Abstract
We aimed to investigate whether comorbid musculoskeletal disorders (MSD)s and pain medication use was associated with in-hospital mortality among patients with coronavirus disease 2019 (COVID-19). Adult patients (≥20 years old) with a positive COVID-19 diagnosis until 5 June 2020 were included in this study, based on the National Health Insurance COVID-19 database in South Korea. MSDs included osteoarthritis, neck pain, lower back pain, rheumatoid arthritis, and others, while pain medication included paracetamol, gabapentin, pregabalin, glucocorticoid, nonsteroidal anti-inflammatory drugs (NSAIDs), opioids (strong and weak opioids), and benzodiazepine. Primary endpoint was in-hospital mortality. A total of 7713 patients with COVID-19 were included, and in-hospital mortality was observed in 248 (3.2%) patients. In multivariate logistic regression analysis, no MSDs (p > 0.05) were significantly associated with in-hospital mortality. However, in-hospital mortality was 12.73 times higher in users of strong opioids (odds ratio: 12.73, 95% confidence interval: 2.44–16.64; p = 0.002), while use of paracetamol (p = 0.973), gabapentin or pregabalin (p = 0.424), glucocorticoid (p = 0.673), NSAIDs (p = 0.979), weak opioids (p = 0.876), and benzodiazepine (p = 0.324) was not associated with in-hospital mortality. In South Korea, underlying MSDs were not associated with increased in-hospital mortality among patients with COVID-19. However, use of strong opioids was significantly associated with increased in-hospital mortality among the patients.
Keywords: analgesics, opioid, musculoskeletal diseases, pain, population
1. Introduction
The coronavirus disease 2019 (COVID-2019) was declared a pandemic by the World Health Organization on 11 March 2020 [1]. As of 6 April 2021, the global toll of COVID-19 cases was 131,699,808, and the number of deaths was 2,859,642 [2]. Although vaccine administration began on 8 December 2020 [3,4], limitations associated with the volume of vaccine production and the rapidity of administration hampered the attainment of herd immunity against COVID-19. Thus, the COVID-19 crisis remains the most serious global health issue in 2021.
Immune-mediated inflammation is the main mechanism of COVID-19 infection, known to be an important prognostic factor among patients who contracted the disease [5,6]. Further, due to impaired immune defences both from underlying disease and treatment, immunocompromised patients with respiratory virus infection are at risk of a more severe infection [7,8]. Immunocompromised patients with cancer and organ transplantation are known to have worse COVID-19 prognosis; however, the prognosis of other immunocompromised patients treated with biologics for chronic disease or those with acquired immune deficiency syndrome remains controversial [9].
As immune system dysregulation may play a role in chronic pain, and individuals with chronic musculoskeletal pain reportedly had abnormal immune responses [10], it might affect the prognosis of patients with COVID-19. Furthermore, pain medications such as opioids and glucocorticoids are known to cause immunosuppression if prescribed long-term [11,12,13]. Thus, long-term prescription of opioids or glucocorticoids is associated with increased mortality in a South Korean population [14,15]. Based on evidence of the immunosuppressive effects of long-term opioid use, the prognosis of long-term opioid users might worsen after COVID-19 [16]. However, information regarding the impact of chronic musculoskeletal disorders (MSD) or the use of pain medication on the prognosis of patients with COVID-19 remains unidentified.
We hypothesized that comorbid MSDs and use of pain medication might increase in-hospital mortality among patients with COVID-19. Therefore, we aimed to investigate this hypothesis in South Korea.
2. Materials and Methods
2.1. Study Design and Ethical Statement
This population-based cohort study was conducted according to the Reporting of Observational Studies in Epidemiology guidelines [17]. Deliberation of the study protocol was exempted by the Institutional Review Board (IRB) of Seoul National University Bundang Hospital (X-2004-604-905) and the National Health Insurance Service (NHIS) data sharing service (NHIS-2020-1-424). Informed consent was waived by the IRB, as the analyses were performed retrospectively using anonymized data derived from the South Korean NHIS database.
2.2. NHIS-COVID-19 Cohort Database and Study Population
The NHIS-COVID-19 cohort database was created in cooperation between The Korea Disease Control and Prevention Agency (KDCPA) and NHIS for medical research associated with the COVID-19 crisis in South Korea. The KDCPA provides data of individuals who were diagnosed with COVID-19 in the polymerase chain reaction (PCR) test from 1 January to 4 June 2020. Therefore, the database contains information on all patients with COVID-19 regardless of disease severity, which includes demographic information, date of diagnosis, and treatments results. However, the data from patients who were receiving ongoing in-hospital treatment were not included, as the treatment results were not determined at that time. As a sole public insurance system, all disease diagnoses of patients with COVID-19 from 2015 to 2020 were registered in the database using International Classification of Diseases (ICD)-10 codes. Additionally, all prescription information of drugs and/or procedures from 2015 to 2020 was also included.
For this study, we included individuals who received a positive COVID-19 diagnosis between 1 January 2020 to 4 June 2020 in South Korea, and individuals <20 years old were excluded from the analysis. In South Korea, patients with COVID-19 are admitted to the hospital only if they have severe symptoms such as pneumonia. However, if they have no symptoms or only mild symptoms, they are asked to isolate and are closely monitored in specific centres managed by the government.
2.3. Exposure Variables: Musculoskeletal Disease and Pain Medication
Osteoarthritis, neck pain, low back pain, rheumatoid arthritis, and other MSDs were defined as MSD in this study. A previous MSD diagnosis was evaluated using the ICD-10 codes of the NHIS database from 2015 to 2019 (data shown in Table S1). Additionally, instances of cancer, metastatic solid tumours, and major depressive symptoms were also included in the analysis, as they are closely related to the use of pain medication.
For pain-related medications, prescription data from 2019 to 2020 were extracted for drugs including paracetamol, gabapentin, pregabalin, glucocorticoids, nonsteroid anti-inflammatory drugs (NSAIDs), opioids (strong and weak opioids), and benzodiazepines. Considering the variability in opioid potency [18], codeine, dihydrocodeine, hydrocodone, and tramadol were categorized as weak opioids, and all others (e.g., fentanyl, morphine, oxycodone, hydromorphone, and methadone) were categorized as strong opioids. Pain medication users were defined as those prescribed a continuous drug supply over a period of ≥90 days from 2019 until the date of COVID-19 diagnosis. For example, an individual who was prescribed strong opioids, benzodiazepines, and gabapentin over a period of ≥90 days was classified as a user of strong opioids, benzodiazepines, and gabapentin in this study. Only patients who continuously took the drug within 1 month before the date of COVID-19 diagnosis by a PCR test were considered pain medication users. In South Korea, opioids, benzodiazepines, and gabapentin need to be prescribed by physicians; thus, there were no missing prescription data for these drugs. However, paracetamol and NSAIDs are available in convenience stores or the market without a prescription.
2.4. Endpoints
The primary endpoint of this study was in-hospital mortality among patients with COVID-19 in the NHIS-COVID-19 database, evaluated from 1 January 2020 to 27 August 2020. In-hospital mortality was defined as COVID-19-related deaths among patients with COVID-19. If a patient died after end of isolation, as the virus was no longer detected in the PCR test, it was not considered a COVID-related death.
2.5. Covariates
Some information was extracted as confounders for this study, which included demographic characteristics such as age and sex. The NHIS classified age into the following seven groups (categorical variable) to maintain anonymity in the database: 20–29, 30–39, 40–49, 50–59, 60–69, 70–79, and ≥80 years old groups. Annual income level in 2020 and place of residence were collected and used as confounders to reflect socio-economic status of the study participants. The place of residence was divided into the following five groups based on the COVID-19 cases until 4 June 2020: Seoul, Gyeonggi-do, Daegu, Gyeongsangbuk-do, and other areas. Comorbid status among the patients was reflected based on the underlying disability and the Charlson comorbidity index, calculated using the registered ICD-10 diagnostic codes (Table S2), from 1 January 2015 to 31 December 2019. In South Korea, the social welfare system requires all individuals with disabilities to be registered in the NHIS database to get various benefits. The disabilities were divided into six grades according to the severity, and we used two severity groups (1–3: severe disability; 4–6: mild-to-moderate disability).
2.6. Statistical Analysis
Baseline characteristics of the patients with COVID-19 are presented as mean values with standard deviations for continuous variables (Charlson comorbidity index) and numbers with percentages for categorical variables (all other variables). First, we performed univariate logistic regression analysis to identify the individual association of all variables with in-hospital mortality among patients with COVID-19 in South Korea. We then constructed a multivariate logistic regression model to identify the independent associations of all variables with in-hospital mortality among patients with COVID-19 in South Korea. In the multivariate model, all covariates were included for multivariate adjustment. No multicollinearity was observed in any multivariate model of the entire cohort, with a variance inflation factor <2.0. The results of the logistic regression analyses are presented as odds ratios (ORs) with 95% confidence intervals (CIs). R software (version 4.0.3; R Foundation for Statistical Computing, Vienna, Austria) and SAS software version 9.4 (SAS Institute Inc., Cary, NC, USA) were used for all analyses, and p < 0.05 was considered statistically significant.
3. Results
3.1. Study Population
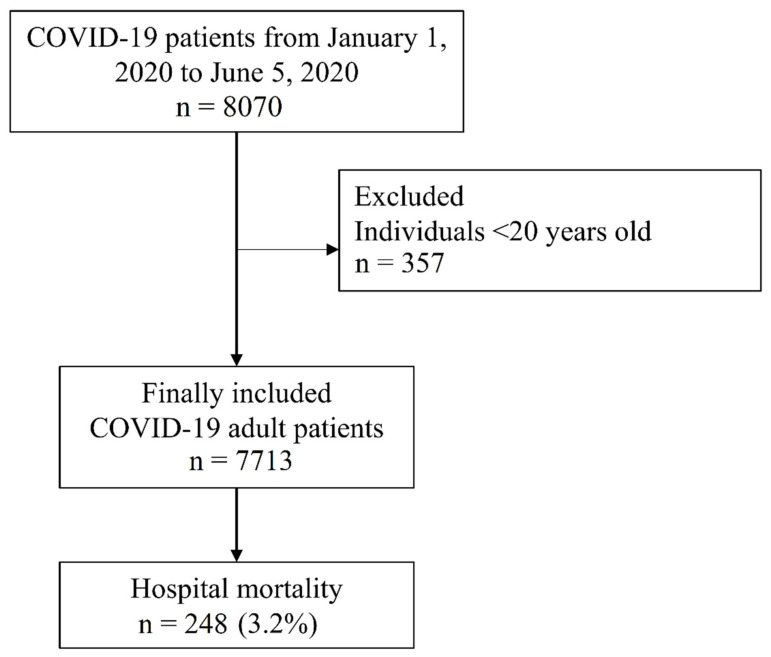
The NHIS-COVID-19 database included 8070 patients with COVID-19. Among them, 357 individuals aged <20 years old were excluded from the analysis. Finally, 7713 patients with COVID-19 were included. From these patients, 216 (3.0%) were admitted to the intensive care unit, 127 (1.8%) received mechanical ventilation, and 21 (0.3%) received extracorporeal membrane oxygenation. Finally, in-hospital mortality was observed in 248 (3.2%) patients (Figure 1). Baseline characteristics of the patients with COVID-19 are presented in Table 1. There were 3641 (47.2%) patients with osteoarthritis, 1971 (25.6%) with neck pain, 4836 (62.7%) with lower back pain, 739 (9.6%) with rheumatoid arthritis, and 4908 (63.6%) had other MSDs. Among pain medications, 58 (0.8%) patients used paracetamol, 148 (1.9%) used gabapentin or pregabalin, 63 (0.8%) used glucocorticoid, one (0.0%) used NSAIDs, nine (0.1%) used strong opioids, 240 (3.1%) used weak opioids, and 259 (3.4%) used benzodiazepine. The nine patients with chronic strong opioid use included three patients with cancer and six patients with chronic MSD.
Figure 1.
Flow chart depicting selection of patients with COVID-19 in South Korea. COVID-19, coronavirus disease 2019.
Table 1.
Baseline characteristic of COVID-19 patients in South Korea (n = 7713).
| Variable | Number (%) | Mean (SD) |
|---|---|---|
| Sex, male | 3048 (39.5%) | |
| Age | ||
| 20–29 | 2057 (26.7%) | |
| 30–39 | 832 (10.8%) | |
| 40–49 | 1036 (13.4%) | |
| 50–59 | 1567 (20.3%) | |
| 60–69 | 1199 (15.5%) | |
| 70–79 | 617 (8.0%) | |
| ≥80 | 405 (5.3%) | |
| Income in qurtile | ||
| Q1 (Lowest) | 2439 (31.6%) | |
| Q2 | 1445 (18.7%) | |
| Q3 | 1577 (20.4%) | |
| Q4 (Highest) | 2135 (27.7%) | |
| unknown | 117 (1.5%) | |
| Underlying disability | ||
| Mild degree | 318 (4.1%) | |
| Moderate to severe degree | 293 (3.8%) | |
| Residence | ||
| Seoul | 510 (6.6%) | |
| Gyeonggi-do | 431 (5.6%) | |
| Daegu | 5036 (65.3%) | |
| Gyeongsangbukdo | 933 (12.1%) | |
| Other area | 803 (10.4%) | |
| Charlson comorbidity index | 2.7 (2.7) | |
| Any cancer | 602 (7.8%) | |
| 70 (0.9%) | ||
| Metastatic solid tumour | 3641 (47.2%) | |
| Neck pain | 1971 (25.6%) | |
| Lower back pain | 4836 (62.7%) | |
| Rheumatoid arthritis | 739 (9.6%) | |
| Other musculoskeletal disease | 4908 (63.6%) | |
| Major depressive disorder | 1450 (18.8) | |
| Pain medication | ||
| Paracetamol | 58 (0.8%) | |
| Gabapentin or pregabalin | 148 (1.9%) | |
| Glucocorticoid | 63 (0.8%) | |
| NSAIDs | 1 (0.0%) | |
| Strong opoioid | 9 (0.1%) | |
| Weak opioid | 240 (3.1%) | |
| Benzodiazepine | 259 (3.4%) |
Presented as mean with standard deviation or number with percentage. COVID-19, coronavirus disease 2019; SD, standard deviation; NSAIDs, non-steroidal anti-inflammatory drugs.
3.2. In-Hospital Mortality among Patients with COVID-19
Table 2 and Table 3 show the results of univariate and multivariate logistic regression analysis for in-hospital mortality among patients with COVID-19. In the multivariate model, osteoarthritis (OR: 1.11, 95% CI: 0.75–1.65; p = 0.589), neck pain (OR: 0.74, 95% CI: 0.52–1.05; p = 0.095), lower back pain (OR: 0.73, 95% CI: 0.49–1.10; p = 0.133), rheumatoid arthritis (OR: 0.78, 95% CI: 0.50–1.23; p = 0.291), and other MSDs (OR: 0.73, 95% CI: 0.49–1.09; p = 0.129) were not associated with in-hospital mortality.
Table 2.
Univariate logistic regression analysis for in-hospital mortality among COVID-19 patients in South Korea.
| Variable | Univariate Analysis | p-Value |
|---|---|---|
| OR (95% CI) | ||
| Age, 10 year increase | 3.56 (3.13, 4.05) | <0.001 |
| Sex, male (vs. female) | 1.90 (1.47, 2.45) | <0.001 |
| Annual income level in 2020 | ||
| Q1 (Lowest) | 1 | |
| Q2 | 0.63 (0.42, 0.95) | 0.026 |
| Q3 | 0.87 (0.61, 1.25) | 0.446 |
| Q4 (Highest) | 1.08 (0.79, 1.47) | 0.636 |
| Unknown | 0.73 (0.23, 2.34) | 0.595 |
| Residence at 2010 | ||
| Seoul | 1 | |
| Gyeonggi-do | 5.19 (1.73, 15.56) | 0.003 |
| Daegu | 3.94 (1.45, 10.67) | 0.007 |
| Gyeongsangbukdo | 7.92 (2.86, 21.99) | <0.001 |
| Other area | 3.23 (1.10, 9.51) | 0.033 |
| Underlying disability | ||
| Mild degree (vs. no disability) | 5.05 (3.46, 7.37) | <0.001 |
| Moderate to severe (vs. no disability) | 5.72 (3.93, 8.33) | <0.001 |
| Charlson comorbidity index, 1 point increase | 1.40 (1.35, 1.45) | <0.001 |
| Any cancer | 3.70 (2.71, 5.04) | <0.001 |
| Metastatic solid tumour | 4.57 (2.24, 9.31) | <0.001 |
| Major depressive disorder | 4.18 (3.23, 5.40) | <0.001 |
| Osteoarthritis | 3.26 (2.45, 4.35) | <0.001 |
| Neck pain | 0.99 (0.74, 1.33) | 0.956 |
| Lower back pain | 1.94 (1.44, 2.61) | <0.001 |
| Rheumatoid arthritis | 1.69 (1.18, 2.42) | 0.004 |
| Other musculoskeletal disease | 1.63 (1.23, 2.18) | <0.001 |
| Pain medication | ||
| Paracetamol | 0.99 (0.35, 2.52) | 0.921 |
| Gabapentin or pregabalin | 4.42 (2.65, 7.35) | <0.001 |
| Glucocorticoid | 2.63 (1.04, 6.61) | 0.040 |
| NSAIDs | 0.00 (0.00-) | 0.978 |
| Strong opoioid | 38.38 (10.24, 143.81) | <0.001 |
| Weak opioid | 3.06 (1.92, 4.88) | <0.001 |
| Benzodiazepine | 3.64 (2.37, 5.57) | <0.001 |
COVID-19, coronavirus disease 2019; OR, odds ratio; CI, confidence interval; NSAIDs, non-steroidal anti-inflammatory drugs.
Table 3.
Multivariate logistic regression analysis for in-hospital mortality among COVID-19 patients in South Korea.
| Variable | Multivariate Model | p-Value |
|---|---|---|
| OR (95% CI) | ||
| Age, 10 year increase | 3.21 (2.75, 3.75) | <0.001 |
| Sex, male (vs. female) | 2.13 (1.57, 2.88) | <0.001 |
| Annual income level in 2020 | ||
| Q1 (Lowest) | 1 | |
| Q2 | 1.11 (0.69, 1.79) | 0.666 |
| Q3 | 1.01 (0.67, 1.54) | 0.949 |
| Q4 (Highest) | 0.86 (0.59, 1.24) | 0.411 |
| Unknown | 0.82 (0.22, 3.10) | 0.773 |
| Residence at 2010 | ||
| Seoul | 1 | |
| Gyeonggi-do | 2.82 (0.83, 9.54) | 0.096 |
| Daegu | 1.76 (0.59, 5.20) | 0.308 |
| Gyeongsangbookdo | 2.08 (0.68, 6.37) | 0.199 |
| Other area | 2.34 (0.72, 7.61) | 0.157 |
| Underlying disability | ||
| Mild degree (vs. no disability) | 0.91 (0.59, 1.40) | 0.653 |
| Moderate to severe (vs. no disability) | 2.88 (1.81, 4.60) | <0.001 |
| Charlson comorbidity index, 1 point increase | 1.19 (1.12, 1.26) | <0.001 |
| Any cancer | 1.00 (0.66, 1.52) | 0.986 |
| Metastatic solid tumour | 0.79 (0.27, 2.31) | 0.665 |
| Major depressive disorder | 1.28 (0.93, 1.76) | 0.125 |
| Osteoarthritis | 1.11 (0.75, 1.65) | 0.589 |
| Neck pain | 0.74 (0.52, 1.05) | 0.095 |
| Lower back pain | 0.73 (0.49, 1.10) | 0.133 |
| Rheumatoid arthritis | 0.78 (0.50, 1.23) | 0.291 |
| Other musculoskeletal disease | 0.73 (0.49, 1.09) | 0.129 |
| Pain medication | ||
| Paracetamol | 0.98 (0.37, 2.62) | 0.973 |
| Gabapentin or pregabalin | 0.77 (0.41, 1.45) | 0.424 |
| Glucocorticoid | 1.26 (0.43, 3.63) | 0.673 |
| NSAIDs | 0.00 (0.00-) | 0.979 |
| Strong opoioid | 12.73 (2.44, 16.64) | 0.002 |
| Weak opioid | 0.96 (0.55, 1.67) | 0.876 |
| Benzodiazepine | 0.77 (0.46, 1.29) | 0.324 |
Variables with statistical significance are presented in bold font. COVID-19, coronavirus disease-2019; OR, odds ratio; CI, confidence interval; NSAIDs, non-steroidal anti-inflammatory drugs.
However, regarding pain medications, in-hospital mortality was 12.73 times higher for users of strong opioids (OR: 12.73, 95% CI: 2.44–16.64; p = 0.002). In contrast, compared with that for other patients, in-hospital mortality was not significantly high for users of paracetamol (OR: 0.98, 95% CI: 0.37–2.62; p = 0.973), gabapentin or pregabalin (OR: 0.77, 95% CI: 0.41–1.45; p = 0.424), glucocorticoid (OR: 1.26, 95% CI: 0.43–3.63; p = 0.673), NSAIDs (OR: 0.00, 95% CI: 0.00-; p = 0.979), weak opioids (OR: 0.96, 95% CI: 0.55–1.67; p = 0.876), and benzodiazepines (OR: 0.77, 95% CI: 0.46–1.29; p = 0.324).
4. Discussion
This population-based cohort study using the NHIS-COVID-19 database showed that MSDs were not associated with increased in-hospital mortality in patients with COVID-19 compared to those without MSDs. Further, use of strong opioids was associated with higher in-hospital mortality among patients with COVID-19 compared to non-users, while use of other pain medications (paracetamol, gabapentin, pregabalin, glucocorticoids, NSAIDs, weak opioids, and benzodiazepines) was not significantly associated with in-hospital mortality. Our results suggest that comorbid MSDs and use of pain medication, except for strong opioids, do not worsen the prognosis of patients with COVID-19, at least in South Korea.
Although most pain medications were not associated with in-hospital mortality, strong opioids showed a significant association with in-hospital mortality. This could be attributed to the immunosuppression caused by chronic strong opioid use [16]. However, there might be an indication bias in terms of long-term opioid prescription [19], because long-term strong opioid users are more commonly elderly individuals with more comorbidities, who are more likely to develop severe COVID-19 and die. Thus, in addition to long-term strong opioid use, the patients’ age and comorbid status possibly affected the results. It should also be noted that there were only nine long-term strong opioid users, and their OR was 12.73 (95% CI: 2.44–16.44). Thus, the number of strong opioid users was not adequate for estimating OR for in-hospital mortality, and this sparsity bias possibly affected the results [20]. Accordingly, the result regarding the association of strong opioid use with in-hospital mortality should be interpreted with caution and validated in further studies with larger samples.
The association between opioid use and increased mortality was reported in the United States [21,22], the United Kingdom [23], and South Korea [14]. A recent study reported that opioid use was closely related to the growing trend of infectious diseases in the United States, and opioid use created a converging public health crisis with a significant combined impact on morbidity and mortality with regard to infection [24]. Additionally, a recent nationwide cohort study in the United States on hospitalized patients with serious infection showed that underlying opioid use disorder was linked to poorer hospital outcomes [25]. Another prospective cohort study reported the association between higher all-cause mortality and long-term opioid prescription among both human immunodeficiency virus-infected and uninfected individuals [26].
With respect to the relationship between opioid use and COVID-19 outcomes, the biological plausibility of a correlation between opioid use disorder and worse COVID-19 outcomes was suggested in July 2020 [27]. In September 2020, Wang et al. reported that substance disorders, including opioid use disorder, were associated with increased mortality among patients with COVID-19 in the United States [28]. However, there were some differences between the study by Wang et al. and ours. First, Wang et al. used just age, sex, race, and insurance type for adjustment as covariates, whereas we included numerous covariates that might be closely related to opioid use, such as Charlson comorbidity index, MSD, depression, and various pain medications, including benzodiazepines. Second, we focused on long-term opioid users instead of individuals with opioid use disorder, suggesting that the users of strong opioids in our study were appropriately prescribed medication by physicians for pain management. Considering all of the above, our results should be interpreted carefully. Furthermore, in addition to individuals with opioid use disorder, the risk of mortality in normal strong opioid users might be increased among patients with COVID-19. Recent reports emphasized the importance of prevention of opioid use disorder during the COVID-19 pandemic, as primary care physicians had to prescribe larger opioid doses for longer periods or prescribe remotely to maintain physical distancing [29,30]. Therefore, the results of our study also suggest that prevention and management among opioid users are important during the COVID-19 pandemic.
The impact of MSDs on in-hospital mortality among patients with COVID-19 remains unclear. In a single-centre retrospective cohort study, Fredi et al. reported that older age and comorbidities are associated with poorer outcomes among patients with rheumatic and musculoskeletal diseases [31]. In another prospective cohort study, COVID-19 outcomes were worse in patients with underlying inflammatory arthritis who were receiving glucocorticoids [32]. However, no previous studies evaluated whether MSDs might be a risk factor for poorer prognosis among patients with COVID-19 compared to the general population [31,32]. MSDs are critical conditions for human function, impairing mobility, dexterity, and the ability to work and actively participate in all aspects of life [33]. Based on our initial findings on the associations of MSDs with in-hospital mortality among patients with COVID-19 in South Korea and the aforementioned studies, the impact of MSDs on COVID-19 prognosis should be further evaluated.
This study has some limitations. First, some important variables, including body mass index and lifestyle factors such as history of smoking and alcohol consumption, were not included in the analysis, as they were not available in the NHIS-COVID-19 database. Second, we defined comorbidities using ICD-10 codes. However, the diseases specified by the ICD-10 codes may differ from the actual underlying diseases in our study population. Third, because NSAIDs and paracetamol are available in convenience stores or the market without a prescription in South Korea, there could be missing cases involving use of these drugs in our database, and the association of NSAIDs and paracetamol use with in-hospital mortality should be interpretated with caution. Fourth, despite our recent cohort study reporting the prevalence of users of strong opioids in 2015 as 0.24% [14], the proportion of users of strong opioids in our study was as low as 0.1% (9 of 7713). Due to this very low proportion in our study, the validity of our results might be controversial. Finally, as mentioned above, the indication bias and the sparsity data bias possibly affected the results regarding the association of strong opioid use with in-hospital mortality.
5. Conclusions
Conclusively, in South Korea, underlying MSDs were not associated with increased in-hospital mortality among patients with COVID-19. However, strong opioid use was associated with higher in-hospital mortality among patients with COVID-19, whereas use of other pain medications (paracetamol, gabapentin, pregabalin, glucocorticoids, NSAIDs, weak opioid, and benzodiazepine) did not show a significant association with in-hospital mortality.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijerph18136804/s1, Table S1: ICD-10 codes and Table S2: The ICD-10 codes used by comorbidity to compute the Charlson comorbidity index.
Author Contributions
Conceptualization, T.-K.O.; methodology, Y.-T.J. and W.E.; formal analysis, T.-K.O.; investigation, T.-K.O., W.E., and I.-A.S.; resources, Y.-T.J. and J.L.; data curation, Y.-T.J. and J.L.; writing—original draft preparation, T.-K.O. and I.-A.S.; writing—review and editing, Y.-T.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Deliberation of the study protocol was exempted by the Institutional Review Board (IRB) of Seoul National University Bundang Hospital (X-2004-604-905) and the National Health Insurance Service (NHIS) data sharing service (NHIS-2020-1-424).
Informed Consent Statement
Informed consent was waived by the IRB, as the analyses were performed retrospectively using anonymized data derived from the South Korean NHIS database.
Data Availability Statement
Data will be available upon reasonable request to the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bedford J., Enria D., Giesecke J., Heymann D.L., Ihekweazu C., Kobinger G., Lane H.C., Memish Z., Oh M.D., Schuchat A., et al. COVID-19: Towards controlling of a pandemic. Lancet. 2020;395:1015–1018. doi: 10.1016/S0140-6736(20)30673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coronavirus Research Center Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Global Map of Cases and Deaths by Country/Region/Sovereignty. [(accessed on 6 April 2021)];2020 Available online: https://coronavirus.jhu.edu/map.html.
- 3.Dagan N., Barda N., Kepten E., Miron O., Perchik S., Katz M.A., Hernán M.A., Lipsitch M., Reis B., Balicer R.D. BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Mass Vaccination Setting. N. Engl. J. Med. 2021;384:1412–1423. doi: 10.1056/NEJMoa2101765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knoll M.D., Wonodi C. Oxford–AstraZeneca COVID-19 vaccine efficacy. Lancet. 2021;397:72–74. doi: 10.1016/S0140-6736(20)32623-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haberman R., Axelrad J., Chen A., Castillo R., Yan D., Izmirly P., Neimann A., Adhikari S., Hudesman D., Scher J.U. Covid-19 in Immune-Mediated Inflammatory Diseases—Case Series from New York. N. Engl. J. Med. 2020;383:85–88. doi: 10.1056/NEJMc2009567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shi Y., Wang Y., Shao C., Huang J., Gan J., Huang X., Bucci E., Piacentini M., Ippolito G., Melino G. COVID-19 infection: The perspectives on immune responses. Cell Death Differ. 2020;27:1451–1454. doi: 10.1038/s41418-020-0530-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manuel O., Estabrook M., The American Society of Transplantation Infectious Diseases Community of Practice RNA respiratory viral infections in solid organ transplant recipients: Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin. Transplant. 2019;33:e13511. doi: 10.1111/ctr.13511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Waghmare A., Englund J.A., Boeckh M. How I treat respiratory viral infections in the setting of intensive chemotherapy or hematopoietic cell transplantation. Blood. 2016;127:2682–2692. doi: 10.1182/blood-2016-01-634873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fung M., Babik J.M. COVID-19 in Immunocompromised Hosts: What We Know So Far. Clin. Infect. Dis. 2021;72:340–350. doi: 10.1093/cid/ciaa863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Generaal E., Vogelzangs N., Macfarlane G., Geenen R., Smit J.H., Dekker J., Penninx B.W. Basal inflammation and innate immune response in chronic multisite musculoskeletal pain. Pain. 2014;155:1605–1612. doi: 10.1016/j.pain.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 11.Wolfe F., Caplan L., Michaud K. Treatment for rheumatoid arthritis and the risk of hospitalization for pneumonia: Associations with prednisone, disease-modifying antirheumatic drugs, and anti-tumor necrosis factor therapy. Arthritis Rheum. 2006;54:628–634. doi: 10.1002/art.21568. [DOI] [PubMed] [Google Scholar]
- 12.Flint T.R., Janowitz T., Connell C.M., Roberts E.W., Denton A., Coll A.P., Jodrell D.I., Fearon D.T. Tumor-Induced IL-6 Reprograms Host Metabolism to Suppress Anti-tumor Immunity. Cell Metab. 2016;24:672–684. doi: 10.1016/j.cmet.2016.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Diasso P.D.K., Birke H., Nielsen S.D., Main K.M., Højsted J., Sjøgren P., Kurita G.P. The effects of long-term opioid treatment on the immune system in chronic non-cancer pain patients: A systematic review. Eur. J. Pain. 2019;24:481–496. doi: 10.1002/ejp.1506. [DOI] [PubMed] [Google Scholar]
- 14.Oh T.K., Jeon Y.-T., Choi J.W. Trends in chronic opioid use and association with five-year survival in South Korea: A population-based cohort study. Br. J. Anaesth. 2019;123:655–663. doi: 10.1016/j.bja.2019.08.012. [DOI] [PubMed] [Google Scholar]
- 15.Oh T.K., Song I.-A. Trends in long-term glucocorticoid use and risk of 5-year mortality: A historical cohort study in South Korea. Endocrine. 2020;69:634–641. doi: 10.1007/s12020-020-02382-6. [DOI] [PubMed] [Google Scholar]
- 16.Shah B.R., Kuo Y.-F., Baillargeon J., Raji M.A. The impact of long-term opioid use on the risk and severity of COVID-19. J. Opioid Manag. 2020;16:401–404. doi: 10.5055/jom.2020.0597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P., STROBE Initiative The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Ann. Intern. Med. 2007;147:573–577. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- 18.Pereira J., Lawlor P., Vigano A., Dorgan M., Bruera E. Equianalgesic Dose Ratios for Opioids: A Critical Review and Proposals for Long-Term Dosing. J. Pain Symptom Manag. 2001;22:672–687. doi: 10.1016/S0885-3924(01)00294-9. [DOI] [PubMed] [Google Scholar]
- 19.Salas M., Hotman A., Stricker B.H. Confounding by Indication: An Example of Variation in the Use of Epidemiologic Terminology. Am. J. Epidemiol. 1999;149:981–983. doi: 10.1093/oxfordjournals.aje.a009758. [DOI] [PubMed] [Google Scholar]
- 20.Greenland S., Mansournia M.A., Altman D.G. Sparse data bias: A problem hiding in plain sight. BMJ. 2016;352:i1981. doi: 10.1136/bmj.i1981. [DOI] [PubMed] [Google Scholar]
- 21.Ray W.A., Chung C.P., Murray K.T., Hall K., Stein C.M. Prescription of Long-Acting Opioids and Mortality in Patients with Chronic Noncancer Pain. JAMA. 2016;315:2415–2423. doi: 10.1001/jama.2016.7789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gomes T., Tadrous M., Mamdani M.M., Paterson J.M., Juurlink D.N. The Burden of Opioid-Related Mortality in the United States. JAMA Netw. Open. 2018;1:e180217. doi: 10.1001/jamanetworkopen.2018.0217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pierce M., Bird S.M., Hickman M., Millar T. National record linkage study of mortality for a large cohort of opioid users ascertained by drug treatment or criminal justice sources in England, 2005–2009. Drug Alcohol Depend. 2015;146:17–23. doi: 10.1016/j.drugalcdep.2014.09.782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schwetz T.A., Calder T., Rosenthal E., Kattakuzhy S., Fauci A.S. Opioids and Infectious Diseases: A Converging Public Health Crisis. J. Infect. Dis. 2019;220:346–349. doi: 10.1093/infdis/jiz133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim J.-H., Fine D.R., Li L., Kimmel S.D., Ngo L.H., Suzuki J., Price C.N., Ronan M.V., Herzig S.J. Disparities in United States hospitalizations for serious infections in patients with and without opioid use disorder: A nationwide observational study. PLoS Med. 2020;17:e1003247. doi: 10.1371/journal.pmed.1003247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weisberg D.F., Gordon K.S., Barry D.T., Becker W.C., Crystal S., Edelman E.J., Gaither J., Gordon A.J., Goulet J., Kerns R.D., et al. Long-term Prescription of Opioids and/or Benzodiazepines and Mortality Among HIV-Infected and Uninfected Patients. J. Acquir. Immune Defic. Syndr. 2015;69:223–233. doi: 10.1097/QAI.0000000000000591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schimmel J., Manini A.F. Opioid Use Disorder and COVID-19: Biological Plausibility for Worsened Outcomes. Subst. Use Misuse. 2020;55:1900–1901. doi: 10.1080/10826084.2020.1791184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang Q.Q., Kaelber D.C., Xu R., Volkow N.D. COVID-19 risk and outcomes in patients with substance use disorders: Analyses from electronic health records in the United States. Mol. Psychiatry. 2021;26:30–39. doi: 10.1038/s41380-020-00880-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.MacKinnon L., Socías M.E., Bardwell G. COVID-19 and overdose prevention: Challenges and opportunities for clinical practice in housing settings. J. Subst. Abus Treat. 2020;119:108153. doi: 10.1016/j.jsat.2020.108153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wilson C.G., Ramage M., Fagan E.B. A Primary Care Response to COVID-19 for Patients with an Opioid Use Disorder. J. Rural. Heal. 2021;37:169–171. doi: 10.1111/jrh.12438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fredi M., Cavazzana I., Moschetti L., Andreoli L., Franceschini F., Airò P., Bazzani C., Crisafulli F., Filippini M., Frassi M., et al. COVID-19 in patients with rheumatic diseases in northern Italy: A single-centre observational and case–control study. Lancet Rheumatol. 2020;2:e549–e556. doi: 10.1016/S2665-9913(20)30169-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haberman R.H., Castillo R., Chen A., Yan D., Ramirez D., Sekar V., Lesser R., Solomon G., Neimann A.L., Blank R.B., et al. COVID-19 in Patients with Inflammatory Arthritis: A Prospective Study on the Effects of Comorbidities and Disease-Modifying Antirheumatic Drugs on Clinical Outcomes. Arthritis Rheumatol. 2020;72:1981–1989. doi: 10.1002/art.41456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Briggs A.M., Woolf A.D., Dreinhöfer K., Homb N., Hoy D.G., Kopansky-Giles D., Åkesson K., March L. Reducing the global burden of musculoskeletal conditions. Bull. World Heal. Organ. 2018;96:366–368. doi: 10.2471/BLT.17.204891. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be available upon reasonable request to the corresponding author.