Abstract
The human population is currently facing the third and possibly the worst pandemic caused by human coronaviruses (CoVs). The virus was first reported in Wuhan, China, on 31 December 2019 and spread within a short time to almost all countries of the world. Genome analysis of the early virus isolates has revealed high similarity with SARS-CoV and hence the new virus was officially named SARS-CoV-2. Since CoVs have the largest genome among all RNA viruses, they can adapt to many point mutation and recombination events; particularly in the spike gene, which enable these viruses to rapidly change and evolve in nature. CoVs are known to cross the species boundaries by using different cellular receptors. Both animal reservoir and intermediate host for SARS-CoV-2 are still unresolved and necessitate further investigation. In the current review, different aspects of SARS-CoV-2 biology and pathogenicity are discussed, including virus genetics and evolution, spike protein and its role in evolution and adaptation to novel hosts, and virus transmission and persistence in nature. In addition, the immune response developed during SARS-CoV-2 infection is demonstrated with special reference to the interplay between immune cells and their role in disease progression. We believe that the SARS-CoV-2 outbreak will not be the last and spillover of CoVs from bats will continue. Therefore, establishing intervention approaches to reduce the likelihood of future CoVs spillover from natural reservoirs is a priority.
Keywords: coronavirus, COVID-19, cross-species transmission, evolution, immune response, SARS-CoV-2
1. Introduction
Coronaviruses (CoVs) have long been known to infect human and animals causing a variety of diseases that affect the respiratory airways, intestine, liver, heart, kidneys, and nervous system [1]. Till the beginning of the current millennium, four CoVs (HCoV-229E, HCoV-NL63, HCoV-OC43 and HCoV-HKU1) were described in humans with mild and self-limiting upper respiratory disease. In the last two decades, the world population had witnessed three outbreaks of CoVs with severe respiratory and systemic outcomes, and considerable death rates.
The first outbreak developed in China in 2002 and spread to several countries worldwide. According to the World Health Organization (WHO), the outbreak that was caused by SARS-CoV-1 affected 8096 cases in 29 countries and costed 774 (9.56%) lives. In 2012, another outbreak caused by MERS-CoV was started in Saudi Arabia, rapidly distributed in the neighboring countries, and further to geographically distant regions [2]. The MERS-CoV outbreak is still ongoing, resulting in a sum of 2519 laboratory-confirmed cases and 866 (34.3%) deaths.
In December 2019, a third outbreak began in Wuhan, China, and was termed later by WHO as “coronavirus disease 2019” (COVID-19) [3]. During the last few months, the disease spanned the globe and affected more than 141 million with about 3 million (2%) losing their lives [4]. The outbreak was caused by SARS-CoV-2, which is highly antigenically and genetically similar to SARS-CoV-1 [3]. Both SARS-CoV-1 and SARS-CoV-2 share some features; (i) they use the same cellular receptor ACE2, (ii) their internal fusion peptides of the S protein are identical, (iii) they have the same genomic organization with 79.5% sequence similarity. However, a number of dissimilarities were reported, such as the length of the S protein which is longer in SARS-CoV-2, and the presence of additional furin cleavage site in the S protein of SARS-CoV-2. In addition, both viruses show somehow different patterns of clinical presentation, pathogenesis, and epidemiology [5]. SARS-CoV-2 is mainly transmitted among human populations by inhalation of aerosol droplets and touching contaminated surfaces [6]. The disease symptoms are generally diverse; ranging from mild to life-threatening. Although the virus affects all age groups, people with high risk (for example, the elderly, immunosuppressed individuals, and patients with comorbidities) may get more severe disease outcomes and require hospitalization and intensive care facilities [7]. As a consequence, unprecedented measures and restrictions have been adopted to control the spread of the disease and its impact on health and economy, including lock down, partial/complete curfew, and travel restrictions [8].
Currently, several vaccine formats (mRNA, viral vectors, inactivated, and subunit vaccines) have been approved and more than 1.65 billion doses administered worldwide. In the current review, the following topics are covered: (i) SARS-CoV-2 genetics and evolution, (ii) S protein and its role in virus evolution and adaptation through receptor usage, (iii) possible ways of virus transmission, (iv) the immune response and its role in SARS-CoV-2 pathogenicity.
2. SARS-CoV-2: Virus Genetics and Evolution
2.1. Taxonomy and Genome Organization
All CoVs are members of the subfamily Orthocoronavirinae, family Coronaviridae, and order Nidovirales. These viruses have the longest genome (26.4–32.0 kb) amongst all recognized RNA viruses [9,10]. The viral RNA genome, which is non-segmented, positive sense, and single stranded, is encapsulated within a helical nucleocapsid and a virus envelope that carries three glycoprotein projections; spike (S), membrane (M), and envelop (E). According to the international committee on taxonomy of viruses (ICTV), four genera have been described within the subfamily Orthocoronavirinae including alphacoronavirus, betacoronavirus, gamma-coronavirus, and deltacoronavirus [11]. Members of the first two genera infect mammals (including human), while CoVs of the latter two genera mostly infect birds [12].
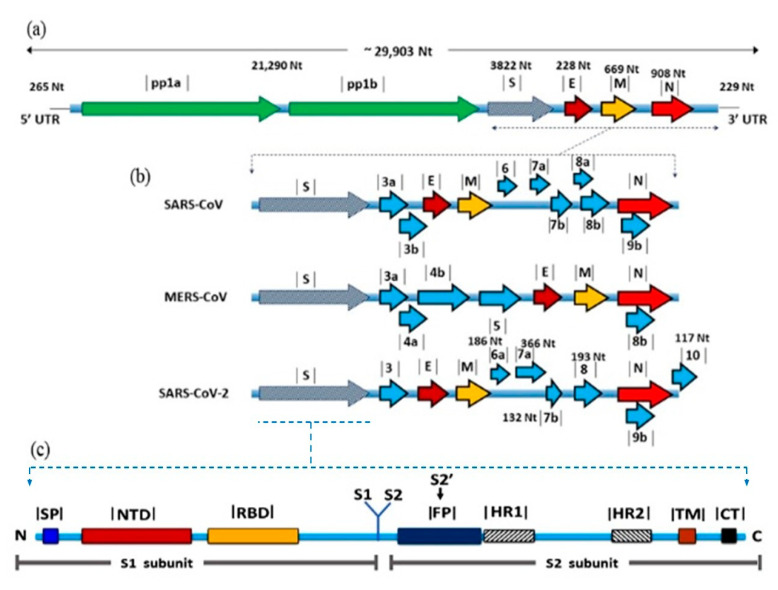
SARS-CoV-2 genome is approximately 29.8 kb long and has a GC content of 38% [13]. The genome is flanked by two untranslated regions (UTRs) and is annotated by 14 open reading frames (ORFs). The first two 5′-ORFs; ORF1ab and ORF1a, extend for about two-thirds of the genome and encodes for 16 non-structural proteins (nsps) that are responsible for virus replication [14]. The last-third ORFs encode for the structural proteins; S, M, E, and nucleocapsid (N), beside eight accessory proteins [15]. The number and location of the accessory proteins are generally variable among CoVs albeit their functions are not fully identified (Figure 1). It is expected that these proteins may play a role in virus replication and pathogenesis [16].
Figure 1.
Genomic organization and gene view of three human betacoronaviruses. (a) Coronavirus genome is a positive sense ssRNA, which is flanked by two untranslated regions, 5’ UTR and 3’ UTR. The first two thirds of the genome, ORF1a/b encoding for non-structural proteins required for virus replication. Structural proteins including E, M and N nucleoprotein, and accessory proteins, (b) comparison between the three CoVs in terms of the number and positions of accessory proteins, (c) detailed structure of the S protein showing the domains involved in receptor binding S1 and membrane fusion S2.
2.2. Origin and Evolution
Sequence and phylogenetic analysis of SARS-CoV-2 structural genes have revealed genetic relevance to SARS-CoV-1 (79%) rather than MERS-CoV (50%) [17]. However, several variations enough to clearly discriminate between both SARS-CoVs still exist. For example, ORF8a is absent in SARS-CoV-2 while present in SARS-CoV-1, ORF8b is 38 aa shorter in SARS-CoV-1, and ORF3b is 132 aa shorter in SARS-CoV-2 [18]. SARS-CoV-2 also shares marked sequence homology with bat SARS-Like CoVs from Zhoushan in Eastern China; bat-SL-CoVZC45 (87.99%) and bat-SL-CoVZXC21 (87.23%). Thus, SARS-CoV-2 was allocated in the subgenus Sarbecovirus with the bat coronaviruses BetaCoV/bat/Yunnan/ RaTG13/2013 and SARS-like bat CoVs [14,17]. The level of genetic similarity with RaTG13 is not enough to consider SARS-CoV-2 as a variant; however, bats are thought to be the natural reservoir where SARS-CoV-2 was originated and spread through an intermediate host [19].
The intermediate host of SARS-CoV-2 is still an enigma, in contrast to SARS-CoV-1 and MERS-CoV in which their intermediate hosts were resolved as palm civet [20], and dromedary camel [21], respectively. Determining the intermediate host is crucial to stop introduction of viruses to the community by blocking the interspecies transmission. Mass slaughtering of palm civets had a great impact on the termination of SARS-CoV-1 epidemic [20].
Early in the pandemic, the virus was thought to spread from a seafood market; however, some patients had no history of visiting these markets [6]. Later on, pangolin was suspected as the intermediate host since highly relevant CoVs were isolated from two dead Malayan pangolins [22]. Complete genome sequences of pangolin CoVs were aligned with different CoVs and confirmed high sequence identity with SARS-CoV-2 (91.02%) and bat RatG13 (90.55%) [23]. The susceptibility of a wide array of laboratory animals, domestic animals, and birds to SARS-CoV-2 was further tested. The virus did not efficiently replicate in birds (chickens and ducks), dogs, and pigs, whereas ferrets and cats were permissive to airborne infections [24].
SARS-CoV, as a typical RNA virus, generates quasi species of viruses during replication as a result of the polymerase errors [25]. Consequently, the virus progeny acquires new genetic and antigenic features that improve fitness in the environment and escape from the pre-existing immunity. Several mutations and recombination sites were recognized throughout the genome of SARS-CoV-2. Most importantly, six potential recombination sites identified in S gene were assumed to be responsible for evolutionary survival and adaptation in humans [19]. An 81-nucleotide deletion (27 aa) was defined in ORF7a, which encodes a protein induces apoptosis, and counteracts the action of BST-2 to facilitate virus release during replication [26,27,28]. Similarly, a 382-nucleotide deletion was observed in ORF8 [29]. The impact of this deletion was previously investigated in SARS-CoV-1, and demonstrated reduced virus replication in vitro [30]. In case of SARS-CoV-2, ∆382 nucleotide variants were associated with milder infections [31]. Interestingly, several variants with mutations in the S protein emerged, such as P1, B.1.1.7, B.1.351, B.1.427, and B.1.429. Such variants are associated with different clinical presentation, reinfection rate, and transmissibility [32,33,34]. In addition, some of the current vaccines were found to be less effective against one or more of these variants [35,36].
3. S Protein: Role in Virus Evolution and Cross-Species Transmission
CoVs have a great potential to jump between species. Numerous host-switching episodes were reported in the last three decades, including animal-to-human, human-to-animal, and animal-to-animal transmission [20]. Such cross-species transmission had resulted in the development of significant diseases in man and animals [37,38,39,40]. The most evident zoonotic transmission of CoVs involved the emergence of SARS-CoV-1, MERS-CoV, and the pandemic SARS-CoV-2. S protein of CoVs is believed to play a vital role in cross-species transmission [41].
S protein is a group I glycoprotein that forms the long projections decorating the surface of CoV particles in a characteristic crown-like shape. It is responsible for initiation of the infection process through binding to specific cell receptors and fusion-mediated entry in host cell [41]. The length of S protein varies among CoVs from 1100 to 1600 amino acids, and the molecular weight is typically around 220 kDa. The primary form of S protein is composed of three defined regions; large ectodomain, transmembrane domain, and cytoplasmic tail (Figure 1b). The ectodomain has two functional domains S1 and S2, which are responsible for receptor binding and membrane fusion, respectively [41,42]. S1 is further subdivided into two subdomains; S1-CTD, which binds to protein receptors [43], and S1-NTD that binds to sugar receptors [40]. After biosynthesis, S proteins are arranged in homotrimers, which exist either in prefusion or post-fusion forms [41]. The prefusion form is metastable and proteolytically cleaved at S1/S2 boundary by various triggers (Table 1) to form the postfusion form [41]. The fact that some host cell proteases are tissue-specific may contribute to CoV tropism to the respiratory tract.
Table 1.
Receptor usage and fusion triggers of most important CoVs species.
| Genus | Species | Receptor | Fusion Triggers | Reference |
|---|---|---|---|---|
| Alphacoronavirus | HCoV-NL63 | ACE2 | [44] | |
| HCoV-229E | Aminopeptidase N (APN) | [45] | ||
| TGEV | [46] | |||
| PEDV | [47] | |||
| PRCV | [48] [48] [48] |
|||
| Feline-CoV | ||||
| Canine-CoV | ||||
| Betacoronavirus | MERS-CoV | Dipeptidyl peptidase 4 (DPP4) |
|
[49] |
| MHV | Carcinoembryonic antigen-related cell adhesion molecule 1 |
|
[50] | |
| Bovine-CoV | 5-N-acetyl-9-O-acetyl neuraminic acid, Neu 5,9 Ac2 | [51] | ||
| HCoV-OC43 | ||||
| HKU4 | Dipeptidyl peptidase 4 |
|
||
| SARS-CoV-1 | ACE2 |
|
[52] | |
| SARS-CoV-2 | [53] | |||
| Gammacoronavirs | IBV | Sugar | [54] |
HCoV: Human coronavirus; TGEV: Transmissible gastroenteritis virus; PEDV: Porcine Epidemic Diarrhea Coronavirus; PRCV: Porcine respiratory coronavirus; CoV: Coronavirus; MHV: Murine hepatitis virus, HKU4: Tylonycteris bat coronavirus (Bat-CoV), IBV: Infectious bronchitis virus; ACE2: Angiotensin-converting enzyme.
Three main features of S protein contribute to the evolution of CoVs including: (1) the outstanding ability of receptor usage, (2) the high mutation rate, (3) the potential of acquiring new proteolytic cleavage sites. No general receptors were described for CoVs; instead, they use numerous receptors to bind with target cells. Interestingly, CoVs from different genera can use the same receptor and CoVs of the same genus may use different receptors. The high mutation rate of S protein is an expected consequence of its role in cell binding, which makes S protein a major target for immune pressure [41]. A single amino acid change in the receptor-binding domain can lead to host-shifting and development of serious epidemics. For example, two amino acid changes, T31K and E38D, in S1-CTD subdomain of SARS-CoV-1 were predicted to strengthen the binding to human ACE2 receptor. Such changes are potentially the cause of cross-species transmission of SARS-CoV-1 from civets to man [55].
Cleavage of S protein and release of the fusion peptide is a crucial step for virus entry. Acquiring new cleavage sites, particularly furin, enhances infectivity and increases the likelihood of systemic disease in many virus infections, such as influenza, Ebola, AIDS, Zika, dengue, and MERS [56,57,58]. The in vitro studies showed that the more furin cleavage sites acquired on S protein of infectious bronchitis (IBV) CoV, the broader host range and the higher ability to infect more cell lines [59]. IBV with new cleavage site on S protein displayed high pathogenicity in chickens [60]. The S protein of SARS-CoV-2 has an additional furin cleavage site that is absent in SARS-CoV-1 [53]. The existence of such new site may enhance virus transmissibility, host range, and the ability to cause systemic infection [61].
S protein of SARS-CoV-2 specifically binds to ACE2 receptors as a prerequisite of cell entry [53]. With the continuous and rapid flow of data, several questions have arisen to help understanding the impact of this process on virus infectivity. For example; (i) what is the degree of sequence similarity between S protein of SARS-CoV-1 and SARS-CoV-2, (ii) do both viruses have the same binding affinity to ACE2. On sequence level, S protein of SARS-CoV-2 shares 98% and 70% sequence identity with its counterparts in RaTG13 and SARS-CoV-1, respectively. Although both SARS-CoVs bind to the same receptor, their S1-CTD subdomains display different antigenic properties. The monoclonal antibodies bind to S1-CTD and the polyclonal antibodies bind to RBD of SARS-CoV-1, failing to recognize their counterparts in SARS-CoV-2 [61]. In contrary, the polyclonal antibodies raised against the complete S protein of SARS-CoV-1 were able to neutralize the infectivity of SARS-CoV-2 [53]. It is worthwhile to mention that S2 domain of both viruses shares high sequence identity (~90%) and many neutralizing epitopes [61]. The binding affinity of S protein of SARS-CoV-2 to ACE2 receptor is generally weaker than the binding of SARS-CoV-1 [3,53,62]. In contrast to SARS-CoV-1 [63], the RBD of SARS-CoV-2 is less accessible due to its laying down dynamic state [53].
4. Transmission of SARS-CoV-2
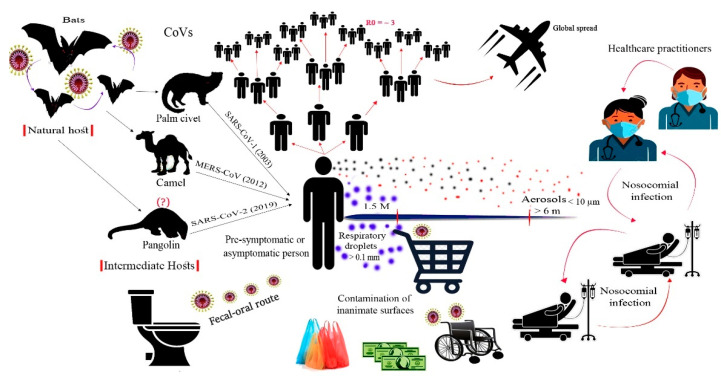
Similar to other respiratory viruses, SARS-CoV-2 is mainly transmitted via respiratory droplets, aerosols, and close contact with infected persons [5]. The contaminated respiratory droplets are generated during speech and sneezing of infected persons. Large droplets do not stay airborne for a long time and settle down on surfaces, whereas, small droplets and aerosols are carried away and stay airborne for hours [64,65,66]. Aerosols have also been generated in hospitals during bronchoscopy, endotracheal intubation, cardiopulmonary resuscitation, and nebulization (Figure 2) [14,64,65]. The large respiratory droplets represent a primary source of infection either by inhalation prior to settling down or by touching contaminated objects. Airborne transmission is the common route of transmission in enclosed settings with inadequate ventilation (for example, public transportation vehicles, classrooms, offices, restaurants, etc.) [67].
Figure 2.
Origin and transmission of SARS-CoV-2. The virus is believed to be originated from bats and spread to humans through an intermediate host. Human-to-human transmission mainly occurred by respiratory aerosols generated when an infected person sneezes or speeches. Respiratory aerosols can travel to long distances, whereas respiratory droplets settle down on nearby surfaces and represent a possible risk of infection. Basic reproduction number (R0) of the virus is estimated as 3.6. The faecal-oral route of transmission was reported due to the ability of the virus to replicate in the gastrointestinal tract. Within hospital settings, nosocomial infection is also known to occur among healthcare practitioners and hospitalized patients.
The other transmission routes that should not be neglected involve the fecal-oral and fecal-respiratory routes. Transmission via these routes was previously reported for SARS-CoV-1 and MERS-CoV [68]. SARS-CoV-2 was detected in stool and urine samples of laboratory-confirmed cases, and the virus was isolated from intestinal contents and anal swabs [69]. Interestingly, the virus was detected in these samples after respiratory clearance, which may indicate the prolonged shedding of SARS-CoV-2 from alternative routes, even in patients with negative respiratory samples (Figure 2). In hospital-based patient care settings, high bioaerosol concentrations from flushing fecal wastes have been recorded [70]. These bioaerosols might lead to surface contamination and fecal-respiratory exposures among patients and healthcare workers.
At the moment, there is no firm evidence that vertical transmission of SARS-CoV-2 occurs; however, the possibility should not be completely omitted. Trials for identification of SARS-CoV-2 RNA on the objects of conception and newborns were all negative [68]. Nonetheless, more recent studies have suggested potential trans-placental transmission of SARS-CoV-2 due to the presence of specific IgG and IgM antibodies [71] and viral RNA in samples collected from newborns at days 2 and 4 post-delivery [72].
Pre-symptomatic and asymptomatic infected individuals are important sources of SARS-CoV-2 transmission. Virus transmission from asymptomatic cases was estimated to cause 86.2% of all reported cases worldwide [65]. Globally, it was estimated that around two-thirds of COVID-19 cases exported from China have remained undetected [73]. Therefore, extensive SARS-CoV-2 screening and early detection of asymptomatic cases would impact the transmission efficiency and disease spread in different communities [65].
Persistence of SARS-CoV-2 in the environment; particularly on inanimate objects, has created a state of fear and insecurity in the public [74]. In general, most CoVs can persist in the environment up to one month depending on the surface type. SARS-CoV-2 loses its infectivity after 3 h on printing and tissue papers, 24 h on cardboard, and 2 days on wood and cloth. The virus is more stable on smooth surfaces and can persist up to 4 days on glass and banknote, and 7 days on stainless steel and plastic [64,75]. SARS-CoV-2 is also sensitive to increased temperature and common household disinfectants (for example, hand soap). The virus can withstand temperatures of 4 °C, 22 °C, 37 °C, 56 °C, and 70 °C for 2 weeks, 7 days, 1 day, 10 min, and 5 min, respectively. Interestingly, the virus is stable at a wide range of pH (3–10) [75].
Therefore, precautions should be considered by individuals and authorities to reduce virus transmission in the community. Individuals should adopt strict personal hygiene, such as frequent hand washing and mask wearing. Within indoor settings, improved ventilation and avoiding gatherings are necessary. Appropriate biosecurity measures should also be applied in toilets to reduce virus transmission via fecal-oral and fecal-respiratory routes. These measures include closing toilet lids before flushing, keeping toilet fans running, and using the autorun hang washer.
5. Immune Response against SARS-CoV-2
Little knowledge is currently available on the host immune response against SARS-CoV-2 and the immunopathogenesis during COVID-19. Most of the assumptions are based on the available data about SARS-CoV-1 and MERS-CoV [76]. The aggressiveness and disease severity witnessed in SARS-CoV-2 infected individuals, even though in a limited percentage of infected individuals, result from the efficient immune evasion strategies employed by SARS-CoV-2 [77]. It is known that the host antiviral response relies on type I interferon expression of host cells [78]. However, SARS-CoV-1, and most likely SARS-CoV-2, effectively inhibits the interferon response by suppressing activation of the TNF receptor-associated factors (TRAF) 3 and 6, and the transcription factors NFκB, IRF3, IRF7, and reducing secretion of the pro-inflammatory effector cytokines IL-1, IL-6 and TNF-α [79]. Inhibiting type 1 IFN signaling suppresses anti-viral programs, while increasing IL-1, IL-6, and TNF-α expression amplifies hyperinflammation and cytokine storm through positive feedback [77,79]. Altogether, suppression of innate immune mechanisms in infected cells allows SARS-CoV-2 to proliferate without triggering the innate antiviral response machinery.
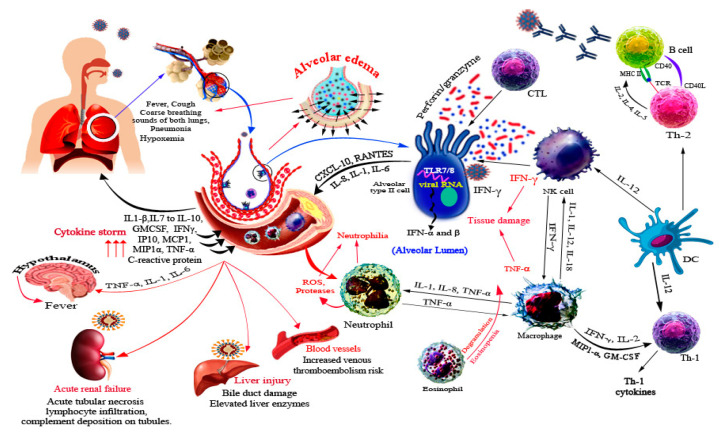
The host immune response to SARS-CoV-2 is not only directed against the virus but also involves immune dysregulation and hyperactivity [80]. SARS-CoV-2 infection initiates a systemic immune response recruiting inflammatory macrophages and monocytes, cytokine production, and priming adaptive T and B cell immune responses (Figure 3). In the majority of cases, the infection resolves on its own, whereas a dysregulated and excessive immune response occurs in some cases, causing severe lung disease and systemic pathology (Figure 3) [6].
Figure 3.
Immune response and immunopathogenesis associated with SARS-CoV-2. SARS-CoV-2 infects mainly type II alveolar cells and upon infection a wide array of cytokines and chemokines is secreted, which recruits several immune innate cells. Recruitment of cells further potentiates the immune response and usually results in tissue damage due to high concentration of IFN-γ and TNF-α. In addition, degranulation of eosinophils, proteases and ROS of neutrophils cause tissue damage. The participation of immune response in disease progression is illustrated by red arrows. SARS-CoV-2 is reported to cause systemic infections of liver, kidneys, and blood vessels.
The cascade of host response against SARS-CoV-2 is initiated by tissue resident alveolar epithelial cells and macrophages by activation of host pattern-recognition receptors (PRRs) that detect the released virus-associated molecular patterns (PAMPs). This leads to a burst of local inflammation releasing pro-inflammatory cytokines and chemokines such as IL-6, IFN-γ, monocyte chemoattractant protein-1 (MCP-1), IL-2, IL-7, IL-10, granulocyte colony-stimulating factor (GM-CSF), IP-10, macrophage inflammatory protein 1α (MIP1-α), and tumor necrosis factor (TNF) [6,81]. These cytokines cause a T helper 1 (TH1) cell-polarized response by attracting immune cells, notably CD14+CD16+ inflammatory monocytes and T lymphocytes, from blood towards the infection site [6,82]. Uncontrollable inflammatory cell infiltration may lead to excessive lung damage through disproportionate release of proteases, reactive oxygen species, and TNF-α causing septic shock and multi-organ failure (Figure 3) [82].
Clinical data of 128 cases in Iran has shown an enhanced number and activity of CD8+ T cells rather than CD4+ T cell responses [83]. The detected virus-specific T cells were mostly central memory phenotype with high frequency of polyfunctional CD4+ and CD8+ T cells secreting IL-2, IFN-γ, and TNF-α. As a result of pro-inflammatory cytokine expression and the presence of nuclear antigens, T cells may trigger a second burst of inflammation at late disease stages [83,84].
Recent data from China demonstrated rapid reduction of T lymphocytes (both CD4+ and CD8+), HLA-DR, and CD38 double-positive fractions in the peripheral blood of SARS-CoV-2 infected patients. Moreover, there was an increased percentage of proinflammatory CCR6+ Th17 cells and an increased concentration of cytotoxic granules in CD8+ T cells [84]. Another group has reported that CD4+ T cells produced less IFN-γ in severe cases with no change in CD8+ T and NK cells [85]. C45RA+ naïve Tregs and memory CD45RO+ memory Tregs were found in low and high proportions, respectively. On recovery, there was a rapid restoration of CD3+, CD4+, and CD8+ T cells along with B and NK cell counts within 2–3 months [85]. Taken together, these changes in lymphocyte populations suggest dramatic dysregulation, evidence of T cell “exhaustion”, and shifts in the adaptive immune response to SARS-CoVs [84]. SARS-CoV-2 infected patients have also shown high levels of IL-1 beta, IFN-γ, IP-10, and MCP-1, which probably leads to activated T-helper-1 cell response and cytokine storm [85]. However, SARS-CoV-1 has been shown to induce pro-inflammatory and NK cells more significantly than SARS-CoV-2, which may explain the higher severity and mortality of the former [86].
Humoral immune response is crucial for virus neutralization and for providing a source of convalescent plasma to treat seriously-ill patients [86]. SARS-CoV-2 infection induces production of IgG against N protein starting from day 4, and IgM on the 9th day of disease onset. The class switching from IgM to IgG was detected in the second week [84]. Early production of neutralizing antibodies may be another factor contributing to organ damage and poor disease outcome. ADE through binding to Fcγ receptors may also contribute to persistent viral replication in immune cells and inflammatory responses causing tissue and organ damage; including acute respiratory distress syndrome (ARDS) [77]. Positive SARS-CoV-2 cases mostly mount an robust IgG antibody response in three or more weeks, which may protect against re-infection [87].
6. SARS-CoV-2 Related Organ Pathogenesis
SARS-CoV-2 virus predominantly infects lung epithelial alveolar cells causing severe pneumonia and occasionally leads to ARDS. Lower respiratory tract symptoms also include fever, dry cough, headache, dizziness, general weakness, vomiting, and diarrhea [88]. Autopsy reports of COVID-19 patients have shown diffuse alveolar impairment with hyaline membrane formation and immune cell infiltration in the alveoli [89]. Other organ systems such as kidneys, liver, intestine, heart, spleen, and brain are also affected in the course of SARS-CoV-2 infection and may induce more severe complications.
Acute kidney injury is a life-threating manifestation that may develop in seriously ill patients and often causes death. The potential mechanisms for such injury involve sepsis-causing cytokine storm and direct viral-mediated cellular injury. This may lead to impairment of gaseous exchange and development of secondary infections [89]. The mechanism by which SARS-CoV-2 induces liver injury remains unclear. However, it is predicted that the viral cytopathic effect and/or the immune-pathology induced by dysregulated inflammatory responses may be responsible for hepatomegaly, degeneration of hepatocytes, and inflammatory cell infiltration in liver [90].
In many recorded cases, gastrointestinal symptoms including nausea, vomiting, and diarrhea may develop. Some patients also experience altered mental status, reduced urine output, cold extremities, low blood pressure, and blotchy skin [91]. Spleen atrophy is often accompanied by necrosis, macrophage hyperplasia, and significant reduction in lymphocytes. Cardiac infection may trigger degeneration and necrosis of cardiomyocytes, and infiltration of monocytes, lymphocytes, and neutrophils in the myocardial interstitium. Sometimes, the brain demonstrates congestion, edema, and scattered neural-degeneration [88,89,91]. Individual with comorbidities such as kidney dysfunctions, hypertension, cancers, and diabetes mellitus are more prone to severe SARS-CoV-2 infections. Hypertension is the most common underlying disease in SARS-CoV-2 patients, followed by obesity and diabetes. However, chronic kidney disorders are usually associated with death in COVID-19 infected individuals [92]. The increased risk of COVID-19 severity in hypertension and diabetic individuals may be attributed to thrombotic complications [93]. In addition, thiazolidinedione, which is usually prescribed for diabetic patients, increases the expression of ACE2 receptor and thus promotes SARS-CoV-2 replication [92,94], similarly for cancer patients receiving immunosuppressive drugs due to enhanced SARS-CoV-2 replication [92].
7. Conclusions
SARS-CoV-2 is a newly emerged virus that has caused a major global pandemic in the 21st century with more than 40 million cases and 1 million deaths. The control measures and restrictions adopted have greatly impacted the economies of all countries worldwide. The virus is believed to have originated from bats and spread to humans via an ill-defined intermediate host. Human-to-human transmission principally occurs through direct inhalation of respiratory droplets and by touching contaminated surfaces. Although SARS-CoV-2 mainly affects the lungs, lesions may also develop in kidneys, liver, intestine, spleen, and brain. In many cases, a cytokine storm, which represents an exaggerated immune response against SAES-CoV-2 infection, exacerbates the disease consequence. Available knowledge regarding virus transmission, evolution, and immunopathogenesis is still lacking to provide a concrete basis for establishing proper and effective control strategies. At present, the scientific community is rushing to collect information on the virus and the disease, besides developing potent drugs, vaccines, and methodologies to reduce the extent of the pandemic on human health and economy.
Acknowledgments
We would like to thank King Saud University and Majmaah University for supporting this study.
Author Contributions
All authors contributed to the writing, review, and editing of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data is contained within the article.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Weiss S.R., Navas-Martin S. Coronavirus Pathogenesis and the Emerging Pathogen Severe Acute Respiratory Syndrome Coronavirus. Microbiol. Mol. Biol. Rev. 2005;69:635–664. doi: 10.1128/MMBR.69.4.635-664.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Assiri A., Al-Tawfiq J.A., Al-Rabeeah A.A., Al-Rabiah F.A., Al-Hajjar S., Al-Barrak A., Memish Z.A. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: A descriptive study. Lancet Infect. Dis. 2013;13:752–761. doi: 10.1016/S1473-3099(13)70204-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shang J., Ye G., Shi K., Wan Y., Luo C., Aihara H., Li F. Structural basis of receptor recognition by SARS-CoV-2. Nature. 2020;581:221–224. doi: 10.1038/s41586-020-2179-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.COVID-19 situation reports. [(accessed on 5 January 2020)]; Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 5.Rossi G.A., Sacco O., Mancino E., Cristiani L., Midulla F. Differences and similarities between SARS-CoV and SARS-CoV-2: Spike receptor-binding domain recognition and host cell infection with support of cellular serine proteases. Infection. 2020;48:665–669. doi: 10.1007/s15010-020-01486-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yadav T., Saxena S.K. Coronavirus Disease 2019 (COVID-19) Springer; Singapore: 2020. Transmission Cycle of SARS-CoV and SARS-CoV-2; pp. 33–42. [DOI] [Google Scholar]
- 7.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ayittey F.K., Ayittey M.K., Chiwero N.B., Kamasah J.S., Dzuvor C. Economic impacts of Wuhan 2019-nCoV on China and the world. J. Med. Virol. 2020;92:473–475. doi: 10.1002/jmv.25706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Song Z., Xu Y., Bao L., Zhang L., Yu P., Qu Y., Zhu H., Zhao W., Han Y., Qin C. From SARS to MERS, Thrusting Coronaviruses into the Spotlight. Viruses. 2019;11:59. doi: 10.3390/v11010059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sawicki S.G. Viral Genome Replication. Springer; Boston, MA, USA: 2008. Coronavirus Genome Replication; pp. 25–39. [DOI] [Google Scholar]
- 11.Li Y., Li H., Fan R., Wen B., Zhang J., Cao X., Wang C., Song Z., Li S., Li X., et al. Coronavirus Infections in the Central Nervous System and Respiratory Tract Show Distinct Features in Hospitalized Children. Intervirology. 2016;59:163–169. doi: 10.1159/000453066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tang Q., Song Y., Shi M., Cheng Y., Zhang W., Xia X.-Q. Inferring the hosts of coronavirus using dual statistical models based on nucleotide composition. Sci. Rep. 2015;5:17155. doi: 10.1038/srep17155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chan J.F., Kok K.H., Zhu Z., Chu H., To K.K., Yuan S., Yuen K.Y. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg. Microbes Infect. 2020;9:221–236. doi: 10.1080/22221751.2020.1719902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang H., Li X., Li T., Zhang S., Wang L., Wu X., Liu J. The genetic sequence, origin, and diagnosis of SARS-CoV-2. Eur. J. Clin. Microbiol. Infect. Dis. 2020;39:1629–1635. doi: 10.1007/s10096-020-03899-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haan C.A.M.D., Rottier P.J.M. Hosting the severe acute respiratory syndrome coronavirus: Specific cell factors required for infection. Cell Microbiol. 2006;8:1211–1218. doi: 10.1111/j.1462-5822.2006.00744.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lu R., Zhao X., Li J., Niu P., Yang B., Wu H., Wang W., Song H., Huang B., Zhu N., et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu A., Peng Y., Huang B., Ding X., Wang X., Niu P., Meng J., Zhu Z., Zhang Z., Wang J., et al. Genome Composition and Divergence of the Novel Coronavirus (2019-nCoV) Originating in China. Cell Host Microbe. 2020;27:325–328. doi: 10.1016/j.chom.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paraskevis D., Kostaki E.G., Magiorkinis G., Panayiotakopoulos G., Sourvinos G., Tsiodras S. Full-genome evolutionary analysis of the novel corona virus (2019-nCoV) rejects the hypothesis of emergence as a result of a recent recombination event. Infect. Genet. Evol. J. Mol. Epidemiol. Evol. Genet. Infect. Dis. 2020;79:104212. doi: 10.1016/j.meegid.2020.104212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rehman S.U., Shafique L., Ihsan A., Liu Q. Evolutionary Trajectory for the Emergence of Novel Coronavirus SARS-CoV-2. Pathogens. 2020;9:240. doi: 10.3390/pathogens9030240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guan Y., Zheng B.J., He Y.Q., Liu X.L., Zhuang Z.X., Cheung C.L., Luo S.W., Li P.H., Zhang L.J., Guan Y.J., et al. Isolation and characterization of viruses related to the SARS coronavirus from animals in southern China. Science. 2003;302:276–278. doi: 10.1126/science.1087139. [DOI] [PubMed] [Google Scholar]
- 21.Haagmans B.L., Al Dhahiry S.H., Reusken C.B., Raj V.S., Galiano M., Myers R., Godeke G.J., Jonges M., Farag E., Diab A., et al. Middle East respiratory syndrome coronavirus in dromedary camels: An outbreak investigation. Lancet Infect. Dis. 2014;14:140–145. doi: 10.1016/S1473-3099(13)70690-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xiao K., Zhai J., Feng Y., Zhou N., Zhang X., Zou J., Li N., Guo Y., Li X., Shen X., et al. Isolation of SARS-CoV-2-related coronavirus from Malayan pangolins. Nature. 2020;583:286–289. doi: 10.1038/s41586-020-2313-x. [DOI] [PubMed] [Google Scholar]
- 23.Zhang T., Wu Q., Zhang Z. Probable Pangolin Origin of SARS-CoV-2 Associated with the COVID-19 Outbreak. Curr. Biol. 2020;30:1346–1351. doi: 10.1016/j.cub.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shi J., Wen Z., Zhong G., Yang H., Wang C., Huang B., Liu R., He X., Shuai L., Sun Z., et al. Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS–coronavirus 2. Science. 2020;368:1016–1020. doi: 10.1126/science.abb7015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mandary M.B., Masomian M., Poh C.L. Impact of RNA Virus Evolution on Quasispecies Formation and Virulence. Int. J. Mol. Sci. 2019;20:4657. doi: 10.3390/ijms20184657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Holland L.A., Kaelin E.A., Maqsood R., Estifanos B., Wu L., Varsani A., Halden R.U., Hogue B.G., Scotch M., Lim E.S., et al. An 81 nucleotide deletion in SARS-CoV-2 ORF7a identified from sentinel surveillance in Arizona (Jan–Mar 2020) J. Virol. 2020 doi: 10.1128/JVI.00711-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taylor J.K., Coleman C.M., Postel S., Sisk J.M., Bernbaum J.G., Venkataraman T., Sundberg E.J., Frieman M.B. Severe Acute Respiratory Syndrome Coronavirus ORF7a Inhibits Bone Marrow Stromal Antigen 2 Virion Tethering through a Novel Mechanism of Glycosylation Interference. J. Virol. 2015;89:11820–11833. doi: 10.1128/JVI.02274-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tan Y., Tan T., Lee M., Tham P., Gunalan V., Druce J., Birch C., Catton M., Fu N., Yu N., et al. Induction of Apoptosis by the Severe Acute Respiratory Syndrome Coronavirus 7a Protein Is Dependent on Its Interaction with the Bcl-XL Protein. J. Virol. 2007;81:6346–6355. doi: 10.1128/JVI.00090-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Su Y., Anderson D., Young B.E., Zhu F., Linster M., Kalimuddin S., Low J., Yan Z., Jayakumar J., Sun L., et al. Discovery of a 382-nt deletion during the early evolution of SARS-CoV-2. bioRxiv. 2020 doi: 10.1101/2020.03.11.987222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Muth D., Corman V.M., Roth H., Binger T., Dijkman R., Theresa L., Florian G.G., Balboni A., Battilani M., Rihtarič D., et al. Attenuation of replication by a 29 nucleotide deletion in SARS-coronavirus acquired during the early stages of human-to-human transmission. Sci. Rep. 2018;8:15177. doi: 10.1038/s41598-018-33487-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Young B.E., Fong S.W., Chan Y.H., Mak T., Ang L.W., Anderson D.E., Lee C.Y., Amrun N., Lee B., Goh Y.G., et al. Effects of a major deletion in the SARS-CoV-2 genome on the severity of infection and the inflammatory response: An observational cohort study. Lancet. 2020;396:603–611. doi: 10.1016/S0140-6736(20)31757-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jewell B.L. Monitoring differences between the SARS-CoV-2 B.1.1.7 variant and other lineages. Lancet. 2021;6:E267–E268. doi: 10.1016/S2468-2667(21)00073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hoffmann M., Arora P., Groß R., Seidel A., Hörnich B.F., Hahn A.S., Krüger N., Graichen L., Hofmann-Winkler H., Kempf A., et al. SARS-CoV-2 variants B.1.351 and P.1 escape from neutralizing antibodies. Cell. 2021;184:2384–2393.e2312. doi: 10.1016/j.cell.2021.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Burki T. Understanding variants of SARS-CoV-2. Lancet. 2021;397:462. doi: 10.1016/S0140-6736(21)00298-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karim S.S.A. Vaccines and SARS-CoV-2 variants: The urgent need for a correlate of protection. Lancet. 2021;397:1263–1264. doi: 10.1016/S0140-6736(21)00468-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bian L., Gao F., Zhang J., He Q., Mao Q., Xu M., Liang Z. Effects of SARS-CoV-2 variants on vaccine efficacy and response strategies. Expert Rev. Vaccines. 2021 doi: 10.1080/14760584.2021.1903879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vijgen L., Keyaerts E., Lemey P., Maes P., Van K., Nauwynck H., Pensaert M., Van Ranst M. Evolutionary history of the closely related group 2 coronaviruses: Porcine hemagglutinating encephalomyelitis virus, bovine coronavirus, and human coronavirus OC43. J. Virol. 2006;80:7270–7274. doi: 10.1128/JVI.02675-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alekseev K.P., Vlasova A.N., Jung K., Hasoksuz M., Zhang X., Halpin R., Wang S., Ghedin E., Spiro D., Saif L.J., et al. Bovine-Like Coronaviruses Isolated from Four Species of Captive Wild Ruminants Are Homologous to Bovine Coronaviruses, Based on Complete Genomic Sequences. J. Virol. 2008;82:12422–12431. doi: 10.1128/JVI.01586-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vijgen L., Keyaerts E., Moës E., Thoelen I., Wollants E., Lemey P., Vandamme A.M., Van Ranst M. Complete genomic sequence of human coronavirus OC43: Molecular clock analysis suggests a relatively recent zoonotic coronavirus transmission event. J. Virol. 2005;79:1595–1604. doi: 10.1128/JVI.79.3.1595-1604.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pfefferle S., Oppong S., Drexler J.F., Gloza-Rausch F., Ipsen A., Seebens A., Müller M.A., Annan A., Vallo P., Adu-Sarkodie Y., et al. Distant Relatives of Severe Acute Respiratory Syndrome Coronavirus and Close Relatives of Human Coronavirus 229E in Bats, Ghana. Emerg. Infect. Dis. 2009;15:1377–1384. doi: 10.3201/eid1509.090224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li F. Structure, Function, and Evolution of Coronavirus Spike Proteins. Annu. Rev. Virol. 2016;3:237–261. doi: 10.1146/annurev-virology-110615-042301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wong S.K., Li W., Moore M.J., Choe H., Farzan M. A 193-amino acid fragment of the SARS coronavirus S protein efficiently binds angiotensin-converting enzyme 2. J. Biol. Chem. 2004;279:3197–3201. doi: 10.1074/jbc.C300520200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Du L., Zhao G., Kou Z., Ma C., Sun S., Poon V.K., Lu L., Wang L., Debnath A.K., Zheng B.J., et al. Identification of a receptor-binding domain in the S protein of the novel human coronavirus Middle East respiratory syndrome coronavirus as an essential target for vaccine development. J. Virol. 2013;87:9939–9942. doi: 10.1128/JVI.01048-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hofmann H., Pyrc K., van der Hoek L., Geier M., Berkhout B., Pöhlmann S. Human coronavirus NL63 employs the severe acute respiratory syndrome coronavirus receptor for cellular entry. Proc. Natl. Acad. Sci. USA. 2005;102:7988–7993. doi: 10.1073/pnas.0409465102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hofmann H., Simmons G., Rennekamp A.J., Chaipan C., Gramberg T., Heck E., Geier M., Wegele A., Marzi A., Bates P., et al. Highly Conserved Regions within the Spike Proteins of Human Coronaviruses 229E and NL63 Determine Recognition of Their Respective Cellular Receptors. J. Virol. 2006;80:8639–8652. doi: 10.1128/JVI.00560-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Delmas B., Gelfi J., L’Haridon R., Vogelt L.K., Sjostromt H., Norent O., Laude H. Aminopeptidase N is a major receptor for the enteropathogenic coronavirus TGEV. Nature. 1992;357:417–420. doi: 10.1038/357417a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu C., Tang J., Ma Y., Liang X., Yang Y., Peng G., Qi Q., Jiang S., Li J., Du L., et al. Receptor usage and cell entry of porcine epidemic diarrhea coronavirus. J. Virol. 2015;89:6121–6125. doi: 10.1128/JVI.00430-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Delmas B., Gelfi J., Sjöström H., Noren O., Laude H. Further Characterization of Aminopeptidase-N as a Receptor for Coronaviruses. In: Laude H., Vautherot J.-F., editors. Coronaviruses: Molecular Biology and Virus-Host Interactions. Springer; Boston, MA, USA: 1993. pp. 293–298. [DOI] [PubMed] [Google Scholar]
- 49.Raj V.S., Mou H., Smits S.L., Dekkers D.H., Müller M.A., Dijkman R., Muth D., Demmers A., Zaki A., Fouchier R.M., et al. Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC. Nature. 2013;495:251–254. doi: 10.1038/nature12005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Williams R.K., Jiang G.S., Holmes K.V. Receptor for mouse hepatitis virus is a member of the carcinoembryonic antigen family of glycoproteins. Proc. Natl. Acad. Sci. USA. 1991;88:5533–5536. doi: 10.1073/pnas.88.13.5533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schultze B., Gross H.J., Brossmer R., Herrler G. The S protein of bovine coronavirus is a hemagglutinin recognizing 9-O-acetylated sialic acid as a receptor determinant. J. Virol. 1991;65:6232–6237. doi: 10.1128/jvi.65.11.6232-6237.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Li W., Moore M.J., Vasilieva N., Sui J., Wong S.K., Berne M.A., Somasundaran M., Sullivan J.L., Luzuriaga K., Greenough T.C., et al. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Walls A.C., Park Y.-J., Tortorici M.A., Wall A., McGuire A.T., Veesler D. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell. 2020;181:281–292.e6. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schultze B., Cavanagh D., Herrler G. Neuraminidase treatment of avian infectious bronchitis coronavirus reveals a hemagglutinating activity that is dependent on sialic acid-containing receptors on erythrocytes. Virology. 1992;189:792–794. doi: 10.1016/0042-6822(92)90608-R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Li F. Receptor recognition and cross-species infections of SARS coronavirus. Antiviral. Res. 2013;100:246–254. doi: 10.1016/j.antiviral.2013.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Braun E., Sauter D. Furin-mediated protein processing in infectious diseases and cancer. Clin. Transl. Immunol. 2019;8:e1073. doi: 10.1002/cti2.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Claas E.C., Osterhaus A.D., van Beek R., Jong J.C., Rimmelzwaan G.F., Senne D.A., Krauss S., Shortridge K.F., Webster R.G. Human influenza A H5N1 virus related to a highly pathogenic avian influenza virus. Lancet Lond Engl. 1998;351:472–477. doi: 10.1016/S0140-6736(97)11212-0. [DOI] [PubMed] [Google Scholar]
- 58.Izaguirre G. The Proteolytic Regulation of Virus Cell Entry by Furin and Other Proprotein Convertases. Viruses. 2019;11:837. doi: 10.3390/v11090837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yamada Y., Liu D.X. Proteolytic activation of the spike protein at a novel RRRR/S motif is implicated in furin-dependent entry, syncytium formation, and infectivity of coronavirus infectious bronchitis virus in cultured cells. J. Virol. 2009;83:8744–8758. doi: 10.1128/JVI.00613-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cheng J., Zhao Y., Xu G., Zhang K., Jia W., Sun Y., Zhao J., Xue J., Hu Y., Zhang G. The S2 Subunit of QX-type Infectious Bronchitis Coronavirus Spike Protein Is an Essential Determinant of Neurotropism. Viruses. 2019;11:972. doi: 10.3390/v11100972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wang Q., Zhang Y., Wu L., Niu C., Song Z., Zhang G., Lu C., Qiao Y., Hu K., Yuen Y., et al. Structural and Functional Basis of SARS-CoV-2 Entry by Using Human ACE2. Cell. 2020;181:894–904.e9. doi: 10.1016/j.cell.2020.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shang J., Wan Y., Luo C., Ye G., Geng Q., Auerbach A., Li F. Cell entry mechanisms of SARS-CoV-2. Proc. Natl. Acad. Sci. USA. 2020;117:11727–11734. doi: 10.1073/pnas.2003138117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yuan Y., Cao D., Zhang Y., Ma J., Qi J., Wang Q., Lu G., Wu Y., Yan J., Shi Y., et al. Cryo-EM structures of MERS-CoV and SARS-CoV spike glycoproteins reveal the dynamic receptor binding domains. Nat. Commun. 2017;8:15092. doi: 10.1038/ncomms15092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Correia G., Rodrigues L., Gameiro da Silva M., Gonçalves T. Airborne route and bad use of ventilation systems as non-negligible factors in SARS-CoV-2 transmission. Med. Hypotheses. 2020;141:109781. doi: 10.1016/j.mehy.2020.109781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Guo Y.-R., Cao Q.-D., Hong Z.S., Tan Y., Chen S., Jin H., Tan K., Wang D., Yan Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak-an update on the status. Mil. Med. Res. 2020;7:11. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Meselson M. Droplets and Aerosols in the Transmission of SARS-CoV-2. N. Engl. J. Med. 2020;382:2063. doi: 10.1056/NEJMc2009324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Xiao S., Li Y., Wong T., Hui D.S.C. Role of fomites in SARS transmission during the largest hospital outbreak in Hong Kong. PLoS ONE. 2017;12 doi: 10.1371/journal.pone.0181558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhou J., Li C., Zhao G., Chu H., Wang D., Yan H.H., Poon V.K., Wen L., Wong B.H., Zhao X., et al. Human intestinal tract serves as an alternative infection route for Middle East respiratory syndrome coronavirus. Sci. Adv. 2017;3:eaao4966. doi: 10.1126/sciadv.aao4966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wang W., Xu Y., Gao R., Lu R., Han K., Wu G., Tan W. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA. 2020;323:1843–1844. doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Knowlton S.D., Boles C.L., Perencevich E.N., Diekema D.J., Nonnenmann M.W., CDC Epicenters Program Bioaerosol concentrations generated from toilet flushing in a hospital-based patient care setting. Antimicrob. Resist. Infect. Control. 2018;7:16. doi: 10.1186/s13756-018-0301-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zeng H., Xu C., Fan J., Tang Y., Deng Q., Zhang W., Long X. Antibodies in Infants Born to Mothers With COVID-19 Pneumonia. JAMA. 2020;323:1848–1849. doi: 10.1001/jama.2020.4861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zeng L., Xia S., Yuan W., Yan K., Xiao F., Shao J., Zhou W. Neonatal Early-Onset Infection With SARS-CoV-2 in 33 Neonates Born to Mothers With COVID-19 in Wuhan, China. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.0878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wei W.E. Presymptomatic Transmission of SARS-CoV-2—Singapore, January 23–March 16, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69 doi: 10.15585/mmwr.mm6914e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fiorillo L., Cervino G., Matarese M., D’Amico C., Surace G., Paduano V., Fiorillo M.T., Moschella A., Bruna A., Romano G.L., et al. COVID-19 Surface Persistence: A Recent Data Summary and Its Importance for Medical and Dental Settings. Int. J. Environ. Res. Public Health. 2020;17:3132. doi: 10.3390/ijerph17093132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chin A.W.H., Chu J.T.S., Perera M.R.A., Hui K.P.Y., Yen H.-L., Chan M.C.W., Peiris M., Poon L.L.M. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe. 2020;1:e10. doi: 10.1016/S2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Felsenstein S., Herbert J.A., McNamara P.S., Hedrich C.M. COVID-19: Immunology and treatment options. Clin. Immunol. 2020;215:108448. doi: 10.1016/j.clim.2020.108448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Prompetchara E., Ketloy C., Palaga T. Immune responses in COVID-19 and potential vaccines: Lessons learned from SARS and MERS epidemic. Asian Pac. J. Allergy Immunol. 2020;38:1–9. doi: 10.12932/ap-200220-0772. [DOI] [PubMed] [Google Scholar]
- 78.Ben Addi A., Lefort A., Hua X., Libert F., Communi D., Ledent C., Macours P., Tilley S.L., Boeynaems J.M., Robaye B. Modulation of murine dendritic cell function by adenine nucleotides and adenosine: Involvement of the A(2B) receptor. Eur. J. Immunol. 2008;38:1610–1620. doi: 10.1002/eji.200737781. [DOI] [PubMed] [Google Scholar]
- 79.De Wit E., Van Doremalen N., Falzarano D., Munster V.J. SARS and MERS: Recent insights into emerging coronaviruses. Nat. Rev. Microbiol. 2016;14:523–534. doi: 10.1038/nrmicro.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhao Y., Zhao Z., Wang Y., Zhou Y., Ma Y., Zuo W. Single-cell RNA expression profiling of ACE2, the putative receptor of Wuhan 2019-nCov. bioRxiv. 2020 doi: 10.1101/2020.01.26.919985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhang B., Zhou X., Qiu Y., Feng F., Feng J., Jia Y., Zhu H., Hu K., Liu J., Liu Z., et al. Clinical characteristics of 82 death cases with COVID-19. medRxiv. doi: 10.1101/2020.02.26.20028191. [DOI] [Google Scholar]
- 82.Qin C., Zhou L., Hu Z., Zhang S., Yang S., Tao Y., Xie C., Ma K., Shang K., Wang W., et al. Dysregulation of Immune Response in Patients With Coronavirus 2019 (COVID-19) in Wuhan, China. Clin. Infect. Dis. 2020;71 doi: 10.1093/cid/ciaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rokni M., Ghasemi V., Tavakoli Z. Immune responses and pathogenesis of SARS-CoV-2 during an outbreak in Iran: Comparison with SARS and MERS. Rev. Med. Virol. 2020;30:e2107. doi: 10.1002/rmv.2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhu H., Rhee J.-W., Cheng P., Waliany S., Chang A., Witteles R.M., Maecker H., Davis M.M., Nguyen P.K., Wu S.M., et al. Cardiovascular Complications in Patients with COVID-19: Consequences of Viral Toxicities and Host Immune Response. Curr. Cardiol. Rep. 2020;22:32. doi: 10.1007/s11886-020-01292-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., Liu S., Zhao P., Liu H., Zhu L., et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rojas M., Rodríguez Y., Monsalve D.M., Acosta-Ampudia Y., Camacho B., Gallo J.E., Rojas-Villarraga A., Ramírez-Santana C., Díaz-Coronado J.C., Manrique R., et al. Convalescent plasma in Covid-19: Possible mechanisms of action. Autoimmun. Rev. 2020;19:102554. doi: 10.1016/j.autrev.2020.102554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wajnberg A., Mansour M., Leven E., Bouvier N.M., Patel G., Firpo A., Mendu R., Jhang J., Arinsburg S., Gitman M., et al. Humoral immune response and prolonged PCR positivity in a cohort of 1343 SARS-CoV 2 patients in the New York City region. medRxiv. 2020 doi: 10.1101/2020.04.30.20085613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Yuki K., Fujiogi M., Koutsogiannaki S. COVID-19 pathophysiology: A review. Clin. Immunol. 2020;215:108427. doi: 10.1016/j.clim.2020.108427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Fanelli V., Fiorentino M., Cantaluppi V., Gesualdo E.L., Stallone G., Ronco C., Castellano G. Acute kidney injury in SARS-CoV-2 infected patients. Crit. Care. 2020;24:155. doi: 10.1186/s13054-020-02872-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Li H., Liu L., Zhang D., Xu J., Dai H., Tang N., Su X., Calo B. SARS-CoV-2 and viral sepsis: Observations and hypotheses. Lancet. 2020;395:1517–1520. doi: 10.1016/S0140-6736(20)30920-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zhou M., Zhang X., Qu J. Coronavirus disease 2019 (COVID-19): A clinical update. Front. Med. 2020;14:126–135. doi: 10.1007/s11684-020-0767-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ng W.H., Tipih T., Makoah N.A., Vermeulen J.G., Goedhals D., Sempa J.B., Burt F.J., Taylor A., Mahalingam S. Comorbidities in SARS-CoV-2 Patients: A Systematic Review and Meta-Analysis. mBio. 2021;12:1. doi: 10.1128/mBio.03647-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Peng Y.H., Lin Y.S., Chen C.H., Tsai K.Y., Hung Y.C., Chen H.J., Liao W.C., Ho W.C. Type 1 diabetes is associated with an increased risk of venous thromboembolism: A retrospective population-based cohort study. PLoS ONE. 2020;15:e0226997. doi: 10.1371/journal.pone.0226997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zhang W., Xu Y.Z., Liu B., Wu R., Yang Y.Y., Xiao X.Q., Zhang X. Pioglitazone upregulates angiotensin converting enzyme 2 expression in insulin-sensitive tissues in rats with high-fat diet-induced nonalcoholic steatohepatitis. Sci. World J. 2014;2014:603409. doi: 10.1155/2014/603409. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is contained within the article.