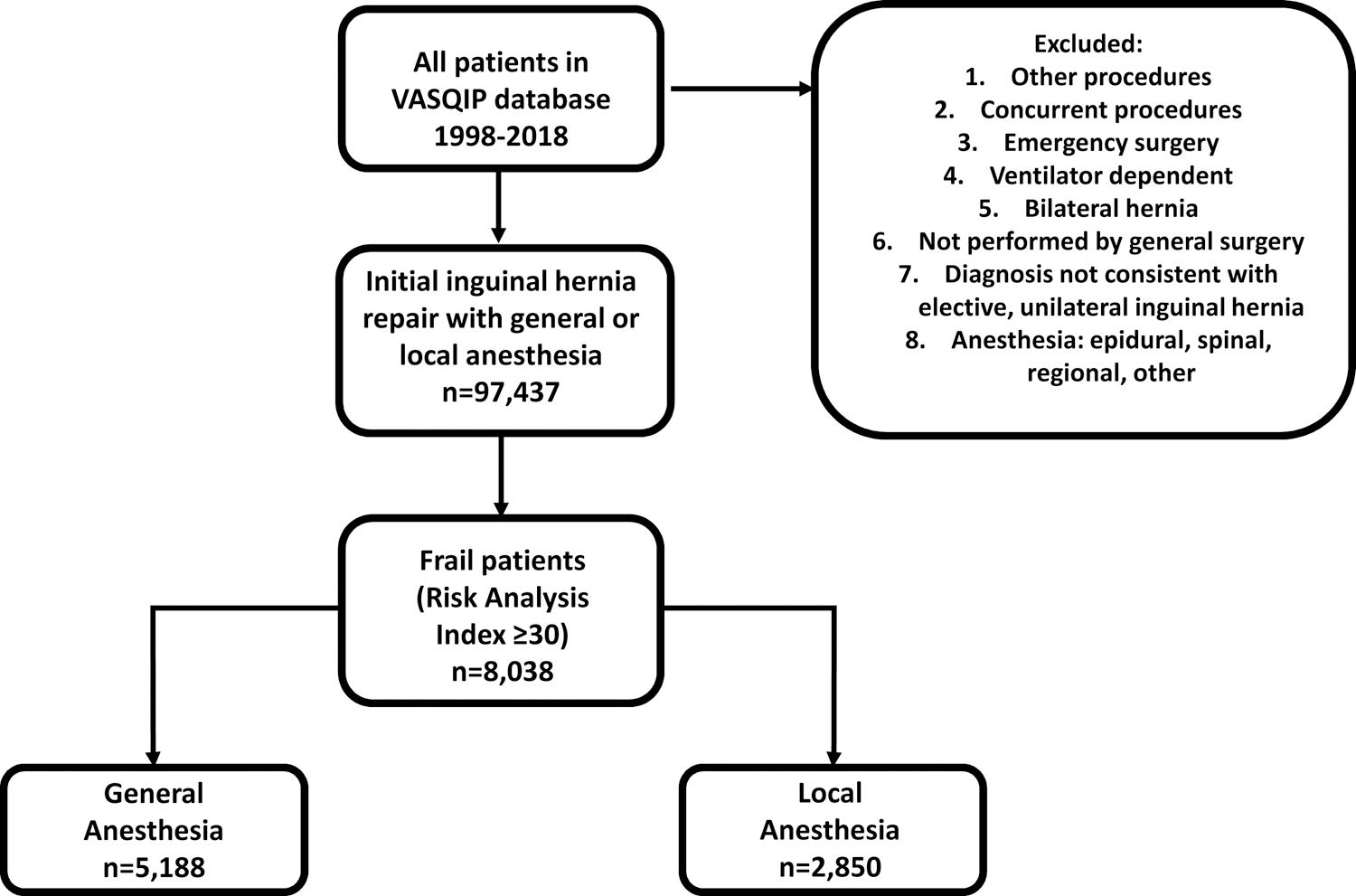
Frail Veterans undergoing open inguinal hernia repair with local and general anesthesia were selected from the Veterans Affairs Surgical Quality Improvement Program database from 1998–2018.
We excluded Veterans who had concurrent procedures, other procedures not consistent with inguinal hernia repair, bilateral hernias, preoperative ventilator dependence, and did not include those whose procedures were not performed by a general surgeon or their anesthesia was coded as epidural, spinal, regional, other, or unknown.
Assessment of frailty
We measured frailty using the Risk Analysis Index (RAI), a recently validated measure of frailty developed using VASQIP data. This index takes dyspnea, functional status, residence, sex, and comorbid conditions into account and creates a summary score. Per the original report, Veterans were considered frail if RAI ≥ 30, and each 5-point increase in RAI was associated with a doubling of predicted mortality.10,11
Outcomes
The primary outcome was occurrence of any postoperative complication within 30 days of surgery. Complications captured by VASQIP include wound infection, dehiscence, pneumonia, re-intubation, pulmonary embolus, failure to wean from the ventilator, renal insufficiency/failure, urinary tract infection, stroke, cardiac arrest, myocardial infarction, postoperative bleeding that requires transfusion, deep vein thrombosis, sepsis/septic shock, and reoperation.
Secondary outcomes included: total operative time (entry to exit from the operating room), and post-anesthesia care unit (PACU) time.
Independent variable
The primary variable/exposure was use of local versus general anesthesia.
Statistical analysis
We used generalized estimating equations to measure effects of local anesthesia on postoperative complications, controlling for clustering within hospitals and adjusting for known confounders such as age, RAI score, race/ethnicity, post-graduate year of the surgeon of record, functional status, and comorbid conditions. For continuous dependent variables, we used hierarchical linear regression with hospitals treated as random effects. Time outcomes were log transformed to enhance model performance, so results are expressed in terms of semi-elasticities (percent change in the dependent variable for a unit change in the independent variable). We assessed functional forms for continuous variables and ran standard model diagnostics, including residual plots, to assess fit and adequacy of model assumptions. Analysis was performed with Stata version 15. Between-group differences were considered significant at α<0.05.
RESULTS
Patient characteristics
We identified 8,038 frail Veterans, 35.5% of whom underwent inguinal hernia repair under local anesthesia, and 64.5% of whom received general anesthesia for this surgery. Compared to those who received general anesthesia, frail Veterans who received local anesthesia were older (81 vs 78 years, p<0.001) but had similar American Society of Anesthesiologists classification and overall comorbidity burdens (Table 1). Veterans who received local anesthesia also were more likely to have attending surgeons as the primary surgeon of record.
Table 1.
Patient characteristics. All values represent N(%) unless otherwise specified
| General | Local | p-value | |
|---|---|---|---|
| N = 5,188 | N = 2,850 | ||
| Age, median (IQR) | 78 (72–85) | 81 (76–86) | p<0.001 |
| Male gender | 5,183 (99.9%) | 2,847 (99.9%) | p=0.90 |
| Race & ethnicity | p<0.001 | ||
| White | 3,456 (66.6%) | 2,102 (73.8%) | |
| Black | 846 (16.3%) | 304 (10.7%) | |
| Hispanic | 143 (2.8%) | 64 (2.2%) | |
| Other | 34 (0.7%) | 17 (0.6%) | |
| Unknown | 709 (13.7%) | 363 (12.7%) | |
| Risk Analysis Index, median (IQR) | 32 (31–35) | 32 (31–36) | p<0.001 |
| Risk Analysis Index (RAI) category | p<0.001 | ||
| RAI 30–34 | 3,687 (71.1%) | 1,985 (69.7%) | |
| RAI 35–39 | 1,124 (21.7%) | 598 (21.0%) | |
| RAI 40–44 | 261 (5.0%) | 189 (6.6%) | |
| RAI 45–49 | 98 (1.9%) | 52 (1.8%) | |
| RAI 50+ | 18 (0.4%) | 26 (0.9%) | |
| American Society of Anesthesiologists class | p=0.55 | ||
| 1 | 10 (0.2%) | 9 (0.3%) | |
| 2 | 637 (12.3%) | 350 (12.3%) | |
| 3+ | 4,539 (87.5%) | 2,490 (87.4%) | |
| Functional status preoperatively | p=0.93 | ||
| Independent | 4,224 (81.4%) | 2,321 (81.4%) | |
| Totally/partially dependent | 964 (18.6%) | 527 (18.5%) | |
| Post-graduate year of surgeon | p<0.001 | ||
| Attending | 2,033 (39.2%) | 1,396 (49.0%) | |
| Intern | 662 (12.8%) | 466 (16.4%) | |
| Second year | 691 (13.3%) | 276 (9.7%) | |
| Third year | 595 (11.5%) | 285 (10.0%) | |
| Fourth year | 312 (6.0%) | 115 (4.0%) | |
| Chief resident | 804 (15.5%) | 291 (10.2%) | |
| Post graduate year>5 | 91 (1.8%) | 21 (0.7%) | |
| Wound class | p=0.71 | ||
| Clean | 4,979 (96.0%) | 2,740 (96.1%) | |
| Clean/contaminated/Infected | 209 (4.0%) | 110 (3.9%) | |
| Diabetes | p=0.002 | ||
| None/controlled with diet | 4,404 (84.9%) | 2,496 (87.6%) | |
| Oral medications | 538 (10.4%) | 231 (8.1%) | |
| Insulin | 246 (4.7%) | 123 (4.3%) | |
| Dyspnea preoperatively | p<0.001 | ||
| None | 3,591 (69.2%) | 1,824 (64.0%) | |
| Minimal exertion | 1,497 (28.9%) | 925 (32.5%) | |
| At rest | 86 (1.7%) | 76 (2.7%) | |
| Alcohol use | 243 (4.7%) | 125 (4.4%) | p=0.54 |
| Congestive heart failure | 1,065 (20.7%) | 405 (14.3%) | p<0.001 |
| Preoperative stroke with deficit | 777 (15.0%) | 409 (14.4%) | p=0.45 |
| Preoperative stroke without deficit | 262 (5.1%) | 150 (5.3%) | p=0.68 |
| Hemiplegia | 341 (6.6%) | 178 (6.2%) | p=0.57 |
| Preoperative transient ischemic attack | 291 (5.6%) | 162 (5.7%) | p=0.89 |
| Bleeding disorder | 332 (6.4%) | 178 (6.2%) | p=0.79 |
| Disseminated cancer | 188 (3.6%) | 109 (3.8%) | p=0.65 |
| Steroid use | 119 (2.3%) | 110 (3.9%) | p<0.001 |
| Weight loss | 362 (7.0%) | 175 (6.1%) | p=0.15 |
| Chronic obstructive pulmonary disease | 1,143 (22.0%) | 739 (25.9%) | p<0.001 |
| Admission Status | p<0.001 | ||
| Inpatient | 718 (13.8%) | 293 (10.3%) | |
| Outpatient | 4,467 (86.1%) | 2,557 (89.7%) |
Local anesthesia was associated with fewer postoperative complications in frail Veterans
Prior to risk-adjustment, frail Veterans who received local anesthesia had a significantly lower rate of postoperative complications (1.8%) than those who received general anesthesia (3.1%) (p<0.0001, Table 1). When we looked at specific complications, the low incidence of individual complications made it difficult to detect significant differences. However, local anesthesia was associated with significantly fewer urinary tract infections (0.5% versus 1%, p<0.012) postoperative intubations (0.04% versus 0.3%, p<0.02), and superficial surgical site infections (0.2% versus 0.5%, p<0.04, Supplemental Table 1). For other VASQIP complications, local anesthesia was typically associated with a reduced incidence compared to general anesthesia, but the differences were not statistically significant.
As expected, higher RAI scores were associated with a significant increase in postoperative complications, with each point above 30 associated with a 6% increase in the odds of complications (OR 1.06, 95% CI 1.01–1.12). However, using local as an alternative to general anesthesia was associated with a significant attenuation of this risk (Figure 2A). After adjusting for factors listed in Table 1, local anesthesia was associated with a 48% decrease in the odds of developing a postoperative complication for frail Veterans (OR 0.52, 95% CI 0.38–0.72).
Figure 2.
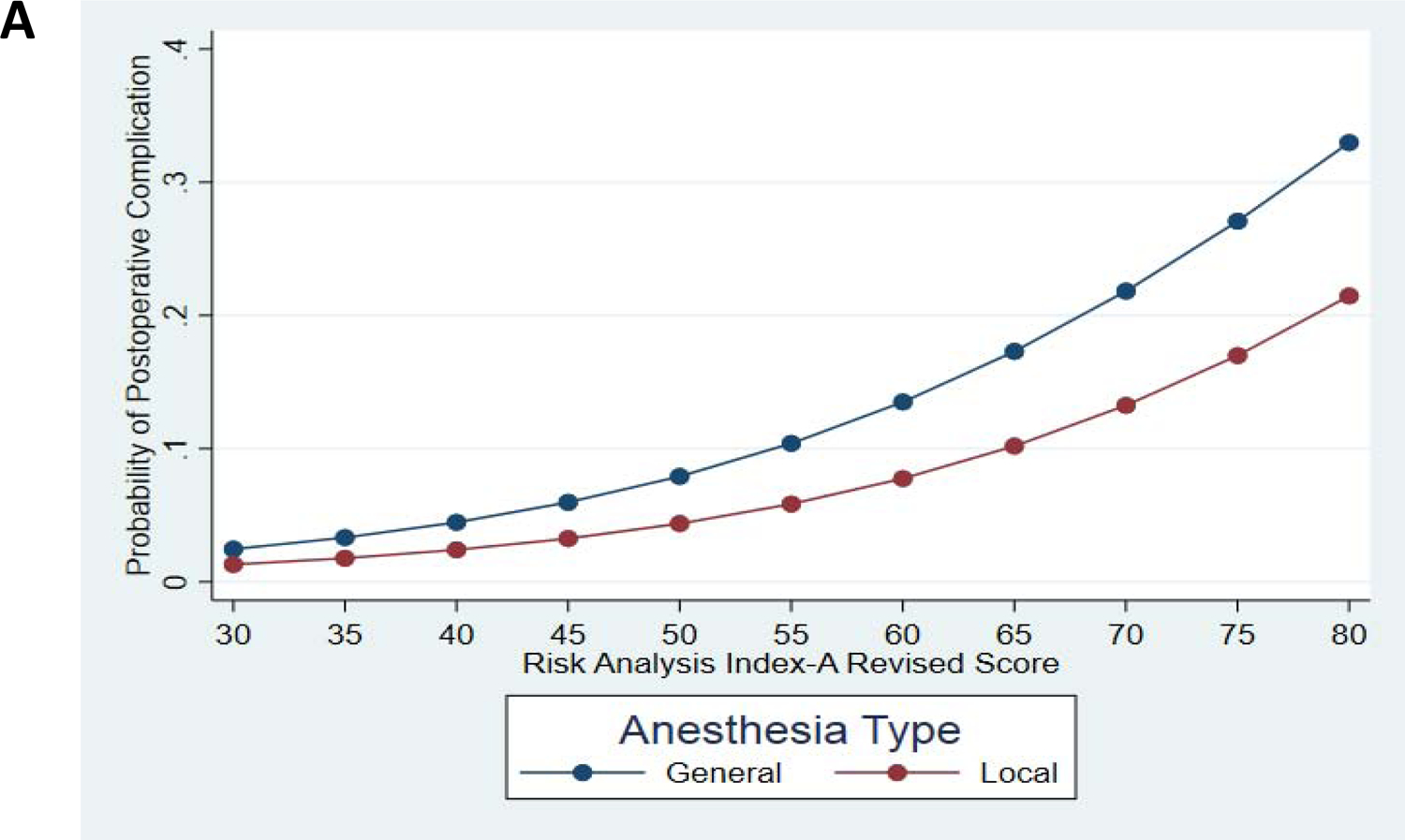
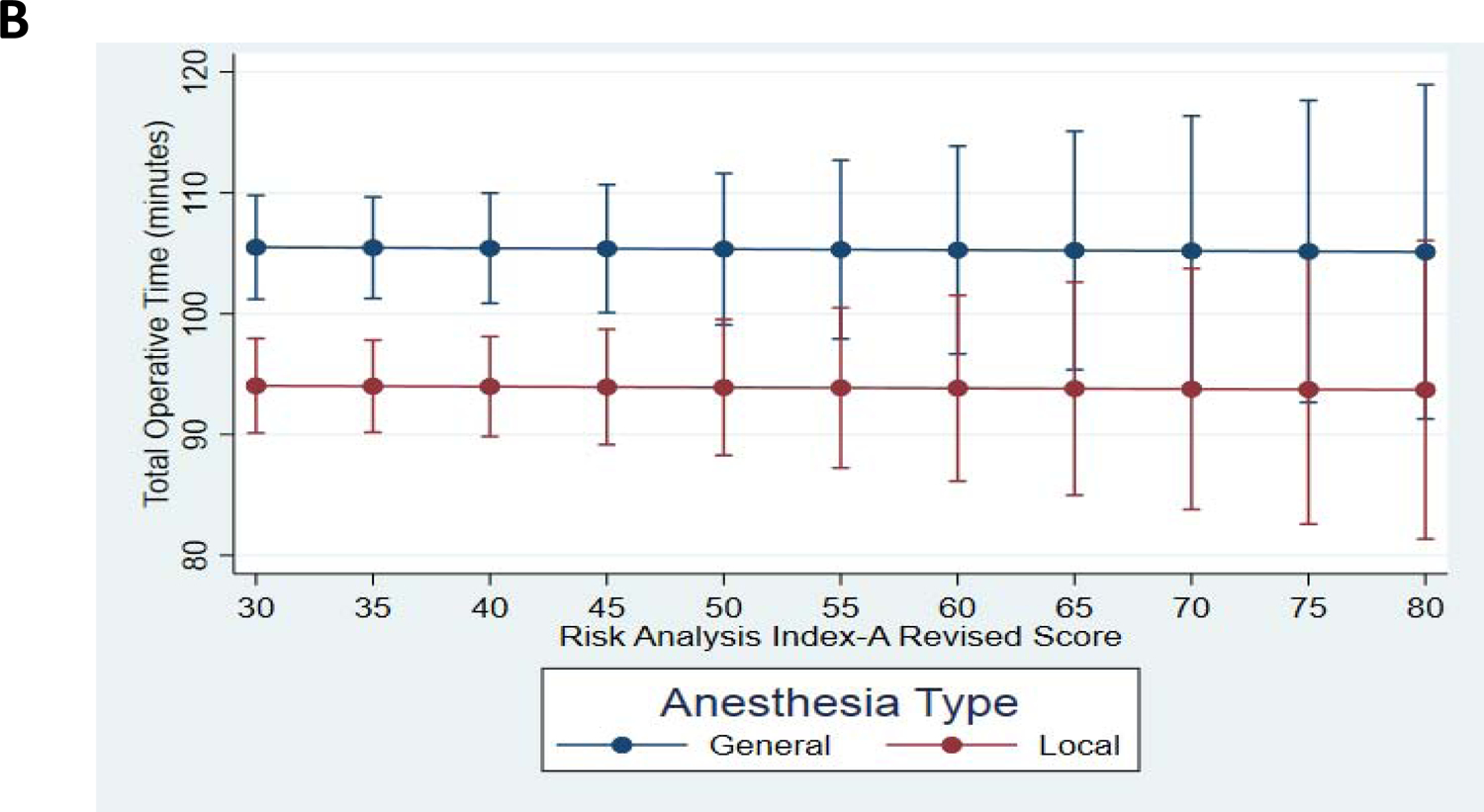
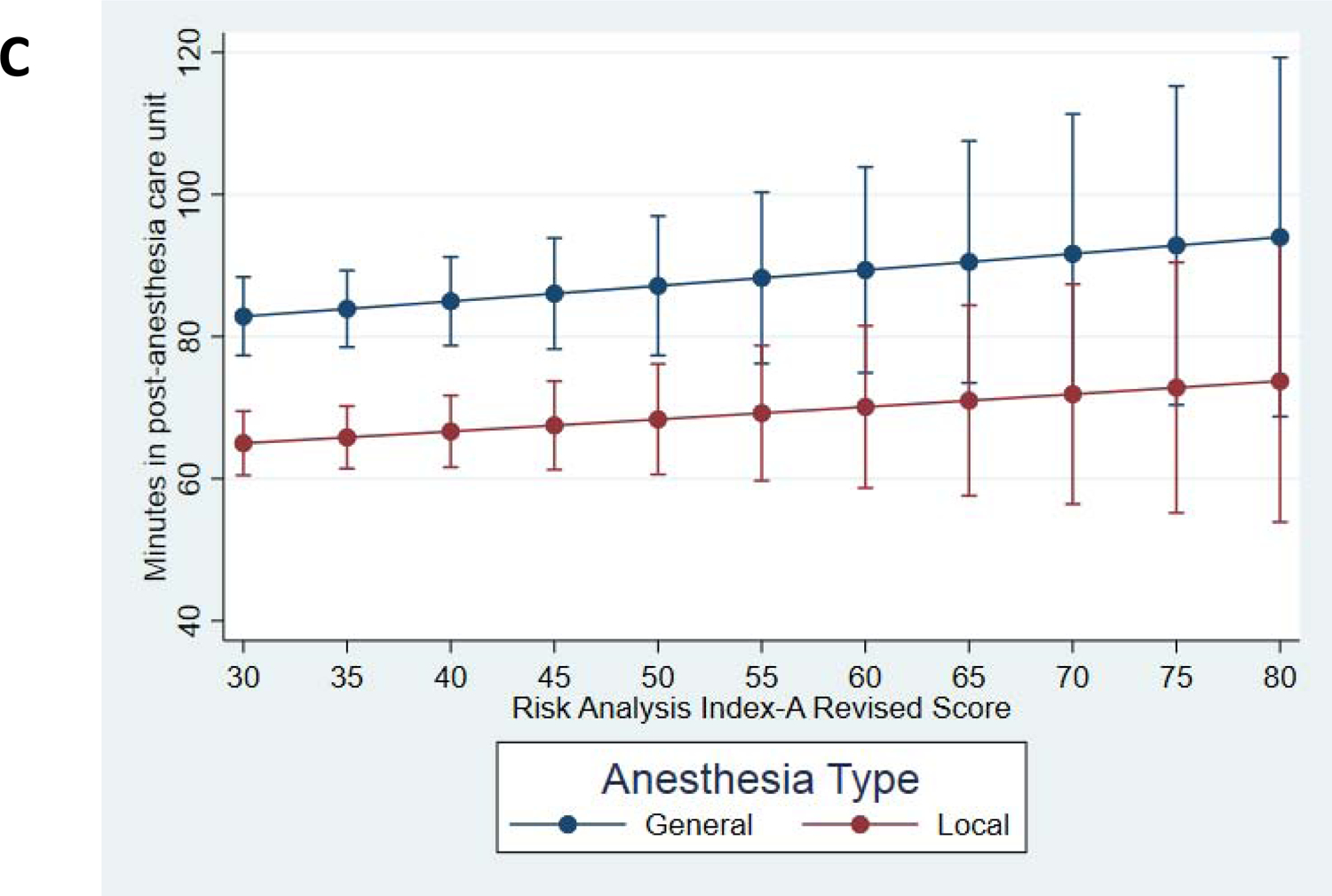
Frail Veterans who received local as opposed to general anesthesia had a reduced risk of complications (2A), faster operative time (2B), and reduced recovery time (2C).
The frailest Veterans (RAI 70–80) had a ~10% decrease in their risk of postoperative complications when local as opposed to general anesthesia was used, though the small sample size for Veterans with this degree of frailty made it difficult to establish stable estimates (Figure 2A, Table 2). As shown in Table 2, Veterans with an RAI of 70–80 had a 22–33% predicted probability of postoperative complications with general anesthesia. Conversely, Veterans with this degree of frailty who underwent inguinal hernia repair under local anesthesia had only a 13–21% predicted probability of developing a postoperative complication. Although the small sample sizes at this degree of frailty made the model estimate somewhat unstable, the overall trend for lower complications with local compared to general anesthesia persisted across the full spectrum of frailty.
Table 2.
Risk-adjusted predicted probability of complications based on risk analysis index score.
| Risk analysis index | General anesthesia | Local anesthesia | ||
|---|---|---|---|---|
| Predicted probability of complication (SE) | 95% CI | Predicted probability of complication (SE) | 95% CI | |
| 30 | 2.4% (0.33) | 1.8%−3.1% | 1.3% (0.26) | 0.8%−1.8% |
| 35 | 3.3% (0.25) | 2.8%−3.8% | 1.8% (0.26) | 1.2%−2.3% |
| 40 | 4.5% (0.75) | 3.0%−5.9% | 2.4% (0.49) | 1.4%−3.4% |
| 45 | 6.0% (1.7) | 2.6%−9.3% | 3.3% (1.0) | 1.3%−5.2% |
| 50 | 7.9% (3.2) | 1.7%−14.1% | 4.4% (1.9) | 0.7%−8.0% |
| 55 | 10.4% (5.2) | 0.15%−20.6% | 5.8% (3.1) | −0.3%−12.0% |
| 60 | 13.5% (8.0) | −2.2%−29.2% | 7.8% (5.0) | −2.0%−17.5% |
| 65 | 17.3% (11.5) | −5.3%−40.0% | 10.2% (7.5) | −4.5%−24.9% |
| 70 | 21.8% (15.8) | −9.1%−52.8% | 13.2% (10.8) | −8.0%−34.5% |
| 75 | 27.1% (20.6) | −13.2%−67.4% | 17.0% (15.0) | −12.3%−46.3% |
| 80 | 33.0% (25.5) | −17.0%−83.0% | 21.5% (19.8) | −17.3%−60.3% |
Local anesthesia was associated with shorter operative times and more rapid discharge from the post-anesthesia care unit in frail Veterans
After adjusting for the factors in Table 1, local anesthesia was associated with an 11% (~11 minute) decrease in operative time (95% CI 13% – 10% decrease) compared to general anesthesia (Figure 2B). This effect was consistent across the range of RAI scores. Additionally, using local rather than general anesthesia was associated with a 24% decrease (95% CI 27% – 21%) in time spent in the post-anesthesia care unit, possibly indicating a more rapid short-term recovery from surgery. Similar to operative time, the benefits of local anesthesia were consistent across the range of frailty (Figure 2C).
DISCUSSION
This study demonstrates that the use of local as opposed to general anesthesia for inguinal hernia repair was associated with a profound decrease in complications, operative time, and postoperative recovery time in frail Veterans. The benefits of choosing local over general anesthesia were evident not only for the frailest Veterans, but across the full spectrum of frailty. This is especially encouraging because frail adults have poor postoperative outcomes, even for minor procedures, and there are few interventions with potential to improve their postoperative recovery.1,12 Additionally, time in the operating room and post-anesthesia care units is among the most expensive and labor-intensive aspects of hospital care. By decreasing time in both settings, using local anesthesia could significantly decrease health care costs.
Our results are consistent with previous studies that showed potentially enhanced recovery when surgeons use local anesthesia for hernia repair. However, unlike prior randomized trials that excluded older and frail patients, we explicitly examined potential benefits of local anesthesia in a vulnerable population.6–8 Although the assumption in surgery has long been that using alternatives to general anesthesia will be beneficial for frail patients, our study is the first to actually quantify and confirm this effect for inguinal hernia repair.
There have been several proposed interventions to improve outcomes for frail patients. Commonly used interventions include exercise therapy or multidisciplinary geriatric teams.3 Exercise therapy-completing a few weeks or months of a program designed to improve strength and physical function- has been effective in improving strength and reducing complications following major abdominal surgery. However, the fact that up to 10% of those randomized did not complete the exercise intervention and many more were unwilling to even participate in the trials significantly limits their dissemination, implementation, and ultimately, impact.13 Multidisciplinary geriatric team interventions that involve preoperative screening and postoperative placement of older adults in dedicated units staffed by clinical and other staff with specialty training in geriatric medicine have also demonstrated improvements in mobility and cognition in orthopedic and other patients.14,15 However, many hospitals lack the resources to provide such dedicated geriatric care, and the benefits of these programs are typically limited to inpatient procedures.3,15 By contrast, it is relatively simple to offer local anesthesia as an option for frail surgical patients. Most anesthesiologists are at least somewhat familiar with the technique, and surgeons repair hernias in the same fashion regardless of anesthetic approach. Consequently, with minimal training and practice, most hospitals can effectively employ local anesthesia for hernia repair and potentially improve outcomes for an extremely vulnerable population. Local anesthesia is also likely to reduce costs because implementing this approach requires no new resources and can reduce operative and PACU time.
Although we have demonstrated a significant association between use of local anesthesia and improved outcomes for frail Veterans, there are several limitations which must be acknowledged. First, the retrospective design of this study means there is potential for unknown confounding which could account for some of the difference noted. However, even if 50% of the observed effect is due to unmeasured confounding, there would still be a strong association between local anesthesia and both reduced complications and improved outcomes. Additionally, by analyzing only frail patients we are already balancing the main confounder (patient ability to tolerate an operation) that influences choice of anesthesia modality. Secondly, the VASQIP database does not record several complications that could be relevant for frail Veterans, including rates of urinary retention, changes in postoperative functional status, or delirium/cognitive changes. The inability to include these complications in our analysis is likely to bias results toward the null, as prior work suggests that local may be superior to general anesthesia with respect to these outcomes.8 Finally, VASQIP does not include specific information on the hernia and techniques used for repair, but it is unlikely that there are systematic biases in approach that would affect our findings.
Although our results suggest that using local anesthesia may offer several benefits for frail patients, we also think it is important to note that there are situations where this is not a viable option. Some patients may strongly prefer general anesthesia regardless of the benefit. It may be more comfortable for the patient if surgeons repair some large or chronically incarcerated hernias under general anesthesia. Finally, bilateral or recurrent hernias may be more effectively repaired laparoscopically and those repairs require using general anesthesia.
CONCLUSIONS
In summary, our large cohort study suggests that surgeons should consider using local rather than general anesthesia for frail patients undergoing open inguinal hernia repair, given the strong association with enhanced recovery. Compared to other interventions that aim to improve outcomes for frail patients, these data suggest that using local anesthesia offers substantial benefit with little cost to hospitals and health systems. Given the observational design of this study, it will be important to test these results in a prospective randomized trial.
Supplementary Material
Local anesthesia may mitigate the effect of frailty for inguinal hernia repair.
Surgeons should consider local rather than general anesthesia for frail Veterans.
Local anesthesia also is associated with reduced operative/recovery time.
ACKNOWLEDGEMENTS
All authors contributed to writing and critical revision of the manuscript. C.B., M.B., J.M. and J.R. contributed to the conception, design, and acquisition of data of the research presented in this article. All authors were responsible for data analysis and interpretation.
This work was supported by a GEMSSTAR grant from the National Institute of Aging (1R03AG056330; for C.J.B.). Dr. Brown was supported, in part, by a VA Rehabilitation R&D Merit Award (1 I01 RX001995). MB acknowledges funding support from National Institutes of Health Beeson K76AG057022 and additional support from National Institutes of Health P30AG028716 and the Duke Anesthesiology Department.
This work was selected for presentation at the Association of VA Surgeons 4/20/20 (cancelled).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Accepted for presentation at the 2020 Association of VA Surgeons Annual Meeting.
REFERENCES
- 1.Makary MA, Segev DL, Pronovost PJ, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010;210(6):901–908. [DOI] [PubMed] [Google Scholar]
- 2.Verver D, Merten H, de Blok C, Wagner C. A cross sectional study on the different domains of frailty for independent living older adults. BMC Geriatr. 2019;19(1):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McIsaac DI, Jen T, Mookerji N, Patel A, Lalu MM. Interventions to improve the outcomes of frail people having surgery: A systematic review. PLoS One. 2017;12(12):e0190071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mull HJ, Rosen AK, Pizer SD, Itani KM. Association Between Postoperative Admission and Location of Hernia Surgery: A Matched Case-Control Study in the Veterans Administration. JAMA Surg. 2016;151(12):1187–1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rutkow IM. Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am. 2003;83(5):1045–1051, v–vi. [DOI] [PubMed] [Google Scholar]
- 6.O’Dwyer PJ, Serpell MG, Millar K, et al. Local or general anesthesia for open hernia repair: a randomized trial. Ann Surg. 2003;237(4):574–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nordin P, Zetterstrom H, Carlsson P, Nilsson E. Cost-effectiveness analysis of local, regional and general anaesthesia for inguinal hernia repair using data from a randomized clinical trial. Br J Surg. 2007;94(4):500–505. [DOI] [PubMed] [Google Scholar]
- 8.Nordin P, Zetterstrom H, Gunnarsson U, Nilsson E. Local, regional, or general anaesthesia in groin hernia repair: multicentre randomised trial. Lancet. 2003;362(9387):853–858. [DOI] [PubMed] [Google Scholar]
- 9.Bhattacharya SD, Vaslef SN, Pappas TN, Scarborough JE. Locoregional versus general anesthesia for open inguinal herniorrhaphy: a National Surgical Quality Improvement Program analysis. Am Surg. 2012;78(7):798–802. [PubMed] [Google Scholar]
- 10.Arya S, Varley P, Youk A, et al. Recalibration and External Validation of the Risk Analysis Index: A Surgical Frailty Assessment Tool. Ann Surg. 2019. [DOI] [PMC free article] [PubMed]
- 11.Hall DE, Arya S, Schmid KK, et al. Development and Initial Validation of the Risk Analysis Index for Measuring Frailty in Surgical Populations. JAMA Surg. 2017;152(2):175–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lin HS, Watts JN, Peel NM, Hubbard RE. Frailty and post-operative outcomes in older surgical patients: a systematic review. BMC Geriatr. 2016;16(1):157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barberan-Garcia A, Ubre M, Roca J, et al. Personalised Prehabilitation in High-risk Patients Undergoing Elective Major Abdominal Surgery: A Randomized Blinded Controlled Trial. Ann Surg. 2018;267(1):50–56. [DOI] [PubMed] [Google Scholar]
- 14.Indrakusuma R, Dunker MS, Peetoom JJ, Schreurs WH. Evaluation of preoperative geriatric assessment of elderly patients with colorectal carcinoma. A retrospective study. Eur J Surg Oncol. 2015;41(1):21–27. [DOI] [PubMed] [Google Scholar]
- 15.Prestmo A, Hagen G, Sletvold O, et al. Comprehensive geriatric care for patients with hip fractures: a prospective, randomised, controlled trial. Lancet. 2015;385(9978):1623–1633. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


