Key Points
Question
Do cognitive behavioral group therapy (CBGT) and mindfulness-based stress reduction (MBSR) produce distinct brain and behavioral effects during cognitive reappraisal and acceptance regulation in adults with social anxiety disorder?
Findings
In this randomized clinical trial including 108 adult participants diagnosed with social anxiety disorder, CBGT and MBSR yielded overlapping and distinct cortical responses in a priori–defined regions of interest for reappraisal and acceptance regulation. Changes in blood oxygen level–dependent functional magnetic resonance imaging during reappraisal and acceptance were associated with reduced social anxiety symptoms 1 year post-CBGT but not 1 year post-MBSR.
Meaning
CBGT and MBSR may reduce clinical symptoms in patients with social anxiety disorder via enhancing reappraisal and acceptance emotion-regulation brain circuitry.
This randomized clinical trial investigates the effects of cognitive behavioral group therapy and mindfulness-based stress reduction on reappraisal and acceptance in patients with social anxiety disorder and tests whether treatment-associated brain changes are associated with social anxiety symptoms 1 year posttreatment.
Abstract
Importance
Cognitive behavioral group therapy (CBGT) and mindfulness-based stress reduction (MBSR) are thought to help patients with social anxiety disorder (SAD) via distinct emotion-regulation mechanisms. However, no study has compared the effects of CBGT and MBSR on brain and negative emotion indicators of cognitive reappraisal and acceptance in patients with SAD.
Objective
To investigate the effects of CBGT and MBSR on reappraisal and acceptance in patients with SAD and to test whether treatment-associated brain changes are associated with social anxiety symptoms 1 year posttreatment.
Design, Setting, and Participants
In this randomized clinical trial, a total of 108 unmedicated adults diagnosed with generalized SAD were randomly assigned to 12 weeks of CBGT, MBSR, or waitlist. The final sample included 31 patients receiving CBGT, 32 patients receiving MBSR, and 32 waitlist patients. Data were collected at the psychology department at Stanford University from September 2012 to December 2014. Data were analyzed from February 2019 to December 2020.
Interventions
CBGT and MBSR.
Main Outcomes and Measures
Changes in self-reported negative emotion and functional magnetic resonance imaging (fMRI) blood oxygen level–dependent (BOLD) signal within an a priori–defined brain search region mask derived from a meta-analysis of cognitive reappraisal and attention regulation 1 year posttreatment.
Results
Of 108 participants, 60 (56%) were female. The mean (SD) age was 32.7 (8.0) years. Self-reported race and ethnicity data were collected to inform the generalizability of the study to the wider population and to satisfy the requirements of the National Institutes of Health. From the categories provided by the National Institutes of Health, 47 participants selected White (43.5%), 42 selected Asian (38.9%) 10 selected Latinx (9.3%), 1 selected Black (1%), 1 selected Native American (1%), and 7 selected more than 1 race (6.5%). CBGT and MBSR were associated with a significant decrease in negative emotion (partial η2 range, 0.38 to 0.53) with no significant between-group differences when reacting (β, −0.04; SE, 0.09; 95% CI, −0.11 to 0.08; t92 = −0.37; P = .71), reappraising (β, −0.15; SE, 0.09; 95% CI, −0.32 to 0.03; t92 = −1.67; P = .10), or accepting (β, −0.05; SE, 0.08; 95% CI, −0.20 to 0.11; t92 = −0.59; P = .56). There was a significant increase in BOLD percentage signal change in cognitive and attention-regulation regions when reappraising (CBGT = 0.031; MBSR = 0.037) and accepting (CBGT = 0.012; MBSR = 0.077) negative self-beliefs. CBGT and MBSR did not differ in decreased negative emotion and increased reappraisal and acceptance BOLD responses. Reappraisal-associated MBSR (vs CBGT) negative emotions and CBGT (vs MBSR) brain responses were associated with social anxiety symptoms 1 year posttreatment.
Conclusions and Relevance
The results of this study suggest that CBGT and MBSR may be effective treatments with long-term benefits for patients with SAD that recruit cognitive and attention-regulation brain networks. Despite contrasting models of therapeutic change, CBT and MBSR may both enhance reappraisal and acceptance emotion regulation strategies.
Trial Registration
ClinicalTrials.gov Identifier: NCT02036658
Introduction
Social anxiety disorder (SAD) is a common psychiatric disorder with lifetime prevalence of 12.1%.1 SAD involves considerable impairment in social, educational, and occupational functioning, as well as poor quality of life.2,3,4 Because it is frequently unrecognized and untreated,5 SAD incurs a serious societal burden.6,7
Cognitive behavioral group therapy (CBGT), a criterion-standard intervention for SAD,8 trains patients to implement cognitive restructuring of maladaptive beliefs and interpretations in the context of within-session and in vivo exposures to feared situations. The effectiveness of CBGT is associated with fear-inhibitory learning, a form of implicit emotion regulation, and with learning cognitive reappraisal of unhelpful responses to specific situations.9,10,11
Research has also demonstrated the efficacy of mindfulness-based stress reduction (MBSR)12 in treating SAD.13 MBSR trains individuals to increase present-moment awareness, curiosity, and an experiential (rather than avoidance) approach via a variety of mindfulness exercises and meditations. Acceptance is a key facet of decentering (ie, the ability to observe one’s thoughts, feelings, and sensations as temporary mental events as opposed to true reflections of the self),14 which is considered a fundamental mechanism of mindfulness and has been shown to predict decreased relapse rates over 24 months in adults with remitted depression.15
Investigations of therapeutic mechanisms in CBGT and MBSR thus far have relied primarily on self-report measures, and have shown equivalent decreases in cognitive distortions and rumination, and increases in reappraisal frequency and self-efficacy, mindfulness skills, and attention focusing and shifting. Comparisons of CBGT and MBSR have demonstrated decreased frequency of subtle avoidance behaviors during CBGT but not during MBSR13 as one point of difference in mechanism. However, more fine-grained analyses of weekly changes during treatment for SAD suggest that, although both CBGT and MBSR produced similar trajectories of social anxiety symptom reduction, CBGT produced greater increases in disputing anxious thoughts and feelings and reappraisal success, while MBSR produced greater acceptance of anxiety and acceptance success.16 Thus, there is some evidence for specificity from self-report measures. However, directly probing SAD-associated brain functioning may provide a more direct assessment of therapeutic mechanisms.
Evidence suggests that both CBT and MBSR for SAD increase recruitment of emotion regulatory brain regions. CBT has been shown to increase activity in the reappraisal-associated dorsolateral, ventrolateral, and medial prefrontal cortical regions.17 For MBSR, attentional deployment of observing present-moment experience (referred to as open monitoring) has been shown to downregulate emotional reactivity to idiographic negative self-beliefs and to increase activity in attention-associated brain regions.18,19,20 However, because no studies, to our knowledge, have directly compared the effects of CBT and MBSR on emotion-regulation brain substrates, there is currently limited understanding about the common and specific effects on frontoparietal brain regions associated with reappraisal and acceptance in patients with SAD.
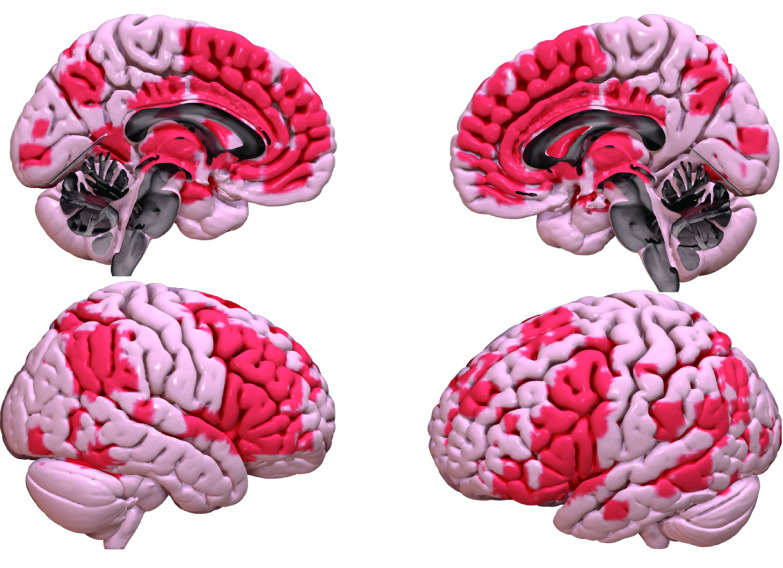
We tested for common and specific effects of CBGT and MBSR on brain activity during two forms of emotion regulation (reappraisal and acceptance) in adults with SAD. We used a validated autobiographical social situation emotion-regulation task17,21,22,23 to examine changes in self-reported negative emotion and functional magnetic resonance imaging (fMRI) blood oxygen level–dependent (BOLD) signal when participants were cued to react, reappraise, or accept idiographic negative self-beliefs embedded in autobiographical social situations pre- and post-CBT, pre- and post-MBSR, and for individuals in the waitlist (WL) control group. We focused our analysis within an a priori–defined brain search region mask (Figure 1) derived from meta-analyses of cognitive reappraisal and attention regulation.24,25,26
Figure 1. A Priori–Defined Brain Search Region Mask Derived From Meta-analyses of Cognitive Reappraisal and Attention Regulation.
Hypothesis 1: We expected that, compared with WL, treatment (CBGT and MBSR) would result in decreased negative emotion and increased BOLD signal in frontoparietal regions implicated in reappraisal and acceptance based on our prior study in healthy adults.23
Hypothesis 2: We expected some degree of specificity in the match between treatment and regulation strategy. For CBGT vs MBSR, we expected greater decreases in negative emotion and greater increases in fMRI BOLD signal in frontoparietal brain regions during reappraisal. For MBSR vs CBGT, we expected greater decreases in negative emotion and greater increases in BOLD signal in frontoparietal brain regions during acceptance.
Hypothesis 3: We expected treatment-mechanism specificity—that is, an interaction of CBGT vs MBSR by negative emotion and brain responses—to be associated with social anxiety symptoms 1 year posttreatment, with stronger association for CBGT during reappraisal and for MBSR during acceptance.
Methods
Participants
The trial protocol can be found in Supplement 1, and the statistical analysis plan can be found in Supplement 2; these have been described in detail elsewhere.27 A total of 108 unmedicated patients were enrolled who met DSM-IV28 criteria for a principal diagnosis of generalized SAD, scored greater than 60 on the Liebowitz Social Anxiety Scale–Self-report,29 met MRI eligibility, and had no evidence of thought disorder or bipolar disorder (see Goldin et al13; eMethods in Supplement 3). Patients were randomly assigned in cohorts of 6 to CBGT (n = 36), MBSR (n = 36), or WL (n = 36) groups. A random number generator determined the sequence of 6 groups per 3 arms of the randomized clinical trial. Individuals in the WL group were rerandomized to CBGT or MBSR, but only their pre-WL and post-WL data were analyzed here. After dropout from CBGT (n = 2), MBSR (n = 3), and WL (n = 1), and exclusion of incomplete neuroimaging data (n = 7), the final sample included 31 individuals in the CBGT group, 32 individuals in the MBSR group, and 32 individuals in the WL group (see Goldin et al13; eFigure 1 in Supplement 3). Participants provided written informed consent as approved by the Stanford University Institutional Review Board. The study followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline. The study design, search region, and data analytic strategy were preregistered at Open Science Framework.27
Procedure
Patients were recruited through referrals and web listings. Baseline assessments were completed before random assignment. Patients completed fMRI and self-report measures at baseline and posttreatment or post-WL, and self-report measures 1 year posttreatment. Research assistants who collected brain and behavioral data were blind to group assignment.
Clinical Assessment
Diagnostic interviews were conducted at baseline using the Anxiety Disorders Interview Schedule for the DSM-IV–Lifetime Version.30 To assess interrater reliability, we had PhD-level clinical psychologists and doctoral students review a random selection of 20% of the interviews. There was 100% agreement with the original principal diagnosis of SAD (κ = 1.0). We measured SAD symptoms with the Liebowitz Social Anxiety Scale–Self-Report at baseline, immediately posttreatment, and 1 year posttreatment.
fMRI Task Assessment
We used a previously23 validated version of the autobiographical social situation emotion-regulation task to assess negative emotion and fMRI BOLD signal during react, reappraise, and accept conditions in response to idiosyncratic negative self-beliefs embedded in participant-generated autobiographical negative social situations (eFigure 2 in Supplement 3). The fMRI task consisted of 3 runs, each consisting of 1 neutral and 2 negative stories. Each negative story was presented with 8 one-line sentences followed by a fixed sequence of 9 trials of negative self-beliefs, during which patients were cued to react (3 trials), reframe, or observe (6 trials). See the eMethods in Supplement 3 for a description of the instructions, fMRI task, training, image acquisition, preprocessing, and data analysis approach.
Treatments
CBGT was delivered by PhD-level clinical psychologists using a protocol consisting of twelve 2.5-hour sessions.31 We gave patients a CBT workbook32 to supplement the treatment protocol, which included psychoeducation and orientation to CBGT; cognitive restructuring training; within-session and between-session exposure to feared social situations; and relapse prevention and termination.
MBSR12 was delivered by an MS-level expert MBSR instructor trained at the University of Massachusetts Center for Mindfulness. The standard protocol was modified to convert the 1-day meditation retreat into 4 additional weekly group sessions between the standard class 6 and 7. This resulted in 12 weekly 2.5-hour sessions to match CBGT dose and duration. We gave patients an MBSR workbook33 to support ongoing meditation practice.
Using a criterion of 9 of 12 sessions attended for treatment completion status, 33 patients (92%) completed CBGT and 33 patients (92%) completed MBSR. Mean (SD) number of sessions attended for CBGT (10.47 [1.56]) and MBSR (10.37 [2.09]) did not differ (t71 = 0.22; P = .82). Adherence-to-protocol ratings conducted in real time in each session indicated that CBGT therapists and the MBSR instructor were in protocol with no between-group differences.
Statistical Analysis
For negative emotion ratings, we implemented intention-to-treat linear mixed models with the nlme package in RStudio version 1.3.1093 and R version 4.0.2 (the R Foundation) with random intercepts to address group by time interaction in hypotheses 1 and 2. For brain responses, we defined an a priori brain search region mask (Figure 1) with an automated meta-analytic tool24 with the search terms cognitive reappraisal and attention regulation, as well as a meta-analysis of reappraisal25 and a meta-analysis of meditation.26 To identify interaction activation clusters for hypotheses 1 and 2, we used the threshold-free cluster enhancement34 method that combines spatial extent and height of BOLD signal, together with voxel-based correction using the corrp package in FSL version 6.0 (FMRIB Software Library) across patients with complete time 1 and 2 data. All brain results were corrected for multiple comparisons at P < .05, familywise error corrected, and all tests were 2-tailed (eMethods in Supplement 3).
For hypothesis 3, we implemented multiple linear regression to test if post-CBGT vs post-MBSR negative emotion ratings or brain responses (mean within-patient β coefficients within the search region) when reappraising or accepting (after controlling for baseline emotion or brain responses) were associated with social anxiety symptoms 1 year posttreatment (residualized scores that control for pretreatment social anxiety symptoms). We reported effect sizes as partial η2.35
Results
Of the 108 included patients, 60 (56%) were female. The mean (SD) age was 32.7 (8.0) years. Self-reported race and ethnicity data were collected to inform the generalizability of the study to the wider population and to satisfy the requirements of the National Institutes of Health. From the categories provided by the National Institutes of Health, 47 participants selected White (43.5%), 42 selected Asian (38.9%) 10 selected Latinx (9.3%), 1 selected Black (1%), 1 selected Native American (1%), and 7 selected more than 1 race (6.5%).
Baseline Preliminary Analyses
As reported previously,13 CBGT, MBSR, and WL groups did not differ significantly in demographic and clinical characteristics (eTables 1 and 2 in Supplement 3). CBGT and MBSR were associated with a similar reduction of social anxiety symptoms from baseline to immediately posttreatment and 1 year posttreatment (eFigure 3 in Supplement 3) with treatment-specific weekly changes in frequency of disputing (CBGT greater than MBSR) and of acceptance (MBSR greater than CBGT) of anxious thoughts and feelings (eFigure 4 in Supplement 3).
Hypothesis 1: Treatment vs WL
Linear mixed models found that, compared with WL, CBGT and MBSR demonstrated greater pretreatment to posttreatment decreases in negative emotion when reacting (β, −0.28; SE, 0.05; 95% CI, −0.39 to −0.17; t92 = −5.12; P < .001), reappraising (β, −0.28; SE, 0.05; 95% CI, −0.37 to −0.19; t92 = −6.08; P < .001), and accepting (β, −0.29; SE, 0.05; 95% CI, −0.39 to −0.19; t92 = −5.64; P < .001).
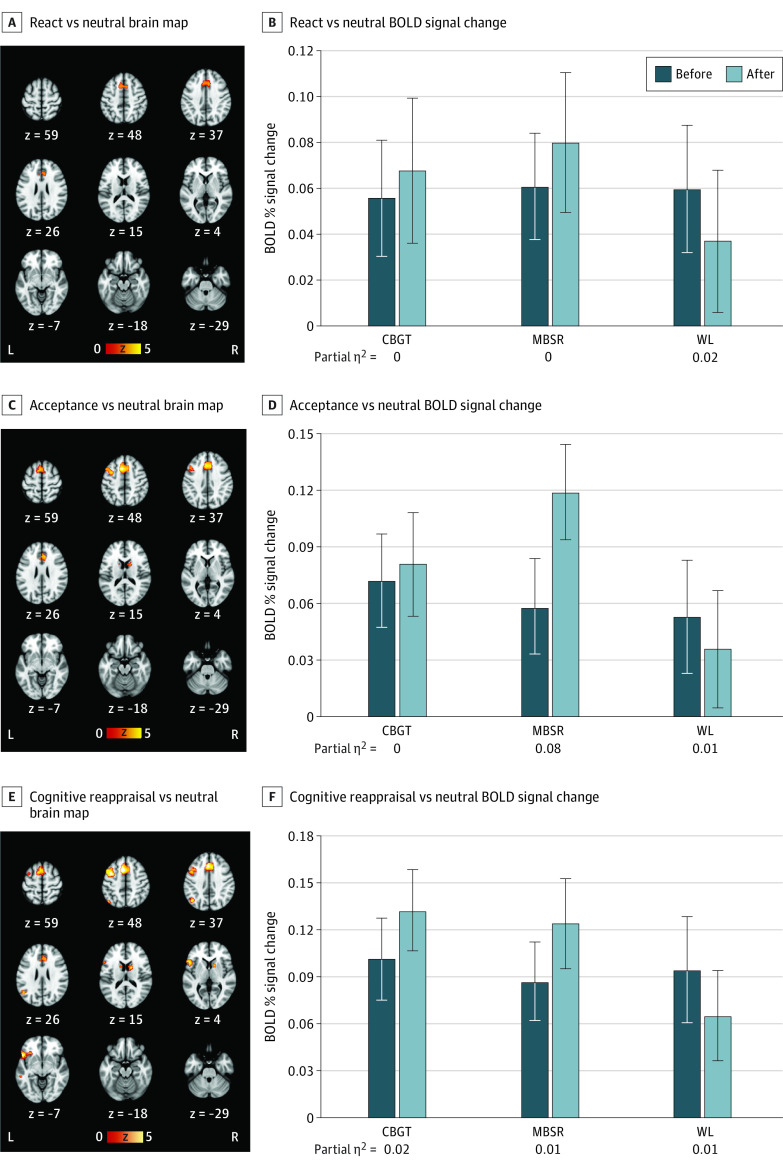
The threshold-free cluster enhancement method identified significant interaction in BOLD signal during reacting, accepting, and reappraising negative self-beliefs (vs reading neutral statements) between groups (treatment vs WL) from pretreatment to posttreatment via familywise error rate corrected (P < .05) (Figure 2). When reacting, there was an interaction of group by time characterized by greater increases in brain responses from pretreatment to posttreatment vs WL in dorsomedial prefrontal cortex (DMPFC) and dorsal anterior cingulate cortex (dACC). When reappraising, there was an interaction of group by time characterized by greater brain activation pretreatment to posttreatment vs WL in DMPFC, dACC, left dorsolateral prefrontal cortex (DLPFC), left ventrolateral prefrontal cortex (VLPFC), left supramarginal gyrus, left posterior superior temporal gyrus, and thalamus. When accepting, there was an interaction of group by time, characterized by greater brain responses pretreatment to posttreatment vs WL in left DLPFC, DMPFC, dACC, and thalamus.
Figure 2. Cognitive Behavioral Group Therapy (CBGT) and Mindfulness-Based Stress Reduction (MBSR) vs Waitlist (WL) Control by Pretreatment and Posttreatment Interaction Brain Maps With CBGT- and MBSR-Specific Blood Oxygen Level–Dependent (BOLD) Signal Changes.
Error bars indicate standard errors.
Hypothesis 2: CBGT vs MBSR
Linear mixed models revealed that CBGT and MBSR yielded similar reductions in negative emotion (partial η2 range, 0.38 to 0.53) with no significant between-group differences (Table 1) when reacting (β, −0.04; SE, 0.09; 95% CI, −0.11 to 0.08; t92 = −0.37; P = .71), reappraising (β, −0.15; SE, 0.09; 95% CI, −0.32 to 0.03; t92 = −1.67; P = .10), or accepting (β,−0.05; SE, 0.08; 95% CI, −0.20 to 0.11; t92 = −0.59; P = .56).
Table 1. Self-reported Negative Emotion Ratings for Individuals in the Cognitive Behavioral Group Therapy (CBGT) Group, the Mindfulness-Based Stress Reduction (MBSR) Group, and the Waitlist (WL) Group.
| Variable | Mean (SD) | ||
|---|---|---|---|
| CBGT (n = 31) | MBSR (n = 32) | WL (n = 32) | |
| Reaction | |||
| Pretreatment | 4.04 (0.54) | 3.89 (0.55) | 3.91 (0.86) |
| Posttreatment | 3.17 (0.72) | 2.98 (0.85) | 3.84 (0.89) |
| F test | 34.10 | 31.71 | 0.65 |
| P value | .001 | .001 | .43 |
| Partial η2 | 0.53 | 0.51 | 0.02 |
| Acceptance | |||
| Pretreatment | 2.99 (0.55) | 2.95 (0.62) | 2.75 (0.74) |
| Posttreatment | 2.45 (0.58) | 2.10 (0.56) | 2.92 (0.80) |
| F test | 21.30 | 60.85 | 32.11 |
| P value | .001 | .001 | .16 |
| Partial η2 | 0.38 | 0.64 | 0.04 |
| Reappraisal | |||
| Pretreatment | 2.82 (0.54) | 2.65 (0.65) | 2.59 (0.68) |
| Posttreatment | 2.23 (0.55) | 1.96 (0.47) | 2.78 (0.76) |
| F test | 34.03 | 38.38 | 3.03 |
| P value | .001 | <.001 | .09 |
| Partial η2 | 0.49 | 0.52 | 0.09 |
CBGT and MBSR were each associated with increased BOLD percentage signal when reacting (CBGT, 0.012; MBSR, 0.019; P > .28), reappraising (CBGT, 0.031; MBSR, 0.037; P > .28), or accepting (CBGT, 0.012; MBSR, 0.077; P > .28), with no significant between-group differences in the brain regions identified above.
Hypothesis 3: Social Anxiety Symptoms 1 Year Posttreatment
For reappraisal, as shown in Table 2, regression revealed an interaction of group by posttreatment negative emotion with social anxiety symptoms 1 year posttreatment. Posttreatment negative emotion was associated with social anxiety 1 year post-MBSR (R2, 0.13; t, 2.25; P = .03; β, 0.79; SE, 0.35; 95% CI, 0.07 to 1.51), but not post-CBGT (t, 1.65; P = .11). For acceptance, regression yielded no interaction of group by posttreatment negative emotion with social anxiety symptoms 1 year posttreatment, with no significant association post-MBSR (t, 1.27; P = .22) or post-CBGT (t, 2.03; P = .05).
Table 2. Linear Regression of Cognitive Behavioral Group Therapy (CBGT)–Associated Changes vs Mindfulness-Based Stress Reduction (MBSR)–Associated Changes in Negative Emotion Ratings and Functional Magnetic Resonance Imaging (fMRI) Blood Oxygen Level–Dependent (BOLD) Signal Associated With Severity of Social Anxiety Symptoms 1 Year Posttreatment (N = 61).
| Measure | R 2 | F 4,57 | P value | β (SE; 95% CI)a | t | P value |
|---|---|---|---|---|---|---|
| Negative emotion rating | ||||||
| Reappraisal | .18 | 3.03 | .03 | |||
| Pretreatment | 0.06 (0.22; −0.38 to 0.50) | 0.29 | .78 | |||
| Posttreatment | 0.63 (0.24; 0.15 to 1.11) | 2.61 | .01 | |||
| CBGT vs MBSR | 0.85 (0.48; −0.11 to 1.82) | 1.77 | .08 | |||
| CBGT vs MBSR × posttreatment | −0.49 (0.22; −0.94 to −0.04) | 2.18 | .03 | |||
| Acceptance | .11 | 1.77 | .15 | |||
| Pretreatment | −0.09 (0.23; −0.55 to 0.37) | 0.40 | .69 | |||
| Posttreatment | 0.52 (0.22; 0.08 to 0.96) | 2.37 | .02 | |||
| CBGT vs MBSR | 0.29 (0.49; −0.68 to 1.27) | 0.60 | .55 | |||
| CBGT vs MBSR × posttreatment | −0.20 (0.21; −0.62 to 0.21) | 0.99 | .33 | |||
| fMRI BOLD Signal | ||||||
| Reappraisal | .12 | 1.81 | .14 | |||
| Pretreatment | 0.67 (0.81; −0.96 to 2.30) | 0.82 | .42 | |||
| Posttreatment | 0.87 (0.84; −0.80 to 2.55) | 1.04 | .30 | |||
| CBGT vs MBSR | −0.34 (0.17; −0.67 to −0.01) | 2.06 | .045 | |||
| CBGT vs MBSR × posttreatment | 1.93 (0.83; 0.26 to 3.60) | 2.31 | .02 | |||
| Acceptance | .09 | 1.34 | .27 | |||
| Pretreatment | 0.32 (0.87; −1.43 to 2.07) | 0.37 | .72 | |||
| Posttreatment | 1.36 (0.88; −0.41 to 3.13) | 1.54 | .13 | |||
| CBGT vs MBSR | −0.17 (0.16; −0.49 to 0.14) | 1.10 | .28 | |||
| CBGT vs MBSR × posttreatment | 1.11 (0.88; −0.66 to 2.87) | 1.26 | .21 | |||
Unstandardized β weight.
For reappraisal, regression revealed an interaction of group by posttreatment brain responses with social anxiety symptoms 1 year posttreatment. Posttreatment brain responses were associated with social anxiety 1 year post-CBGT (R2, 0.17; t, 2.55; P = .02; β, 2.79; SE, 1.10; 95% CI, 0.55 to 5.04), but not post-MBSR (t, 0.91; P = .37). For acceptance, regression showed no interaction of group by posttreatment brain responses with social anxiety symptoms 1 year posttreatment. Posttreatment brain responses were associated with social anxiety 1 year post-CBGT (R2, 0.15; t, 2.25; P = .03; β, 2.58; SE, 1.15; 95% CI, 0.23 to 4.94), but not post-MBSR (t, 0.093; P = .93). Using clinically significant improvement to identify responders vs nonresponders did not yield significant associations between treatment-associated brain changes and social anxiety symptoms immediately posttreatment and 1 year posttreatment.
Discussion
In this randomized clinical trial, we investigated the effects of CBGT and MBSR on self-reported negative emotion and brain responses in adults with SAD while they attempted to reappraise and accept patient-specific negative self-beliefs embedded in autobiographical social situations. Our goals were to examine treatment-specific mechanisms and to test whether brain changes were associated with clinical symptoms at 1 year posttreatment.
Effects of CBT and MBSR on Negative Emotion and Brain Responses
Results for treatment (CBT and MBSR) vs WL provided support for hypothesis 1. Compared with WL, treatment decreased negative emotion and increased recruitment of regulation-associated brain regions (PFC, parietal cortex, and caudate nucleus) during reappraisal and acceptance.
The direct contrast of CBGT vs MBSR found no evidence for the hypothesis 2 association between treatment mechanism specificity in negative emotion and brain responses during reappraisal and acceptance. Prior studies using the autobiographical social situation emotion regulation fMRI task have found similar reductions in negative emotion when reacting and reappraising negative self-beliefs following CBT for SAD17 and when implementing breath-focused and meta-cognitive attention regulation following MBSR for SAD.19,22 While not specifically cued to do so, patients were likely to use newly strengthened emotion-regulation skills during the react condition to decrease reactivity to negative self-beliefs.
CBGT and MBSR resulted in similar increases in brain activation during reappraisal and acceptance in the medial, dorsomedial, dorsolateral, and ventrolateral PFC; superior parietal and lateral occipital regions; and the caudate nucleus. These results converge with previously detected brain patterns in nonanxious healthy adults using the same autobiographical social situation emotion-regulation fMRI task23 in executive attention control during acceptance of sad images,36 and in perspective shifting and effortful attention during decentering from stressful events.37 Clinical fMRI studies have reported similar increased PFC activation in patients with generalized anxiety disorder during acceptance of worry38 and MBSR-associated increases in PFC-parietal circuits in patients with SAD during meta-cognitive observing and acceptance of negative self-beliefs.22 The limited data presented thus far suggest that acceptance-associated emotion-regulation strategies may produce brain responses that overlap with well-documented reappraisal brain networks.25
One interpretation of the overlapping brain activation is that acceptance recruits many of the neuropsychological subcomponents that support reappraisal,25,39 such as cognitive control (DMPFC, DLPFC, and VLPFC), inhibitory control (right DLPFC and VLPFC), working memory (DMPFC and DLPFC), perspective taking (DLPFC), and monitoring and attentional control (superior parietal, MPFC, and DLPFC), but with lesser reliance on linguistic processing (left VLPFC, posterior MTG, and supramarginal gyrus).40 Alternatively, as previously reported using self-rated negative emotion data,13,16 CBGT and MBSR both increased reappraisal and mindfulness skills, including acceptance, and the brain results in this study may reflect greater recruitment of a core domain-general cognitive control network that supports implementation of both emotion-regulation strategies.
Long-term Clinical Outcome
Only the treatment-specific changes during reappraisal were significantly associated with reduced social anxiety symptoms 1 year posttreatment, specifically MBSR (vs CBGT) decreases in negative emotion and CBGT (vs MBSR) increases in fMRI BOLD signal. MBSR-associated enhancement of reappraisal abilities has been previously reported.41 fMRI studies of pretreatment brain predictors have reported that lesser rostral anterior cingulate cortex and lesser left DLPFC activity during reappraisal of negative images,42,43 inverse connectivity between amygdala and right VLPFC during affect labeling,44 greater occipitotemporal activation to angry vs neutral faces,45 and dorsal ACC activation46 during self-referential criticism are associated with response to CBT for SAD. One fMRI study found individual pre-CBT to post-CBT for SAD brain activity increases in right prefrontal cortex, right middle occipital gyrus, and decreases in left posterior superior temporal gyrus during reappraisal of social criticism were associated with 24% of the unique variance in CBT-associated reductions in social anxiety symptoms.11 Our study replicates the finding of CBT-associated increased PFC-parietal brain activity with reduction of social anxiety 1 year post-CBT and further identifies that these results are specific to reappraisal (vs acceptance) and to CBT (vs MBSR).
The clinical implications of our study findings are that CBT and MBSR may strengthen overlapping skills, including refining awareness of thought content and emotions, learning to diminish overlearned reactive avoidant tendencies and instead choose adaptive coping strategies, and weakening the salience of negative self-beliefs (by challenging or reframing them, or by experiencing them as transient mental events). Another inference is that, despite conceptual differences, CBT and MBSR might rely on common core emotion-regulation processes to produce therapeutic improvement in people experiencing anxiety disorders.47
Limitations and Directions for Future Research
Our study had limitations. Future studies could examine a wider range of emotion-regulation strategies (eg, situation modification, expressive suppression) and meditation skills (eg, nonelaboration of thoughts), as well as extinction of emotional reactivity as an implicit emotion-regulation mechanism associated with in vivo exposures. Although CBGT-associated reappraisal and acceptance brain changes were associated with decreased social anxiety symptoms 1 year posttreatment, this finding may be associated with numerous other factors. Because we used an a priori search region mask, we did not detect brain changes previously reported following MBSR, such as amygdala48 and somatosensory regions.49 To strengthen the reliability and generalizability of our results, future studies would benefit from examining a larger sample of patients with different mood and anxiety disorders, as well as examining changes in autonomic physiological responses. Comparison of CBT and MBSR with pharmacotherapy for SAD will help clarify the specificity of the findings reported here as well.
Conclusions
The results of this study suggest that CBGT and MBSR may be effective treatments with long-term benefits for patients with SAD that recruit cognitive and attention-regulation brain networks. Despite contrasting models of therapeutic change, CBT and MBSR may both enhance reappraisal and acceptance emotion regulation strategies.
Study protocol
Statistical analysis plan
eFigure 1. Consolidated Standards of Reporting Trials (CONSORT) diagram for a randomized controlled trial of CBGT vs MBSR vs WL groups
eFigure 2. Experimental task design
eFigure 3. Social Anxiety Symptom Severity (LSAS) over the course of treatment and up to 1 year posttreatment
eFigure 4. Weekly frequency of use of cognitive reappraisal (ie, disputing negative self-beliefs) and of acceptance of anxiety in anxiety triggering situations pretreatment, during treatment and posttreatment
eTable 1. Demographic and clinical characteristic of randomized participants (N = 108)
eTable 2. Interaction of group (CBGT+MBSR vs WL) by time (pretreatment vs posttreatment) on BOLD signal responses during react, reappraise, and accept conditions
eMethods
Data sharing statement
References
- 1.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593-602. doi: 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- 2.Stein MB, Kean YM. Disability and quality of life in social phobia: epidemiologic findings. Am J Psychiatry. 2000;157(10):1606-1613. doi: 10.1176/appi.ajp.157.10.1606 [DOI] [PubMed] [Google Scholar]
- 3.Acarturk C, de Graaf R, van Straten A, Have MT, Cuijpers P. Social phobia and number of social fears, and their association with comorbidity, health-related quality of life and help seeking: a population-based study. Soc Psychiatry Psychiatr Epidemiol. 2008;43(4):273-279. doi: 10.1007/s00127-008-0309-1 [DOI] [PubMed] [Google Scholar]
- 4.Alonso J, Angermeyer MC, Bernert S, et al. ; ESEMeD/MHEDEA 2000 Investigators, European Study of the Epidemiology of Mental Disorders (ESEMeD) Project . Disability and quality of life impact of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004;(420):38-46. doi: 10.1111/j.1600-0047.2004.00329.x [DOI] [PubMed] [Google Scholar]
- 5.Blanco C, Xu Y, Schneier FR, Okuda M, Liu SM, Heimberg RG. Predictors of persistence of social anxiety disorder: a national study. J Psychiatr Res. 2011;45(12):1557-1563. doi: 10.1016/j.jpsychires.2011.08.004 [DOI] [PubMed] [Google Scholar]
- 6.Acarturk C, Smit F, de Graaf R, van Straten A, Ten Have M, Cuijpers P. Economic costs of social phobia: a population-based study. J Affect Disord. 2009;115(3):421-429. doi: 10.1016/j.jad.2008.10.008 [DOI] [PubMed] [Google Scholar]
- 7.Patel A, Knapp M, Henderson J, Baldwin D. The economic consequences of social phobia. J Affect Disord. 2002;68(2-3):221-233. doi: 10.1016/S0165-0327(00)00323-2 [DOI] [PubMed] [Google Scholar]
- 8.Gordon D, Wong J, Heimberg R. Cognitive-behavioral therapy for social anxiety disorder: the state of the science. In: Weeks JW, ed. The Wiley-Blackwell Handbook of Social Anxiety Disorder. Wiley-Blackwell; 2014:477-497. doi: 10.1002/9781118653920.ch22 [DOI] [Google Scholar]
- 9.Wenzel A. Basic strategies of cognitive behavioral therapy. Psychiatr Clin North Am. 2017;40(4):597-609. doi: 10.1016/j.psc.2017.07.001 [DOI] [PubMed] [Google Scholar]
- 10.Goldin PR, Ziv M, Jazaieri H, et al. Cognitive reappraisal self-efficacy mediates the effects of individual cognitive-behavioral therapy for social anxiety disorder. J Consult Clin Psychol. 2012;80(6):1034-1040. doi: 10.1037/a0028555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldin PR, Ziv M, Jazaieri H, Weeks J, Heimberg RG, Gross JJ. Impact of cognitive-behavioral therapy for social anxiety disorder on the neural bases of emotional reactivity to and regulation of social evaluation. Behav Res Ther. 2014; 62:97-106.doi: 10.1016/j.brat.2014.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. Dell Publishing; 1990. [Google Scholar]
- 13.Goldin PR, Morrison A, Jazaieri H, Brozovich F, Heimberg R, Gross JJ. Group CBT versus MBSR for social anxiety disorder: a randomized controlled trial. J Consult Clin Psychol. 2016;84(5):427-437. doi: 10.1037/ccp0000092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gawrysiak MJ, Grassetti SN, Greeson JM, Shorey RC, Pohlig R, Baime MJ. The many facets of mindfulness and the prediction of change following mindfulness-based stress reduction (MBSR). J Clin Psychol. 2018;74(4):523-535. doi: 10.1002/jclp.22521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Segal ZV, Anderson AK, Gulamani T, et al. Practice of therapy acquired regulatory skills and depressive relapse/recurrence prophylaxis following cognitive therapy or mindfulness based cognitive therapy. J Consult Clin Psychol. 2019;87(2):161-170. doi: 10.1037/ccp0000351 [DOI] [PubMed] [Google Scholar]
- 16.Goldin PR, Morrison AS, Jazaieri H, Heimberg RG, Gross JJ. Trajectories of social anxiety, cognitive reappraisal, and mindfulness during an RCT of CBGT versus MBSR for social anxiety disorder. Behav Res Ther. 2017;97:1-13. doi: 10.1016/j.brat.2017.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goldin PR, Ziv M, Jazaieri H, Hahn K, Heimberg R, Gross JJ. Impact of cognitive behavioral therapy for social anxiety disorder on the neural dynamics of cognitive reappraisal of negative self-beliefs: randomized clinical trial. JAMA Psychiatry. 2013;70(10):1048-1056. doi: 10.1001/jamapsychiatry.2013.234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldin PR, Ziv M, Jazaieri H, Gross JJ. Randomized controlled trial of mindfulness-based stress reduction versus aerobic exercise: effects on the self-referential brain network in social anxiety disorder. Front Hum Neurosci. 2012;6(6):295. doi: 10.3389/fnhum.2012.00295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldin PR, Gross JJ. Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion. 2010;10(1):83-91. doi: 10.1037/a0018441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goldin PR, Ramel W, Gross J. Mindfulness meditation training and self-referential processing in social anxiety disorder: behavioral and neural effects. J Cogn Psychother. 2009;23(3):242-257. doi: 10.1891/0889-8391.23.3.242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goldin PR, Manber-Ball T, Werner K, Heimberg R, Gross JJ. Neural mechanisms of cognitive reappraisal of negative self-beliefs in social anxiety disorder. Biol Psychiatry. 2009;66(12):1091-1099. doi: 10.1016/j.biopsych.2009.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldin PR, Ziv M, Jazaieri H, Hahn K, Gross JJ. MBSR vs aerobic exercise in social anxiety: fMRI of emotion regulation of negative self-beliefs. Soc Cogn Affect Neurosci. 2013;8(1):65-72. doi: 10.1093/scan/nss054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goldin PR, Moodie CA, Gross JJ. Acceptance versus reappraisal: behavioral, autonomic, and neural effects. Cogn Affect Behav Neurosci. 2019;19(4):927-944. doi: 10.3758/s13415-019-00690-7 [DOI] [PubMed] [Google Scholar]
- 24.Yarkoni T, Poldrack RA, Nichols TE, Van Essen DC, Wager TD. Large-scale automated synthesis of human functional neuroimaging data. Nat Methods. 2011;8(8):665-670. doi: 10.1038/nmeth.1635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Buhle JT, Silvers JA, Wager TD, et al. Cognitive reappraisal of emotion: a meta-analysis of human neuroimaging studies. Cereb Cortex. 2014;24(11):2981-2990. doi: 10.1093/cercor/bht154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fox KCR, Dixon ML, Nijeboer S, et al. Functional neuroanatomy of meditation: a review and meta-analysis of 78 functional neuroimaging investigations. Neurosci Biobehav Rev. 2016;65:208-228. doi: 10.1016/j.neubiorev.2016.03.021 [DOI] [PubMed] [Google Scholar]
- 27.Goldin PR, Moodie C, Gross J. A randomized controlled trial of the effectiveness of cognitive-behavioral therapy vs. mindfulness-based stress reduction in adults with social anxiety disorder. Accessed December 12, 2018. https://osf.io/j8uy5/?view_only=97e15b7e2ac04e2499043ebb560dc3a0
- 28.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Association; 1994. [Google Scholar]
- 29.Liebowitz MR. Social phobia. Mod Probl Pharmacopsychiatry. 1987;22:141-173. doi: 10.1159/000414022 [DOI] [PubMed] [Google Scholar]
- 30.DiNardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV, Lifetime Version, ADIS-IV-L. Oxford University Press; 1994. [Google Scholar]
- 31.Heimberg RG, Becker RE. Cognitive-Behavioral Group Therapy for Social Phobia: Basic Mechanisms and Clinical Strategies. Guilford Press; 2002. [Google Scholar]
- 32.Hope D, Heimberg R, Turk C. Managing Social Anxiety: A Cognitive-Behavioral Therapy Approach. 2nd ed. Oxford University Press; 2010. [Google Scholar]
- 33.Stahl B, Goldstein E. A Mindfulness-Based Stress Reduction Workbook. New Harbinger; 2010. [Google Scholar]
- 34.Smith SM, Nichols TE. Threshold-free cluster enhancement: addressing problems of smoothing, threshold dependence and localisation in cluster inference. Neuroimage. 2009;44(1):83-98. doi: 10.1016/j.neuroimage.2008.03.061 [DOI] [PubMed] [Google Scholar]
- 35.Pierce CA, Block RA, Aguinis H. Cautionary note on reporting eta-squared values from multifactor ANOVA designs. Educ Psychol Meas. 2004;64(6):916-924. doi: 10.1177/0013164404264848 [DOI] [Google Scholar]
- 36.Smoski MJ, Keng SL, Ji JL, Moore T, Minkel J, Dichter GS. Neural indicators of emotion regulation via acceptance vs reappraisal in remitted major depressive disorder. Soc Cogn Affect Neurosci. 2015;10(9):1187-1194. doi: 10.1093/scan/nsv003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lebois LAM, Papies EK, Gopinath K, et al. A shift in perspective: decentering through mindful attention to imagined stressful events. Neuropsychologia. 2015;75:505-524. doi: 10.1016/j.neuropsychologia.2015.05.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ellard KK, Barlow DH, Whitfield-Gabrieli S, Gabrieli JDE, Deckersbach T. Neural correlates of emotion acceptance vs worry or suppression in generalized anxiety disorder. Soc Cogn Affect Neurosci. 2017;12(6):1009-1021. doi: 10.1093/scan/nsx025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ochsner KN, Silvers JA, Buhle JT. Functional imaging studies of emotion regulation: a synthetic review and evolving model of the cognitive control of emotion. Ann N Y Acad Sci. 2012;1251:E1-E24. doi: 10.1111/j.1749-6632.2012.06751.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Price CJ. A review and synthesis of the first 20 years of PET and fMRI studies of heard speech, spoken language and reading. Neuroimage. 2012;62(2):816-847. doi: 10.1016/j.neuroimage.2012.04.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Garland EL, Hanley AW, Goldin PR, Gross JJ. Testing the mindfulness-to-meaning theory: evidence for mindful positive emotion regulation from a reanalysis of longitudinal data. PLoS One. 2017;12(12):e0187727. doi: 10.1371/journal.pone.0187727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Klumpp H, Fitzgerald JM, Kinney KL, et al. Predicting cognitive behavioral therapy response in social anxiety disorder with anterior cingulate cortex and amygdala during emotion regulation. Neuroimage Clin. 2017;15:25-34. doi: 10.1016/j.nicl.2017.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Klumpp H, Roberts J, Kennedy AE, et al. Emotion regulation related neural predictors of cognitive behavioral therapy response in social anxiety disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2017;75:106-112. doi: 10.1016/j.pnpbp.2017.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Young KS, LeBeau RT, Niles AN, et al. Neural connectivity during affect labeling predicts treatment response to psychological therapies for social anxiety disorder. J Affect Disord. 2019;242:105-110. doi: 10.1016/j.jad.2018.08.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Doehrmann O, Ghosh SS, Polli FE, et al. Predicting treatment response in social anxiety disorder from functional magnetic resonance imaging. JAMA Psychiatry. 2013;70(1):87-97. doi: 10.1001/2013.jamapsychiatry.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Månsson KNT, Frick A, Boraxbekk CJ, et al. Predicting long-term outcome of Internet-delivered cognitive behavior therapy for social anxiety disorder using fMRI and support vector machine learning. Transl Psychiatry. 2015;5:e530. doi: 10.1038/tp.2015.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Campbell-Sills L, Barlow DH. Incorporating emotion regulation into conceptualizations and treatments of anxiety and mood disorders. In: Gross JJ, ed. Handbook of Emotion Regulation. Guilford; 2007:542-559. [Google Scholar]
- 48.Hölzel BK, Hoge EA, Greve DN, et al. Neural mechanisms of symptom improvements in generalized anxiety disorder following mindfulness training. Neuroimage Clin. 2013;2:448-458. doi: 10.1016/j.nicl.2013.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sevinc G, Hölzel BK, Hashmi J, et al. Common and dissociable neural activity after mindfulness-based stress reduction and relaxation response programs. Psychosom Med. 2018;80(5):439-451. doi: 10.1097/PSY.0000000000000590 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Study protocol
Statistical analysis plan
eFigure 1. Consolidated Standards of Reporting Trials (CONSORT) diagram for a randomized controlled trial of CBGT vs MBSR vs WL groups
eFigure 2. Experimental task design
eFigure 3. Social Anxiety Symptom Severity (LSAS) over the course of treatment and up to 1 year posttreatment
eFigure 4. Weekly frequency of use of cognitive reappraisal (ie, disputing negative self-beliefs) and of acceptance of anxiety in anxiety triggering situations pretreatment, during treatment and posttreatment
eTable 1. Demographic and clinical characteristic of randomized participants (N = 108)
eTable 2. Interaction of group (CBGT+MBSR vs WL) by time (pretreatment vs posttreatment) on BOLD signal responses during react, reappraise, and accept conditions
eMethods
Data sharing statement