Abstract
Background
Norwich terriers are affected by an upper airway syndrome (NTUAS) but little is known about outcome in affected dogs.
Objective
To determine outcome in dogs with NTUAS using owner questionnaires.
Animals
Thirty‐four client‐owned dogs.
Methods
At initial assessment, owners were questioned about respiratory noises and exercise tolerance. A NTUAS score was prospectively constructed based on the number and severity of obstructive lesions detected endoscopically (range, 0‐25). Owner questionnaires on respiratory noises, exercise tolerance, and quality of life (QOL) were obtained 2.2‐9.3 years (median, 4.2 years) after endoscopy.
Results
Dogs ranged from 0.5 to 10.7 years of age (median, 4.75 years) at initial examination and no correlation was found between age and NTUAS score (median, 13; range, 1‐25). Of 5 possible laryngeal abnormalities, 7 dogs had 1‐2, 10 dogs had 3, and 17 dogs had 4‐5 abnormalities (median, 3.5). Surgery was performed in 15 dogs, which had higher NTUAS scores (18.5 ± 6.3) than dogs that did not have surgery (7.7 ± 4.7, P < .0001). Scores for QOL ranged from 0 to 31 out of 40, with higher scores indicating worse QOL. Owner surveys resulted in QOL scores of ≤3 in 25/31 dogs (81%), with worse scores in dogs that had surgery performed (median 5, vs 0; P = .003). No correlation was noted between NTUAS and QOL scores, but age at follow‐up was weakly associated with worse QOL.
Conclusions and Clinical Importance
Despite variable severity of NTUAS scores, owners reported excellent QOL for most Norwich terriers examined.
Keywords: anatomy and pathology, endoscopy, laryngeal//pharyngeal inflammatory disease, larynx, pharynx, respiratory tract, surgery
Abbreviations
- BOAS
brachycephalic obstructive airway syndrome
- NTUAS
Norwich terrier upper airway syndrome
- QOL
quality of life
1. INTRODUCTION
Norwich terriers are affected by a genetic disorder of the larynx that mimics some clinical features of classic brachycephalic obstructive airway syndrome (BOAS) but appears clinically distinct enough from this syndrome to be considered its own entity. 1 , 2 , 3 , 4 Some affected dogs can be stertorous or stridorous or experience marked respiratory distress, whereas others can appear relatively normal despite substantial morphologic changes in the upper airway. 2 Although the primary abnormality is unclear, the majority of affected Norwich terriers, unlike brachycephalic dogs, have normal nares and palate but often have excessive supraglottic tissue and a narrow key hole or V‐shaped lumen in the immediate infraglottic region. 2 , 4 Narrowing of the laryngeal opening increases resistance to airflow, which could augment soft tissue swelling in the oropharynx. A mutation in the gene for ADAMTS3 metallopeptidase enzyme, responsible for promotion of lymphangiogenesis, could make Norwich terriers predisposed to develop this exuberant soft tissue swelling because of lymphedema. 5
Treatment for classic BOAS relies on surgical amelioration of structures causing airway obstruction and traditionally involves a combination of alar fold resection or other rhinoplasty to widen the nares, ventriculectomy (sacculectomy), and staphylectomy. 6 , 7 , 8 , 9 , 10 In dogs with classic BOAS, 30% to 90% improvement in clinical signs has been reported after surgery. 7 , 8 , 11 The role of ventricular resection in the management of BOAS is controversial, with 1 retrospective study reporting increased complications in dogs that had sacculectomy performed as part of treatment. 12 Ventricular edema and eversion can persist or recur if the primary source of airway obstruction remains unresolved. 13
Owners and breeders have been aware of NTUAS for decades, but little is known about appropriate surgical intervention or outcome in Norwich terriers with various forms of airway obstruction. A scoring system was created to stratify the upper airway abnormalities common to the Norwich terrier breed 4 (https://norwichterrierclub.org/wp-content/uploads/2020/06/NTUAS-Score-Sheet-2020-05-25-1.pdf) and there are ongoing efforts to identify appropriate breeding pools that have minimal manifestations of NTUAS. Until this goal has been achieved, affected dogs will continue to require medical and often surgical intervention.
Our primary objective was to assess owner reports of long‐term outcome in Norwich terriers with upper airway syndrome. To accomplish this, owners of Norwich terriers that had undergone upper airway endoscopy over a 7‐year period were asked to complete a follow‐up questionnaire describing respiratory noise and dysfunction and to quantify quality of life (QOL), using a survey modified from a previously validated assessment of QOL in dogs with cardiac disease. 14 We hypothesized that dogs with higher NTUAS scores on initial endoscopic evaluation would have poorer exercise tolerance, increasing body weight with age because of poor exercise ability, and higher scores on an abbreviated QOL survey, indicating worse QOL, as reported by the owner. The role of surgical intervention also was investigated and contrasted with endoscopic findings, surgery, and postoperative management in typical brachycephalic breeds.
2. METHODS
Norwich terriers that had upper airway endoscopy performed between 2011 and 2018 at the University of California William R. Pritchard Veterinary Medical Teaching Hospital were eligible for inclusion in the study. Owners were asked to quantify the following clinical signs as absent, rare (<1 time per week), occasional (a few times a week), intermittent (1 time per day), frequently (several times daily), or all of the time: respiratory noise (loud, raspy, or gurgly), difficult breathing, excessive panting, coughing, gagging, collapse, and snoring. Exercise tolerance was graded on a scale of 0‐5, with a score of 0 indicating no restrictions, 1: can run but has to sit, 2: walks well but has to sit, 3: short walks but pants heavily, 4: will collapse on walks, 5: cannot exercise at all. Dogs were excluded if the medical record was incomplete or if a recording of endoscopy at initial evaluation was unavailable for appropriate scoring of upper airway abnormalities.
All endoscopic procedures were performed in standardized fashion by one of the authors (LRJ). Abnormalities in laryngeal structures were noted including swelling of the dorsal pharyngeal wall obscuring the corniculate processes, redundant supraglottic tissue with obliteration of the piriform recess, and narrowing of the infraglottic lumen into a V or keyhole shape. 2 Laryngeal ventricular eversion (stage 1 laryngeal collapse) and midline apposition or overlap of the cuneiform processes (stage 2 laryngeal collapse) 15 also were recorded for a total of 5 possible laryngeal abnormalities (Figure 1). Findings were entered into a NTUAS upper airway examination scoring sheet (Appendix I) in which points were assigned for the severity of abnormality noted. The NTUAS score was created only at the initial visit. If previous ventriculectomy had been performed, dogs were assigned the maximum score for that abnormality. Possible NTUAS scores ranged from 0 to 25, with higher scores reflecting worse obstruction. The type of abnormalities identified in each dog and the number of abnormalities per dog were recorded.
FIGURE 1.

Endoscopic view of the larynx illustrating several abnormalities associated with NTUAS. 1: the dorsal pharyngeal wall is normal in this case. 2: exuberant tissue obscures the piriform recess bilaterally. 3: both cuneiform processes are deviated to the midline. 4: ventricular edema and eversion is present. The infraglottic lumen is not visible in this image
Age, weight, sex, and body condition score (BCS) on a scale 1 to 9 were recorded at the time of initial examination. Previous surgical interventions were noted in addition to surgical or medical treatment provided at the time of endoscopy or at any time up until follow‐up.
Owners were contacted by phone and email to participate in follow‐up evaluation of outcome by use of questionnaires distributed and collected electronically. If the dog was no longer alive, the circumstances of death were requested. Owners reported body weight, presence of other diseases, and use of supplements or medications. Owners were queried about clinical signs and exercise tolerance as described above and also were asked to complete a modified QOL survey (Appendix II). A maximum score of 40 points was possible for QOL, with higher scores reflecting worsened QOL.
3. STATISTICAL ANALYSIS
Clinical data were assessed for normality using D'Agostino & Pearson omnibus normality test. Normally distributed data are presented as mean ± SD and data that were not normally distributed are presented as median with range. Statistical comparisons were made using a Student's t test for normally distributed data and the Mann‐Whitney U test for nonparametric data. Linear regression was used to correlate age at study entry with NTUAS score, and age at follow‐up with QOL score. Outliers were identified and excluded based on the method of residuals. Exercise tolerance at study entry and at follow‐up was compared using the Wilcoxon matched‐pairs signed rank test. Quality of life and NTUAS scores were compared between dogs that did and did not have surgery. All statistical analyses were performed using commercially available software (GraphPad Prism v5.0f, San Diego, CA) with a significance level of P < .05.
4. RESULTS
Between 2011 and 2018, upper airway endoscopy was performed on 48 Norwich terriers. Clinical features of some of these dogs were reported previously. 2 Twenty‐nine dogs had been enrolled in a larger study of NTUAS. 4 Two of these 29 dogs were lost to follow‐up and did not participate in the current study. An additional 19 dogs were presented to the University of California William R. Pritchard Veterinary Medical Teaching Hospital for upper airway evaluation, 4 of which were excluded because of nasopharyngeal disease and 1 because of a laryngeal polyp. In the remaining 14 dogs, 4 laryngeal examinations could not be scored because of missing or inadequate capture of endoscopic recordings, and 3 owners declined to participate, resulting in a total of 34 Norwich terriers in the present study, completed in September 2020.
Mean age of dogs at the time of initial examination was 4.3 ± 3.3 years, mean weight was 5.7 ± 0.8 kg, and mean body condition score was 5 ± 1 out of 9. The group consisted of 14 females (6 intact, 8 spayed) and 20 males (11 intact and 9 neutered). Two dogs had undergone ventriculectomy and 1 had both ventriculectomy and staphylectomy performed by the referring veterinarian before evaluation. Increased respiratory noise was reported on initial presentation in 20/34 dogs (59%), excessive panting in 14/34 dogs (41%), and owners of 15/34 (44%) dogs indicated that the dogs snored often or sometimes while sleeping. Three of 34 dogs were reported to have difficulty sleeping. Norwich terrier upper airway syndrome scores ranged from 1 to 25 out of 25 with a median of 13. No correlation was found between age at examination and NTUAS score (P = .2).
The most common laryngeal abnormality found in all dogs (34/34) examined was ventricular eversion, which also was found in 3 dogs that had previously undergone ventriculectomy. The second most common abnormality was excessive supraglottic tissue with obliteration of the piriform recess in 28/34 dogs (82%), which was moderate in 13 and severe in 15. Narrowing of the infraglottic lumen was present in 24/34 dogs (71%) and stage 2 laryngeal collapse, characterized by midline or overlapping cuneiform processes, was identified in 16/34 dogs (47%). Swelling of the dorsal pharyngeal wall overlapping the corniculate processes was found in 14/34 dogs (41%). Of the 5 possible laryngeal abnormalities listed above, 4 dogs had 1, 3 dogs had 2, 10 dogs had 3, 9 dogs had 4, and 8 dogs had 5 abnormalities (median, 3.5 abnormalities per dog). One dog had mild elongation of the soft palate characterized by 5‐6 mm extension of the soft palate beyond the caudal pole of the tonsil; epiglottic entrapment was not visualized in any dog.
Immediately after endoscopy, bilateral ventriculectomy was performed in 10 dogs and unilateral ventriculectomy was performed in 3 dogs using endoscopic Metzenbaum scissors. One dog also had removal of a subepiglottic cyst, and 1 dog had staphylectomy alone. Of the 3 dogs in which unilateral ventriculectomy was performed, 1 had previously undergone laser excision of the ventricles with regrowth and protrusion on the right, and 2 dogs had severe eversion on only 1 side, in conjunction with other manifestations of NTUAS. The NTUAS score was higher in dogs that had surgery performed (18.5 ± 6.3) than in dogs that did not (7.7 ± 4.7; Figure 2, P < .0001). Dogs that had ventriculectomy performed had a median of 5 laryngeal abnormalities detected (range, 1‐5) in comparison to a median of 3 (range, 1‐4) in dogs that did not have ventriculectomy performed (P = .0006).
FIGURE 2.
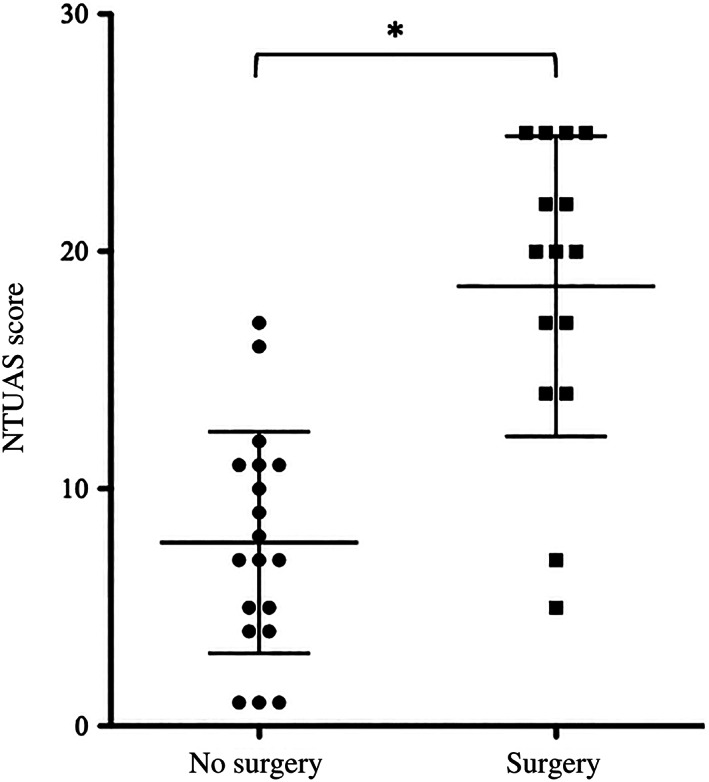
The severity of NTUAS score was significantly higher in dogs that had surgery performed (n = 15) than in those that did not (n = 19), *P < .0001
Postoperative corticosteroids were utilized in all dogs that had ventriculectomy performed and in 1 dog that did not have surgery. A tapering dose of PO prednisone at anti‐inflammatory dosages (0.5 mg/kg/day) was administered over 1‐2 weeks in 8 dogs, inhaled fluticasone (110 μg/puff) was dispensed to 5 dogs for postoperative and intermittent use as needed, and a combination was used in 1 dog. Four dogs with NTUAS scores of 25, 14, 17, and 17 had a second ventriculectomy 6 or 9 months and 3 or 4 years after the original surgery. One of these dogs (NTUAS score, 14) also had redundant supraglottic tissue excised from the piriform recess and the mucosa oversutured to improve the airway opening 6 months after sacculectomy, as did a second dog 5 years after its original surgery (NTUAS score, 22). Both of these dogs had been reevaluated at the hospital for complaints of marked respiratory distress and cyanosis during excitement or exercise.
Follow‐up information was obtained by owner questionnaires a median of 4.2 years (range, 2.2‐9.3 years) after the original visit. Mean age at follow‐up was 8.4 ± 3.5 years. Two dogs had died at ages 14 and 15 and a third was euthanized at age 15 (46, 49, and 112 months after initial evaluation), and NTUAS scores in these dogs were 14, 20, and 25. All of these dogs had undergone ventriculectomy at the time of endoscopy. Follow‐up surveys were completed on the remaining 31 dogs. Median age at follow‐up was 9.3 years (range, 2.75‐15.3 years). Weight of dogs at follow‐up (6.1 ± 0.9 kg) was not significantly different from weight at the original examination (P = .1). Respiratory noise, snoring, and panting had continued or developed in many dogs (Figure 3) regardless of whether or not surgery had been performed. Difficulty sleeping was reported in only 1 dog at follow‐up.
FIGURE 3.
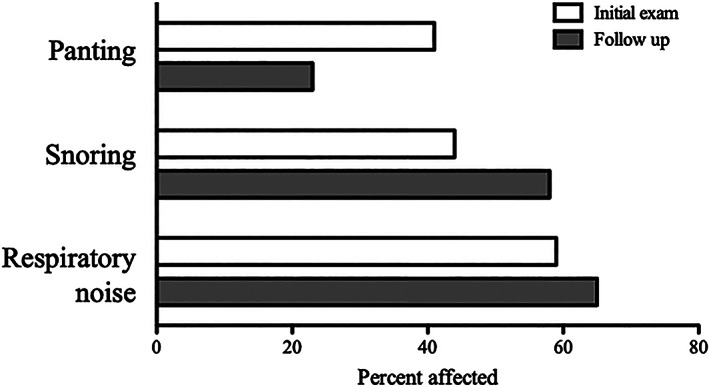
The percentage of Norwich terriers reported by owners to have panting, snoring, and respiratory noise are presented at initial exam (white bars) and at follow‐up (gray bars)
Exercise tolerance was not different at study entry (median, 0.5; range, 0‐4) compared to follow‐up (median, 1; range, 0‐3; P = .42), although only 3 dogs had moderate to severe exercise restriction (score, 2‐4) at either time point. Exercise tolerance at study entry did not differ between dogs that had surgery performed (median, 1; range, 0‐5) and those that did not (median, 1; range, 1‐3; P = .44), and surgical intervention did not play a role in changes in exercise tolerance, with a median score of 1 for dogs that did or did not have surgery.
Quality of life scores at follow‐up ranged from 0 to 31 out of a total of 40, with a median value of 0, which was reported for 16/31 (52%) dogs. Scores ranging from 1 to 3 were calculated for an additional 9/31 (29%) dogs, and scores >5 were found in only 6/31 (19%) dogs, all of which had surgery performed. Scores for QOL did not correlate with NTUAS score (P = .61) or with change in weight (P = .91) but had a weak correlation with age (P = .007, r 2 = .23, Figure 4), indicating worse QOL with aging. Quality of life score at follow‐up was significantly higher (worse) in dogs that had surgery performed (median, 5; range, 0‐31) than in those that did not (median, 0; range, 0‐3; P = .003, Figure 5).
FIGURE 4.
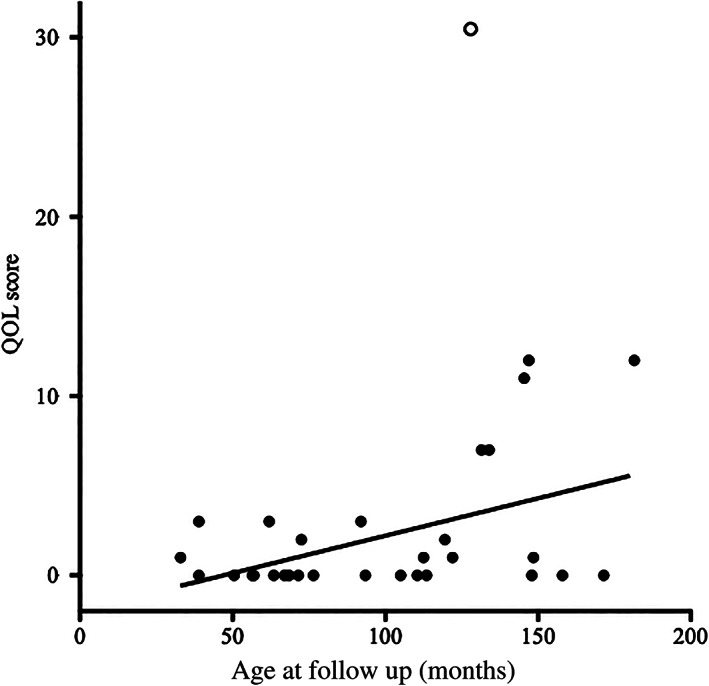
Quality of life (QOL) score showed a weak but significant correlation with age at follow‐up evaluation, P = .008, r 2 = .23. The open circle represents an outlier
FIGURE 5.
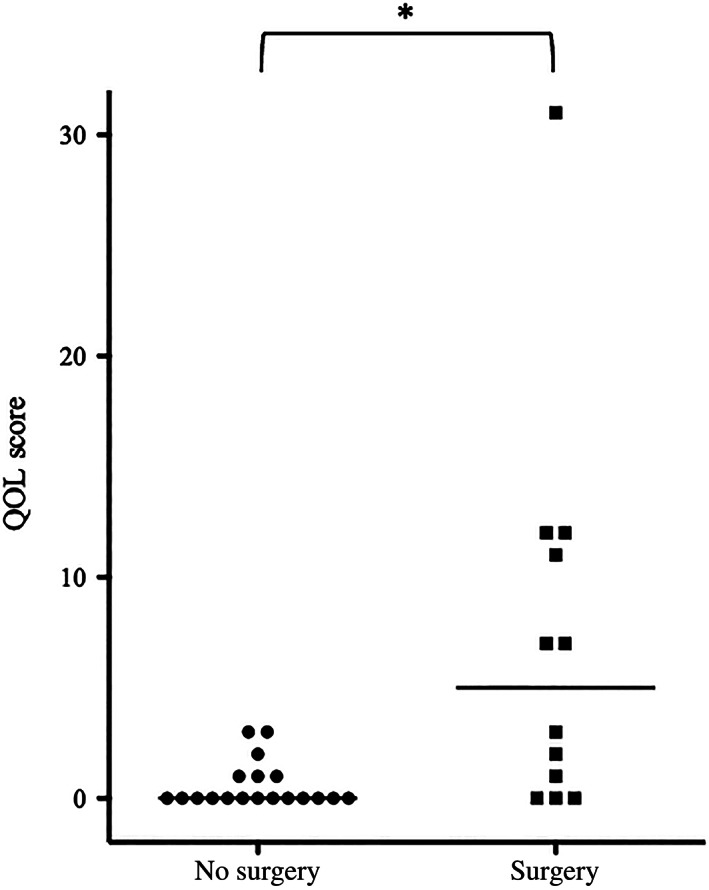
Quality of life score at follow‐up was significantly higher (worse) in dogs that had surgery performed at initial evaluation than those that did not, *P = .003
5. DISCUSSION
Our study was designed to assess exercise tolerance and QOL in Norwich terriers with variable severity of upper airway syndrome, and we also evaluated the effect of surgery on these outcome measures. The most common clinical complaints at initial evaluation were respiratory noises, excess panting, and snoring, which were also present at follow‐up, regardless of whether or not ventriculectomy or other surgery had been performed. Up to 40% of owners of brachycephalic dogs do not recognize stertor, stridor, or snoring as abnormal but instead accept it as a breed standard. 6 , 16 , 17 It is possible that a similar situation also could play a role in the disease manifested by Norwich terriers. Snoring and excess panting commonly persist postoperatively in brachycephalic breeds 7 and findings in the Norwich terriers examined here were similar, despite a lack of nasal obstruction in this breed. Although snoring was common, only a single owner reported possible sleep‐disordered breathing, a condition recognized in the Cavalier King Charles spaniel, 18 which is another breed of dog with unusual manifestations of BOAS.
The NTUAS scores were higher in dogs that had surgery performed, and these dogs had a higher number of laryngeal abnormalities detected. It is likely that the severity of obstructive abnormalities noted played a role in the decision to pursue surgery in an attempt to alleviate some degree of airway obstruction with a relatively straightforward surgical procedure. Removal of everted laryngeal ventricles as a sole procedure is not recommended in typical breeds of brachycephalic dogs because alleviation of more rostral sources of airway obstruction (eg, stenotic nares, soft palate elongation) resolves clinical signs. 6 , 8 Also, removal of a single saccule is not sufficient to resolve edema or eversion in the contralateral saccule. 13 Laryngeal ventriculectomy is a well‐described procedure commonly performed in BOAS dogs, but indications for its use in NTUAS have not been fully explored and further studies are warranted.
Ventricular eversion is a common secondary complication of upper airway obstruction in multiple brachycephalic breeds, 8 , 10 , 12 but the other specific findings related to excessive tissue swelling found in Norwich terriers are not. Therefore, it is curious that owners reported such good QOL scores for most of the dogs examined in our study. Excessive supraglottic tissue obscuring the piriform recess was frequently observed in our study (82% of dogs). These abnormalities are not commonly reported in other brachycephalic breeds, despite the fact that both English and French Bulldogs also have a genetic mutation in the ADAMTS3 metallopeptidase enzyme. 5 Resection of the excessive and redundant supraglottic tissue is more challenging, and 2 dogs in our study had this intervention performed when they represented postoperatively with more severe and progressive clinical signs. This procedure has not been well‐described, and no previous studies of its therapeutic benefit are available in dogs. Supraglottoplasty using debridement or laser ablation has proven useful in management of redundant arytenoid mucosa in children with congenital laryngomalacia. 19 , 20 Also, early intervention in affected infants resulted in resolution of signs as well as improved QOL for children and caregivers. 20 , 21 Additional study is required to determine whether resection of redundant supraglottic tissue earlier in the course of the disease would benefit affected Norwich terriers, regardless of clinical signs of obstruction.
Narrowing of the infraglottic lumen (71% of dogs) and medial displacement of the cuneiform processes (47% of dogs) also were common in this group of dogs. These obstructions can require aggressive surgical procedures in dogs with classic BOAS, 22 , 23 such as ventral laryngotomy, laryngeal stents, and permanent tracheostomy, none of which were pursued in our study. It is surprising that these more invasive procedures were not required given that the extent of obstructive lesions was severe in most Norwich terriers examined in our study, with >3 of 5 possible laryngeal abnormalities visualized in 27/34 (79%) of dogs. This could be a reflection of the diligence of Norwich terrier owners in maintaining ideal body weight and condition for their dogs and in managing activity levels when necessary. Most dogs in our study lived in warm to hot environments, but the low humidity in the region might have afforded some protection against additional obstructive signs.
Ventriculectomy did not improve exercise tolerance at the time of follow‐up, but most dogs were not severely exercise‐restricted despite the extent of their obstructive lesions. It is likely that the questions used in this study to assess exercise tolerance were not sufficient to detect deficiencies. Norwich terriers are known for vigorous activities in rodent hunting and agility trials, and only 3/34 dogs were reported to have poor exercise tolerance in our cohort. The 3 or 6 minute walk tests have been used extensively to evaluate respiratory dysfunction in more typical brachycephalic dogs, 24 , 25 , 26 , 27 and it is likely that a similar evaluation would be more useful in assessing Norwich terriers before and after interventions.
Age at the time of diagnosis did not play a role in the overall severity of airway obstruction as reflected by the NTUAS score, with severe manifestations of obstruction present in young as well as older animals. The effect of age on the severity of brachycephaly in typically affected breeds is difficult to discern, yet in some studies, very young dogs have displayed severe manifestations of disease 24 , 28 similar to what was observed in our study. The age at which brachycephalic abnormalities should be surgically addressed remains controversial, with younger age reported as a negative prognostic indicator in 1 study, 22 although it also has been suggested that early intervention might improve breathing later in life. 29 Despite the fact that multiple obstructive lesions were identified in most Norwich terriers examined in our study, many dogs experienced extended survival over 9 years after the initial evaluation, with only 3 dogs having died at ages 14 to 15.
Not surprisingly, QOL scores were worse at follow‐up in dogs that had undergone ventriculectomy or other surgery, likely reflecting the severity of disease present originally, but most dogs in each group were given very low QOL scores by owners, suggesting that they believed their dogs enjoyed good QOL. Worsened QOL could be related to other aging disorders that were not evaluated in our study such as concurrent gastrointestinal, endocrine, or orthopedic problems. Other potential benefits of surgery likely were present, such as a decrease in the stimulus for further soft tissue swelling related to surgical alleviation of the ventricular component of airway obstruction. Future intubation efforts might have been facilitated by an increase in the size of the laryngeal opening, and the possibility for decreased risk of aspiration events in subsequent anesthetic episodes should be considered, as has been reported in brachycephalic breeds that have had corrective surgery performed. 30 Long‐term studies in Norwich terriers are indicated to address the impact of breathing abnormalities throughout life.
Our study had several limitations. Dogs were not reexamined at follow‐up, and therefore surveys relied on owner‐reported signs and scoring of both QOL and exercise tolerance. Most of the owners remained in contact with the investigators over the course of the study, but some owners did not respond to the invitation to participate in the study, which could have biased results. Therefore, conclusions of our study might not apply to all Norwich terriers affected by NTUAS. Many dogs in our study were recruited into a large scale investigation of NTUAS, which might have selected for specific types of dogs or owners. Although surveys were collected in real time, differences in owner perceptions could have impacted results. Quality of life was not assessed at study entry to allow comparison with follow‐up results, and effects of surgery on this variable could change over time, as indicated by the worsened QOL scores associated with aging. Finally, most scoring systems that are available for clinical studies imply an equal contribution of each variable to the final score. The NTUAS score and QOL survey are no exceptions and do not attempt to weight 1 finding or response higher than another. It is possible that the clinical impact of ventricular eversion varies from that of excessive supraglottic tissue with obliteration of the piriform recess, but a linear score cannot account for variable consequences of these different types of obstruction.
Despite these limitations, results of our follow‐up evaluation are encouraging given the long term survival and good QOL scores in most Norwich terriers despite the severity of airway obstruction observed initially. Medial displacement of the cuneiform processes (stage 2 laryngeal collapse) often results in debilitating signs in typical brachycephalic dogs yet the dogs examined in our study apparently coped well with the disorder. This might reflect the lack of nasal, palatal, or glossal obstructions, which play a substantial role in airway obstructive signs in typical brachycephalic breeds. It also could be related to the lack of gastrointestinal abnormalities in Norwich terriers, which appear to worsen or complicate disease in many dogs with classic BOAS 6 as well as in children with laryngomalacia. 21 Finally, excellent long term results could be related to other conformational differences such as neck girth or length, or to the low rate of obesity in the Norwich terriers compared to typical brachycephalic breeds.
CONFLICT OF INTEREST DECLARATION
Authors declare no conflict of interest.
OFF‐LABEL ANTIMICROBIAL DECLARATION
Authors declare no off‐label use of antimicrobials.
INSTITUTIONAL ANIMAL CARE AND USE COMMITTEE (IACUC) OR OTHER APPROVAL DECLARATION
Approved by the University of California, Davis IACUC, number 18893.
HUMAN ETHICS APPROVAL DECLARATION
Authors declare human ethics approval was not needed for this study.
Supporting information
Appendix I: Scoring system for Norwich Terrier upper airway syndrome
Appendix II: Modified quality of life survey for Norwich terriers.
ACKNOWLEDGMENT
Funding provided by the Bailey Wrigley Fund, University of California Davis and the American Kennel Club Canine Health Foundation Grant No. 02232‐MOU.
Johnson LR, Mayhew PD, Culp WTN, Stanley BJ. Results of owner questionnaires describing long‐term outcome in Norwich terriers with upper airway syndrome: 2011‐2018. J Vet Intern Med. 2021;35(4):1950–1956. 10.1111/jvim.16180
Funding information American Kennel Club Canine Health Foundation, Grant/Award Number: 02232‐MOU; The Bailey Wrigley Fund University of California
REFERENCES
- 1. Dietschi E, Ruchti M, Gaillard C, et al. Oberes Luftweg‐Syndrom beim Norwich Terrier. J Swiss Cynological Soc SKG. 2010;19:3. [Google Scholar]
- 2. Johnson LR, Mayhew PD, Steffey MA, et al. Upper airway obstruction in Norwich terriers. J Vet Int Med. 2013;27:1409‐1415. [DOI] [PubMed] [Google Scholar]
- 3. Koch DA, Rosaspina M, Wiestner T, et al. Comparative investigations on the upper respiratory tract in Norwich terriers, brachycephalic and mesaticephalic dogs. Schweiz Arch Tierheilkd. 2014;156:119‐124. [DOI] [PubMed] [Google Scholar]
- 4. Lai GP, Stanley BJ, Nelson NC, et al. Clinical and laryngoscopic characterization of Norwich terrier upper airway syndrome (NTUAS): preliminary results. Paper presented at: European College of Veterinary Surgeons Annual Meeting; 2018; Athens, Greece.
- 5. Marchant TW, Dietschi E, Rytz U, et al. An ADAMTS3 missense variant is associated with Norwich Terrier upper airway syndrome. PLoS Genetics. 2019;15(5):e1008102. 10.1371/journal.pgen.1008102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Poncet CM, Dupre GP, Freiche VG, Bouvy BM. Long‐term results of upper respiratory syndrome surgery and gastrointestinal tract medical treatment in 51 brachycephalic dogs. J Small Anim Pract. 2006;47:137‐142. [DOI] [PubMed] [Google Scholar]
- 7. Torrez CV, Hunt GB. Results of surgical correction of abnormalities associated with brachycephalic airway obstruction syndrome in dogs in Australia. J Small Anim Pract. 2006;47:150‐154. [DOI] [PubMed] [Google Scholar]
- 8. Riecks TW, Birchard SJ, Stephens JA. Surgical correction of brachycephalic syndrome in dogs: 62 cases (1991‐2004). J Am Vet Med Assoc. 2007;230:1324‐1328. [DOI] [PubMed] [Google Scholar]
- 9. Fasanella FJ, Shivley JM, Wardlaw JL, Givaruangsawat S. Brachycephalic airway obstructive syndrome in dogs: 90 cases (1991‐2008). J Am Vet Med Assoc. 2010;237:1048‐1051. [DOI] [PubMed] [Google Scholar]
- 10. Bernaerts F, Talavera J, Leemans J, et al. Description of original endoscopic findings and respiratory functional assessment using barometric whole‐body plethysmography in dogs suffering from brachycephalic airway obstruction syndrome. Vet J. 2010;183:95‐102. [DOI] [PubMed] [Google Scholar]
- 11. Haimel G, Dupre G. Brachycephalic airway syndrome: a comparative study between pugs and French bulldogs. J Small Anim Pract. 2015;56:714‐719. [DOI] [PubMed] [Google Scholar]
- 12. Hughes JR, Kaye BM, Beswick AR, Ter Haar G. Complications following laryngeal sacculectomy in brachycephalic dogs. J Small Anim Pract. 2018;59:16‐21. [DOI] [PubMed] [Google Scholar]
- 13. Cantatore M, Gobbetti M, Romussi S, et al. Medium term endoscopic assessment of the surgical outcome following laryngeal saccule resection in brachycephalic dogs. Vet Rec. 2012;170:518‐525. [DOI] [PubMed] [Google Scholar]
- 14. Freeman LM, Rush JE, Farabaugh AE. Development and evaluation of a questionnaire for assessing health‐related quality of life in dogs with cardiac disease. J Am Vet Med Assoc. 2005;226:1864‐1868. [DOI] [PubMed] [Google Scholar]
- 15. Leonard HC. Collapse of the larynx and adjacent structures in the dog. J Am Vet Med Assoc. 1960;137:360‐363. [PubMed] [Google Scholar]
- 16. Packer R, Hendricks A, Burn C. Do dog owners perceive the clinical signs related to conformational inherited disorders as “normal” for the breed? A potential constraint to improving canine welfare. Anim Welf. 2012;21:81‐93. [Google Scholar]
- 17. Liu N‐C, Sargan D, Adams V, et al. Characterisation of brachycephalic obstructive airway syndrome in French bulldogs using whole‐body barometric plethysmography. PLoS One. 2015;10(6):e0130741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hinchcliffe TA, Liu N, Ladlow J. Sleep‐disordered breathing in the Cavalier King Charles spaniel: a case series. Vet Surg. 2019;49:497‐504. [DOI] [PubMed] [Google Scholar]
- 19. Zainal A, Goh BS, Mohamed AS. Supraglottoplasty for laryngomalacia: who will benefit? Asian J Surg. 2011;34:92‐96. [DOI] [PubMed] [Google Scholar]
- 20. Vandjelovic ND, Brown JR, Traboulsi HT, Thottam PJ. Impact of infant supraglottoplasty on quality of life. Otolaryngol Head Neck Surg. 2018;159:564‐571. [DOI] [PubMed] [Google Scholar]
- 21. Garritano FG, Carr MM. Characteristics of patients undergoing supraglottoplasty for laryngomalacia. Int J Pediatric Otorhinolaryngol. 2014;78:1095‐1100. [DOI] [PubMed] [Google Scholar]
- 22. Liu N‐C, Oechtering GU, Adams VJ, et al. Outcomes and prognostic factors of surgical treatments for brachycephalic obstructive airway syndrome in 3 breeds. Vet Surg. 2017;46:271‐280. [DOI] [PubMed] [Google Scholar]
- 23. Gobbetti M, Romussi S, Buracco P, et al. Long‐term outcome of permanent tracheostomy in 15 dogs with severe laryngeal collapse secondary to brachycephalic airway obstructive syndrome. Vet Surg. 2018;47:648‐653. [DOI] [PubMed] [Google Scholar]
- 24. Liu N‐C, Adams V, Kalmar L, et al. Whole‐body barometric plethysmography characterizes upper airway obstruction in 3 brachycephalic breeds dogs. J Vet Intern Med. 2016;30:853‐865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lilja‐Maula L, Lappalainen AK, Hyytiäinen HK, et al. Comparison of submaximal exercise test results and severity of brachycephalic obstructive airway syndrome in English bulldogs. Vet J. 2017;219:22‐26. [DOI] [PubMed] [Google Scholar]
- 26. Aromaa M, Lilja‐Maula L, Rajamäki MM. Assessment of welfare and brachycephalic obstructive airway syndrome signs in young, breeding age French bulldogs and pugs, using owner questionnaire, physical examination and walk tests. Anim Welf. 2019;28:287‐298. [Google Scholar]
- 27. Riggs J, Liu N‐C, Sutton DR, et al. Validation of exercise testing and laryngeal auscultation for grading brachycephalic obstructive airway syndrome in pugs, French bulldogs, and English bulldogs by using whole‐body barometric plethysmography. Vet Surg. 2019;48:488‐496. [DOI] [PubMed] [Google Scholar]
- 28. Pink J, Doyle R, Hughes J, et al. Laryngeal collapse in seven brachycephalic puppies. J Small Anim Pract. 2006;47:131‐135. [DOI] [PubMed] [Google Scholar]
- 29. Huck JL, Stanley BJ, Hauptman JG. Technique and outcome of nares amputation (Trader's technique) in immature Shih Tzus. J Am Anim Hosp Assoc. 2008;44:82‐85. [DOI] [PubMed] [Google Scholar]
- 30. Doyle CR, Aarnes TK, Ballash GA, et al. Anesthetic risk during subsequent anesthetic events in brachycephalic dogs that have undergone corrective airway surgery: 45 cases (2007‐2019). J Am Vet Med Assoc. 2020;257:744‐749. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix I: Scoring system for Norwich Terrier upper airway syndrome
Appendix II: Modified quality of life survey for Norwich terriers.


