Abstract
Racial/ethnic disparities in coronavirus disease 2019 (COVID-19) hospitalization and mortality have emerged in the United States, but less is known about whether similar differences exist in testing, and how this changed as COVID-19 knowledge and policies evolved. We examined racial/ethnic variations in COVID-19 testing over time among veterans who sought care for COVID-19 symptoms or exposure. In the national population of all Veterans who sought Veterans Health Administration (VHA) care for COVID-19 symptoms or exposure (n = 913,806), we conducted multivariate logistic regressions to explore race/ethnicity-by-time period differences in testing from 3/1/2020–11/25/2020, and calculated predicted probabilities by race/ethnicity and time period.
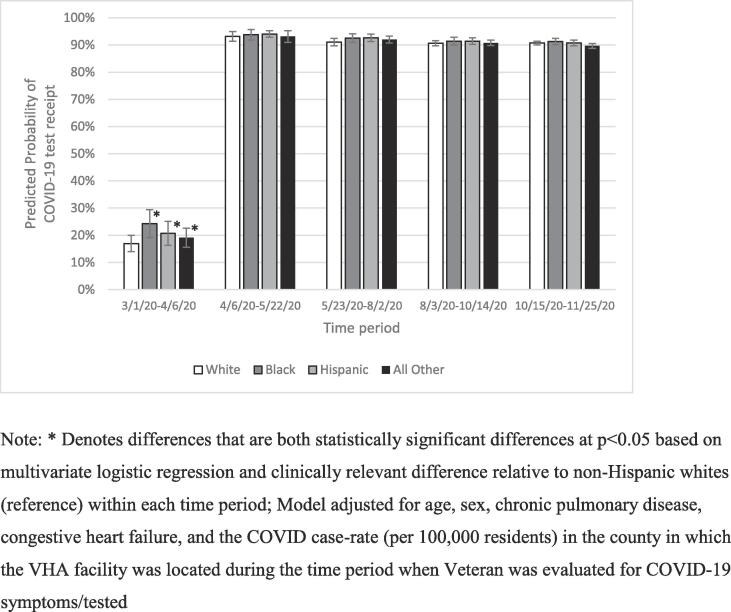
Early in the pandemic (3/1/2020–4/6/2020) when testing was limited and there was less awareness of racial/ethnic disparities, non-Hispanic Black, Hispanic, and other non-White racial/ethnic minority Veterans who sought care from VHA for COVID-19 symptoms or exposure were more likely than non-Hispanic White Veterans to receive a COVID-19 test (p < 0.05). In subsequent time periods (4/7/2020–11/25/2020), testing was similar among all racial/ethnic groups.
Among Veterans with COVID-19 symptoms or exposure, non-Hispanic Black and Hispanic patients were just as likely, and in some cases, more likely, to receive a COVID-19 test versus non-Hispanic White patients. The United States faced testing shortages at the start of the third wave of the pandemic; additional shortages are likely to emerge as the pandemic continues to peak and ebb. It is important to ensure that racial/ethnic minorities and others at greater risk for infection continue to have access to COVID-19 testing with each of these peaks.
Keywords: COVID-19 screening, Racial/ethnic disparities, Veterans
1. Introduction:
Widespread testing is crucial for COVID-19 prevention, mitigating community spread and facilitating early initiation of treatment (Pulia et al., Aug 2020). Although racial/ethnic disparities in COVID-19 positivity and severe COVID-19 outcomes (e.g., mortality) have emerged (Mackey et al., 2021), less is known about racial/ethnic differences in COVID-19 testing. Testing differences, particularly earlier in the pandemic when testing kits were limited and prioritized for those who recently traveled, could have potentially contributed to COVID-19 racial/ethnic disparities (Dodds and Fakoya, 2020).
Two studies, conducted early in the pandemic, found racial/ethnic testing disparities within a regional healthcare system (Azar et al., 2020) and in non-White New York City neighborhoods (Lieberman-Cribbin et al., 2020). Several reasons may contribute to racial/ethnic testing disparities. First, segregation has resulted in fewer healthcare resources in communities of color (Io, 2003:780.). There have been reports of a dearth of COVID-testing sites in predominately minority communities (Lieberman-Cribbin et al., 2020, Singh, 2020). Second, healthcare providers may take racial/ethnic minority patients’ health concerns less seriously than non-Hispanic White (hereafter, “White”) patients’ concerns, resulting in underdiagnoses and undertreatment of racial/ethnic minority patients (Hoffman et al., 2016). For example, the news media has reported instances where non-Hispanic Black (hereafter, “Black”) patients were denied COVID-19 testing despite exhibiting symptoms (Elidon and Burch, 2020). Although greater awareness of COVID-19 disparities may diminish the effects of implicit bias, entrenched segregation continues to disadvantage communities of color. Third, healthcare access barriers, such as being uninsured, may contribute to racial/ethnic disparities in COVID-19 care (Price-Haywood et al., 2020).
Our objective was to examine racial/ethnic differences in testing over time among Veterans who sought care from the Veterans Health Administration (VHA) for COVID-19 symptoms or exposure. We hypothesized that racial/ethnic minority Veterans would be less likely to receive a COVID-19 test compared to non-Hispanic White Veterans, with greater disparities earlier in the pandemic due to limited awareness of COVID-19 racial/ethnic disparities and restrictions on testing. This analysis built upon existing analyses (Azar et al., 2020, Lieberman-Cribbin et al., 2020) by using a national, geographically-diverse setting to explore temporal changes over a longer study period. The pandemic has changed significantly since initial studies have explored racial/ethnic disparities in COVID-19 testing: (Azar et al., 2020, Lieberman-Cribbin et al., 2020) new hot-spots have emerged, testing capacity has increased, and there is greater acknowledgement of COVID-19 racial/ethnic disparities. Testing shortages may emerge with subsequent surges in COVID-19 infections (American Society for Microbiology, 2020). Our findings can also inform prioritization of testing resources in future pandemics when testing may initially be limited, and healthcare (e.g., provider biases) and societal factors (e.g., testing locations) may pose barriers to testing among racial/ethnic minorities.
2. Methods
2.1. Data and Sample
Our sample included Veterans who sought care for COVID-19 exposure, symptoms, or testing from any VHA facility between 3/1/2020 and 11/25/2020. Data came from VHA’s national database of VHA-users evaluated for respiratory illness or COVID-19 exposure, VHA’s administrative records, and USAFacts, which compiles data on COVID-19 cases from the Centers for Disease Control and Prevention (CDC), and state- and local-level public health agencies (USA Facts, 2020). Individuals were identified as undergoing evaluation for respiratory illness based on ICD-10 codes, Health Factors, and provider notes (appendix).
2.2. Measures
Our dependent variable was receipt of a COVID-19 test. Our main independent variable was a categorical indictor of Veterans’ race/ethnicity: White (reference), Black, Hispanic, and all other racial/ethnic groups (American Indian/Alaskan Native, Asian, Native Hawaiian/other Pacific Islander, multi-race, and those with unknown or missing race/ethnicity).
We created a time period indicator based on the date of the visit for COVID-19 symptoms or COVID-19 testing. If Veterans were evaluated multiple times for COVID-19 symptoms or received multiple tests, we used the date of their first visit. We identified five key time periods based on key dates of COVID-19 pandemic developments (Staff, 2020, Neilson 0000):
-
•
3/1/2020–4/6/2020: limited awareness of COVID-19 racial/ethnic disparities; testing restrictions;
-
•
4/7/2020–5/22/2020: initial reports emerged during the week of 4/7/2020 about COVID-19 racial/ethnic disparities leading to increase awareness of COVID-19 disparities; states, counties, and cities implemented shelter-in-place orders to help flatten the curve; by 4/7/2020, ~95% of the U.S. population were under “lockdown;”
-
•
5/23/2020–8/2/2020: COVID-19 cases increased as states loosened shelter-in-place orders; Memorial Day weekend ushered in summertime travel;
-
•
8/3/2020–10/14/2020: on 8/3/2020, Dr. Deborah Brix (White House Coronavirus Task Force coordinator) stated that the U.S. had entered “a new phase” where the pandemic was “extraordinarily widespread” and no longer limited to urban areas;
-
•
10/15/2020–11/25/2020: on 10/15, the U.S. reached the milestone of 60,000 new cases, beginning another wave of the pandemic that continued past November.
Control variables include age (<60 years, 60–64 years, 65–69 years, 70–74 years, 75–79 years, and ≥80 years), gender, diagnoses of chronic pulmonary disease and congestive heart failure between 3/1/18–2/29/20 from ICD to 10 diagnosis codes, and the COVID-19 case rate in the county where the VHA facility was located during the time period of the COVID-19 symptom/test visit. Because chronic pulmonary disease and congestive heart failure can have symptoms similar to COVID-19 (e.g., shortness of breath, coughing), these prior diagnoses may affect how providers treat patients with COVID-19 symptoms. County-level COVID-19 case rates may affect provider behavior and facility testing policies.
2.3. Statistical analysis
We calculated descriptive statistics for the sample, stratified by COVID-19 testing status, and the proportion of tests conducted during each time period among Veterans seeking care for COVID-19 symptoms or exposure. We fit logistic regression models with an interaction term between race/ethnicity and time period, adjusting for age, gender, diagnosis of chronic pulmonary disease or congestive heart failure, and the case-rate in the VHA facility county. Models clustered standard errors at the VHA facility level. We calculated predicted probabilities for each racial/ethnic group by time period using the margins postestimation command. We further calculated linear combinations to determine racial/ethnic differences in COVID-19 testing relative to Whites within each time period. We used a two-tail p < 0.05 to denote statistical significance. Predicted probability differences between racial/ethnic minority groups and Whites (reference group) were considered clinically relevant if differences were ≥10% of the predicted probability for Whites. Analyses were conducted in Stata version 15.1 (College Station, TX). [Institution name blinded for peer-review] Institutional Review Board determined this to be a non-research activity.
3. Results
Between 3/1/2020–11/25/2020, in our sample of 913,806 Veterans seeking care for COVID-19 exposure or symptoms, 83% received a COVID-19 test. Those receiving a test were more likely to be Black, male, have a congestive heart failure diagnosis, and have received care from VHA facilities located in counties with a higher COVID-19 case rate (Table 1). From 3/1/2020–4/6/2020, only 18% of Veterans with COVID-19 exposure or symptoms received a COVID-19 test, but in all subsequent time periods, 90% or more received a COVID-19 test.
Table 1.
Characteristics for Veterans with COVID-19 symptoms or exposures from 3/1/2020 to 11/25/2020 and testing by time period.
| Tested (n = 760,426) | Not Tested (n = 153,380) | Total (Dodds and Fakoya, 2020) | p-value | |
|---|---|---|---|---|
| Race/ethnicity, % | ||||
| White | 61.4 | 63.6 | 61.7 | <0.001 |
| Black | 22.4 | 20.7 | 22.1 | |
| Hispanic | 8.5 | 8.3 | 8.4 | |
| All other groups (Pulia et al., Aug 2020) | 7.8 | 7.5 | 7.7 | |
| Age, mean years (SD) | 61.2 (15.7) | 60.0 (15.8) | 61.0 (15.7) | 0.048 |
| Gender, % | ||||
| Male | 89.0 | 86.9 | 88.6 | <0.001 |
| Female | 11.0 | 13.1 | 11.4 | |
| Chronic pulmonary disease, % | 24.6 | 26.6 | 25.0 | 0.001 |
| Congestive heart failure, % | 12.1 | 10.2 | 11.7 | <0.001 |
| COVID-19 case-rate (per 100,000 population) in VHA facility county, mean (SD) | 1078.6.7 (701.9) | 535.4 (735.9) | 987.5 (736.2) | <0.001 |
| Time Period(Mackey et al., 2021) | ||||
| 3/1/2020–4/6/2020 (n = 102,236) |
19.6 | 80.5 | 11.2 | <0.001 |
| 4/7/2020–5/22/2020 (n = 85,316) |
93.5 | 6.5 | 9.3 | |
| 5/23/2020–8/2/2020 (n = 183,318) |
91.6 | 8.4 | 20.1 | |
| 8/3/2020–10/14/2020 (n = 258,655) |
90.8 | 9.2 | 31.1 | |
| 10/15/2020–11/25/2020 (n = 258,655) |
90.7 | 9.4 | 28.3 | |
Notes: 1. Includes American Indian/Alaskan Native, Asian, Native Hawaiian/Other Pacific Islander, multi-race, and unknown/missing/declined race Veterans; 2. Tested and Not Tested columns present row percentages indicating the % of Veterans who did or did not receive a test during each time period; 3. Total column represents column percentages of Veterans with COVID-19 symptoms or exposure (i.e., Veterans who should have received a COVID-19 test) for each variable.
Statistical differences for mean age determined with an independent t-test; statistical differences between proportions for all other variables determined with chi squared tests.
At the beginning of the pandemic, between 3/1/2020–4/6/2020, the predicted probability of getting a COVID-19 test for White Veterans (reference group) was 17.0% (95% confidence interval [CI]: 14.0–19.9%). We considered predicted probability differences of ≥1.7% to be clinically relevant (10% of the reference group’s predicted probability [17%]), i.e., predicted probabilities outside of the range of 15.3% to 18.5%. Black (predicted probability: 24.3% 95% CI: 19.2%–29.5%), Hispanic (predicted probability:20.7%, 95%CI: 16.3%-25.1%), and Veterans of other race/ethnicities (predicted probability: 19.1%, 95%CI: 15.6–22.6%) were more likely to receive a COVID-19 test than White Veterans after adjusting for Veterans’ demographic and health characteristics and the county-level COVID-19 case rate (Fig. 1).
Fig. 1.
Predicted probability of receiving a COVID-19 test by race/ethnicity and time period, from 3/1/2020–11/25/2020. Note: * Denotes differences that are both statistically significant differences at p < 0.05 based on multivariate logistic regression and clinically relevant difference relative to non-Hispanic whites (reference) within each time period; Model adjusted for age, sex, chronic pulmonary disease, congestive heart failure, and the COVID case-rate (per 100,000 residents) in the county in which the VHA facility was located during the time period when Veteran was evaluated for COVID-19 symptoms/tested.
In subsequent time periods, across all racial/ethnic groups, more than 90% of our sample received a COVID-19 test. During the summer period (5/23/2020–8/2/2020), Black Veterans, Hispanic Veterans, and Veterans of other race/ethnicities had statistically significantly higher odds of receiving a COVID-19 test than White Veterans, but during the fall (10/15/2020–11/25/2020), Veterans of other race/ethnicities had statistically significant lower odds of receiving a COVID-19 test; however, none of these differences were clinically relevant. From 5/23/2020–8/2/2020, differences in the predicted probability of COVID-19 test receipt for racial/ethnic minority groups ranged from 0.95% (all other racial/ethnic minority groups) to 1.6% (Hispanic) greater predicted probability of COVID-19 test receipt compared to White Veterans; from 10/15/2020–11/25/2020, individuals in the all other racial/ethnic minority group had a 0.14% lower predicted probability of test receipt than White Veterans.
4. Discussion
We found that Black and Hispanic Veterans were equally, or more likely, to receive a COVID-19 test as White Veterans who sought COVID-19-related care. Black and Hispanic Veterans with COVID-19 symptoms or exposure were more likely than White Veterans to receive a COVID-19 test at the beginning of the pandemic. By early April 2020, most Veterans presenting for evaluation of non-specific or influenza-like respiratory illness received a COVID-19 test, with small differences in testing by race/ethnicity.
Despite COVID-19′s disproportionate impact on Black and Hispanic patients (Mackey et al., 2021), we did not find evidence of testing disparities among racial/ethnic minorities in our sample. This differs from regional studies that found lower testing among racial/ethnic minority patients and communities (Azar et al., 2020, Lieberman-Cribbin et al., 2020). Testing may be more prevalent among racial/ethnic minority individuals in our sample, given VHA’s efforts to improve access and reduce health inequities, including through rigorous data collection, monitoring of quality and disparities, social risk factor screening, and communication about health disparities (Wong et al., 2019, Moy, 2020). Our findings are partially consistent with a study of testing rates in VHA enrollees, that found higher population testing rates among Black and Hispanic Veterans versus White Veterans (Rentsch et al., 2020). While that study included individuals who previously used VHA care regardless of their current COVID-19 test-seeking behavior, our sample focused on patients who should have all received COVID-19 testing if shortages or implicit biases in the healthcare system did not exist.
Provider biases have led to underdiagnoses and undertreatment of Black and Hispanic patients with other conditions (Hoffman et al., 2016), and reports of challenges in receiving COVID-19 testing (Elidon and Burch, 2020). However, our findings suggest that within VHA, implicit biases within the healthcare system were unlikely to negatively affect receipt of testing among racial/ethnic minority Veterans who presented with COVID-19 symptoms or exposure. In fact, these patients were more likely to receive testing. However, it is possible that racial/ethnic minority patients presented later and with more severe symptoms than their White counterparts, thus warranting higher rates of COVID-19 testing.
We were encouraged to find that COVID-19 testing was high across all racial/ethnic groups as the pandemic progressed. In fact, widespread testing is one of the most effective interventions in controlling COVID-19 transmission – and may be more effective than other policies, such as shelter-in-place orders (Rannan-Eliya et al., 2021). Ensuring that racial/ethnic minority individuals can receive COVID-19 testing can potentially play an important role in mitigating transmission, particularly because shelter-in-place orders may have limited influence since racial/ethnic minority individuals are more likely to be essential workers. However, our sample includes only those who sought care from VHA. It is possible that racial/ethnic disparities may exist in the ability to access testing at VHA among those who were infected or at high-risk for infection. For example, racial/ethnic minority individuals may experience greater transportation challenges, which could delay testing.
We also found Black, Hispanic, and all other racial/ethnic minority groups were statistically significantly more likely to receive a COVID-19 test from 5/23/2020–8/2/2020 when COVID-19 cases increased as states loosened stay-at-home orders, and that all other racial/ethnic minority groups were less likely to receive a COVID-19 test from 10/15–2020-11/25/2020 as cases increased. However, these differences are unlikely to be clinically meaningfully, as predicted probability differences were small (<1.5%), and most Veterans with COVID-19 symptoms or exposure received a test.
4.1. Limitation
VHA-users differ from the general U.S. population in ways that may influence COVID-19 test-seeking (e.g., older and sicker (Agha et al., 2000)). However, this study’s strengths include use of a national sample, which reduces potential for regional differences in testing, and several months of data that allowed us to consider temporal trends as social distancing policies, knowledge of COVID-19, and regional hotspots changed.
5. Conclusion
Healthcare systems and health departments may have to consider implementing regulations that prioritize who receives a test when cases increase during the current COVID-19 pandemic (Abbott and Lovett, 2020) and in future pandemics. Widespread testing is a crucial way to prevent transmission (Pulia et al., Aug 2020, Rannan-Eliya et al., 2021) and may be an important tool to prevent transmission in racial/ethnic minority communities, particularly since Black and Hispanic individuals may be at higher risk for exposure. As VHA and other healthcare systems address periodic testing shortages with assessments about which patients to test, our study suggests that decisions should be monitored for concordance with COVID-19 population risk. Future pandemics will likely also have initial and periodic shortages of test kits; it will be crucial to ensure that racial/ethnic minorities who present with symptoms are able to receive tests.
Funding
This work was supported by the VA Office of Health Equity (OHE) and Quality Enhancement Research Initiative (QUERI) through grant #PEC-15–239 to the OHE/QUERI National Partnered Evaluation Center, and by VA HSR&D (grant #SDR-20–402). The views expressed within are those of the authors and do not necessarily represent those of the Department of Veterans Affairs or the United States Government.
CRediT authorship contribution statement
Michelle S. Wong: Conceptualization, Writing – original draft, Writing - review & editing. Anita H. Yuan: Data curation, Writing - review & editing. Taona P. Haderlein: Data curation, Writing - review & editing. Kenneth T. Jones: Writing - review & editing. Donna L. Washington: Conceptualization, Writing - review & editing, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Pulia M.S., O'Brien T.P., Hou P.C., Schuman A., Sambursky R. Multi-tiered screening and diagnosis strategy for COVID-19: a model for sustainable testing capacity in response to pandemic. Ann Med. Aug 2020;52(5):207–214. doi: 10.1080/07853890.2020.1763449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackey K, Ayers CK, Kondo KK, et al. Racial and Ethnic Disparities in COVID-19-Related Infections, Hospitalizations, and Deaths : A Systematic Review. Ann Intern Med. Dec 1 2020;doi:10.7326/m20-6306. [DOI] [PMC free article] [PubMed]
- Dodds C., Fakoya I. Covid-19: ensuring equality of access to testing for ethnic minorities. BMJ. 2020;369 doi: 10.1136/bmj.m2122. [DOI] [PubMed] [Google Scholar]
- Azar KMJ, Shen Z, Romanelli RJ, et al. Disparities In Outcomes Among COVID-19 Patients In A Large Health Care System In California. Health Aff (Millwood). May 21 2020:101377hlthaff202000598. doi:10.1377/hlthaff.2020.00598. [DOI] [PubMed]
- Lieberman-Cribbin W., Tuminello S., Flores R.M., Taioli E. Disparities in COVID-19 Testing and Positivity in New York City. American Journal of Preventive Medicine. 2020;59(3):326–332. doi: 10.1016/j.amepre.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Io M. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. The National Academies Press. 2003:780. [PubMed] [Google Scholar]
- Singh M. New testing shortages hit California's vulnerable hardest amid record Covid-19 infections. The Guardian. 2020 July 25. Accessed 2020 August 26. https://www.theguardian.com/us-news/2020/jul/25/california-coronavirus-testing-shortage-minority-low-income.
- Hoffman K.M., Trawalter S., Axt J.R., Oliver M.N. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci U S A. 2016;113(16):4296–4301. doi: 10.1073/pnas.1516047113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elidon J, Burch ADS. Questions of Bias in COVID-19 Treatment Add to the Mourning for Black Families. The New York Times. May 10, 2020. Accessed August 5, 2020. https://www.nytimes.com/2020/05/10/us/coronavirus-african-americans-bias.html.
- Price-Haywood E.G., Burton J., Fort D., Seoane L. Hospitalization and Mortality among Black Patients and White Patients with Covid-19. New England Journal of Medicine. 2020;382(26):2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Society for Microbiology. Supply Shortages Impacting COVID-19 and Non-COVID Testing. Updated November 9, 2020. Accessed November 9, 2020, https://asm.org/Articles/2020/September/Clinical-Microbiology-Supply-Shortage-Collecti-1#:~:text=50.0%25%20of%20labs%20have%20a,bronchitis%20and%20urinary%20tract%20infections).
- USA Facts. COVID-19 Data. Accessed 2020/6/26, https://usafacts.org/articles/detailed-methodology-covid-19-data/.
- Staff A. A Timeline of COVID-19 Developments in 2020. Updated November 25, 2020. December 11, 2020. https://www.ajmc.com/view/sabcs-session-dives-deep-into-whether-all-patients-with-breast-cancer-should-receive-genetic-testing.
- Neilson S, Woodward A. A comprehensive timeline of the coronavirus pandemic at 12 months, from China's first case to the present Business Insider. https://www.businessinsider.com/coronavirus-pandemic-timeline-history-major-events-2020-3#january-20-the-first-us-case-was-reported-a-35-year-old-man-in-snohomish-county-washington-6.
- Wong M.S., Hoggatt K.J., Steers W.N., Frayne S.M., Huynh A.K., Yano E.M., Saechao F.S., Ziaeian B., Washington D.L. Racial/Ethnic Disparities in Mortality Across the Veterans Health Administration. Health Equity. 2019;3(1):99–108. doi: 10.1089/heq.2018.0086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moy EM. VHA Health Equity Action Plan FY2021 Operational Plan. 2020. https://www.va.gov/HEALTHEQUITY/docs/OHE_Operational_Plan_FY2021-12162020.pdf.
- Rentsch CT, Kidwai-Khan F, Tate JP, et al. Covid-19 by Race and Ethnicity: A National Cohort Study of 6 Million United States Veterans. medRxiv. May 18 2020;doi:10.1101/2020.05.12.20099135.
- Rannan-Eliya RP, Wijemunige N, Gunawardana J, et al. Increased Intensity Of PCR Testing Reduced COVID-19 Transmission Within Countries During The First Pandemic Wave. Health Affairs. 0(0):10.1377/hlthaff.2020.01409. doi:10.1377/hlthaff.2020.01409. [DOI] [PubMed]
- Agha Z., Lofgren R.P., VanRuiswyk J.V., Layde P.M. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160(21):3252–3257. doi: 10.1001/archinte.160.21.3252. [DOI] [PubMed] [Google Scholar]
- Abbott B, Lovett I. Covid-19 Test Shortages Prompt Health Authorities to Narrow Access. Wall Street Journal. 2020, July 23. Accessed 2020, August 26. https://www.wsj.com/articles/covid-19-test-shortages-prompt-health-authorities-to-narrow-access-11595515592.