Abstract
Background
Social anxiety disorder (SAD) commonly occurs among individuals at clinical high-risk (CHR) for psychosis. Extant research has yet to examine the prevalence and clinical/functional correlates of SAD in this population compared to a community control (CC) sample. This comparison may improve the generalizability that traditional nonpsychiatric control samples cannot provide. Additionally, it remains unknown how SAD contributes to symptom severity and social impairments in individuals at CHR for psychosis.
Methods
Both CHR and CC groups were recruited from general community sources; CC participants were not excluded in this analysis on the basis of any psychopathology except psychosis. A total of 245 adolescents and young adults (CHR = 81; CC = 164) were administered the Social Phobia Scale, the Structured Interview for Psychosis-risk Syndromes, Structured Clinical Interview for DSM-5 Research Version, and the Social Functioning Scale.
Results
The CHR group was at increased risk for having SAD relative to CC (42% CHR; 13% CC; RR = 3.28) and, to a lesser degree, a non-SAD anxiety disorder (41% CHR; 29% CC; RR = 1.42). Greater social anxiety was related to higher levels of negative (r = 0.29) but not positive (r = 0.05) symptoms within the CHR group. Furthermore, elevated social anxiety was found to be linked with poor social functioning in the CHR group (r = −0.31).
Conclusions
These findings demonstrate the specificity of SAD over and above other anxiety disorders in individuals at CHR for psychosis and the critical target of SAD to treat subclinical psychotic symptoms and social functioning.
Keywords: psychosis-risk, prodrome, social anxiety, social functioning
Introduction
Anxiety disorders are among the most common comorbid diagnoses in individuals with psychotic disorders.1,2 Among anxiety-related disorders, social anxiety, specifically, is highly prevalent among individuals with psychosis2–5 and is reflected in aspects of both positive (eg, paranoia, persecutory ideation) and negative (eg, anhedonia, alogia, and blunted expression of emotion) psychotic symptoms.6 In psychosis, social anxiety has important contributions to reduced quality of life,4 social function,4,7,8 and self-esteem.9 Social anxiety may also contribute to impairments in social support and quality of social relationships associated with worsening course and recurrence of psychotic episodes.10 This relationship to the clinical course may be particularly important for those at clinical-high risk for psychosis (CHR), who also experience elevated levels of anxiety disorders that lead them to seek treatment.11 Additionally, social anxiety may relate to the risk for psychosis (attenuated psychosis symptoms) and social functioning in CHR individuals. The prevalence and clinical impact of social anxiety may have implications for first psychosis onset, functional outcomes, and treatment targets.12
The potential influence of anxiety disorders can often be overlooked in clinical research, despite estimates of anxiety disorders in CHR individuals being high (14%–53%).13–18 However, extant research does not provide a clear comparison of prevalence rates between CHR individuals and their community peers. Instead, most extant literature compares CHR samples to non-help-seeking controls who do not endorse major psychiatric illness.16,19 By nature, this approach selects a comparison group that does not necessarily represent the general population. The few studies that have compared the rates of anxiety in help-seeking CHR individuals16,18 found social anxiety to be the most prevalent. As a result, questions remain regarding the generalizability and specificity of inferences that can be made about the comorbidity of social anxiety with CHR for psychosis.20 Nonpsychiatric samples inflate the effect of the independent variables, complicating the interpretation of study findings.21 Extant studies focused on the prevalence of social anxiety disorder (SAD) may overestimate the magnitude of the difference between groups.
The few studies that have examined the relationship between social anxiety and attenuated psychotic symptoms in CHR individuals16,18 have found conflicting results, similar to studies examining this relationship in psychosis.9,22,23 One study demonstrated a unique relationship between social anxiety and positive symptoms in CHR individuals16; the other found that social anxiety symptoms were related to both positive symptoms and negative symptoms.18 Thus, social anxiety appears related to symptom severity, but the specificity of that relationship to positive or negative symptom domains remains unclear. As a result, questions remain regarding how comorbid social anxiety may relate to symptom severity and course in those at CHR for psychosis.
Further, addressing social anxiety may attenuate social dysfunction in CHR individuals and potentially reduce the risk for worsening course.10,24 Despite a paucity of research investigating social anxiety in the psychosis-risk syndrome, a number of studies have identified the critical role of social functioning and social support in the clinical course in individuals at CHR for psychosis. People at CHR for psychosis exhibit impairments in social functioning,25 deficits in the number, and quality of close relationships, which leads to lower quality of life.26 Early impaired social functioning and quality of life in CHR individuals appears to be a core feature of risk for psychosis,24,26–31 and may be related to the presence of comorbid anxiety disorders.32,33 Yet, the particular role of social anxiety to these interpersonal functioning deficits is unknown, though social anxiety may contribute to a reduced social function.
The current study examined the prevalence of social anxiety and other anxiety disorders in a community sample of CHR young adults and community control (CC) sample. This CC comparison group includes individuals with a range of psychopathology. We hypothesized that the CHR group would be at greater risk for having a SAD diagnosis and elevated social anxiety symptoms compared to the CC group. We predicted that CHR status would be specifically related to social anxiety and not reflect a general increased risk for anxiety disorders. Next, in an effort to better understand how social anxiety is related to other core components of the CHR syndrome, the current study examined the relationship of social anxiety symptom severity to positive and negative symptom domains in the CHR group. Based on conflicting conclusions of previous studies,16,18 our analysis was exploratory. Finally, the current study examined the association between social anxiety and social functioning, specifically within a sample of CHR young adults, which may have clinical implications for the targeted treatment of social anxiety to improve functional impairments. We predicted that increased social anxiety symptoms among the CHR group would relate to decreased social functioning.
Methods
Participants
Participants included adolescents and young adults who were recruited as part of the ongoing Multisite Assessment of Psychosis-Risk34 (MAP; 2017–2020 for current analytic sample) study. The MAP study is a large investigation of early identification and evaluation of psychosis-risk within the community. Participants were recruited through various outlets, including Craigslist posts, online ads (eg, through Facebook), online student volunteer pools, a refer-a-friend link, and hanging flyers in public locations across the catchment areas: the greater Philadelphia, Chicago, and Baltimore areas. In concordance with the study goals of assessing psychosis risk in a nontreatment seeking, community comparison group, clinical locations such as outpatient clinics and hospitals were not targeted for recruitment. Inclusion criteria for the MAP study also required that all participants were proficient in English, ages 16–30, and had a normal or corrected vision. Although the presence of a past or current psychotic diagnosis (n = 3; assessed at in-person visit) was not an exclusion criterion, those with psychotic diagnoses were excluded from the current analyses.
Participant selection contained two phases: first, participants (n = 3460) completed an online survey that included a battery of questionnaires, among which were two self-report scales of psychosis-risk: the Prodromal Questionnaire35 (PQ; psychosis-risk threshold = reporting ≥ 8 distressing items on the positive symptom subscale) and the PRIME Screen36 (psychosis-risk threshold = endorsing reporting two ratings of 5s or one rating of 6). Second, eligibility to participate in Phase 2 was determined by being either above the predetermined psychosis-risk threshold (Questionnaire High Risk; n = 651) or randomly selected from participants below the threshold (Questionnaire Low Risk; n = 656). There were no other exclusion criteria. Finally, eligible participants were invited for in-person clinical interviews. At the time of the current analysis, 539 participants had completed interviewers or were in progress. The analytic dataset included 245 participants that had data available for variables of interest (eg, Social Functioning Scale [SFS], Social Phobia Scale [SPS], Structured Interview for Psychosis-Risk Syndromes [SIPS] positive and negative scores, complete Structured Clinical Interview for DSM-5). All raters were advanced research assistants, doctoral students in clinical psychology, and postdoctoral fellows. To ensure accurate and consistent diagnoses across the study sites the following procedures were followed: (1) all clinical interviewers were SIPS certified at an official SIPS training, (2) diagnostic consensus phone meetings (with one senior rater from each site) were held to review interviews with clinical symptoms, and (3) if there were disagreements in consensus calls, cases were triaged to the PI meeting and the 3 PIs resolved disagreements (majority rule).34
Clinical Measures
During the MAP study Phase 1, the SPS37 and the SFS38 were administered online. The SPS is a 20-item self-report measure with questions pertaining to anxiety related to scrutiny and being observed by others. Each item is rated on how accurately the question characterizes the respondent on a scale of 0 (not at all) to 4 (extremely). The SPS is a reliable and valid measure of social anxiety symptoms.39 The SFS is a 79-item self-report measure designed to assess social functioning in schizophrenia. Items rate ability and performance related to social engagement, interpersonal contact, recreation, independence and competence in activities, and activities of daily living and employment.38 The SFS is a well-established measure within psychosis literature, demonstrates strong internal reliability and consistency, and is a sensitive measure of social functioning.38 The SFS is a measure designed for adults, and as such, the MAP study modified it to reflect impairments of the target adolescent/young adult demographic. Modifications consisted of excluding subscales assessing ability and performance of skills necessary for independent living (independence-competence and independence-performance subscales). Additionally, the occupation/employment subscale of the SFS may not be an appropriate scale for most high school or college-age samples and was adjusted to fit the adolescent/young adult sample. Subsequently, the scoring of this occupation/employment subscale was adapted to account for these changes. A higher total SFS score indicates better social functioning.
Phase 2 of the MAP study consisted of in-person interviews. Among these interviews, the SIPS40 and the Structured Clinical Interview for DSM-5, Research Version41 (SCID-5-RV) were used. The current study focused on the CHR group consisted of individuals meeting SIPS criteria for attenuated positive symptoms syndrome (APSS). This inclusion criteria included those identified as APSS persistent (CHR persistent; n = 44; symptom severity and frequency have remained stable over the past 12 months) or APSS progressive (CHR progressive; n = 37; attenuated symptoms have begun or worsened in severity and frequency within the past year). A chi-square analysis determined that there was no significant difference in the prevalence of SAD diagnosis between these subgroups, χ2 = 1.8, p = 0.18, and the categorical analyses in this study combined these subgroups into one single CHR group. The SIPS rates positive symptom severity on a 7-point Likert-type scale rated absent (0) to psychotic (6). For the current study, sum scores were used to quantify positive and negative symptoms. Participants at Phase 2 that did not meet the criteria for a CHR syndrome were considered part of the CC group (n = 164). The SCID-5-RV is a semi-structured interview used to assess the presence of major DSM-5 mental diagnoses.41 The SCID-5-RV has demonstrated moderate-to-strong reliability and is currently considered the “gold standard” of clinical diagnostic assessment. The study used the SCID-5-RV to assess the presence of a current diagnosis of SAD.
Statistical Approach
All analyses were estimated using R version 3.6.1.42 Independent samples t-tests and chi-square tests of independence were used to examine differences in age and gender between experimental groups. Chi-square tests were used to examine group differences in the prevalence of SAD diagnosis, other anxiety disorder diagnoses, and no anxiety-related diagnosis. Individuals with a SAD diagnosis only, as well as individuals with a SAD diagnosis and comorbid disorders, were included in the “SAD category.” The “other anxiety-related disorder” category included multiple anxiety-related diagnoses (ie, generalized anxiety disorder, specific phobia, agoraphobia, and panic disorder). The low frequency of each of these anxiety disorders warranted combining them into one group to most conservatively estimate the difference between other anxiety-related disorders and social anxiety in CHR and CC groups. Consistent with the rationale for a community sample comparison group, the “no anxiety-related diagnosis” category is not an artificially “clean” category, but rather identifies those who do not have any DSM-5 anxiety disorder, though these individuals may still have another non-anxiety diagnosis (see Supplemental table 1). A follow-up examination of the standardized residuals (ie, normalized residuals of the observed and expected frequencies in the omnibus chi-square test) was conducted to identify cells that significantly contributed to the chi-square value. In the current study, a large standardized residual (±2) indicated that more or less participants than expected by chance were part of a cell, and thus, significantly contributed to the omnibus chi-square result.43 Additionally, follow-up relative risk ratios44,45 were calculated46 (epiR). Relative risk ratios provide estimates of the likelihood of an outcome (SAD, other anxiety-related disorder, and no anxiety-related disorder) for an exposed group (CHR) relative to the likelihood of the outcome in the control group44,45(CC). Separate linear regression models42 were employed in two separate analyses to investigate the relationship between social anxiety symptom levels and positive and negative symptoms (lm base function). Next, to examine the relationship between social anxiety symptom severity and social functioning within the CHR group, linear models were used to examine the association between SAD symptom level and social functioning. Continuous social anxiety symptom severity was used in this analysis. Relatedly, the categorical diagnosis was also examined in relation to positive and negative symptoms and social functioning. In evaluating the pattern of missing data, the finalfit47 R packages were used. There were minimal missing data for the variables of interest (SAD diagnosis n = 0; SPS total n = 9; SIPS positive symptoms total n = 1; SIPS negative symptoms total n = 19, SFS total n = 14). Missing data were assessed for bias but were found to be missing completely at random, following no trends by group, sex, or age, as assessed by missing_pairs and missing_compare R functions.
Results
Demographics of the CHR and CC Samples
There were no significant differences between CHR (n = 81) and CC (n = 164) groups for gender, χ2(1) = 0.44, p = 0.50, age, t(137.51) = 1.52, p = 0.13, race, χ2(5) = 5.19, p = 0.39, or household income, χ2(17) = 19.76, p = 0.29. See table 1 for demographic information and Supplemental table 2 for household income, years of education completed, and current role information. Within the CHR group, there was no significant difference in age, t(137.51) = 1.52, p = 0.13, nor gender, χ2 = 0.44, p = 0.50, between CHR persistent and CHR progressive subgroups.
Table 1.
Demographic Variables and Current Diagnosis by Group with Standard Error of the Mean Reflected in Parentheses
| CHR | Community Controls | |
|---|---|---|
| N | 81 | 164 |
| Age Gender (% female) |
20.30 (2.01) 72% |
19.90 (1.70) 70% |
| Race (% of group) | ||
| Black or African American | 16.0% | 20.7% |
| Asian | 21.0% | 29.3% |
| American Indian or Alaskan | 0% | 1.2% |
| White | 54.3% | 42.7% |
| More than 1 race | 7.4% | 4.9% |
| Unknown | 1.2% | 1.2% |
| Diagnostic comorbidities (% of group) | ||
| Depression | 63% | 56% |
| Anxiety disorders | 83% | 42% |
| Bipolar disorder | 16% | 0% |
| Substance-related disorders | 38% | 0% |
| Feeding/eating-related disorders | 25% | 0% |
| Trauma-related disorders | 19% | 1% |
| Obsessive-compulsive disorders | 17% | 28% |
Note: CHR, clinical high-risk for psychosis.
Group Differences in the Prevalence of Social Anxiety and Other Anxiety Diagnoses
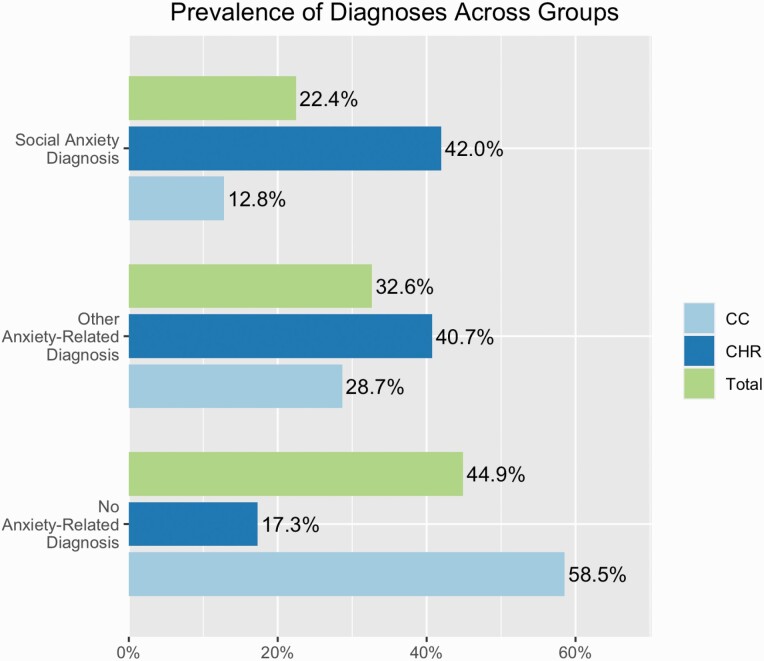
The prevalence of SAD diagnosis, other anxiety-related diagnoses, and no anxiety-related diagnoses was compared across CHR and CC groups using a 3 × 2 chi-square analysis. There was a significant difference in the prevalence of SAD, other anxiety-related diagnoses, and no anxiety-related diagnoses between CHR and CC groups, χ2(2) = 43.52, p < 0.001 (figure 1). Follow-up examination of the standardized residuals from the omnibus chi-square showed that significantly fewer participants in the CHR group than expected by chance had no anxiety-related diagnosis (Std. Residual = −2.9, p = 0.004), and significantly more than expected by chance had a SAD diagnosis (Std. Residual = 3.7, p < 0.001). In contrast, significantly more CC participants than expected by chance had no anxiety-related diagnosis (Std. Residual = 4.6, p < 0.001) and significantly fewer than expected by chance had a SAD diagnosis (Std. Residual = −2.6, p = 0.009). Follow-up risk ratios demonstrated that the CHR group, relative to CC, had an increased risk of having SAD by approximately 3-fold (RR = 3.30, 95% CI: 2.04–5.27, OR = 4.93). Additionally, the risk of having no anxiety-related diagnosis was 0.30 times less in the CHR group relative to CC (RR = 0.29, 95% CI: 0.18–0.48, OR = 0.15). Furthermore, the CHR group had approximately 1.4 times greater risk compared to the CC group (RR = 1.42, 95% CI: 1.00–2.03, OR = 1.71) of having another, non-SAD anxiety disorder. Supplemental table 1 provides the frequency of other anxiety-related disorders and no-anxiety-related diagnostic groups across CHR and CC groups. The increased risk of SAD in the CHR group, which was even greater than the relative risk of having another anxiety-related diagnosis, further supports subsequent analyses solely examining SAD’s relationship to subclinical psychotic symptoms and social function. Chi-square analyses were also conducted excluding individuals with comorbid diagnoses and including these individuals as their own group, and both demonstrated significant differences in base rates across CHR and CC groups (see Supplemental Materials [SM]).
Fig. 1.
Prevalence of clinical diagnoses. Bar plot reflects the percentage of clinical high-risk (CHR), community control (CC), and total participants (CHR + CC groups) in the sample that met SCID-5-RV criteria for social anxiety disorder, other anxiety, or no anxiety related diagnoses.
Group Differences in Levels of Social Anxiety Symptoms
Social anxiety symptoms were compared across CHR and CC groups in an independent sample t-test. CHR and CC groups differed in self-reported social anxiety, such that the CHR group exhibited increased symptoms of social anxiety (M = 31.70, SEM = 2.07) compared to the CC group (M = 20.50, SEM = 1.30), t(234) = 4.71, p < 0.001, d = 0.63.
Relationship Between Social Anxiety to Positive and Negative Symptom Severity
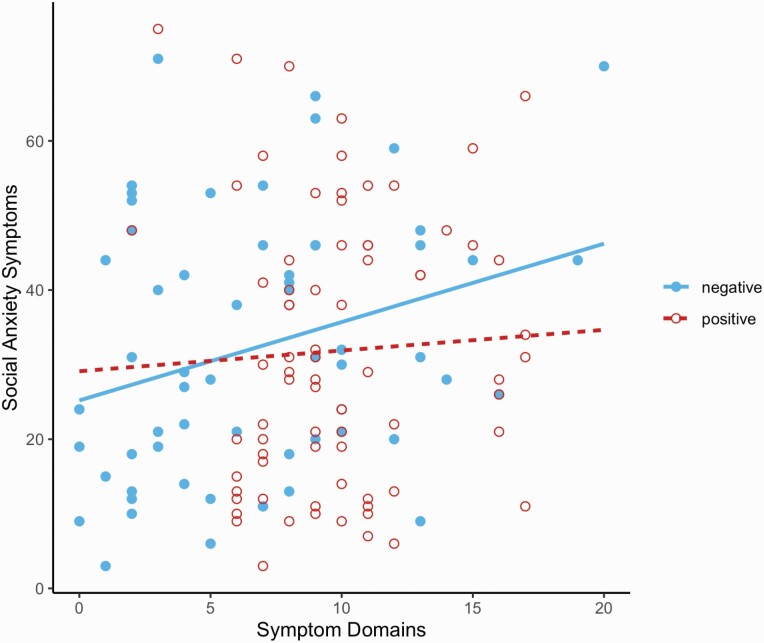
Two separate linear regression analyses examined the relationship of social anxiety symptoms to positive and negative symptoms in the CHR group, figure 2. Greater negative symptoms (total negative symptoms score) were related to greater social anxiety symptoms (total SPS score) among CHR participants, b = 1.05, t(57) = 2.28, r = 0.29, r2 =0.07, p = 0.03. Total positive symptoms score was not significantly related to the total SPS score, b = 0.28, t(74) = 0.43, r = 0.05, r2 = −0.01, p = 0.67, among the CHR group. Supplemental analyses examined this question with categorical diagnoses, and individuals who met DSM criteria for comorbid SAD had greater positive, but not negative, symptoms compared to those who did not (SM).
Fig. 2.
Social anxiety relates to negative symptoms. Results of linear modeling of the relationship between social anxiety symptoms and positive and negative symptoms in the CHR group. The graph demonstrates that negative symptom severity is positively associated with social anxiety symptom severity.
Functional Outcomes of Social Anxiety
To investigate the relationship between social anxiety and social functioning in the CHR group, linear modeling was employed. Social anxiety symptoms were negatively correlated with social functioning, b = −0.25, t(69) = −2.71, r =−0.31, r2 = 0.08, p = 0.008, demonstrating that increased symptoms of social anxiety were associated with decreased social functioning in the CHR group. Additionally, a supplemental analysis found that the CHR group had significantly lower social functioning compared to the CC group (SM). The related supplemental analysis also examined social functioning by categorical diagnoses within the CHR group only and found no significant difference between individuals in the CHR group by SAD diagnosis of SAD (SM).
Discussion
Individuals at CHR for psychosis showed approximately 3 times greater risk of having a SAD diagnosis relative to a heterogenous CC sample and showed a specific vulnerability to SAD. While the CHR group demonstrated an increased risk for both SAD and other anxiety-related diagnoses compared to the CC group, the risk of having a non-SAD anxiety diagnosis was approximately half of the relative risk of having a SAD diagnosis. Furthermore, the severity of social anxiety symptoms was related to both increased severity of negative symptoms and reduced social functioning among CHR individuals. Interestingly, social anxiety symptoms are related to negative and not positive symptoms. These results suggest that social anxiety is prevalent in people that meet the criteria for CHR syndrome and may be an important area of further study to address social difficulties and negative symptoms in those in the psychosis risk period. Collectively, these findings provide insight into the scope of social anxiety and its clinical and functional importance among CHR individuals, in particular, when compared to their peers in the general population.
Individuals at CHR for psychosis are at greater risk of having a comorbid SAD relative to their CC peers. Indeed, the relative risk of having comorbid SAD was greater than the risk of having another anxiety-related disorder in CHR individuals compared to their CC counterparts. The findings of the current study provide new evidence that SAD may be more common than other anxiety disorders in CHR individuals. Consistent with previous studies,13–15,17 approximately 42% of the CHR group met criteria for comorbid SAD; matching an estimate from a previous study16 exactly. By using a general community sample, the current study advances previous findings that CHR populations have an increased prevalence of social anxiety compared to their peers in two ways. First, the use of a general community sample reduces the bias in a traditionally nonpsychiatric sample toward lower rates of SAD.20,21 Second, as it is unlikely that we underestimated the rates of social anxiety in our control participants, we can be confident that the CHR group has a 3-fold greater risk of having social anxiety compared to community peers. This difference in prevalence suggests that social anxiety may be a critical area for future research to focus on the contribution of social anxiety to mechanisms of psychosis, treatment, and outcome.
Within the CHR group, social anxiety was also related to symptom severity for negative but not positive symptoms. This finding is consistent with results by McAusland et al.18 that report that social anxiety symptoms were related to negative symptoms. Additionally, work by Mazeh et al.6 demonstrated that avoidant cognitions within social anxiety were specifically associated with negative symptoms in patients with schizophrenia. However, it is also possible that social anxiety contributes to secondary negative symptoms in a primary/secondary negative symptom theoretical framework.48,49 This theory postulates that negative symptoms are considered primary if they are a direct result of psychosis but are considered secondary if they are driven by other mechanisms, such as social anxiety.49 For example, negative symptoms in CHR individuals, such as asociality, could be due to social anxiety and not a result of CHR syndromes. The current study provides support for the potential for social anxiety to be a treatment target for future investigation to improve negative symptom severity. To further clarify our understanding here, future studies should examine specific features of social anxiety (eg, avoidance and fear6) as well. In addition to symptoms, social anxiety was related to deficits in social function among those at CHR for psychosis. This finding was consistent with established results from previous literature that social anxiety and social functioning impairments were present in patients with a psychosis spectrum diagnosis22,50 and in CHR individuals.27
In a supplemental analysis, social functioning did not differ among CHR individuals with and without a comorbid SAD diagnosis. This categorical approach revealed a great deal of heterogeneity in social anxiety symptoms and social functioning by diagnosis, which masked a relationship between social anxiety symptoms and social functioning that were apparent when social anxiety symptoms were examined dimensionally (SM figure 1). Parallel supplemental analyses revealed that positive, but not negative, symptoms were greater in CHR individuals with a comorbid diagnosis of SAD. It is possible that positive symptoms are only related to social anxiety when the social anxiety levels are sufficiently high to meet diagnostic criteria, but warrants further investigation. This supplemental finding speaks to the differences between categorical diagnosis and subthreshold levels of social anxiety, as the relationship between negative symptoms and social anxiety was evident when social anxiety was measured using dimensional symptom level. Further, this result suggests that attenuated positive symptoms may be more relevant to diagnostically significant SAD. Additionally, there is a notable challenge of disentangling primary negative symptoms from those that are secondarily caused by other psychopathology, such as social anxiety. Collectively these supplemental findings highlight the benefit of examining social anxiety symptoms dimensionally and suggest that diagnostic heterogeneity may partially account for inconsistent findings in previous literature.
The current study advances the generalizability of previous findings and clarifies the complex nature of social functioning in the early identification of psychosis. Future studies should explore the potential for extant treatments targeted at social anxiety that might improve social functioning in individuals at risk for psychosis as a strategy to improve quality of life. Additionally, future studies should examine the impact of social anxiety on social support, as social support has direct implications for psychosis course.51 It is also noteworthy that psychosocial interventions, such as Cognitive Behavioral Therapy, are well-established treatments for social anxiety, thus improving social functioning.24,52,53 In conclusion, social anxiety reflects an opportunity for low-risk interventions that may increase social functioning.
Although this study has strength in its external validity, there are some notable limitations. First, the current study has no follow-up information that could provide insight into future clinical course and conversion to psychosis. Second, the study sample had a higher proportion of females, which was reflective of the larger MAP study from which these participants were recruited. Although there were no significant differences in the number of males and females across the experimental groups, social anxiety affects more women than men,16 with odds ratios ranging between 1.5 and 2.2.54 Therefore, females within each experimental group may be overestimating the true prevalence and severity in both the CHR and CC groups. However, it is noteworthy that the current recruitment approach differs from the typical help-seeking recruitment approach,34 meaning that traditional help-seeking samples may be more severe. The current study was limited to CHR individuals with persistent or progressive symptoms rather than those whose symptoms were improving. As such, prospective, longitudinal studies examining social anxiety in individuals whose symptoms have improved (APSS remission) may further shed light on complex relationships between psychosis-risk, anxiety, clinical course, and functioning. Due to the considerable comorbidity between depression and anxiety-related psychopathology, the current study was unable to meaningfully parse apart their individual relationship to psychosis-risk symptoms (SM) and warrants future investigation. A notable limitation of the current study, as well as the current literature broadly, is that there is no in-depth self-report measure of social functioning specifically designed for people at clinical high risk. This highlights the necessity to either develop measures catered to this clinical population or to validate existing measures that were developed for psychosis populations for use within CHR individuals. Additionally, the results of the current study could be extended by examining the relationship of social anxiety with specific domains of social functioning (eg, withdrawal/social engagement, prosocial behavior, and recreation).
Supplementary Material
Acknowledgments
We would like to thank the individuals who participated in the study and the multisite research team for their help with data collection and entry. Special thanks to Jadyn Park for assisting in collecting literature. The authors have declared that there are no conflicts of interest in relation to the subject of this study.
Funding
This work was supported by the National Institute of Mental Health (MH094650, MH112545, MH103231, MH094650 to VM; 5R01MH112613-03, 3R01MH112613-02S1, and 5R01MH112613-02 to LME; 5R01MH112612-03, 5R01MH112612-02, and 1R01MH112612-01).
References
- 1. Achim AM, Maziade M, Raymond E, Olivier D, Mérette C, Roy MA. How prevalent are anxiety disorders in schizophrenia? A meta-analysis and critical review on a significant association. Schizophr Bull. 2011;37(4):811–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Braga RJ, Reynolds GP, Siris SG. Anxiety comorbidity in schizophrenia. Psychiatry Res. 2013;210(1):1–7. [DOI] [PubMed] [Google Scholar]
- 3. Penn DL, Hope DA, Spaulding W, Kucera J. Social anxiety in schizophrenia. Schizophr Res. 1994;11(3):277–284. [DOI] [PubMed] [Google Scholar]
- 4. Pallanti S, Quercioli L, Hollander E. Social anxiety in outpatients with schizophrenia: a relevant cause of disability. Am J Psychiatry. 2004;161(1):53–58. [DOI] [PubMed] [Google Scholar]
- 5. Michail M, Birchwood M. Social anxiety disorder in first-episode psychosis: incidence, phenomenology and relationship with paranoia. Br J Psychiatry. 2009;195(3):234–241. [DOI] [PubMed] [Google Scholar]
- 6. Mazeh D, Bodner E, Weizman R, Delayahu Y, Cholostoy A, Martin T, Barak Y. Comorbid social phobia in schizophrenia. Int J Soc Psychiatry. 2009;55(3):198–202. [DOI] [PubMed] [Google Scholar]
- 7. Blanchard JJ, Mueser KT, Bellack AS. Anhedonia, positive and negative affect, and social functioning in schizophrenia. Schizophr Bull. 1998;24(3):413–424. [DOI] [PubMed] [Google Scholar]
- 8. Romm KL, Melle I, Thoresen C, Andreassen OA, Rossberg JI. Severe social anxiety in early psychosis is associated with poor premorbid functioning, depression, and reduced quality of life. Compr Psychiatry. 2012;53(5):434–440. [DOI] [PubMed] [Google Scholar]
- 9. Gumley A, O’grady M, Power K, Schwannauer M. Negative beliefs about self and illness: a comparison of individuals with psychosis with or without comorbid social anxiety disorder. Aust N Z J Psychiatry. 2004;38(11–12):960–964. [DOI] [PubMed] [Google Scholar]
- 10. Hooley JM, Parker HA. Measuring expressed emotion: an evaluation of the shortcuts. J Fam Psychol. 2006;20(3): 386–396. [DOI] [PubMed] [Google Scholar]
- 11. Stowkowy J, Colijn MA, Addington J. Pathways to care for those at clinical high risk of developing psychosis. Early Interv Psychiatry. 2013;7(1):80–83. [DOI] [PubMed] [Google Scholar]
- 12. Haidl TK, Rosen M, Ruhrmann S, Klosterkötter J. Social Anxiety in individuals with clinical high-risk state for psychosis. Fortschr Neurol Psychiatr. 2019;87(5):284–297. [DOI] [PubMed] [Google Scholar]
- 13. Woods SW, Addington J, Cadenhead KS, et al. Validity of the prodromal risk syndrome for first psychosis: findings from the North American Prodrome Longitudinal Study. Schizophr Bull. 2009;35(5):894–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Addington J, Cornblatt BA, Cadenhead KS, et al. At clinical high risk for psychosis: outcome for nonconverters. Am J Psychiatry. 2011;168(8):800–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Marshall C, Addington J, Epstein I, Liu L, Deighton S, Zipursky RB. Treating young individuals at clinical high risk for psychosis. Early Interv Psychiatry. 2012;6(1):60–68. [DOI] [PubMed] [Google Scholar]
- 16. Rietdijk J, Ising HK, Dragt S, et al. Depression and social anxiety in help-seeking patients with an ultra-high risk for developing psychosis. Psychiatry Res. 2013;209(3): 309–313. [DOI] [PubMed] [Google Scholar]
- 17. Fusar-Poli P, Nelson B, Valmaggia L, Yung AR, McGuire PK. Comorbid depressive and anxiety disorders in 509 individuals with an at-risk mental state: impact on psychopathology and transition to psychosis. Schizophr Bull. 2014;40(1): 120–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. McAusland L, Buchy L, Cadenhead KS, et al. Anxiety in youth at clinical high risk for psychosis. Early Interv Psychiatry. 2017;11(6):480–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Millman ZB, Gold JM, Mittal VA, Schiffman J. The critical need for help-seeking controls in clinical high-risk research. Clin Psychol Sci. 2019;7(6):1171–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Schiffman J, Ellman LM, Mittal VA. Individual differences and psychosis-risk screening: practical suggestions to improve the scope and quality of early identification. Front Psychiatry. 2019;10:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kendler KS. The super-normal control group in psychiatric genetics: possible artifactual evidence for coaggregation. Psychiatric Genetics. 1990;1:45–53. [Google Scholar]
- 22. Voges M, Addington J. The association between social anxiety and social functioning in first episode psychosis. Schizophr Res. 2005;76(2–3):287–292. [DOI] [PubMed] [Google Scholar]
- 23. Lysaker PH, Salyers MP. Anxiety symptoms in schizophrenia spectrum disorders: associations with social function, positive and negative symptoms, hope and trauma history. Acta Psychiatr Scand. 2007;116(4):290–298. [DOI] [PubMed] [Google Scholar]
- 24. Thompson E, Millman ZB, Okuzawa N, et al. Evidence-based early interventions for individuals at clinical high risk for psychosis: a review of treatment components. J Nerv Ment Dis. 2015;203(5):342–351. [DOI] [PubMed] [Google Scholar]
- 25. Hooley JM. Social factors in schizophrenia. Curr Dir Psychol Sci. 2010;19(4):238–242. [Google Scholar]
- 26. Robustelli BL, Newberry RE, Whisman MA, Mittal VA. Social relationships in young adults at ultra high risk for psychosis. Psychiatry Res. 2017;247:345–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Carrión RE, Goldberg TE, McLaughlin D, Auther AM, Correll CU, Cornblatt BA. Impact of neurocognition on social and role functioning in individuals at clinical high risk for psychosis. Am J Psychiatry. 2011;168(8):806–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cornblatt BA, Carrión RE, Addington J, et al. Risk factors for psychosis: impaired social and role functioning. Schizophr Bull. 2012;38(6):1247–1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hui C, Morcillo C, Russo DA, et al. Psychiatric morbidity, functioning and quality of life in young people at clinical high risk for psychosis. Schizophr Res. 2013;148(1–3):175–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Asher L, Zammit S, Sullivan S, Dorrington S, Heron J, Lewis G. The relationship between psychotic symptoms and social functioning in a non-clinical population of 12 year olds. Schizophr Res. 2013;150(2–3):404–409. [DOI] [PubMed] [Google Scholar]
- 31. Lee SJ, Kim KR, Lee SY, An SK. Impaired social and role function in ultra-high risk for psychosis and first-episode schizophrenia: its relations with negative symptoms. Psychiatry Investig. 2017;14(5):539–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Fusar-Poli P, Nelson B, Valmaggia L, Yung AR, McGuire PK. Comorbid depressive and anxiety disorders in 509 individuals with an at-risk mental state: impact on psychopathology and transition to psychosis. Schizophr Bull. 2014;40(1):120–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Madsen HK, Nordholm D, Krakauer K, Randers L, Nordentoft M. Psychopathology and social functioning of 42 subjects from a Danish ultra high-risk cohort. Early Interv Psychiatry. 2018;12(6):1181–1187. [DOI] [PubMed] [Google Scholar]
- 34. Ellman LM, Schiffman J, Mittal VA. Community psychosis risk screening: an instrument development investigation. J Psychiatry Brain Sci. 2020;5:e200019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Loewy RL, Bearden CE, Johnson JK, Raine A, Cannon TD. The prodromal questionnaire (PQ): preliminary validation of a self-report screening measure for prodromal and psychotic syndromes. Schizophr Res. 2005;79(1):117–125. [PubMed] [Google Scholar]
- 36. Miller TJ, Cicchetti D, Markovich PJ, McGlashan TH, Woods SW. The SIPS screen: a brief self-report screen to detect the schizophrenia prodrome. Schizophr Res. 2004;70:78–78. [Google Scholar]
- 37. Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behav Res Ther. 1998;36(4):455–470. [DOI] [PubMed] [Google Scholar]
- 38. Birchwood M, Smith J, Cochrane R, Wetton S, Copestake S. The Social Functioning Scale. The development and validation of a new scale of social adjustment for use in family intervention programmes with schizophrenic patients. Br J Psychiatry. 1990;157:853–859. [DOI] [PubMed] [Google Scholar]
- 39. Brown EJ, Turovsky J, Heimberg RG, Juster HR, Brown TA, Barlow DH. Validation of the Social Interaction Anxiety Scale and the Social Phobia Scale across the anxiety disorders. Psychol Assess. 1997;9(1):21. [Google Scholar]
- 40. Miller TJ, McGlashan TH, Rosen JL, et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull. 2003;29(4):703–715. [DOI] [PubMed] [Google Scholar]
- 41. First MB, Williams JBW, Karg RS, Spitzer RL.. Structured Clinical Interview for DSM-5—Research Version (SCID-5 for DSM-5, Research Version; SCID-5-RV). Arlington, VA: American Psychiatric Association; 2015:1–94. [Google Scholar]
- 42. R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2019. Retrieved from https://www.R-project.org—Regression results tables and plots when modelling. R package version 1.0.1. [Google Scholar]
- 43. Sharpe D. Chi-square test is statistically significant: now what? Pract Assess Res Eval. 2015;20(1):8. [Google Scholar]
- 44. Schmidt CO, Kohlmann T. When to use the odds ratio or the relative risk? Int J Public Health. 2008;53(3):165–167. [DOI] [PubMed] [Google Scholar]
- 45. Andrade C. Understanding relative risk, odds ratio, and related terms: as simple as it can get. J Clin Psychiatry. 2015;76(7):857–861. [DOI] [PubMed] [Google Scholar]
- 46. Stevenson M, Nunes T, Heuer C, Marshall J, Sanchez J, Thornton R, Reiczigel J, Robison-Cox J, Sebastiani P, Solymos P, Yoshida K, Jones G, Pirikahu S, Firestone S, Kyle R, Popp J, Jay M, Reynard C. epiR: Tools for the Analysis of Epidemiological Data. R Package Version 1.0-14; 2020. https://CRAN.R-project.org/package=epiR
- 47. Harrison E, Drake T, Riinu O. finalfit: Quickly Create Elegant Regression Results Tables and Plots When Modelling. R Package Version 1.0.1; 2020. https://CRAN.R-project.org/package=finalfit
- 48. Kirschner M, Aleman A, Kaiser S. Secondary negative symptoms—a review of mechanisms, assessment and treatment. Schizophr Res. 2017;186:29–38. [DOI] [PubMed] [Google Scholar]
- 49. Strauss GP, Cohen AS. A transdiagnostic review of negative symptom phenomenology and etiology. Schizophr Bull. 2017;43(4):712–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Chudleigh C, Naismith SL, Blaszczynski A, Hermens DF, Hodge MA, Hickie IB. How does social functioning in the early stages of psychosis relate to depression and social anxiety? Early Interv Psychiatry. 2011;5(3): 224–232. [DOI] [PubMed] [Google Scholar]
- 51. Norman RM, Malla AK, Manchanda R, Harricharan R, Takhar J, Northcott S. Social support and three-year symptom and admission outcomes for first episode psychosis. Schizophr Res. 2005;80(2-3):227–234. [DOI] [PubMed] [Google Scholar]
- 52. Gould RA, Buckminster S, Pollack MH, Otto MW, Massachusetts LY. Cognitive‐behavioral and pharmacological treatment for social phobia: a meta‐analysis. Clin Psychol Sci Pract. 1997;4(4):291–306. [Google Scholar]
- 53. Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry. 1996;153(3):321–330. [DOI] [PubMed] [Google Scholar]
- 54. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Washington, DC: American Psychiatric Pub; 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.