Abstract
Introduction
Engaging communities and intended beneficiaries at various stages of health research is a recommended practice. The contribution of community engagement to non-communicable disease research in low- and middle-income countries has not yet been extensively studied or synthesised. This protocol describes the steps towards generating an understanding of community engagement in the context of non-communicable disease research, prevention and health promotion using a realist review approach. A realist lens enables a rich explanatory approach to causation while capturing complexity, and an openness to multiple outcomes, including unintended consequences. The review will thus develop an understanding of community engagement without assuming that such practices result in more ethical research or effective interventions.
Methods and analysis
We propose a realist approach aiming to examine how, why, under what circumstances and for whom community engagement works or does not work. The iterative review steps include clarifying the review scope; searching for evidence; appraising studies and extracting data; synthesising evidence and drawing conclusions; and disseminating, implementing and evaluating the findings. Principles of meta-narrative review (pragmatism, pluralism, historicity, contestation, reflexivity and peer review) are employed to ensure practicable and contextualised review outputs. The proposed review will draw on theoretical and empirical literature beyond specific diseases or settings, but with a focus on informing non-communicable disease research and interventions in low- and middle-income countries. The synthesis of existing literature will be complemented by qualitative realist interviews and stakeholder consultation. Through drawing on multiple types of evidence and input from both experts and intended beneficiaries, the review will provide critical and pragmatic insights for research and community engagement in low- and middle-income countries.
Ethics and dissemination
Ethical approval has been obtained from the University of the Witwatersrand. Dissemination will include traditional academic channels, institutional communications, social media and discussions with a wide range of stakeholders.
Keywords: public health, ethics (see medical ethics), preventive medicine
Strengths and limitations of this study.
The realist review approach will provide novel explanatory evidence, transcending mere descriptions to unearth what mechanisms and contextual elements are at play to achieve meaningful community engagement with non-communicable disease research in low- and middle-income countries.
The review will integrate information obtained from multiple sources to develop robust explanatory models on the specifics of interventions and research around non-communicable diseases.
The protocol draws on the meta-narrative review principles of pragmatism, pluralism, historicity, contestation, reflexivity and peer review to ensure a rich and rigorous synthesis.
Effective stakeholder engagement with a diverse range of stakeholders is limited by the COVID-19 pandemic.
A realist review cannot produce an exhaustive account of all contexts, mechanisms and outcomes of potential relevance to non-communicable disease prevention.
Introduction
Community engagement
The concept and practices of community engagement can be traced back to the pursuit of participatory approaches in scientific research from the 1960s onwards, particularly in the fields of global health and international development.1 In the context of health research, community engagement can be viewed as a strategy for building and maintaining 'relationships between researchers and the stakeholder community—the unique collection of diverse stakeholders who have interests in the conduct and/or outcomes of a given research project'.2 Community engagement is, however, used to refer to a multitude of practices, and the concept is somewhat ambiguous when it comes to both terms: ‘community’ and ‘engagement’.3–5 Communities can, for example, consist of intended beneficiaries, residents of a particular geographical area, or a group of individuals with shared interests or connected identities. However, researchers and the perceived communities may have rather different ways of understanding of what constitutes a community, and who belongs to it.6 Engagement can mean: minimal outreach with limited involvement from stakeholders, mostly with the purpose of providing them information about the research; consultation with some input from stakeholders to researchers; stakeholder and participant involvement at different stages of research; different forms of collaboration; and most comprehensively, shared leadership with a strong bidirectional relationship between stakeholders and researchers.7 In practice, the involvement of non-academic stakeholders through practices such as community engagement or participatory methods plays an important role in public health research and interventions; and large funding bodies are increasingly emphasising community or public engagement when awarding grants for large trials.2 7–9
Guidance for developing and evaluating complex public health interventions recommends involving intended beneficiaries and other relevant stakeholders throughout the process.10 11 Approaches such as co-design or co-production are gaining popularity, at least within the jargon used to describe intervention research.12 While there are many ethical and practical reasons13 to promote the participation of community members and stakeholders in different phases of research, intervention development, implementation and dissemination, there are also numerous reasons for individuals or communities to not want to engage with research either as participants or in advisory roles. Moreover, those individuals or groups who do participate actively in shaping research questions or guiding intervention design bring with them their own agendas, which may or may not align with other intended outcomes of research and interventions.
In recognition of this complexity, Abimbola14 calls for a move beyond a positive a priori bias in favour of community engagement, which typically involves assumptions that people want to participate in decision-making about their health, and that community engagement will generally lead to favourable outcomes. These assumptions are particularly important to question in the context of non-communicable disease (NCD) prevention, which is less visibly characterised by civil society activism and community-led responses than, for example, HIV/AIDS.15 16 Indeed, although NCDs are the leading causes of morbidity and mortality worldwide, and increasingly so in low- and middle-income countries (LMICs), the prevention of NCDs has tended to be deprioritised vis-à-vis problems perceived as more acute and urgent.17
Previous research on community engagement and participatory research approaches indicates that trust and power-sharing between researchers and communities,18 19 and expected or tangible benefits received by the community,20 play a role in contributing towards how appealing engagement is from the point of view of potential participants and targeted communities. Furthermore, factors such as resource constraints, varying levels of education, existing inequalities, historical tensions, or even a history of harm done under the guise of public health research, are bound to influence people’s willingness and ability to engage with research or interventions.14 19–21 It is, therefore, important to examine how different approaches to community engagement, from purely researcher-led to more community-centred or transformative practices with more power-sharing, may have different outcomes in terms of ethics, effectiveness, scalability and sustainability.7 22–24
As described by Adhikari et al,3 the goals of community engagement in health research can broadly be divided into research-related and ethical outcomes, although there are notably also overlaps between these categories. For example, enhancing participant recruitment and ensuring retention are predominantly research-related goals of community engagement, while supporting the consent process can be seen as both an ethical and a research-related goal. In practice, without deliberate effort,2 even the ethical goals of community engagement, such as minimising risks, burdens and exploitation, may not go much beyond institutional demands for research ethics, which do not necessarily capture community interests beyond minimising obvious harms.25 Indeed, it is important to acknowledge that community engagement itself can be harmful or contribute to harmful research.20 This review will, therefore, explore an understanding of the contexts and mechanisms that can produce harmful outcomes, and those that can protect participants and communities from harm.
NCD prevention and community engagement in LMICs
NCDs comprise a huge variety of diseases and conditions to which over 70% of the global burden of mortality can be attributed.26 Globally, a vast majority of NCD-related deaths occur in LMICs that are seeing a shift from predominantly communicable diseases and childhood illnesses to a disease burden characterised mostly by NCDs.27 An increased focus on NCD prevention, management and treatment has been seen in both research and policy, but funding priorities still often reflect a focus on specific communicable diseases.28 29
If health promotion is seen as 'the process of empowering people to increase control over their health and its determinants',30 community engagement and participatory approaches are suitable elements for research that aims to prevent NCDs and promote health. However, due to the prevailing perceptions in many settings that NCDs are ‘lifestyle’ illnesses, non-urgent or self-inflicted,17 and the often relatively asymptomatic nature of some NCDs such as hypertension,31 it can be expected that interest for engaging with NCD prevention efforts may be limited among communities affected by NCDs. Indeed, qualitative evidence from South Africa suggests that the immediacy of concerns such as unemployment, safety and food insecurity understandably mean that potential future health outcomes are low on many people’s agendas, and ‘health and its determinants’ are not under individuals’ direct control due to socioeconomic and structural constraints.32–34
Nevertheless, there are also examples of successful engagement of communities in addressing NCDs in LMIC settings. A community-based diabetes prevention trial in Bangladesh found participatory learning and action groups to be an effective intervention to prevent type 2 diabetes, while also using methods such as participatory visual analysis to engage participants in interpreting the results of the trial.35–37 Similarly, a successful community-based mental health intervention called the ‘Friendship Bench’ was developed in Zimbabwe following community stakeholders’ call for an intervention.38 39 Globally, civil society actors play a pivotal role in involving community voices and the lived experience of people with NCDs in campaigns and advocacy demanding government action on NCDs.40
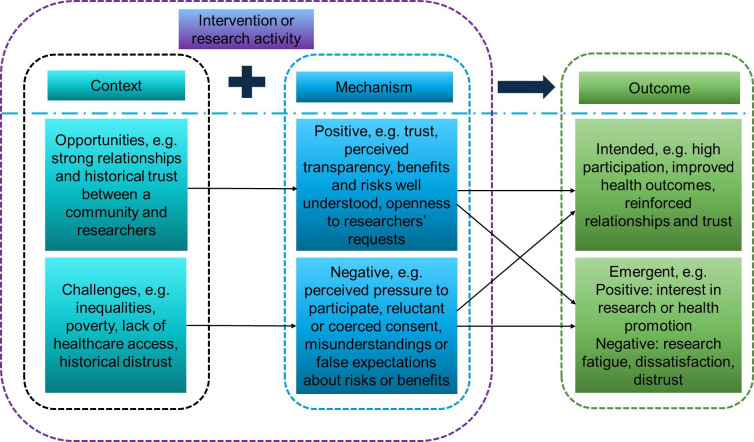
For the purposes of this review, community engagement is conceptualised as a part of NCD research or interventions rather than an intervention or programme on its own. Research or interventions can take place without community engagement, and communities can carry out activities without any connection to research or interventions. In this sense, community engagement can be viewed as a bridge41 that connects research or interventions to a community. As illustrated in figure 1, community-based interventions without community engagement (figure 1A) can have both intended and emergent outcomes. With community engagement (figure 1B), the same is true, but the range of different potential outcomes may be wider due to the added element of community engagement.
Figure 1.

The role of community engagement in health interventions.
Critical realism and realist reviews
Critical realism is a philosophical framework that draws on elements of positivist and interpretivist paradigms to propose an understanding of social activity whereby both social structure (an organised set of social institutions and patterns of institutionalised relationships) and agency (thoughts and actions taken by people) find a place.42 43 Critical realism as a research paradigm involves a multilayered view of reality (see table 1), hypothesising the existence of mechanisms (underlying entities that can cause an event to occur) that produce social events, whether these are observed or not.44 Realist methodology, building on critical realism through an interpretation originally referred to as scientific realism,45 is increasingly used to evaluate public health interventions while maintaining an openness to both intended and unintended outcomes. It enables in-depth analyses of different causal mechanisms at play in generating those outcomes and in tandem consideration of contextual elements that (dis)activate these mechanisms.46
Table 1.
Key concepts
| Concept | Definition |
| Critical realism | A philosophical framework that combines positivist (the paradigm underpinning natural sciences) and interpretivist (a paradigm that emphasises experiences and interpretations over the ‘objective’ truth assumed by positivism) understanding of the world.65 Of particular relevance to realist research is the concept of ontological depth,49 depicting a stratified reality with three layers: the empirical (things and events that are observed); the actual (things that exist and events that occur but are not observed); and the real (mechanisms that are not directly observable but can potentially cause events to occur).43 62 65 |
| Scientific realism | An approach to theory development and testing that draws on critical realism, and makes use of realist concepts and methods, such as retroduction.45 This is the original framework underpinning realist evaluation and reviews,45 66 but applications of scientific realism and interpretations of the relationship between scientific and critical realism are varied and contested in the field of realist evaluation.51 |
| Realist review | A theory-driven and iterative approach to reviewing and synthesising literature in order to provide an explanation of how, why, for whom and under what circumstances programmes, policies and interventions work or do not work.47 48 |
| Programme theory | Theories that link activities and outcomes to explain how and why a change is expected to take place, representing how the mechanisms introduced into pre-existing contexts can generate outcomes.48 67 |
| Context (C) | The conditions (eg, individual, organisational and environmental features), historical elements or relational and dynamic features that can potentially (dis)activate existing or introduced mechanisms.48 49 68 This is not the same as ‘setting’ or ‘context’ in a generic sense of providing background information, and only captures those aspects of the context that have a bearing on mechanisms and outcomes. |
| Mechanism (M) | An underlying entity that produces specific outcomes in specific contexts. Mechanisms are a combination of resources (eg, components of an intervention) and responses (eg, the perceptions of participants) highlighting the importance of examining how interventions are received as opposed to merely considering how they are intended.48 49 |
| Outcome (O) | Expected or actual change achieved by the combination of specific contexts and mechanisms.48 49 |
| Context–mechanism–outcome (CMO) configuration | CMO configurations are representations of a causal relationship between contexts and mechanisms that lead to specific outcomes.49 50 |
| Community engagement in research | A strategy for building and maintaining relationships between researchers and the communities the research concerns, or who are intended to benefit from interventions or research findings.2 |
| Participatory research | A research approach that involves research participants at different stages of the research process, for example, study design, planning and analysis, rather than merely as informants or recipients of an intervention. Many different methods, such as visual participatory analysis, exist under this general approach.36 |
| Health promotion | Health promotion refers to actions and processes that create better conditions for health through, for example, strengthening people’s control over their own health and addressing societal determinants of ill-health.30 |
| Abductive thinking | A form of inventive and intuitive (‘hunch-driven’) thinking that allows a researcher to creatively imagine, for example, potential mechanisms to be investigated.45 69 |
| Retroduction | Theorising and testing of hidden causal mechanisms that have, for example, been imagined through abductive thinking or inductively inferred from descriptions of existing studies.45 49 69 |
| Counterfactual thinking | The consideration and application of contradictory evidence or alternative explanations to an interpretation, such as a CMO configuration, to further test and refine it.48 70 |
While more traditional reviews of public health interventions, especially systematic reviews, tend to be concerned with the effectiveness of said interventions in achieving intended and clearly specified outcomes, realist reviews combine theory and empirical observations to uncover how, why and for whom such interventions work or not by adopting an explicit explanatory approach.47–49 The key outputs of realist reviews are, therefore, theories and models of generative causation, often captured by a heuristic approach that explains how entities such as contexts and mechanisms interact in different ways to produce different intended or emergent (unintended) outcomes. The functioning of contexts (C) and mechanisms (M) in ways that produce outcomes (O) is captured by configurations referred to as CMO configurations. These concepts, and other central terms used in this review protocol, are defined in table 1. While realist-informed research may also make use of other explanatory factors,50 such as interventions and actors, as part of heuristic configurations, the starting point for the proposed review is to use CMO configurations as it provides sufficient explanatory depth and coherence. Other elements may be introduced if the review process seems to require it for clarity and to enhance realist causal explanations in a way that can, for example, disentangle agency from structure.51
Aim and objectives
This realist review protocol proposes steps towards generating an understanding of how and why community engagement enhances the benefits (or not) of interventions to facilitate NCD-related research, prevention and health promotion in LMIC settings. More specifically, the objectives of the realist review are:
To review existing theoretical and empirical literature across disciplines and settings to understand how, why, for whom and under what circumstances community engagement and participatory research approaches work or do not work.
To situate the reviewed community engagement and health research in historical perspectives, vis-à-vis bioethics and, for example, legacies of exploitative medical research and other past transgressions, including top-down or irrelevant interventions.
To inform, and formulate recommendations for, future research and interventions with a focus on drawing lessons for ethical, community-centred NCD prevention research and health promotion in LMIC settings.
Context of the review
The need for a realist review stems from current work around NCD prevention and preconception health promotion in South Africa, and a recognition that the pursuit of ethical research informed by community perspectives is challenging when the health topics in question are, understandably, low on intended beneficiaries’ agendas. SK and CED are involved in various research initiatives in South Africa, including qualitative research on improving community engagement practices in Soweto. However, the author team and advisors include experiences and perspectives from a range of settings beyond South Africa, helping to ensure that any transferable findings of the review can be drawn on more widely.
Currently, another realist review of community engagement with health research is being conducted by BA and other colleagues with a focus on malaria trials or other communicable disease interventions in LMICs.8 We are not aware of other realist reviews of community engagement in NCD prevention and health promotion in LMICs, and thus consider our work to be complementary to, rather than a duplication of, existing or ongoing work.
Methods and analysis
Study design
The design of this review is based on the realist review process developed by Pawson et al,48 Realist And Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES) guidelines47 52 and recently published realist review protocols.8 53–55 The realist search and review process is iterative and not as linear or rigid as a traditional systematic review.56 57 It is, therefore, complex and not fully predictable, with decisions and changes being made along the way as opposed to all criteria and specifications being predefined. In addition to specific guidance for realist reviews, this review also draws on the six cross-cutting principles of meta-narrative reviews: pragmatism, pluralism, historicity, contestation, reflexivity and peer review.52 Their definitions and roles in the proposed review are summarised in figure 2. The following sections describe the five planned review steps, as well as progress so far, but it is likely that the exact process will evolve somewhat as the review takes shape.
Figure 2.
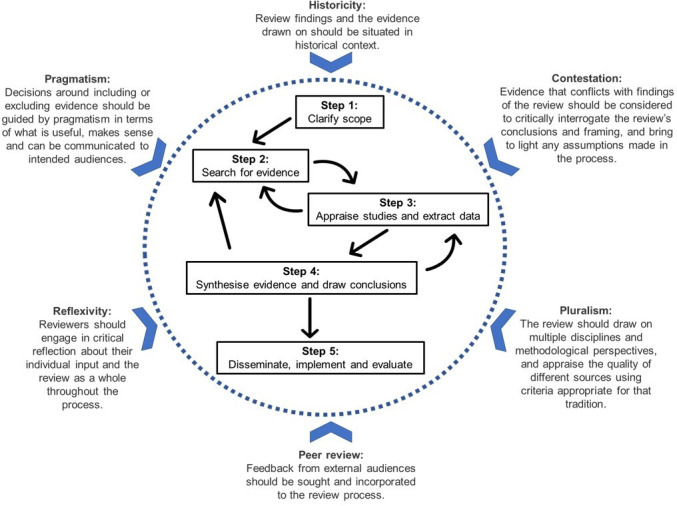
Realist review process and cross-cutting principles.47–49 52
Step 1: clarify scope
This step involved refining the review focus and purpose through initial informal searches, discussions, and drawing on existing theoretical and empirical literature. In terms of identifying literature and developing initial theories, the starting point was finding published articles on community engagement in NCD prevention in LMICs. This was soon expanded to include any setting, particularly literature from high-income countries that describes community engagement or participatory research with Indigenous communities, as this literature often explicitly grapples with histories of harm inflicted through research.19 21 After thorough and iterative discussions about the review aim and objectives, two articles identified through initial, evolving searches and reading were selected (‘berrypicking’58) to elicit the initial theories.44 The rationale for selection was to allow a consideration of both beneficial and harmful engagement, and relevance for NCDs, even if not explicitly describing NCD research or interventions.19 20 A list of initial theories was first elicited through abductive thinking and retroductive theorising (see table 1).45 This meant considering the outcomes of research and interventions described in the two selected studies, and "working backwards to think about the conditions of reality that are necessary for such effects to manifest".45 The list was developed into a conceptual diagram, and the theories were further abstracted following discussions within the author team.
Based on these phases described under step 1, figure 3 illustrates the initial selection of different salient CMO configurations. The micro-theories within the model are potential causal trajectories, presented from the perspective of participants or community members as the primary actors. The figure, therefore, captures how their perceptions and experiences (including past encounters with research or interventions) mediate how new engagement or participation occurs. This enables the review to remain open to both positive and negative, intended and emergent, and ethical or other outcomes. For example, a historically good relationship between a community and researchers (C) can engender trust (M1), and thus openness to researchers’ requests (M2), which can lead to outcomes (O) such as high research participation. The initial exploratory model is not unique to NCDs, and can thus apply more broadly to health promotion efforts and research that use community engagement. Through later steps of the review, the focus will be to refine the initial exploratory theory to specifically inform NCD research and interventions.
Figure 3.
Initial theories: potential community engagement trajectories in health research and interventions.8 13 18–20 49
Stakeholder consultation has been initiated through online correspondence with researchers who are able to give input on the review focus and initial theories based on their experience and expertise of community engagement or realist research. More comprehensive stakeholder engagement will be undertaken at later stages.
Step 2: search for evidence
Informed by the first step, a semisystematic approach to literature searching has been developed and piloted, and will be implemented by SK. This will involve using combinations of search terms such as “community engagement”, participatory, “non-communicable disease”, community-led, “low-income country”, “middle-income country”, LMIC, NCD, diabetes, hypertension, “blood pressure”, cardiovascular, cancer, chronic, “mental health”, depression, anxiety, intervention, prevention and more in PubMed, Scopus and Google Scholar, as well as forward and backward reference checking and recommendations from stakeholders. The search will focus on NCDs to ensure a manageable scope, but other literature will be included where it can be expected to inform the review due to potentially similar mechanisms.59 The initial search strategies are relatively narrow and targeted (see online supplemental file 1), but further iterations of the searches (eg, including search terms such as ‘Indigenous’), as well as searches targeting programme theories,57 will likely be undertaken as the review progresses, and these will be reported on transparently.
bmjopen-2021-050632supp001.pdf (11KB, pdf)
Study selection will be purposive, meaning that the review is not expected to represent the existing evidence base in its entirety, but rather only include what the authors deem relevant for expanding, refuting or refining the initial theories. Initial screening of studies based on title, abstract and keywords will take place simultaneously to the searches. Selected articles may be NCD-focused studies or accounts of other health research or intervention work, or any other topic, using any research design, that may feasibly inform community engagement in NCD research and interventions in LMICs. Out of studies initially identified as potentially relevant, SK will select studies in consultation with other reviewers.
The following inclusion criteria will be used:
Study design: any.
Publication date: any, with priority given to more recent studies or particularly influential older studies that have informed later research and practice.
Document type: any that can inform the review, including commentaries and practice-based articles, as long as they come from peer-reviewed journals or reputable and relevant sources of grey literature.60 61
Population or setting: any, with priority given to LMICs or Indigenous or other marginalised communities in high-income countries.
Content: describes some aspect of community engagement or participatory research approaches, or provides relevant perspectives and applicable information beyond these topics even if focusing on communicable diseases or NCD management rather than prevention.
Language: English.
Step 3: appraise studies and extract data
Data extraction and appraisal will be carried out using a template that will be developed and piloted specifically for this realist review, covering both any data relevant to inform CMO configurations and study characteristics needed for conducting a quality assessment of each study. The template and data extraction process will also be informed by a realist approach to thematic analysis, which incorporates different forms of reasoning (inductive, deductive, abductive and retroductive) into thematic analysis, and requires all three ontological layers to be considered.62 While the use of a data extraction template resembles a codebook approach to thematic analysis, the realist approach will be used to consider both manifest semantic content, such as outcomes, as well as latent content, such as potential mechanisms. This approach will enable us to start eliciting theories already at the data extraction phase.
The starting point for quality assessment will be to use the relevant design-specific Critical Appraisals Skills Programme checklist63 to appraise each peer-reviewed study, and Tyndall’s checklist for grey literature.60 Additional design-specific appraisal tools may be sought where needed, and their use will be reported transparently in the review.
Further inclusion and exclusion of literature, and refinement of inclusion criteria, may occur at this point. This step of the process will incorporate the review team’s judgement of ‘fitness for purpose’ in relation to the review’s aims with existing quality assessment criteria for different study designs. Considerations of ‘fitness for purpose’ will be guided by the two key criteria of relevance (does the research address the review’s objectives and theories being developed?) and rigour (do the conclusions put forward by researchers or the review team hold in relation to the data presented?) as well as the six principles detailed in figure 2.47 48 52
Step 4: synthesise evidence and draw conclusions
Analysis and synthesis of data extracted in the previous step will be carried out through further iterations of the realist approach to thematic analysis,62 with a particular focus on using abductive thinking and retroductive theorising (table 1) to elicit new theories and build on the initial theories presented here.45 Abductive thinking will allow us to postulate what types of mechanisms might be involved in generating specific outcomes. Through retroduction, we will link the hypothesised constructs to formulate mechanism-based explanatory models.44 Counterfactual thinking (table 1) will be applied with the help of evidence that seems to refute or disagree with the emerging conclusions. For example, there could be an emerging conclusion that remuneration and related expectations around community engagement are a dominant mechanism determining outcomes, such as participant retention, in contexts of poverty and inequality. This observation would be considered against evidence of community engagement through which high participant retention has been successfully achieved without significant material gains being expected or received by the community.
These analytical phases will be done in consultation with the review team and stakeholders to further develop, refine or refute the initial programme theory, as well as consider historical context (for example, colonialism, ethically sound or exploitative research, and donor dynamics) of findings. The analysis and synthesis of review findings to draw conclusions will be a particularly iterative step in the process, and will likely involve further data extraction and identification of additional relevant literature (see figure 2). Changes and developments in programme theories will be documented and transparently reported to show a trail of gradual theory building.
Step 5: disseminate, implement and evaluate
The output of this proposed review is expected to have practical applications in NCD research, interventions and other health promotion efforts. To ensure this, further stakeholder consultation will be carried out in the form of discussions and realist interviews64 with researchers, activists and community members in the research context in which SK and CED work in South Africa. These consultations will contribute to further iterations of the review steps as relevant, and form an evaluative component of the review, through which the six guiding principles can be further realised.52 See the Ethics and dissemination section for further details about dissemination and implementation.
Patient and public involvement
This realist review involves stakeholder consultation at different stages. Initial expert stakeholder consultation has targeted researchers internationally, whereas later stages will gather input from researchers, practitioners, community organisations and individuals in South Africa through the consultation process described above, and an adjacent qualitative study of community engagement in health research in South Africa. Using in-depth qualitative methods, such as realist interviews64 in combination with informal online (email, video call) feedback consultations with experts, will enable capturing varied input on theories and other review findings from a range of stakeholders.
Ethics and dissemination
Formal ethics review is not required for the review itself, as it constitutes secondary research with elements of peer feedback from relevant researchers. Ethical approval has been obtained (M200641) from the University of the Witwatersrand Human Research Ethics Committee (Medical) for wider stakeholder consultation, including qualitative fieldwork with a range of participants. Dissemination will include traditional academic channels (publications, conferences, seminars), inclusion of findings in new community engagement strategies developed by authors for their research units, as well as sharing of findings at community engagement events in South Africa and beyond, through plain language publications or summaries, social media and in discussions with a wide range of stakeholders.
Supplementary Material
Acknowledgments
The authors would like to thank all colleagues and stakeholders who have contributed time and feedback to this review protocol during globally challenging times. Eleanor Winpenny’s initial inspiration for adopting a realist review approach is gratefully acknowledged.
Footnotes
Twitter: @sonkling, @Bipin_Tropmed, @DrCathD, @bossedna1, @PTiigah, @DeborahNyirend1, @Mcferdious
Contributors: SK conceptualised the study with input from FCM, CED and BA. SK designed and drafted the review protocol. FCM, BA, CED, ENB, PT and DN contributed to protocol development. FCM and BA provided methodological guidance. BA and SK developed initial programme theories with input from other authors and stakeholders. BA, CED, FCM, ENB, PT and DN critically reviewed and edited the manuscript. All authors read and approved the final manuscript.
Funding: The work of SK was supported by Koneen Säätiö (grant number 201901846).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Reynolds L, Sariola S. The ethics and politics of community engagement in global health research. Crit Public Health 2018;28:257–68. 10.1080/09581596.2018.1449598 [DOI] [Google Scholar]
- 2.King KF, Kolopack P, Merritt MW, et al. Community engagement and the human infrastructure of global health research. BMC Med Ethics 2014;15:84. 10.1186/1472-6939-15-84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adhikari B, Pell C, Cheah PY. Community engagement and ethical global health research. Glob Bioeth 2020;31:1–12. 10.1080/11287462.2019.1703504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marsh VM, Kamuya DK, Parker MJ, et al. Working with concepts: the role of community in international collaborative biomedical research. Public Health Ethics 2011;4:26–39. 10.1093/phe/phr007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilkinson A, Parker M, Martineau F, et al. Engaging ‘communities’: anthropological insights from the West African Ebola epidemic. Philos Trans R Soc B 2017;372:20160305. 10.1098/rstb.2016.0305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hamed S, Klingberg S, Mahmud AJ, et al. Researching health in diverse neighbourhoods: critical reflection on the use of a community research model in Uppsala, Sweden. BMC Res Notes 2018;11:612. 10.1186/s13104-018-3717-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clinical and Translational Science Awards Consortium Community Engagement Key Function Committee Task Force on the Principles of Community Engagement . Principles of community engagement, second edition; 2011. https://www.atsdr.cdc.gov/communityengagement/pdf/PCE_Report_508_FINAL.pdf
- 8.Adhikari B, Vincent R, Wong G, et al. A realist review of community engagement with health research. Wellcome Open Res 2019;4:87. 10.12688/wellcomeopenres.15298.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dickert N, Sugarman J. Ethical goals of community consultation in research. Am J Public Health 2005;95:1123–7. 10.2105/AJPH.2004.058933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bartholomew Eldredge LK, Markham CM, Ruiter RAC, et al . Planning health promotion programs : an intervention mapping approach. 4 edn. Jossey-Bass, 2016. [Google Scholar]
- 11.O'Cathain A, Croot L, Duncan E, et al. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open 2019;9:e029954. 10.1136/bmjopen-2019-029954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williams O, Sarre S, Papoulias SC, et al. Lost in the shadows: reflections on the dark side of co-production. Health Res Policy Syst 2020;18:43. 10.1186/s12961-020-00558-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jagosh J, Macaulay AC, Pluye P, et al. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. Milbank Q 2012;90:311–46. 10.1111/j.1468-0009.2012.00665.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abimbola S. Beyond positive a priori bias: reframing community engagement in LMICs. Health Promot Int 2020;35:598–609. 10.1093/heapro/daz023 [DOI] [PubMed] [Google Scholar]
- 15.Ndinda C, Hongoro C, Chilwane D. Civil society activism for the prevention and treatment of non-communicable diseases in South Africa: implications for policy and practice, 2015: 191–207. [Google Scholar]
- 16.Ndinda C, Ndhlovu TP, Juma P, et al. The evolution of non-communicable diseases policies in post-apartheid South Africa. BMC Public Health 2018;18:956. 10.1186/s12889-018-5832-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Luna F, Luyckx VA. Why have non-communicable diseases been left behind? Asian Bioeth Rev 2020;12:5–25. 10.1007/s41649-020-00112-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jagosh J, Bush PL, Salsberg J, et al. A realist evaluation of community-based participatory research: partnership synergy, trust building and related ripple effects. BMC Public Health 2015;15:725. 10.1186/s12889-015-1949-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Waddell CM, Herron RV, Gobeil J, et al. Grounded in culture: reflections on sitting outside the circle in community-based research with Indigenous men. Qual Health Res 2020;30:2343–50. 10.1177/1049732320960050 [DOI] [PubMed] [Google Scholar]
- 20.Nyirenda D, Sariola S, Kingori P, et al. Structural coercion in the context of community engagement in global health research conducted in a low resource setting in Africa. BMC Med Ethics 2020;21:90. 10.1186/s12910-020-00530-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bird-Naytowhow K, Hatala AR, Pearl T. Ceremonies of relationship: engaging urban Indigenous youth in community-based research. Int J Qual Methods 2017;16. 10.1177/1609406917707899 [DOI] [Google Scholar]
- 22.Burgess RA, Jain S, Petersen I, et al. Social interventions: a new era for global mental health? Lancet Psychiatry 2020;7:118–9. 10.1016/S2215-0366(19)30397-9 [DOI] [PubMed] [Google Scholar]
- 23.Campbell C, Burgess R. The role of communities in advancing the goals of the movement for global mental health. Transcult Psychiatry 2012;49:379–95. 10.1177/1363461512454643 [DOI] [PubMed] [Google Scholar]
- 24.De Weger E, Van Vooren NJE, Drewes HW, et al. Searching for new community engagement approaches in the Netherlands: a realist qualitative study. BMC Public Health 2020;20:508. 10.1186/s12889-020-08616-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sambiéni NE. Differences and structural weaknesses of institutional mechanisms for health research ethics: Burkina Faso, Palestine, Peru, and Democratic Republic of the Congo. BMC Med Ethics 2018;19:47. 10.1186/s12910-018-0284-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.GBD 2017 Causes of Death Collaborators . Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the global burden of disease study 2017. Lancet 2018;392:1736–88. 10.1016/S0140-6736(18)32203-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gouda HN, Charlson F, Sorsdahl K, et al. Burden of non-communicable diseases in sub-Saharan Africa, 1990-2017: results from the global burden of disease study 2017. Lancet Glob Health 2019;7:e1375–87. 10.1016/S2214-109X(19)30374-2 [DOI] [PubMed] [Google Scholar]
- 28.Allotey P, Davey T, Reidpath DD. NCDs in low and middle-income countries - assessing the capacity of health systems to respond to population needs. BMC Public Health 2014;14 Suppl 2:S1. 10.1186/1471-2458-14-S2-S1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bosire E, Mendenhall E, Omondi GB, et al. When diabetes confronts HIV: biological Sub-citizenship at a public hospital in Nairobi, Kenya. Med Anthropol Q 2018;32:574–92. 10.1111/maq.12476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Health Organization . WHO EMRO health promotion and disease prevention through population-based interventions, including action to address social determinants and health in equity, 2021. Available: http://www.emro.who.int/about-who/public-health-functions/health-promotion-disease-prevention.html [Accessed 3 Feb 2021].
- 31.Lynch HM, Green AS, Clarke Nanyonga R, et al. Exploring patient experiences with and attitudes towards hypertension at a private hospital in Uganda: a qualitative study. Int J Equity Health 2019;18:206. 10.1186/s12939-019-1109-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ware LJ, Prioreschi A, Bosire E, et al. Environmental, social, and structural constraints for health behavior: perceptions of young urban black women during the preconception Period-A healthy life trajectories initiative. J Nutr Educ Behav 2019;51:946–57. 10.1016/j.jneb.2019.04.009 [DOI] [PubMed] [Google Scholar]
- 33.Draper CE, Bosire E, Prioreschi A, et al. Urban young women’s preferences for intervention strategies to promote physical and mental health preconception: A Healthy Life Trajectories Initiative (HeLTI). Prev Med Rep 2019;14:100846. 10.1016/j.pmedr.2019.100846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Draper CE, Prioreschi A, Ware LJ, et al. Pilot implementation of Bukhali: A preconception health trial in South Africa. SAGE Open Med 2020;8:2050312120940542. 10.1177/2050312120940542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morrison J, Akter K, Jennings HM, et al. Participatory learning and action to address type 2 diabetes in rural Bangladesh: a qualitative process evaluation. BMC Endocr Disord 2019;19:118. 10.1186/s12902-019-0447-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mannell J, Davis K, Akter K, et al. Visual participatory analysis: a qualitative method for engaging participants in interpreting the results of randomized controlled trials of health interventions. J Mix Methods Res 2021;15:18–36. 10.1177/1558689820914806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fottrell E, Ahmed N, Morrison J, et al. Community groups or mobile phone messaging to prevent and control type 2 diabetes and intermediate hyperglycaemia in Bangladesh (DMagic): a cluster-randomised controlled trial. Lancet Diabetes Endocrinol 2019;7:200–12. 10.1016/S2213-8587(19)30001-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chibanda D, Mesu P, Kajawu L, et al. Problem-Solving therapy for depression and common mental disorders in Zimbabwe: piloting a task-shifting primary mental health care intervention in a population with a high prevalence of people living with HIV. BMC Public Health 2011;11:828. 10.1186/1471-2458-11-828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chibanda D, Weiss HA, Verhey R, et al. Effect of a primary care-based psychological intervention on symptoms of common mental disorders in Zimbabwe: a randomized clinical trial. JAMA 2016;316:2618–26. 10.1001/jama.2016.19102 [DOI] [PubMed] [Google Scholar]
- 40.NCD Alliance . Our views, our voices, 2021. Available: https://ncdalliance.org/what-we-do/capacity-development/our-views-our-voices [Accessed 19 Feb 2021].
- 41.Nyirenda D, Sariola S, Gooding K, et al. 'We are the eyes and ears of researchers and community': understanding the role of community Advisory groups in representing researchers and communities in Malawi. Dev World Bioeth 2018;18:420–8. 10.1111/dewb.12163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mukumbang FC. A realist evaluation of the antiretroviral treatment adherence Club programme in the metropolitan area of the Western Cape Province, 2018. Available: https://etd.uwc.ac.za/handle/11394/5745 [Accessed 19 Jul 2021]. 10.1136/bmjopen-2015-009977 [DOI] [PMC free article] [PubMed]
- 43.Bhaskar R. A realist theory of science. Routledge/Taylor & Francis Group, 2008. [Google Scholar]
- 44.Mukumbang FC, van Wyk B. Leveraging the Photovoice methodology for critical realist theorizing. Int J Qual Methods 2020;19 10.1177/1609406920958981 [DOI] [Google Scholar]
- 45.Jagosh J. Retroductive theorizing in Pawson and Tilley’s applied scientific realism. J Crit Realism 2020;19:121–30. 10.1080/14767430.2020.1723301 [DOI] [Google Scholar]
- 46.de Souza DE. Culture, context and society - The underexplored potential of critical realism as a philosophical framework for theory and practice. Asian J Soc Psychol 2014;17:141–51. 10.1111/ajsp.12052 [DOI] [Google Scholar]
- 47.Wong G, Greenhalgh T, Westhorp G, et al. RAMESES publication standards: realist syntheses. BMC Med 2013;11:21. 10.1186/1741-7015-11-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pawson R, Greenhalgh T, Harvey G, et al. Realist review--a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10 Suppl 1:21–34. 10.1258/1355819054308530 [DOI] [PubMed] [Google Scholar]
- 49.Jagosh J. Realist synthesis for public health: building an Ontologically deep understanding of how programs work, for whom, and in which contexts. Annu Rev Public Health 2019;40:361–72. 10.1146/annurev-publhealth-031816-044451 [DOI] [PubMed] [Google Scholar]
- 50.De Weger E, Van Vooren NJE, Wong G, et al. What’s in a Realist Configuration? Deciding Which Causal Configurations to Use, How, and Why. Int J Qual Methods 2020;19:160940692093857. 10.1177/1609406920938577 [DOI] [Google Scholar]
- 51.Hinds K, Dickson K. Realist synthesis: a critique and an alternative. J Crit Realism 2021;20:1–17. 10.1080/14767430.2020.1860425 [DOI] [Google Scholar]
- 52.Wong G, Greenhalgh T, Westhorp G, et al. RAMESES publication standards: meta-narrative reviews. BMC Med 2013;11:20. 10.1186/1741-7015-11-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Caswell RJ, Maidment I, Ross JDC, et al. How, why, for whom and in what context, do sexual health clinics provide an environment for safe and supported disclosure of sexual violence: protocol for a realist review. BMJ Open 2020;10:e037599. 10.1136/bmjopen-2020-037599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Abrams R, Wong G, Mahtani KR, et al. Understanding the impact of delegated home visiting services accessed via general practice by community-dwelling patients: a realist review protocol. BMJ Open 2018;8:e024876. 10.1136/bmjopen-2018-024876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Duddy C, Wong G. Explaining variations in test ordering in primary care: protocol for a realist review. BMJ Open 2018;8:e023117. 10.1136/bmjopen-2018-023117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Greenhalgh T, Thorne S, Malterud K. Time to challenge the spurious hierarchy of systematic over narrative reviews? Eur J Clin Invest 2018;48:e12931. 10.1111/eci.12931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Booth A, Briscoe S, Wright JM. The "realist search": A systematic scoping review of current practice and reporting. Res Synth Methods 2020;11:14–35. 10.1002/jrsm.1386 [DOI] [PubMed] [Google Scholar]
- 58.Bates MJ. The design of browsing and berrypicking techniques for the online search interface. Online Review 1989;13:407–24. 10.1108/eb024320 [DOI] [Google Scholar]
- 59.Wong G, Westhrop G, Pawson R. Realist synthesis RAMESES training materials, 2013. Available: http://ramesesproject.org/media/Realist_reviews_training_materials.pdf [Accessed 22 Feb 2021].
- 60.Tyndall J. AACODS checklist, 2010. Available: https://dspace.flinders.edu.au/xmlui/bitstream/handle/2328/3326/AACODS_Checklist.pdf;jsessionid=67E9E0E44805CE646B50C475C7ACD013?sequence=4 [Accessed 19 Feb 2021].
- 61.Adams J, Hillier-Brown FC, Moore HJ, et al. Searching and synthesising 'grey literature' and 'grey information' in public health: critical reflections on three case studies. Syst Rev 2016;5:164. 10.1186/s13643-016-0337-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wiltshire G, Ronkainen N. A realist approach to thematic analysis: making sense of qualitative data through experiential, inferential and dispositional themes. J Crit Realis 2021. 10.1080/14767430.2021.1894909 [DOI] [Google Scholar]
- 63.Critical appraisal skills programme. CASP checklists, 2021. Available: https://casp-uk.net/casp-tools-checklists/ [Accessed 4 May 2021].
- 64.Mukumbang FC, Marchal B, Van Belle S, et al. Using the realist interview approach to maintain theoretical awareness in realist studies. Qual Res 2020;20:485–515. 10.1177/1468794119881985 [DOI] [Google Scholar]
- 65.Bhaskar R. Forms of realism. Philosophica 1975;15:99–127. [Google Scholar]
- 66.Pawson R, Tilley N. Realistic evaluation. SAGE Publications Ltd, 1997. [Google Scholar]
- 67.Mukumbang FC, Marchal B, Van Belle S, et al. A realist approach to eliciting the initial programme theory of the antiretroviral treatment adherence Club intervention in the Western Cape Province, South Africa. BMC Med Res Methodol 2018;18:47. 10.1186/s12874-018-0503-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Greenhalgh J, Manzano A. Understanding ‘context’ in realist evaluation and synthesis. Int J Soc Res Methodol 2021;41:1–13. 10.1080/13645579.2021.1918484 [DOI] [Google Scholar]
- 69.Ritz B. Comparing abduction and retroduction in Peircean pragmatism and critical realism. J Crit Realism 2020;19:456–65. 10.1080/14767430.2020.1831817 [DOI] [Google Scholar]
- 70.Eastwood JG, Jalaludin BB, Kemp LA. Realist explanatory theory building method for social epidemiology: a protocol for a mixed method multilevel study of neighbourhood context and postnatal depression. Springerplus 2014;3:1–12. 10.1186/2193-1801-3-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-050632supp001.pdf (11KB, pdf)