Abstract
Background:
Vegetable intake is below recommended levels among adults served by the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC).
Objective:
The aim of this study was to determine whether a novel, theory-driven, farm-to-WIC intervention to promote vegetable intake showed promise of being successful and is therefore appropriate for efficacy testing.
Design:
From June 2019 to January 2020, the intervention was piloted in 3 WIC agency sites (one randomized to the intervention study group and two to the control group) selected based on similarity in size and the demographics of participants served.
Participants/setting:
Recruited between June 3, 2019 and August 1, 2019, participants were 297 primarily Hispanic adults served by a large WIC agency located in a densely populated urban area in New Jersey (160 were enrolled at the intervention site and 137 at control sites).
Intervention:
The intervention combined behaviorally focused instruction and handouts with the introduction of a WIC-based farmers’ market, field trips to an area farmers’ market, telephone coaching and support before and after trips, and recipe demonstrations and tastings.
Main outcome measures:
The primary outcomes were vegetable intake (measured objectively using dermal carotenoids as a biomarker of intake and via self-report) and the redemption of vouchers provided through the WIC Farmers’ Market Nutrition Program (FMNP) for fruit and vegetable purchases at farmers’ markets (objectively assessed using data provided by WIC).
Statistical analyses performed:
Between-group differences in vegetable intake were examined at mid- and post-intervention (3 and 6 months post-baseline, respectively) with linear mixed-effects models adjusted for baseline vegetable intake and covariates. Logistic regression analysis was used to relate FMNP voucher redemption to study group and covariates.
Results:
At mid-intervention, objectively measured vegetable intake was higher among participants in the control group as compared to the intervention group; self-reported intake did not differ by group. Post-intervention, objectively measured and self-reported vegetable intake were higher among participants in the intervention group as compared to the control group. Receipt of the intervention was associated with a greater likelihood of FMNP voucher redemption. Voucher redemption rates were 87% in the intervention group and 28% in the control group (OR = 17.39, 95% CI [8.64, 35.02]).
Conclusions:
Meaningful associations found between the intervention, vegetable intake, and FMNP voucher redemption suggest that the program is appropriate for efficacy testing.
Keywords: Vegetable intake, farm-to-institution, WIC program, pilot study
INTRODUCTION
Although fruits and vegetables are widely recommended for their health-promoting properties,1 increasing evidence acknowledges a distinction between fruits and vegetables both in their health benefits and consumption patterns.2 The benefits of a diet rich in vegetables also are increasingly recognized.2 A high intake of vegetables has been associated with reduced risk of cardiovascular disease, type 2 diabetes, various cancers, dementia, and cognitive decline.2 Relationships between intakes of specific vegetable types or groups and improved health outcomes also have been found.2 For example, intakes of dark green leafy vegetables have been associated with reduce risk of type 2 diabetes, various cancers, and depression, and intakes of cruciferous, beta-carotene-rich, and yellow- and red-pigmented vegetables have been associated with reduced risk of various cancers.2 Yet, only 9.3% of US adults consume recommended daily amounts of vegetables.3
Low income is a risk factor for low vegetable intake,4 highlighting the need for intervention policies and programs to promote vegetable intake in low-income groups. The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) safeguards the health of low-income, nutritionally at-risk pregnant and postpartum women and preschool children by providing healthy foods to supplement diets, nutrition education, and health care referrals.5 WIC serves more than half of all infants born in the US, along with their mothers, providing a promising opportunity for intervention to promote vegetable intake in low-income families.5
In 1992, Congress established the WIC Farmers’ Market Nutrition Program (FMNP).6 The program provides seasonal vouchers for fruit and vegetable purchases at farmers’ markets.6 Previous work has shown that WIC participants who receive the vouchers have higher vegetable intake and higher fruit and vegetable intake combined relative to those who do not.7,8 Yet, FMNP voucher redemption is low (nationwide in 2019, 55% of voucher recipients redeemed the vouchers).9 Farm-to-institution programs are recommended to facilitate access to fresh fruits and vegetables from regional farms to institutions.10 Comprehensive programs incorporate nutrition education and experiential learning opportunities to build consumer knowledge and skills.10 Programs implemented in urban, underserved areas hold potential for addressing limited vegetable access as a barrier to intake.11 Despite their promise for improving vegetable access and intake, farm-to-WIC interventions are few.
Pilot studies, research undertaken to help investigators prepare for full-scale research leading to intervention, are recommended when there are few published studies using a particular intervention approach.12 Many are designed to test a new approach in a limited way to determine whether it yields trends in the predicted direction, i.e., better outcomes among those who receive the intervention relative to those who do not.12 This pilot study was undertaken to test a novel, theory-driven farm-to-WIC intervention to promote vegetable intake by increasing the use of FMNP vouchers and vegetable-related knowledge, attitudes, and behaviors. Differences between intervention and control study groups in primary outcomes of vegetable intake (assessed objectively using dermal carotenoids as a biomarker of intake and via self-report) and FMNP voucher redemption (objectively assessed using data provided by WIC) were examined. The moderating effects of FMNP voucher redemption also were examined in exploratory analyses. The objective was to determine whether the intervention showed promise of being successful and is therefore appropriate for efficacy testing.12
MATERIALS AND METHODS
Setting, Design, and Sample
The setting was a large, New Jersey-based WIC agency located in a primarily Hispanic urban area. The intervention was piloted in three of the agency’s 17 sites selected based on similarity in size and the demographics of participants served (one randomized to the intervention study group and two to the control group). As the intervention was delivered at the site level, randomization was by site to prevent contamination of the control group. This design is subject to the n=1 confound which occurs when the intervention or control group contains a single study unit, and therefore does not support causal attribution despite random selection of the intervention site.13,14
Inclusion criteria were 1) English- or Spanish-speaking adult, 2) FMNP voucher recipient or caregiver of a child voucher recipient, 3) no known restrictions on food intake, 4) not less than 3 months from expected delivery date (if pregnant), and 5) eligible to receive WIC benefits for at least 6 months after study entry. Not every family is guaranteed to receive FMNP vouchers owing to funding constraints.15 At the time of the study in New Jersey, pregnant, postpartum, and breastfeeding women and children aged 2 to 5 years were eligible to receive the vouchers. Two $10 vouchers per participant were provided; thus, a household consisting of an eligible adult and child would qualify to receive $40 worth of vouchers.
Recruitment occurred from June 3, 2019 to August 1, 2019. Across sites, trained bilingual English/Spanish-speaking research staff contacted participants considered eligible to receive FMNP vouchers based on information provided by WIC by telephone prior to forthcoming appointments, provided a description of the study, and confirmed eligibility. Interested adults were orally administered an outcome battery of self-report measures. During appointments, biometric measures (height, weight, and carotenoid levels) were taken. Participants also were recruited from the WIC clinic where they completed all measures in person. All participants provided informed consent verbally, prior to completing telephone assessments, and in writing prior to completing in-person assessments. Thereafter, a WIC administrator confirmed whether adults completing all assessments had received FMNP vouchers. Those who did not were informed that they were ineligible and were thanked for their involvement. The study was approved by the William Paterson University Institutional Review Board for Human Subject Research (2018–339) and registered with ClinicalTrials.gov (NCT04038385).
In total, 297 adults were enrolled. Participants enrolled at the intervention site (n = 160) received routine services provided by WIC and the farm-to-WIC intervention. Those enrolled at control sites (n = 137) received routine services only. Across sites, all participants were contacted to complete follow-up measures at mid- and post-intervention (3 and 6 months post-baseline, respectively). As at baseline, research staff administered the outcome battery to participants prior to appointments with WIC; during appointments, biometric measures were taken. To enhance retention, across sites, research staff mailed appointment reminders to participants and confirmed appointments via telephone one day in advance, maintained multiple contacts for participants, and updated participants’ contact information at each assessment. Honoraria, gift cards redeemable at local supermarkets and discount chain stores, also were provided to participants for completing successive assessments. Participants received a $10 honorarium at baseline and at mid-intervention; to enhance response rates, the amount was increased to $20 at post-intervention [participants received up to $40 in honoraria in total]).
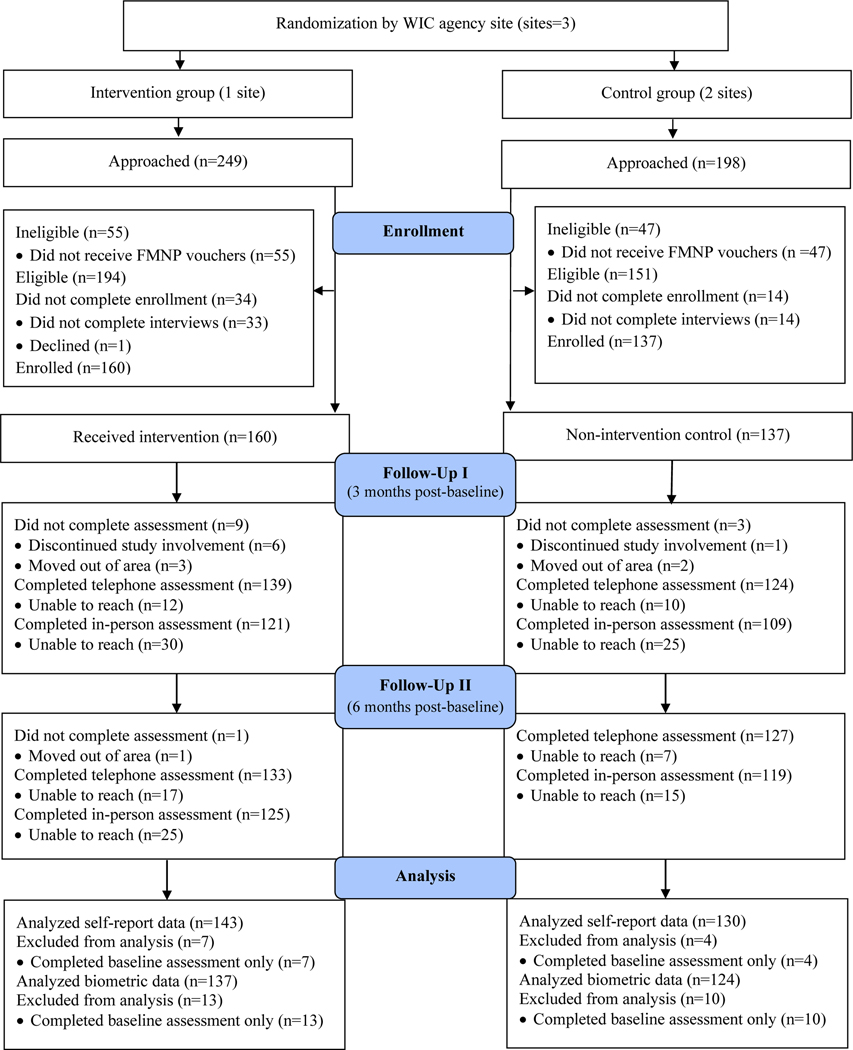
For self-report data assessed via the outcome battery, 273 participants completed at least one post-baseline assessment (143 participants in the intervention group and 130 in the control group); for biometric measures, the corresponding figure was 261 (137 in the intervention group and 124 in the control group). The flow of participants through the study is shown in Figure 1.
Figure 1.
Flow of 297 urban, WIC-enrolled adults through a pilot study of a farm-to-WIC intervention
WIC indicates Special Supplemental Nutrition Program for Women, Infants, and Children; FMNP, Farmers’ Market Nutrition Program
Intervention
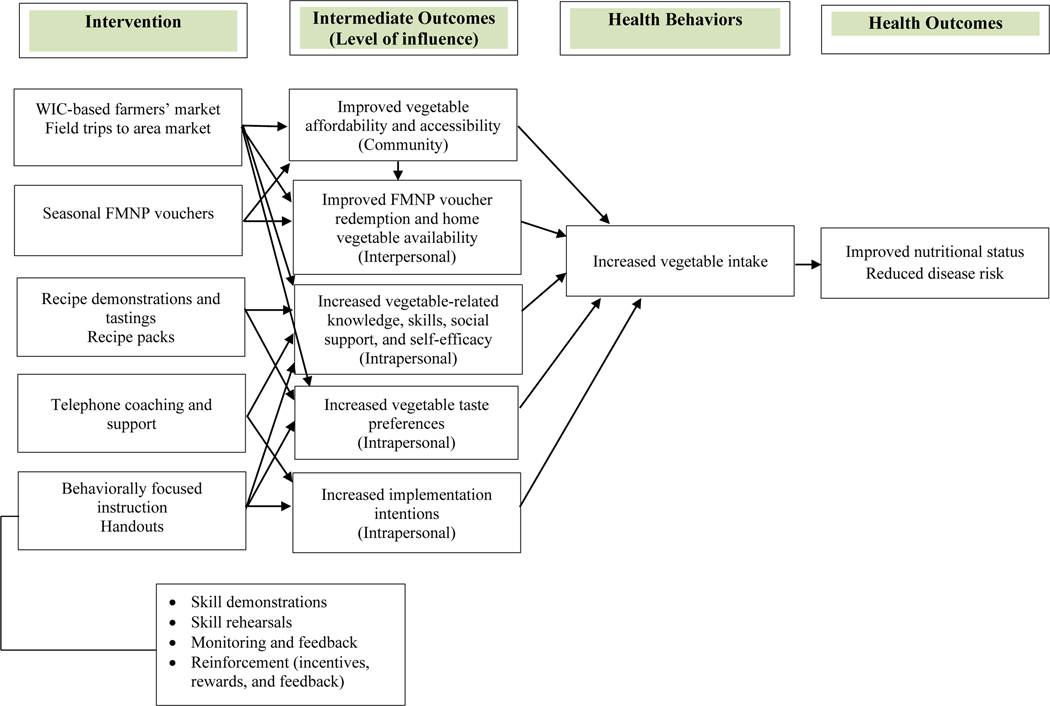
In earlier work, the investigators established the feasibility and user acceptability of the planned intervention,16 supporting further research to pilot the program.12 Conceptually grounded in the Social Ecological Model and Social Cognitive Theory, the intervention consisted of 1) a WIC-based farmers’ market implemented in July and August during the FMNP voucher issuance period to improve community access to vegetables, and among those purchasing items at the market, home vegetable availability; 2) behaviorally focused individual and group-based instruction to enhance social support for vegetable consumption and build relevant knowledge, skills, and self-efficacy; 3) recipe demonstrations and tastings to build vegetable knowledge, preparation skills, and taste preferences, and 4) handouts to reinforce vegetable knowledge and preparation skills.
Based on lessons learned in preliminary work, three monthly field trips to an area farmers’ market or one each in September, October, and November were added to further improve vegetable access, provide opportunities for experiential and hands-on learning, and enable participants to apply knowledge and skills learned at the WIC-based market to a real-world setting. Telephone coaching and support before and after trips also was added to facilitate plans to incorporate vegetables into daily meals. In addition, point-of-sale messaging or posters (in English and Spanish) with information on and strategies to increase vegetable intake were displayed at the WIC-based market to reinforce vegetable knowledge and skills.17–19 Recipe demonstrations and tastings were expanded. In addition to three recipes demonstrated at the WIC-based market, 3 recipes each were demonstrated on trips to the area farmers’ market (12 recipes in total), and after demonstrations and tastings, participants received recipe packs containing the ingredients for one of the recipes to try at home (4 recipe packs in total). The logic model guiding intervention development is shown in Figure 2. New intervention messages and materials were pretested and finalized in in-depth interviews in English and Spanish with 30 adults served by the collaborating WIC agency. The fully developed intervention was implemented between July 1, 2019 and November 30, 2019.
Figure 2.
Logic model for a farm-to-WIC intervention to promote vegetable intake among urban, WIC-enrolled adults
WIC indicates Special Supplemental Nutrition Program for Women, Infants, and Children; FMNP, Farmers’ Market Nutrition Program. Adapted with permission from Liberato SC, Bailie R, Brimblecombe J. Nutrition interventions at point-of-sale to encourage healthier food purchasing: a systematic review. BMC Public Health. 2014;14: 919.
The 5-month intervention was theory-driven, i.e., based on explicit theoretical models as described above.20 The program also was novel, i.e., among the few farm-to-institution initiatives conducted in the WIC setting. Although the promise of establishing a farmers’ market onsite at WIC has been examined,21,22 a difference with other programs was that trained nutrition educators provided behaviorally focused nutrition education and conducted recipe demonstrations and tastings at the market. Moreover, the program was more comprehensive, i.e., included point-of-sale messaging, field trips, and telephone coaching and support not found in existing programs. 21,22
Strategies to ensure cultural sensitivity included matching the intervention to observable characteristics of the targeted population, e.g., using staff matched with participants based on race and Hispanic ethnicity and origin to recruit participants, conduct assessments, and deliver the intervention, and providing intervention materials and measures in English and Spanish.23 Further, the program was structured to recognize cultural values within targeted Hispanic and African American ethnic/racial groups,24 e.g., by communicating motivators for making lifestyle changes reported in preliminary work, i.e., to promote healthy prenatal development and set an example for children to follow. This meets the Latino cultural concept of familismo (familism), including being a positive role model for one’s family and community. The Latino and Afrocentric cultural value of collectivism was incorporated via group-based instruction and by providing social support and opportunities for socializing at on-site and area farmers’ markets.24,25
Measures
At baseline, participants reported their age, race, ethnicity, nativity, language preference and years in the US (if foreign born), pregnancy and breastfeeding status, educational attainment, car ownership and access, supplement use, smoking status, and past 7-day exposure to secondhand smoke. Food security status was assessed with an item from the Household Food Security Survey Module (“Have you or other adults in your household worried whether your food would run out before you got money to buy more?”).26 Meeting physical activity guidelines was assessed with a 2-item measure shown to be reliable with validity similar to that of more detailed self-report activity measures.27 Height and weight were measured by trained research staff with participants wearing light clothing without shoes using standardized methods and equipment.28 Body mass index (BMI) was calculated as weight in kilograms divided by height in square meters.29 As weight and height were measured at the time of study entry, among pregnant participants, weight and height prior to pregnancy and correspondingly, pre-pregnancy BMI could not be determined. Pregnant women (n = 54) were therefore excluded from analyses of BMI. Participants also completed a validated measure of social desirability trait, the tendency to respond to self-report measures in a manner consistent with expected norms.30,31As children aged 2 to 5 years were eligible to receive FMNP vouchers, a measure of the number of children per household aged 2 to 5 years was constructed based on FMNP voucher data provided by WIC.
Vegetable intake was objectively measured with pressure-mediated reflection spectroscopy, a safe, reliable, and valid method for noninvasively assessing dermal carotenoids as a biomarker of intake.32–34 Carotenoid levels were assessed with a portable device, the Veggie Meter® (Longevity Link Inc., Salt Lake City, UT), by scanning the tip of the finger. Scans were conducted in triplicate and the average of the three scans was recorded. Scores can range from zero to 800, with higher scores indicating higher dermal carotenoid levels. Vegetable intake also was assessed via self-report with one of two items in a brief fruit and vegetable screener developed by the National Cancer Institute (“How many cups of vegetables [including 100% vegetable juice] do you eat or drink each day?”).35 To facilitate the estimation of food portions, participants were told that a cup was about the size of their fist.36 FMNP voucher redemption was objectively measured once retrospectively for the entire voucher redemption period (June 1 to November 30, 2019). WIC reported whether participants redeemed any FMNP vouchers (yes/no) during this period.
Statistical Analysis
Differences by study group in baseline participant characteristics and vegetable intake were examined with chi-square analyses and independent samples t tests as appropriate. A reliable adjustment for the clustering of sites after baseline was not analytically possible because the intervention group contained only one site. For this reason, subsequent analyses were not adjusted for the nesting of participants within sites. Overall attrition was 12% for biometric data and 8% for self-report data and was higher in the intervention group relative to the control group (14% and 10%, respectively, for biometric measures and 11% and 5%, respectively, for self-report data). The combination of overall and differential attrition was acceptable by attrition standards; therefore, a formal attrition analysis was not conducted.37
Between-group differences in vegetable intake were examined using linear mixed-effects models with two repeated measures (mid- and post-intervention). Covariates included baseline measures of intake and prognostic factors or potential influences on intake. A common set of prognostic factors was identified for inclusion across analyses, i.e., age, race, breastfeeding status, and exposure to secondhand smoke. When prognostic factors had a different distribution by study group at baseline, they were included as covariates in subsequent analyses. Supplement use, a potential confounder of carotenoid data, and social desirability trait, shown to influence self-reports of behavior, also were included in analyses of objectively measured and self-reported vegetable intake, respectively.31,38 In addition to tests of the significance of differences between least square means by study group at each time point, 95% confidence intervals were estimated for the differences. To quantify the magnitude of between-group differences, adjusted Cohen’s d was calculated as the difference between least square means divided by the square root of the residual variance. Analysis sample sizes were sufficiently large to detect differences as small as d = 0.35 for objectively measured intake and d = 0.34 for self-reported intake with power ≥ 0.80 at the 0.05 significance level in two-tailed tests.
Logistic regression analysis was used to relate FMNP voucher redemption to study group. The analysis was adjusted for the aforementioned covariates, i.e., age, race, breastfeeding status, and exposure to secondhand smoke. Odds ratios (ORs) were estimated with 95% confidence intervals. For FMNP voucher redemption, effect size was measured using ORs, where 1.5 is a small effect, 2.5 is a medium effect, and 4 is a large effect.39
The potential moderating role of FMNP voucher redemption was examined with general linear models relating post-intervention measures of vegetable intake to the redemption of FMNP vouchers in interaction with study group, adjusting for covariates. Adjusted Cohen’s d was estimated among those who redeemed FMNP vouchers and those who did not. Analyses were conducted in February and March 2020 with SAS statistical software, version 9.4.40 Across analyses, P values of < 0.05 indicated statistical significance.
RESULTS
Baseline participant characteristics and vegetable intake are shown in Table 1. Participants had a mean ± SD age of 31.7 ± 7.2 years; most (190 or 64%) reported not identifying as any race, with 189 of the 190 (98%) reporting a Hispanic ethnicity. Of the 297 participants, 217 (73%) were Hispanic. Most Hispanics (82%) were born outside of the U.S. (primarily in the Dominican Republic and Ecuador), with 86% of foreign-born Hispanics preferring to speak Spanish. Small percentages of participants were pregnant (18%) and breastfeeding (25%); 55% reported a high school education or less. Of the 59% of participants who owned a car, 58% reported they could always use the car, whereas 71% of those who did not own a car reported it was difficult or very difficult to borrow a car. Half of participants (51%) were taking supplements, 95% were non-smokers, 15% had recently been exposed to secondhand smoke, 40% were food insecure, and 59% reported meeting physical activity guidelines. The mean BMI in the sample was 29.9 ± 6.9. Most participants were an unhealthy weight (36% and 39%, respectively, were classified in overweight and obese CDC weight status categories).29 Four-fifths of participants (81%) had at least one child aged 2 to 5 years. The mean Veggie Meter score in the sample was 269.54 ± 96.24; on average, participants reported consuming 1.49 ± 1.07 cups of vegetables/day.
Table 1.
Baseline data, by study group, among 297 urban, WIC-enrolled adults participating in a farm-to-WIC intervention
| Characteristic | Intervention (n=160) | Control (n=137) | Entire sample (n=297) | P valuea |
|---|---|---|---|---|
| Age, Mean ± SDb | 30.5 ± 7.2 | 33.1 ± 6.9 | 31.7 ± 7.2 | .001 |
| Race, n (%) | .003 | |||
| Did not identify a race | 111 (70%) | 79 (58%) | 190 (64%) | |
| Black/African American | 26 (16%) | 16 (12%) | 42 (14%) | |
| White or otherc | 23 (14%) | 42 (30%) | 65 (22%) | |
| Hispanic ethnicity, n (%) | .618 | |||
| Non-Hispanic | 45 (28%) | 35 (26%) | 80 (27%) | |
| Hispanic | 115 (72%) | 102 (74%) | 217 (73%) | |
| Nativity, n (%) | .242 | |||
| US-born | 52 (32%) | 36 (26%) | 88 (30%) | |
| Foreign-born | 108 (68%) | 101 (74%) | 209 (70%) | |
| Foreign-born (n = 209) | ||||
| Place of birth, n (%) | ≤ .001 | |||
| Dominican Republic | 57 (53%) | 12 (12%) | 69 (33%) | |
| Ecuador | 2 (2%) | 25 (25%) | 27 (13%) | |
| Mexico | 7 (6%) | 19 (19%) | 26 (12%) | |
| Other birthplace | 42 (39%) | 45 (44%) | 87 (42%) | |
| Language preference, n (%) | .644 | |||
| English | 24 (22%) | 22 (22%) | 46 (22%) | |
| Spanish | 78 (72%) | 76 (75%) | 154 (74%) | |
| Other | 6 (6%) | 3 (3%) | 9 (4%) | |
| Years in US, Mean ± SD | 10.4 ± 8.0 | 11.3 ± 7.3 | 10.9 ± 7.6 | .381 |
| Pregnancy status, n (%) | .784 | |||
| Not pregnant | 130 (81%) | 113 (83%) | 243 (82%) | |
| Pregnant | 30 (19%) | 24 (17%) | 54 (18%) | |
| Breastfeeding status, n (%) | .005 | |||
| Not breastfeeding | 131 (82%) | 93 (68%) | 224 (75%) | |
| Breastfeeding | 29 (18%) | 44 (32%) | 73 (25%) | |
| Educational attainment, n (%) | .068 | |||
| Some high school or less | 25 (15%) | 36 (26%) | 61 (20%) | |
| High school diploma or equivalent | 57 (36%) | 46 (34%) | 103 (35%) | |
| More than high school | 78 (49%) | 55 (40%) | 133 (45%) | |
| Car ownership, n (%) | .312 | |||
| Did not own a reliable car | 70 (44%) | 52 (38%) | 122 (41%) | |
| Owned a reliable car | 90 (56%) | 85 (62%) | 175 (59%) | |
| Car access | ||||
| Ease of borrowing a car (if not owned; n = 122), n (%) | .014 | |||
| Very difficult | 41 (58%) | 14 (27%) | 55 (45%) | |
| Difficult | 14 (20%) | 18 (35%) | 32 (26%) | |
| Medium | 4 (6%) | 7 (13%) | 11 (9%) | |
| Easy | 9 (13%) | 10 (19%) | 19 (16%) | |
| Very easy | 2 (3%) | 3 (6%) | 5 (4%) | |
| How often can use car (if owned; n = 175), n (%) | .370 | |||
| Never | 10 (11%) | 6 (7%) | 16 (9%) | |
| Rarely | 3 (3%) | 6 (7%) | 9 (5%) | |
| Sometimes | 14 (16%) | 12 (14%) | 26 (15%) | |
| Often | 8 (9%) | 14 (17%) | 22 (13%) | |
| Always | 55 (61%) | 47 (55%) | 102 (58%) | |
| Supplement use, n (%) | .171 | |||
| Not taking supplements | 84 (53%) | 61 (45%) | 145 (49%) | |
| Taking supplements | 76 (47%) | 76 (55%) | 152 (51%) | |
| Smoking status, n (%) | .300 | |||
| Not at all | 147 (94%) | 127 (95%) | 274 (95%) | |
| Some days | 7 (4%) | 2 (2%) | 9 (3%) | |
| Every day | 3 (2%) | 4 (3%) | 7 (2%) | |
| Past 7-day exposure to secondhand smoke, n (%) | .003 | |||
| No | 127 (79%) | 124 (92%) | 251 (85%) | |
| Yes | 33 (21%) | 11 (8%) | 44 (15%) | |
| Food security statusd | .640 | |||
| Food secure | 91 (58%) | 83 (61%) | 174 (60%) | |
| Food insecure | 65 (42%) | 53 (39%) | 118 (40%) | |
| Meeting physical activity guidelines, n (%)e | .086 | |||
| No | 59 (37%) | 64 (47%) | 123 (41%) | |
| Yes | 101 (63%) | 73 (53%) | 174 (59%) | |
| BMI (n = 242)f | 29.5 ± 6.8 | 29.4 ± 6.8 | 29.9 ± 6.9 | .933 |
| CDC weight status category (n = 242), n (%)g | .806 | |||
| Underweight (< 18.5 kg/m2) | 4 (3%) | 3 (3%) | 7 (3%) | |
| Normal (18.5 to < 25 kg/m2) | 28 (22%) | 26 (23%) | 54 (22%) | |
| Overweight (25 to < 30 kg/m2) | 44 (34%) | 44 (39%) | 88 (36%) | |
| Obese (≥ 30 kg/m2) | 53 (41%) | 40 (35%) | 93 (39%) | |
| Social desirability traith | 1.41 ± 1.75 | 3.22 ± 1.51 | 2.25 ± 1.88 | ≤ .001 |
| Children in the household aged 2–5 years | .778 | |||
| None | 28 (18%) | 28 (20%) | 56 (19%) | |
| One | 119 (74%) | 97 (71%) | 216 (73%) | |
| Two | 13 (8%) | 12 (9%) | 25 (8%) | |
| Veggie Meter® score, Mean ± SDi | 265.17 ± 87.57 | 274.61 ± 105.50 | 269.54 ± 96.24 | .401 |
| Self-reported vegetable intake, Mean ± SDj | 1.46 ± 1.07 | 1.52 ± 1.07 | 1.49 ± 1.07 | .637 |
P values are for tests of between-group differences (assessed with chi-square analysis and independent samples t tests).
SD indicates standard deviation.
Includes 9 participants reporting more than one race.
Assessed with an item from the Household Food Security Survey Module (“Have you or other adults in your household worried whether your food would run out before you got money to buy more?”). As the interest was in measuring current food security status, the reference period was changed from the past 12 months to the past month.26
Assessed with a validated 2-item measure. 27 The measure queried the frequency and duration of moderate and vigorous intensity physical activity, respectively, in a typical week. Item responses were assigned point values and summed to derive a total score. Score ranges were used to classify participants as meeting physical activity guidelines (yes/no).
BMI indicates body mass index (calculated as weight in kilograms divided by height in square meters). 29 As weight and height were measured at the time of study entry, among pregnant participants, weight and height prior to pregnancy and correspondingly, pre-pregnancy BMI could not be determined. Pregnant women (n = 54) were therefore excluded from analyses of BMI.
CDC indicates Centers for Disease Control and Prevention. Standard weight status categories for adults are shown.29
Assessed with a 5-item measure of social desirability response set, the SDRS-5. Scores could range from 0 to 5. Higher scores indicated a greater tendency to respond to self-report measures in a manner consistent with expected norms.30
Vegetable intake was objectively measured using a pressure-mediated reflection spectroscopy device (the Veggie Meter®) (Longevity Link Inc., Salt Lake City, UT), to assess dermal carotenoids as a biomarker of intake. Scans were conducted in triplicate and the average of the three scans was recorded. Scores can range from zero to 800, with higher scores indicating higher dermal carotenoid levels.34
Assessed with one of two items in a brief fruit and vegetable screener developed by the National Cancer Institute (“How many cups of vegetables [including 100% vegetable juice] do you eat or drink each day?”).35 To facilitate the estimation of food portions, participants were informed that a cup was about the size of their fist.36
The following participant characteristics differed at baseline by study group despite randomization: age, social desirability trait, race, birthplace (among foreign-born participants), breastfeeding status, car access, and past 7-day exposure to secondhand smoke (Table 1). Relative to those in the control group, participants in the intervention group were younger and had a higher social desirability trait; higher percentages did not identify as any race or identified as African American, reported a birthplace of the Dominican Republic (if foreign-born), were not breastfeeding, reported it was very difficult to borrow a car (if not owned), and were recently exposed to secondhand smoke. The large between-group differences for some of the characteristics are likely due to the small number of study sites and between-site differences. Baseline measures of vegetable intake did not differ by group.
Least square means and standard errors for mid- and post-intervention measures of vegetable intake are shown in Table 2, along with 95% confidence intervals and P values for tests of between-group differences. Whereas at mid-intervention, objectively measured intake was higher among those in the control group relative to the intervention group, post-intervention, it was higher among participants in the intervention group relative to the control group. Self-reported intake did not differ by group at mid-intervention; however, post-intervention, it was higher among participants in the intervention group relative to the control group. Adjusted Cohen’s d for post-intervention differences between study groups was 0.35 for objectively measured vegetable intake and 0.34 for self-reported intake. Adjusted rates of FMNP voucher redemption were 87% in the intervention group and 28% in the control group (OR = 17.39, 95% CI [8.64, 35.02]).
Table 2.
Least square means and standard errors for measures of vegetable intake at mid- and post-intervention, by study group, among 297 urban, WIC-enrolled adults participating in a farm-to-WIC interventiona,b
| Study Group, Least Square Mean ± Standard Error |
||||
|---|---|---|---|---|
| Intake Measure | Interventionc | Controld | Mean difference (95% CI)e | P value |
| Objectively measured intake (Veggie Meter® scores)f | ||||
| Mid-intervention | 227.11 ± 9.91 | 269.98 ± 10.06 | −42.87 (−65.25, −20.49) | .001 |
| Post-intervention | 236.01 ± 9.77 | 212.10 ± 9.79 | 23.91 (2.21, 45.62) | .031 |
| Self-reported intake (cups/day of vegetables consumed)g | ||||
| Mid-intervention | 1.78 ± 0.11 | 1.84 ± 0.12 | −0.06 (−0.33, 0.21) | .662 |
| Post-intervention | 1.83 ± 0.11 | 1.55 ± 0.12 | 0.28 (0.00, 0.55) | .047 |
WIC indicates Special Supplemental Nutrition Program for Women, Infants, and Children.
Data were analyzed with linear mixed-effects models. Covariates included baseline measures of vegetable intake, age, race, breastfeeding status, and exposure to secondhand smoke; supplement use (in the analysis of objectively measured intake), and social desirability trait (in the analysis of self-reported intake).
Sample sizes for longitudinal analyses were 137 (Veggie Meter scores) and 143 (self-reported intake).
Sample sizes for longitudinal analyses were 124 (Veggie Meter scores) and 130 (self-reported intake).
CI indicates confidence interval.
Vegetable intake was objectively measured using a pressure-mediated reflection spectroscopy device (the Veggie Meter®) (Longevity Link Inc., Salt Lake City, UT), to assess dermal carotenoids as a biomarker of intake. Scans were conducted in triplicate and the average of the three scans was recorded. Scores can range from zero to 800, with higher scores indicating higher dermal carotenoid levels.34
Assessed with one of two items in a brief fruit and vegetable screener developed by the National Cancer Institute (“How many cups of vegetables [including 100% vegetable juice] do you eat or drink each day?”).35 To facilitate the estimation of food portions, participants were informed that a cup was about the size of their fist.36
In exploratory analyses of the moderating role of FMNP voucher redemption, adjusted Cohen’s d for between-groups differences in objectively measured vegetable intake was 0.31 among participants who redeemed FMNP vouchers and 0.09 among those who did not. For self-reported intake, the corresponding values were 0.34 and 0.07, respectively.
DISCUSSION
In the present study, objectively measured vegetable intake was higher among participants in the control group relative to the intervention group at mid-intervention; self-reported intake did not differ by group. Post-intervention, objective and self-reported vegetable intake were higher among participants in the intervention as compared to the control group. Receipt of the intervention was associated with FMNP voucher redemption. In exploratory analyses, the relationship between the intervention and vegetable intake was moderated by FMNP voucher redemption.
The between-group differences in vegetable intake were similar in magnitude to differences reported elsewhere. In a synthesis of reviews and meta-analyses of interventions to promote fruit and vegetable intake in adults, between-group differences were meaningful (defined as ≥ 0.30).41 In a meta-analytic review of electronic and telephone-based interventions to promote vegetable intake, the differences ranged from 0.11 to 0.40.42 Comparable data for interventions to promote FMNP voucher redemption are lacking, owing to the small number of such programs to date. Among programs that have been evaluated, no or small between-group differences in voucher redemption (i.e., ≤ 8%) are found.8,16,43 In this study, the between-group difference in voucher redemption was 59%; the corresponding effect size of 17.39 was large, suggesting that the intervention has the potential to exert a substantial impact on FMNP voucher redemption.
The finding that at mid-intervention, objectively measured vegetable intake was higher among those in the control group relative to the intervention group was unexpected. Possibly, the difference was an artifact of skin carotenoid response to changes in vegetable intake. The amount of time it takes for a substantial and sustained increase in intake to manifest in a change in dermal carotenoids is unclear as research in this area is limited and findings are mixed. For example, Mayne and colleagues reported that skin carotenoid concentrations reflect intake over at least the past two months, whereas Jahns et al. reported that carotenoid concentrations respond quickly to changes in intake, i.e., within two weeks.38,44 If, for example, the scores reflected a longer (3-month) lag, between-group differences found at mid-intervention would in reality indicate that at baseline, vegetable intake was higher among those in the control as compared to intervention group and that by mid-intervention, the trend reversed, possibly due to intervention. If, however, the lag was shorter (up to one month), the higher intake found among those in the control as compared to the intervention group at mid-intervention may be explained by the ongoing nature of intervention, with higher intake expected among participants in the intervention as compared to the control group after the intervention concluded as was found. Further research is needed to clarify the lag between intake changes and skin carotenoid response. In the interim, program planners designing studies of this type might consider adding a 3-month follow-up data collection point to account for a potentially longer-than-expected lag.
Analyses also revealed that the relationship between the intervention and vegetable intake was stronger among participants who redeemed FMNP vouchers relative to those who did not. In previous work, having previously redeemed FMNP vouchers was associated with farmers’ market use; positive associations between farmers’ market use and vegetable intake also were found.45,46 Those redeeming vouchers may have purchased vegetables more often, possibly explaining the stronger relationship in this group. Alternatively, individuals who were most responsive to the intervention may have increased both their FMNP voucher use and vegetable intake (independent of FMNP purchases) to a greater extent than participants who were less responsive to the program.
Limitations and Strengths
The self-selected sample limits the generalizability of findings. Program outcomes were assessed immediately after intervention. Replication studies with longer follow-up periods are needed to determine whether post-intervention between-group differences in vegetable intake are sustained over time. As some fruits are high in carotenoids, Veggie Meter scores may have reflected fruit rather than vegetable intake. This was considered unlikely however in the light of the intervention focus on the promotion of vegetable intake and the consistency of post-intervention findings, i.e., higher objectively measured and self-reported vegetable intake among those in the intervention as compared to the control group and, assuming the lag between intake changes and changes in dermal carotenoids was relatively short, the similar magnitude of between-group differences in intake. Although the focus of intervention was vegetable consumption, the FMNP provides vouchers for fruit and vegetable purchases; as such, it was not always possible to separate fruits and vegetables and there was the possibility that participants purchased both fruits and vegetables with the vouchers. The use of a self-report measure of vegetable intake was a weakness of the study in light of the degree of overall bias in data collected via self-report and the potential for differential response bias between study groups.47 In future studies of this type, 24-hour recalls are recommended over other self-report methods, i.e., food frequency questionnaires and brief screeners, including single-item measures as used in this study.47 The small number of clusters and the single site in the intervention group limit the extent to which findings can be causally attributed to the intervention despite the randomized design. Moreover, the single intervention site did not allow us to reliably control for clustering. In light of these limitations, findings should be interpreted as suggestive rather than definitive.
Despite these limitations, the research is responsive to the call for programs to address individual and broader systems-level influences on vegetable intake,4 grounded in preliminary work highlighting the feasibility and acceptability of a farm-to-WIC intervention,16 and builds upon research demonstrating the effectiveness of multicomponent theory-based interventions, programs providing face-to-face nutrition education,2,48 and those combining nutrition education with the introduction of farmers’ markets in community-based settings.10 The randomized design and objective measures of vegetable intake and FMNP voucher redemption are study strengths. The relatively new device for measuring dermal carotenoids is a novel feature of the study.
CONCLUSIONS
This study found positive and meaningful associations between a novel, theory-driven, farm-to-WIC intervention, vegetable intake, and the redemption of FMNP vouchers provided by WIC for fruit and vegetable purchases at farmers’ markets. These findings suggest that the program shows promise of being successful and is therefore appropriate for efficacy testing.12 A future large-scale trial with more sites is planned to rigorously evaluate the intervention.
Research Question
Does an intervention for WIC-enrolled adults incorporating such elements as an onsite farmers’ market, field trips to an area farmers’ market, and recipe demonstrations and tastings show promise for promoting vegetable purchases and consumption?
Key Findings
Designed to increase the redemption of vouchers for produce purchases and vegetable-related knowledge, attitudes, and behaviors, the intervention was piloted in 3 WIC agency sites (one intervention and two control sites) with 297 urban, primarily Hispanic adults. Post-intervention differences were found in primary outcomes of vegetable intake and voucher redemption favoring participants who received the intervention relative to those who did not.
Acknowledgments
Funding disclosure: Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Number R21CA230476. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The study is registered at www.clinicaltrials.gov (NCT04038385).
Footnotes
Conflict of interest disclosure: No conflicts of interest were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jennifer Di Noia, Department of Sociology, William Paterson University, 300 Pompton Road, Wayne, NJ, 07470.
Dorothy Monica, Saint Joseph’s WIC Program, 800 Main Street, Paterson, NJ, 07503.
Alla Sikorskii, Department of Psychiatry, Michigan State University, 909 Fee Road, 321 West Fee Hall, East Lansing, MI, 48824.
Julia Nelson, Department of Sociology, William Paterson University, 300 Pompton Road, Wayne, NJ, 07470.
References
- 1.Slavin JL, Lloyd B. Health benefits of fruits and vegetables. Adv Nutr. 2012;3(4):506–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Appleton KM, Hemingway A, Saulais L, Dinnella C, Monteleone E, Depezay L, et al. Increasing vegetable intakes: rationale and systematic review of published interventions. Eur J Nutr.2016;55(3):869–896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. State Indicator Report on Fruits and Vegetables, 2018. Available at: https://www.cdc.gov/nutrition/downloads/fruits-vegetables/2018/2018-fruit-vegetable-report-508.pdf.Accessed December 16, 2020.
- 4.Robinson T. Applying the socio-ecological model to improving fruit and vegetable intake among low-income African Americans. J Community Health. 2008;33(6):395–406. [DOI] [PubMed] [Google Scholar]
- 5.US Department of Agriculture, Food and Nutrition Service. About WIC: WIC at a Glance. Available at: https://www.fns.usda.gov/wic/about-wic-wic-glance.Accessed April 21, 2020.
- 6.US Department of Agriculture. WIC Farmers’ Market Nutrition Program. Available at: https://fns-prod.azureedge.net/sites/default/files/fmnp/WICFMNPFactSheet.pdf.Accessed April 21, 2020.
- 7.Kropf ML, Holben DH, Holcomb JP, Anderson H. Food security status and produce intake and behavior of Supplemental Nutrition Program for Women, Infants, and Children and Farmers’ Market Nutrition Program participants. J Am Diet Assoc. 2007;107:1903–1908. [DOI] [PubMed] [Google Scholar]
- 8.Anderson JV, Bybee DI, Brown RM, McLean DF, Garcia EM, Breer ML, et al. 5 a day fruit and vegetable intervention improves consumption in a low-income population. J Am Diet Assoc. 2001;101:195–202. [DOI] [PubMed] [Google Scholar]
- 9.US Department of Agriculture, Food and Nutrition Service. WIC FMNP FY 2018 FNS-203 Report. Alexandria, VA: Food and Nutrition Service; 2020. [Google Scholar]
- 10.Harris D, Lott M, Lakins V, Bowden B, Kimmons J. Farm to institution: creating access to healthy local and regional foods. Adv Nutr. 2012;3(3):343–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hosler AS, Rajulu DT, Rosani AE, Frederick BL. Assessing retail fruit and vegetable availability in rural and urban underserved communities. Prev Chronic Dis. 2008;5(4). [PMC free article] [PubMed] [Google Scholar]
- 12.Bowen DJ, Kreuter M, Spring B, Cofta-Woerpel L, Linnan L, Weiner D, et al. How we design feasibility studies. Am J Prev Med. 2009;36(5):452–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Campbell MK, Piaggio G, Elbourne DR, Altman DG. Consort 2010 statement: extension to cluster randomised trials. BMJ. 2012;345:e5661. [DOI] [PubMed] [Google Scholar]
- 14.US Department of Education, Institute of Education Sciences, What Works Clearinghouse, WWC Standards Brief. Confounding Factors. Available at https://ies.ed.gov/ncee/wwc/Docs/referenceresources/wwc_brief_confounds_101117.pdf.Accessed November 13, 2020.
- 15.McDonnell L, Morris MN, Holland J. WIC participants’ perceived behavioral control, attitudes toward, and factors influencing behavioral intentions to redeeming cash-value vouchers at certified farmers markets. Calif J Health Promot. 2014;12(2):22–31. [Google Scholar]
- 16.Di Noia J, Monica D, Sikorskii A, Gonzalez K, Abuhadba L. Feasibility of a farm-to-WIC intervention. Public Health Nutr. 2019;22(18):3405–3415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Skov LR, Lourenco S, Hansen GL, Mikkelsen BE, Schofield C. Choice architecture as a means to change eating behaviour in self-service settings a systematic review. Obes Rev. 2013;14(3):187–196. [DOI] [PubMed] [Google Scholar]
- 18.Kahn-Marshall JL, Gallant MP. Making healthy behaviors the easy choice for employees: a review of the literature on environmental and policy changes in worksite health promotion. Health Educ Behav. 2012;39(6):752–776. [DOI] [PubMed] [Google Scholar]
- 19.Escaron AL, Meinen AM, Nitzke SA, Martinez-Donate AP. Supermarket and grocery store-based interventions to promote healthful food choices and eating practices: a systematic review. Prev Chronic Dis. 2013;10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vanderplasschen W, De Maeyer J. Theory-driven interventions. In: Michalos AC, ed. Encyclopedia of Quality of Life and Well-Being Research. Springer; Netherlands; 2014: 6629–6632. [Google Scholar]
- 21.Stallings TL, Gazmararian JA, Goodman M, Kleinbaum D. The Georgia WIC Farmers’ Market Nutrition Program’s influence on fruit and vegetable intake and nutrition knowledge and competencies among urban African American women and children. J Hunger Environ Nutr. 2016;11(1):86–101. [Google Scholar]
- 22.Ball L, McCauley A, Paul T, Gruber K, Haldeman L, Dharod J. Evaluating the implementation of a farmers’ market targeting WIC FMNP participants. Health Promot Pract. 2018;19(6):946–956. [DOI] [PubMed] [Google Scholar]
- 23.Kreuter MW, Lukwago SN, Bucholtz RD, Clark EM, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav. 2003;30:133–146. [DOI] [PubMed] [Google Scholar]
- 24.Elder JP, Ayala GX, Parra-Medina D, Talavera GA. Health communication in the Latino community: issues and approaches. Annu Rev Public Health. 2009;30:2227–2251. [DOI] [PubMed] [Google Scholar]
- 25.Di Noia J, Furst G, Park K, Byrd-Bredbenner C. Designing culturally sensitive dietary interventions for African Americans: review and recommendations. Nut Rev. 2013;71(4):224–238. [DOI] [PubMed] [Google Scholar]
- 26.US Department of Agriculture, Economic Research Service. U.S. Household Food Security Survey Module. Available at: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/survey-tools/.Accessed September12, 2020.
- 27.Marshall AL, Smith BJ, Bauman AE, Kaur S. Reliability and validity of a brief physical activity assessment for use by family doctors. Br J Sports Med. 2005;39:294–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention. National Health and Nutrition Examination Anthropometry Procedures Manual. Available at: https://wwwn.cdc.gov/nchs/data/nhanes/2017-2018/manuals/2017_Anthropometry_Procedures_Manual.pdf.Accessed April 21, 2020.
- 29.Centers for Disease Control and Prevention. About Adult BMI. Available at: https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html.Accessed April 21, 2020.
- 30.Hays RD, Hayashi T, Stewart AL. A five-item measure of socially desirable response set. Educ Psychol Meas. 1989;49(3):629–636. [Google Scholar]
- 31.Di Noia J, Weber Cullen K, Monica D. Social desirability trait is associated with self-reported vegetable intake among women enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children. J Acad Nutr Diet. 2016;116(12):1942–1950. [DOI] [PubMed] [Google Scholar]
- 32.Jahns L, Johnson LK, Conrad Z, et al. Concurrent validity of skin carotenoid status as a concentration biomarker of vegetable and fruit intake compared to multiple 24-h recalls and plasma carotenoid concentrations across one year: a cohort study. Nutr J. 2019;18(1):78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Radtke MD, Pitts SJ, Jahns L, et al. Criterion-related validity of spectroscopy-based skin carotenoid measurements as a proxy for fruit and vegetable intake: a systematic review. Adv Nutr. 2020;11(5):1282–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Scherr RE, Laugero KD, Graham DJ, et al. Innovative techniques for evaluating behavioral nutrition interventions. Adv Nutr. 2017;8(1):113–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yaroch AL, Tooze J, Thompson FE, Blanck HM, Thompson OM, Colon-Ramos O, et al. Evaluation of three short dietary instruments to assess fruit and vegetable intake: the national cancer Institute’s food attitudes and behaviors (FAB) survey. J Acad Nutr Diet. 2012;112(10):1570–1577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ogunbode A, Owolabi M, Ogunbode O, Ogunniyi A. What’s in your hands? A systematic review of dietary assessment methods and estimation of food sizes in a Primary Care Clinic J Med Trop. 2018;20(2):93–103. [Google Scholar]
- 37.US Department of Education, Institute of Education Sciences, What Works Clearinghouse. Assessing Attrition Bias. Available at: https://ies.ed.gov/ncee/wwc/Document/243.Accessed September 12,2020.
- 38.Mayne ST, Cartmel B, Scarmo S, Jahns L, Ermakov IV, Gellermann W. Resonance Raman spectroscopic evaluation of skin carotenoids as a biomarker of carotenoid status for human studies. Arch Biochem Biophys. 2013;539(2):163–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rosenthal JA. Qualitative descriptors of strength of association and effect size. J Soc Serv Res. 1996;21(4):37–59. [Google Scholar]
- 40.SAS [computer program]. Version 9.4. Cary, NC: SAS Institute Inc; 2018. [Google Scholar]
- 41.Sweet SN, Fortier MS. Improving physical activity and dietary behaviours with single or multiple health behaviour interventions? A synthesis of meta-analyses and reviews. Int J Environ Res Public Health. 2010;7(4):1720–1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nour M, Chen J, Allman-Farinelli M. Efficacy and external validity of electronic and mobile phone-based interventions promoting vegetable intake in young adults: systematic review and meta-analysis. J Med Internet Res. 2016;18(4):e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Seidel M, Brink L, Hamilton M, Gordon L. Increasing WIC Farmers’ Market Nutrition Program redemption rates: results and policy recommendations. Prog Community Health Partnersh. 2018;12(4):431–439. [DOI] [PubMed] [Google Scholar]
- 44.Jahns L, Johnson LK, Mayne ST, Cartmel B, Picklo MJ Sr, Ermakov IV, et al. Skin and plasma carotenoid response to a provided intervention diet high in vegetables and fruit: uptake and depletion kinetics. Am J Clin Nutr. 2014;100(3):930–937. [DOI] [PubMed] [Google Scholar]
- 45.Racine EF, Vaughn AS, Laditka SB. Farmers’ market use among African-American women participating in the Special Supplemental Nutrition Program for Women, Infants, and Children. J Am Diet Assoc. 2010;110:441–446. [DOI] [PubMed] [Google Scholar]
- 46.Grin BM, Gayle TL, Saravia DC, Sanders LM. Use of farmers markets by mothers of WIC recipients, Miami-Dade County, Florida, 2011. Prev Chronic Dis. 2013;10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.National Institutes of Health, National Cancer Institute. Dietary Assessment Primer. Available at: https://dietassessmentprimer.cancer.gov/approach/intervention.html.Accessed September 12, 2020.
- 48.Pomerleau J, Lock K, Knai C, McKee M. Interventions designed to increase adult fruit and vegetable intake can be effective: a systematic review of the literature. J Nutr. 2005;135(10):2486–2495. [DOI] [PubMed] [Google Scholar]