Abstract
Fatalistic attitudes have a negative impact on a broad variety of health behaviors and behavioral determinants of health. A growing body of research has documented an association between media exposure and fatalism; however, scholarship has not been able to ascertain the causal direction. This review synthesizes the current state of the literature. A major finding is that most studies purporting to assess the relationship between media exposure and fatalism use conflated measures of fatalism. Among those that use an appropriate measure, there is some evidence that increased exposure to media increases fatalism. Although there is a substantive theoretical rationale for such effects, more research is needed to make a definitive claim and to explain the mechanism for such effects.
Keywords: Fatalism, media exposure, information overload, measurement issues
Fatalism is often envisioned as a tendency to believe that events are inevitable, and nothing can be done to change these events (Chavez, Hubbell, Mishra, & Valdez, 1996; Egede & Ellis, 2010; Flórez et al., 2009; Powe & Finnie, 2003). The consequences of fatalism can be serious: in the health realm, for example, fatalistic beliefs are likely to result in non-adherence to recommendations for healthy behaviors because few benefits are perceived (e.g. nothing can be done about the disease or the disease is God’s will). And there is a large body of literature that demonstrates the negative impact of fatalism on a broad variety of health behaviors and their determinants (Espinosa de los Monteros & Gallo, 2011; Shen, Condit, & Wright, 2009). However, little is known about what causes fatalism.
One potential cause of fatalistic beliefs is the news media: the high volume of news coverage about the determinants and prevention of cancer in particular been implicated in the cultivation of fatalistic beliefs (Adelman & Verbrugge, 2000; Niederdeppe, Fowler, Goldstein, & Pribble, 2010; Russell, 1999; Taubes, 1995; Viswanath et al., 2006). Additionally, advances in communication technologies have led to an increasingly rich information environment, which in turn has led to an explosion of information available to many individuals (Viswanath et al., 2012). The consequences of this overabundance of information may not always be positive. For example, in a healthcare environment where patients are active participants in medical decision-making, making sense of this rich information environment is an increasingly important contributor to health (Kelly et al., 2010), yet individuals and subgroups may be ill-equipped to sift through the information to obtain what they need to make informed decisions. Furthermore, the content matters: research has shown the current media environment can be characterized by substantial controversy and contradiction (Carlson, 2017; Clarke & Everest, 2006; Dreier & Martin, 2010; Gill & Babrow, 2007; Hurley, Kosenko, & Brashers, 2011). This is particularly true for complex and heavily researched topics such as cancer and nutrition (Kelly et al., 2010; Nagler, 2014) and can be in part explained by the evolutionary nature of the science of such topics that can lead to changing health recommendations (e.g. Squiers et al., 2011). While scientists and health professionals are trained to cope with this conflicting environment, the public lacks this thorough training and may not be able to deal as effectively. Whereas the news media could serve as gatekeepers and interpreters for the general public, many journalists lack the scientific training that would allow them to take on that role (Schwartz & Woloshin, 2002). Among individuals, this inability to cope with the evolutionary nature of research, combined with uneven or deliberately controversial reporting, interferes with people’s ability to make sense of information and could lead to adverse cognitive and health effects (Goldberg & Sliwa, 2011; Nagler & Hornik, 2012). For example, many people report feeling overwhelmed and confused about cancer information and nutrition (Arora et al., 2008; Nagler, 2014; Niederdeppe & Levy, 2007). Studies also have shown that conflicting messages and controversy can lead to confusion and possibly even non-adherence to medical advice (Schwartz & Woloshin, 2002; Woloshin et al., 2000). This paradoxical and increasingly worrisome consequence of such a rich information environment has led to an interest in the role of media, particularly the news media, on fatalistic beliefs, in which a growing body of research has documented an association between media exposure and fatalistic beliefs (e.g. (Niederdeppe et al., 2010).
The aim of the present study is to create a better understanding of the relationship between fatalism and the media by exploring the different directions for this phenomenon and providing a structured overview of the existing work examining the relationship between fatalism and media exposure.
Although our primary examples come from health communication and relate to health outcomes, we argue that understanding fatalism is important for communication more broadly and may be applied to research programs in political communication (e.g. see Scheufele, Nisbet, & Brossard 2003 on how people with fatalistic beliefs are likely to avoid content that disagrees with their political preference and avoid political discussions with heterogeneous social networks) and other areas.
Defining fatalism
Fatalism has been defined and operationalized in a variety of ways, and this has contributed to a lack of clarity about its association with either media exposure or health outcomes. Many of the fatalism scales are disease specific and concentrate on a single dimension of fatalism (e.g. pessimism). Shen et al. (2009) have found the literature on fatalism to contain at least one of the following three domains: predestination, pessimism, and attribution of one’s health to luck. These three domains are all cognitive in nature. Fatalism is therefore seen as a set of beliefs, in which an individual has a situation-specific attitude towards a specific outcome. This is concordant with a growing body of evidence that fatalistic beliefs can be changed (Espinosa de los Monteros & Gallo, 2011; Hamilton, Best, Galbraith, Worthy, & Moore, 2014; Portnoy, Leach, Kaufman, Moser, & Alfano, 2014; Powe & Weinrich, 1999).
Predestination comprises the perceived lack of control that an individual has over external events. This conceptualization of fatalism is cognate with the locus of control concept (Rotter, 1966), which refers to the control that an individual perceives over events that affect him/her. Locus of control may be internal (when individuals perceive they can control their lives) or external (when individuals perceive their lives are mostly controlled by chance, fate or powerful others). While operational definitions of fatalism are regularly based on the concept of health locus of control (Egede & Ellis, 2010), some studies suggest that this is different from fatalism both conceptually (e.g. death is imminent versus having no control over one’s health) and psychometrically (Boone, De Brabander, Gerits, & Willeme, 1990; Espinosa de los Monteros & Gallo, 2011).
Examples of fatalistic beliefs from the predestination domain include the beliefs that health is beyond human control (Neff & Hoppe, 1993; Rundmo & Hale, 2003; Schnoll et al., 2002; Straughan & Seow, 1998; Urizar & Sears, 2006); that illness is a punishment for wrong doings (Conrad, Brown, & Conrad, 1996); and that nothing can be done about disease (Chavez et al., 1996; Unger et al., 2002). Often the perceived lack of control over external events includes beliefs that outcomes are God’s will (Egede & Bonadonna, 2003; Egede & Ellis, 2010; Yeh, Inman, Kim, & Okubo, 2006).
The pessimism domain refers to beliefs that negative consequences will happen regardless of behaviors. This domain is often captured with measures of powerlessness, hopelessness, and meaninglessness (Shen et al., 2009; Shen & Condit, 2012). The pessimism domain is based on the definition of cancer fatalism by Powe (1995); Powe and Finnie (2003); Powe and Weinrich (1999) and has been used in numerous cancer studies (Lee, Long, Slater, & Song, 2014; Michielutte, Dignan, Sharp, Boxley, & Wells, 1996; Niederdeppe & Levy, 2007; Ramírez, 2014; Ramírez, Finney Rutten, et al., 2013). Examples of fatalism as pessimism include the perception that death is inevitable following cancer diagnosis (Powe, 1995; Powe & Finnie, 2003), that everything causes cancer (Lee et al., 2014; Nelson et al., 2004; Niederdeppe & Levy, 2007; Ramírez, 2014; Ramírez, Finney Rutten, et al., 2013) and that there is not much people can do to lower their chances of getting cancer (Berman & Wandersman, 1990; Lee et al., 2014; Niederdeppe & Levy, 2007; Ramírez, 2014; Ramírez, Finney Rutten, et al., 2013). The pessimism dimension of fatalism has been predominant in cancer research, and also used outside cancer research, from diabetes self-management (Egede & Ellis, 2010), to coping with extreme stress (Yeh et al., 2006), and substance abuse (Unger et al., 2002).
The final dimension of fatalism is the attribution of one’s health to luck - the perception that health is based on luck, destiny, or fate. An example of this is the idea that some people are just unlucky and nothing they can do, including any behavioral or lifestyle change, will prevent them from having poor health (Davison, Frankel, & Smith, 1992). Other examples include perceptions that nothing can be done, because poor health is a result of fate (Zimrin, 1986) or chance (Cohen & Nisbett, 1998).
Although the three domains may be conceptualized separately, a hierarchical factor analysis done by Shen et al. (2009) found that ‘fatalism’ is a unique construct overlying these three sub-constructs. Their results showed multidimensionality on the first order (i.e. predetermination, pessimism, and attribution of one’s health to luck differ) and unidimensionality on the second order (i.e. fatalism). Recent research by Esparza, Wiebe, and Quiñones (2015) suggests that fatalism is a multidimensional construct as well. The multidimensional nature of fatalism may therefore explain the large variety of measurements and different conceptualizations.
While the constructs measuring fatalism may be multidimensional in nature, this does not mean that all measures currently used to assess fatalism are explained by an underlying fatalism dimension. The underlying fatalism construct is different from other constructs frequently conflated with fatalism, such as ‘locus of control’ and ‘information overload’ (see below), based on a key distinction as explained by Rippetoe and Rogers (1987): acceptance of their predicament. A fatalistic individual has accepted any adverse outcomes and therefore will not need to engage in any coping.
Fatalism, measurement issues, and information overload
Studies examining the relationship between fatalism and media exposure have predominantly taken place in the context of cancer. Recent research suggests that measures of fatalism frequently used in cancer communication research might be conflating what is more generally accepted as fatalism with an information overload sentiment (Jensen et al., 2014; Ramírez, 2014). Many studies investigating cancer fatalism have used measures from the National Cancer Institute’s Health Information National Trends Survey (HINTS; www.hints.cancer.gov) that address three components of fatalism to assess fatalistic beliefs. These components have been dubbed helplessness (‘There’s not much people can do to lower their chances of getting cancer’), pessimism (‘It seems like almost everything causes cancer’) (This component should not be confused with pessimism as defined in this review: the belief that negative consequences will happen regardless of behaviors), and confusion (‘There are so many recommendations about preventing cancer, it’s hard to know which ones to follow’) (Nelson et al., 2004). However, a recent line of research suggests that the last two items, ‘There are so many recommendations about preventing cancer, it’s hard to know which ones to follow’ and ‘It seems like almost everything causes cancer’ might be capturing the distinct construct of information overload rather than fatalism (Jensen et al., 2014; Ramírez, 2014). A key distinction is that these items seem not to measure an acceptance of one’s fate in which there is no need to engage in any coping (fatalism); as such, these items therefore might have a different relationship with media exposure than measures that more accurately capture the dimensions of fatalism.
Information overload could be the consequence of an over-abundant information environment. Recent research has suggested that an overabundance of information has potentially negative consequences on knowledge, attitudes, and adherence to recommended health behavior (Jensen et al., 2014). Additionally, the nature of the over-abundant media environment might be an important factor: research has shown the current media environment can be characterized by substantial controversy and contradiction (Clarke & Everest, 2006; Gill & Babrow, 2007; Hurley et al., 2011). Controversy in news coverage can impact both perceptions (Jensen & Hurley, 2012) as well as behavior (Weeks, Friedenberg, Southwell, & Slater, 2012). Under this explanation, the issue is not so much the content of any specific message, but rather the nature of the information environment as a whole: the information environment is comprised of dueling messages and it is the lack of concordance that produces information overload (and has been called fatalism in the literature).
Potential directions
In our effort to better understand the relationship between media exposure and fatalism, we discuss both causal directions (i.e. media exposure affecting fatalism and fatalism affecting media exposure) and use two (not mutually exclusive) explanations for these directions: (1) fatalism may be a trait or set of beliefs that individuals are predisposed to and which produces selective exposure to health information or (2) fatalism may be an outcome of exposure to the media.
Causal direction 1: fatalism as a trait/cultural belief affects media exposure
Research in health outcomes has generally attributed fatalistic beliefs to culture, with specific cultural groups having stronger fatalistic beliefs. Research has shown that Latinos and African-Americans have stronger fatalistic beliefs compared to individuals of other races/ethnicities (Chavez et al., 1996; Cuéllar, Arnold, & González, 1995; Niederdeppe & Levy, 2007; Ramírez, Finney Rutten, et al., 2013; Spurlock & Cullins, 2005). For instance, fatalism (‘fatalismo’) is seen as a cultural belief held by Latinos. Cultural differences in fatalistic beliefs might result in media exposure differences, such as reduced health information-seeking behavior. Following this perspective, fatalismo presumably deters Latinos from engaging in protective behaviors (Abraído-Lanza et al., 2007). Recent research has also found that fatalistic beliefs are retained even in Latinos who otherwise appear to have acculturated to mainstream U.S. culture, reinforcing the idea that there is some underlying cultural aspect to fatalism (Ramírez, 2014).
However, the perspective of fatalism as a cultural trait is challenged by research that has shown that education and income are negatively associated with fatalism, which suggests that differences attributed to race/ethnic rather reflect the reality of the economic and social disparities (Mayo, Ureda, & Parker, 2001; Powe, 2001). For instance, Latinos score worse on a variety of health determinants and outcomes (Abraído-Lanza, Chao, & Flórez, 2005), and also higher on measures of fatalism, compared with non-Latino Whites (Freeman, 1989; Pérez-Stable, Sabogal, Otero-Sabogal, Hiatt, & McPhee, 1992; Ramírez, Freres, et al., 2013). However, consistent with studies discussed in an overview by Abraído-Lanza et al. (2007) some found differences disappeared when controlling for knowledge and education (Ramírez, Freres, et al., 2013), while others did not (Pérez-Stable et al., 1992). Similarly, fatalism has also been ascribed to other ethnic minority populations such as African-Americans, who also suffer from economic, social, and health disparities (Powe, 1995; Powe & Finnie, 2003).
A related psychological explanation suggests that fatalism may be an individual personality trait - stable and enduring (Scheier & Bridges, 1995). Individuals differ in the way they approach the world around them. While some are naturally more optimistic, others are more pessimistic and expect bad outcomes (Scheier & Carver, 1985). Researchers have suggested that these individual differences are stable across settings and time (Scheier & Carver, 1985). If fatalistic beliefs are believed to be stable, external influences have little effect on fatalism, but they can affect the amount of exposure to media an individual seeks.
The distinction between personality trait and cultural belief is not perfect (Ruiu, 2012). However, the discussion of this distinction does not fall within the scope of the present study. We argue that both approaches favor the explanation that it is fatalistic beliefs that affect media exposure, rather than the reverse. In this explanation, fatalism may be a trait or set of beliefs that individuals are predisposed to and which produces selective exposure to health information.
Causal direction 2: fatalism as an outcome of media exposure
In contrast to the still widespread idea that fatalism is a stable trait (by group or individual) in health research, research investigating the effects of media exposure on fatalism does not usually envision fatalism as a stable and enduring trait. Rather, when fatalism is construed as an outcome of media exposure, it is envisioned as a set of malleable health beliefs, which can change based on external influences such as media exposure.
We explore two potential approaches to explain the relationship between media exposure and fatalism: (1) an individual-level approach, using the Extended Parallel Process Model (EPPM) and (2) a macro-social approach, examining cultivation processes.
Extended parallel process model
Fatalism as a result of media exposure is consistent with fear control as explained by the EPPM. The EPPM (Witte, 1992) is an integrative model originally developed to explain the persuasiveness of fear appeals. The EPPM postulates that the response to a fear appeal consists of two appraisals: threat and efficacy. The first appraisal judges the severity and susceptibility of the threat. If the severity and susceptibility of the threat are perceived to be high, then fear is evoked and action is necessary. The second appraisal determines whether the initial appraisal is adaptive or maladaptive. During this second appraisal, judgments about self-efficacy (‘belief of being able to perform the recommended behavior’ Basil & Witte, 2012, p. 43) and response efficacy (‘a feeling that the behavior will actually be effective in avoiding the risk’ Basil & Witte, 2012, p. 43) are made. When the perceived threat is judged to warrant action and the efficacy judgment suggests that the response can avert the threat, then people are motivated to engage in danger control processes, according to the EPPM. Danger control processes in turn should lead to an adaptive change in which the message is accepted and individuals respond to the threat. However, when the threat is perceived to be high and efficacy low, the fear response is intensified as a person believes they are unable to avert the threat resulting in fear control processes. In this case, an individual is now motivated to cope with the fear, and these fear control processes lead to a maladaptive change.
The EPPM has been found to be generally supported (Witte & Allen, 2000). However, some ambiguity exists. Witte and Allen (2000) conducted a meta-analysis of EPPM studies and found that regardless of the level of efficacy information, maladaptive coping may occur if the level of threat is high enough. These findings are in contrast to a meta-analysis by Floyd, Prentice-Dunn, and Rogers (2000), which found that efficacy is the best predictor for adaptive coping. Despite this ambiguity in the literature, both meta-analyses support the explanation that fatalism could be a maladaptive response to the current media environment that is threatening and lacking efficacy information.
Lower self-efficacy has been found to be related to information overload as well as fatalism (Jensen et al., 2014; Straughan & Seow, 1998). In an experimental setting, Rippetoe and Rogers (1987) found that participants in a high-threat, low self-efficacy, and low response-efficacy condition showed more fatalistic attitudes compared to participants in a high-threat, high self-efficacy, and high response-efficacy condition. Content analyses of news coverage of health risks such as smoking (He, Shen, Yin, Xu, & Lan, 2014), influenza (Dudo, Dahlstrom, & Brossard, 2007; Goodall, Sabo, Cline, & Egbert, 2012), cancer (Jensen, Moriarty, Hurley, & Stryker, 2010; Shim, Kim, Kye, & Park, 2016), and other risks such as climate change (Feldman, Hart, & Milosevic, 2015; Hart & Feldman, 2014) have shown that information about threat is more prevalent compared to efficacy information. Media reports containing cancer news also often include confusing and conflicting information (Clarke & Everest, 2006; Gill & Babrow, 2007; Hurley et al., 2011). It is therefore plausible that the severity and susceptibility of the threat are communicated in the news, while the efficacy component is not. The lack of efficacy information in the media could lead to fear control processes operating causing fatalism as a defense mechanism (maladaptive coping).
Consistent with EPPM, information overload could also result in a fear control process. The contradictory overwhelming nature of media undermines cognitions by straining limited storage and processing capabilities (Jensen et al., 2014, 2016) leading people to feel less efficacious and resulting in maladaptive coping such as information avoidance.
Cultivation effects
Exposure to news coverage may influence fatalistic beliefs through cultivation effects. Cultivation theory suggests that people who are more exposed to television are more likely to perceive social reality as portrayed by television compared to those who are less exposed to television (Gerbner, Gross, Morgan, & Signorielli, 1980; Hetsroni & Tukachinsky, 2006; Morgan, Shanahan, & Signorielli, 2015). Further, when individuals have limited experiences with a particular topic, the influence television has on beliefs is at its strongest (Pfau, Mullen, & Garrow, 1995; Quick, 2009).
Cultivation has been investigated in the context of multiple topics, including violence and crime, gender roles, politics, religion, and health (Bilandzic & Busselle, 2008; Chung, 2014; Romer, Jamieson, & Aday, 2003). Most studies examining cultivation effects of television news found significant associations between watching television and beliefs resembling the reality portrayed on television (Niederdeppe et al., 2010). For example, Lowry, Nio, and Leitner (2003) and Gross and Aday (2003) found that local television news viewing increased beliefs that crime is the most important problem facing their environment. Romer et al. (2003) reported that local television news viewing was associated with fear of crime and concern about violence. Health-related examples include studies suggesting that viewing medical dramas might impact perceptions about healthcare professionals (Chory-Assad & Tamborini, 2003; Foss, 2011) and expectations about cardiopulmonary resuscitation survival rates (Jones, Brewer, & Garrison, 2000; Van den Bulck, 2002).
Cultivation effects can be split into two types: first-order and second-order cultivation (Shanahan & Morgan, 1999). First-order cultivation represents effects on frequency estimates (e.g. a disease mortality rate). These frequency estimates can be determined both by media occurrence as well as actual occurrence in reality (Shrum & Lee, 2012). When making such a frequency estimation, a spontaneous answer is often not available and memory needs to be consulted. The accessibility model of cultivation effects maintains that heavy coverage from the media increases the memory accessibility of exemplars presented by the media (Shrum, Lee, Burroughs, & Rindfleisch, 2011). However, the exemplars presented by the media often do not match reality. For example, news coverage about different cancers does not match population mortality and incidence (Cohen et al., 2008; Jensen et al., 2010), and contain little information about what can be done to reduce risk (Russell, 1999; Taubes, 1995). It is therefore possible that a media environment with a high accessibility of exemplars full of threat and low on efficacy cultivates fatalism.
Second-order cultivation represents effects on values and attitudes. Value and attitude judgments are simpler to make, occur frequently, and are not likely to be constructed from memory retrieved exemplars (Shrum et al., 2011). Instead, these judgments are made when information is encountered and the recall of the stored judgments formed during this moment result in cultivation effects (Shrum, Burroughs, & Rindfleisch, 2003). For example, news media have the tendency to overemphasize new cancer risk at the expense of more balanced reporting that includes follow-up information about what can be done to reduce this cancer risk (Russell, 1999; Taubes, 1995). In second-order cultivation, the overrepresentation of cancer risk and incidence would not make people use their memory to remember probability of items causing cancer (a first-order effect), but cultivate judgments about social reality such as ‘cancer is unavoidable’. Cultivation effects are particularly likely in the area of health, because individuals’ personal experiences with such issues are often limited (Chung, 2014).
Current study
There is little agreement about the causes of fatalistic beliefs or the extent to which these might be modifiable, yet this is an important area of study considering the significant impact of fatalism on health behaviors. One potential explanation is the news media: there has been exponential growth of available health information and a tremendous interest on the part of the media to report on health and illness, and people rely on the media for their health information (Brodie, Hamel, Altman, Blendon, & Benson, 2003; Lee & Niederdeppe, 2011). Given this dependence on the media for health information, it is important to investigate the connection between fatalism and media. There is a growing body of literature investigating the exposure–fatalism relationship, however, to date, there have been no syntheses of this literature, and no unifying theoretical approach to understanding the association. In addition, we know that usage and exposure differs between media and across population segments. We therefore expect potential differences in the relationship between exposure and fatalism for different media. The present review synthesizes the current state of the literature examining a relationship between fatalism and media exposure, provides a preliminary assessment of the evidence for potential explanations for the relationship between fatalism and media exposure, and proposes unifying theoretical mechanisms to expand understanding of how media exposure influences fatalism.
Method
Search strategy
To locate articles for this research synthesis, we conducted systematic searches of five electronic databases: ‘PsychInfo’ (1967–2015), ‘PubMed’ (1966–2015), ‘Medline’ (1950–2015), ‘Communication Abstracts’ (1973–2015), and ‘Communication Source’ (1933–2015). The search was conducted on 6 November 2015 using the following term: fatalis* AND (media OR TV OR television OR newspaper OR internet OR news OR radio OR coverage) NOT intervention. This approach yielded 14 articles that tested an association between exposure to media and fatalism.
Study selection
All articles were checked for duplicates by the authors. Unique articles were judged for their relevance based on title and abstract. Relevant articles were subjected to a second screening of the full text. Strict inclusion and exclusion criteria were applied to the articles to be included in the review: only peer-reviewed publications in English language journals were included. Studies were required to include a quantitative or qualitative assessment of fatalism in addition to a quantitative or qualitative assessment of media exposure. Finally, the studies must have investigated the relationship between fatalism and media exposure. See Figure 1 for a flow diagram of the inclusion process.
Figure 1.
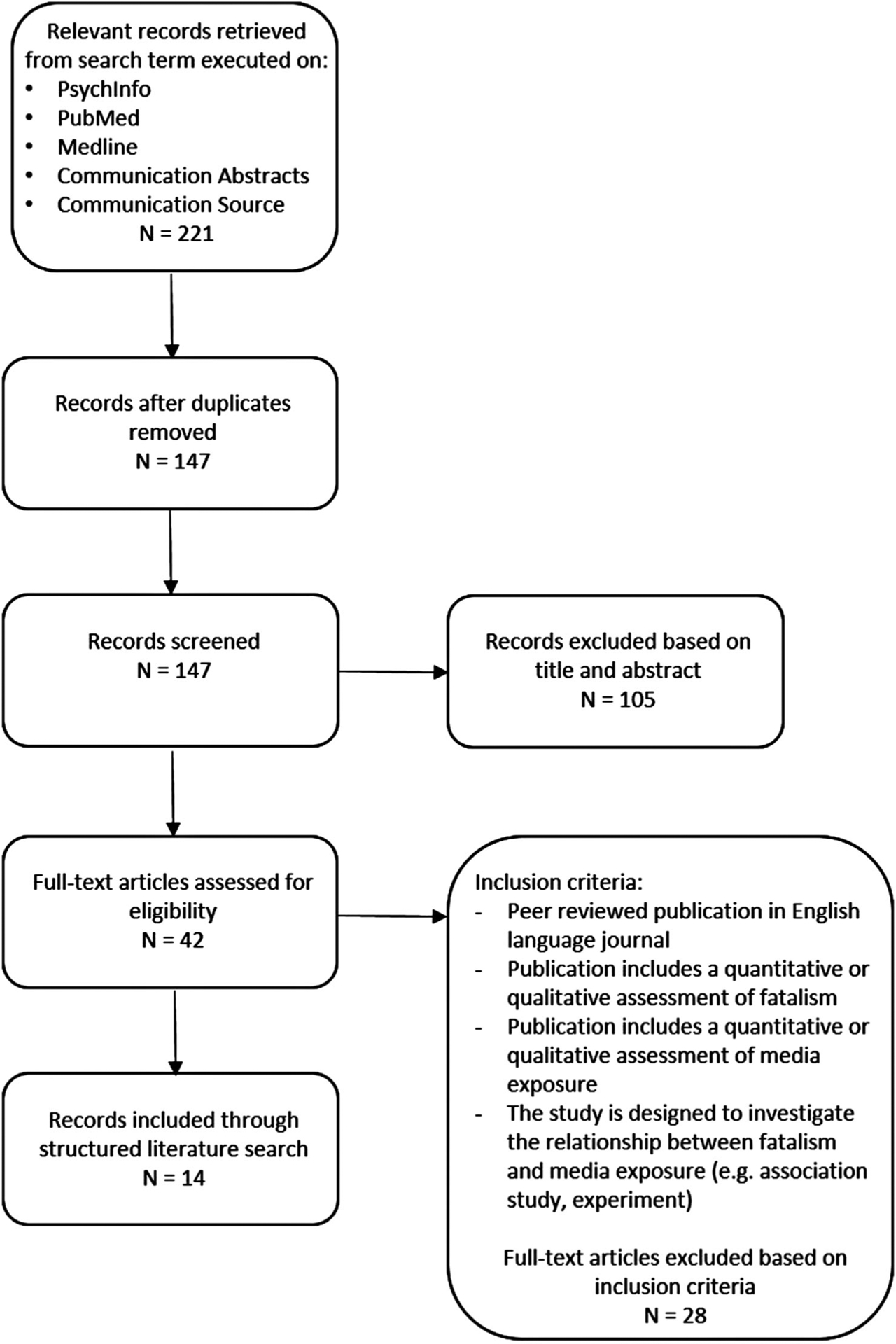
Flow diagram of the systematic literature review process.
Results
Of the 14 included studies, 7 studies focused on the association between media exposure and fatalism and 2 investigated the association between fatalism and information avoidance/media use using cross-sectional survey methods (Table A1). Two studies examined the effects of media on fatalism using longitudinal panel data. Lastly, three studies investigated media exposure and fatalism using a randomized experiment. Four studies focusing on the effect of media exposure on fatalism used the Annenberg National Health Communication Survey (ANHCS) (year: 2005 (×2), 2007 and 2011) and three studies used HINTS (years: 2005 and 2008). Both surveys included identical questions to measure fatalism (as defined by HINTS): fatalistic beliefs characterized by pessimism, helplessness, and confusion (Nelson et al., 2004).
Conflated constructs
An important finding pertains to the fragmentation of the literature. While our search aimed to identify studies examining the association of media exposure and fatalism, 10 of the studies used measures that conflate other constructs with fatalism, including information overload and locus of control. We therefore organize reporting on the evidence for potential explanations for the association between fatalism and media exposure by measure (fatalism, fatalism and information overload, information overload, and locus of control) and medium (multimedia, television, Internet, and other).
Evidence for causal direction 1: fatalism affecting media exposure
Most studies approached the relationship between media exposure and fatalism from a perspective in which media influence fatalistic beliefs. However, the majority of the studies are cross-sectional in nature and do not preclude the reverse. A consideration that fatalism causes media exposure is one in which fatalism is considered a stable trait.
In the present study, we found minimal evidence for this pathway: only three studies examined this relationship from a perspective in which media exposure was the outcome, and of these, only one had significant effects.
Fatalism
In a cross-sectional study, Miles et al. (2008) found a positive association between fatalism and information avoidance in a sample of older adults using Powe’s cancer fatalism inventory. The information avoidance scale included subjective measures of avoiding reading, watching television, and listing to radio programs about cancer.
Information overload
In order to draw stronger causal inferences, Lee and Niederdeppe (2011) used two-wave longitudinal survey data using two items suspected of measuring information overload (‘everything causes cancer’ and ‘there are so many different recommendations’). In this study, media exposure at wave 1 was used as a predictor of fatalism at wave 2, while controlling for fatalistic beliefs at wave 1. Reverse associations (i.e. wave 1 fatalism, wave 2 media exposure) were also tested. In a predominantly non-Hispanic White sample, viewing local television news at time 1 predicted higher fatalistic beliefs at time 2 (1 year later), controlling for fatalistic beliefs at time 1. However, fatalism at time 1 did not significantly predict overall or local television viewing at time 2 after controlling for confounders, leading the authors to conclude that the causal argument that television viewing influences its audiences’ perceptions is more likely than the reverse (Lee & Niederdeppe, 2011).
Locus of control
In one of the earliest studies on the topic Surlin (1977) found no significant relationship between fatalism and radio use after controlling for education. However, a locus of control measure was used instead of (but called) fatalism.
Evidence for causal direction 2: fatalism as an outcome of media exposure
The majority of the articles included in this review approached their study from a perspective in which media affects fatalism; taken together, these studies consistently found significant positive associations between media exposure and fatalistic beliefs.
Six of seven studies investigating the association between media exposure and fatalism using cross-sectional survey designs found a significant positive association, and this was true for a broad spectrum of mass media. None of the studies used a conflated measure of fatalism outside of information overload.
Fatalism
Randomized experiments have been utilized to make stronger causal claims about the relationship between media exposure and fatalism, and specific content features that may contribute to fatalistic beliefs. A multiple message experimental study investigated the possible effects of exposure to news media reports about an earthquake on judgment of preventability, fatalism, and estimates of damage. In this study, with 75 participants, the authors did not find any significant differences in fatalistic beliefs between participants who read fatalistic messages compared to participants who read informed messages (McClure & Velluppillai, 2013). A possible explanation for this lack of cultivation might be that participants were only exposed one or two times, which might have been insufficient to cultivate fatalistic beliefs. However, it is plausible that the non-significant results are a result of a lack of statistical power given the small number (n = 75) of participants included in the study.
Not surprisingly, the reviewed studies suggest that the nature of the content is an important factor in cultivating fatalistic beliefs. This provides us with methods to intervene to reduce fatalistic beliefs that in turn affect health behaviors. However, this process is delicate. To investigate if hedging (i.e. recognizing the ambiguity of the information) affects the perceptions of news consumers, Jensen et al. (2011) conducted a large (n = 1082) multiple message experiment. The authors were interested in discourse-based hedging wherein entire sentences are used to describe limitations and uncertainties. Results showed that streamlining news (i.e. reporting new research findings without acknowledging the ambiguity) resulted in more fatalistic beliefs compared to news that was hedged. The negative impact of streamlined news on fatalism might be the result of situations in which new research findings reported by streamlined news contradicts existing research.
However, another experiment (n = 558) designed to investigate if the amount and content of cancer-related stories influence health beliefs, found that adding uncertainty to a story (e.g. presenting a story as speculative so no conclusions can be drawn) about both causes of cancer and preventive behaviors might result in higher fatalistic beliefs in some cases (i.e. for individuals who do not pay habitual attention to health). No significant effects for the number of cancer-related stories on fatalistic beliefs were found, suggesting that it is not merely the amount of information that is available that contributes to fatalism. While scientific uncertainty should be recognized in news reporting, the authors caution against publishing about uncertain cancer prevention behaviors (Niederdeppe et al., 2014).
Fatalism and information overload
Investigating the relationship between television use and fatalism, using a national sample consisting primarily of non-Hispanic White adults, Niederdeppe et al. (2010) found that increased exposure to local television news was positively associated with cancer fatalism. No association between reading newspapers, watching national television news, listening to radio, and using Internet were found. Comparable results between television use and fatalism were also found in a more diverse sample (30% Caucasian, 26% Hispanic, 19% African American, and 19% Asian). In this sample, the authors found positive associations between general television viewing and television news use and fatalistic beliefs about healthy eating (Northup, 2014).
The association between exposure to television content - independent of the content itself - and measures of fatalism and information overload is generally positive: exposure is associated with holding fatalistic beliefs. However, not all media seem to have the same relationship. In contrast to television, individuals who used the Internet to find cancer information were less likely to hold fatalistic beliefs compared to those who relied on their physician for information about cancer (Befort et al., 2013). In this same study using HINTS data from 2008, with primarily White non-Hispanics, no significant associations between using print sources (books/newspapers/magazines) as an information source and fatalism were found (Befort et al., 2013).
While the included studies have generally found associations between media exposure and fatalism, and hypothesized the direction of the effects, causal statements cannot be made based on cross-sectional data. In order to draw stronger causal inferences, a panel study examined if higher Internet use - using a combination of information scanning and seeking - for health information in wave 1 resulted in higher fatalistic beliefs at wave 2. This nationally representative longitudinal study using online surveys found that Internet use was associated with lower fatalistic beliefs after controlling for confounders. Using print media and television to acquire health information, and local television watching were not related with lower fatalistic beliefs. After examining moderation effects, the authors found that Internet use only was associated with reduced fatalism for individuals with average or lower levels of education and health knowledge (Lee et al., 2012). Overall, both the cross-sectional and the longitudinal studies suggest that television use has the potential to result in higher fatalistic beliefs while Internet use has the potential to results in lower fatalistic beliefs.
Information overload
Five studies investigated the relationship between media exposure and fatalism using measures suspect of being information overload. Nagler (2014) found that increased exposure to certain types of information - conflicting nutrition messages - in the media was positively associated with confusion about healthy food choices. No significant relation between endorsing lung cancer fatalism items and attention to media in the last week was found in a study by Portnoy et al. (2014). However, they did find a significant temporal association between two high-profile cancer events and lower odds of endorsing cancer fatalism items (Portnoy et al., 2014).
As described earlier in the ‘Evidence for causal direction 1: fatalism affecting media exposure’ section, local television news viewing predicted higher fatalistic beliefs 1 year later, using a panel study. No bivariate relations were found between fatalism and other media, including newspapers, radio news listening, and Internet news reading (Lee & Niederdeppe, 2011). Chung (2014) using a national sample consisting primarily of non-Hispanic White adults found that exposure to local television news and medical dramas was positively associated with cancer fatalism. In addition, Chung (2014) found that newspaper and news radio were negatively associated with holding fatalistic beliefs. Han et al. (2009) investigated perceived ambiguity in colon, skin, and lung cancer using television, radio, Internet, and newspaper exposure. They also examined television, Internet, and print health news exposure and found that television exposure and newspaper exposure were positively associated with perceived ambiguity about skin and colon cancer, respectively. Internet health news exposure was negatively related to colon cancer ambiguity (Han et al., 2009).
Fatalism measurement
Most studies (10 out of 14) included in this study used a fatalism measure that might be conflated with other constructs. One study that reported no significant relationship between media exposure and fatalism actually defined and assessed fatalism as locus of control (Surlin, 1977). All of the non-experimental studies (n = 9) included in this review that approached their study from a perspective in which media affects fatalism used measures that could be considered information overload. Four of those studies used scales with a combination of information overload and fatalism components. These questions were combined in a single scale to investigate the relationship between media exposure and fatalism, which precludes an examination of the difference between information overload and fatalism in studies utilizing a scale. Han et al. (2009) and Nagler (2014) included only the HINTS confusion component (‘There are so many recommendations about preventing cancer, it’s hard to know which ones to follow’) in their studies. Portnoy et al. (2014) included only the HINTS pessimism component (‘It seems like almost everything causes cancer’). Lee and Niederdeppe (2011) and Chung (2014) used a combination of the pessimism and confusion components to measure fatalism. Only one study (Niederdeppe et al., 2014) made a distinction between information overload and fatalism and found differential effects. Exposure to a combination of stories about potential cancer causes and prevention was found to predict information overload, while fatalism was only predicted for individuals who do not pay a good deal of attention to health topics and only when a cause story was combined with an uncertain prevention story.
Discussion
Our aim for the present study was to create a better understanding of the relationship between fatalism and the media by examining the evidence for causal influence. However, this process is severely complicated by measurement confounds. Only 4 of the 14 studies used a non-conflated measure of fatalism (i.e. Jensen & Hurley, 2012; McClure & Velluppillai, 2013; Miles et al., 2008; Niederdeppe et al., 2014). The results of the studies with designs required to make stronger causal claims suggest that fatalism is affected by media exposure. When examining studies that used a mixture of fatalism and information overload measures, all four survey (including a panel study) studies found a relationship between media exposure and fatalism (Befort et al., 2013; Lee et al., 2012; Niederdeppe et al., 2010; Northup, 2014). The only study designed to make a causal claim suggested that fatalism is affected by media exposure as well (Lee et al., 2012). Overall, these results provide strong evidence for a relationship between media exposure and suggest that fatalism is affected by media exposure. However, more research is necessary with more generally accepted measures of fatalism.
Conflated constructs
One of two studies (Surlin, 1977) that reported no significant relationship between media exposure and fatalism actually defined and assessed fatalism as locus of control. While fatalism and locus of control are related constructs, previous literature suggests that there are discrete differences between these concepts (Boone et al., 1990; Espinosa de los Monteros & Gallo, 2011). In addition, most studies ostensibly measuring fatalism included potential information overload measures; five studies (Chung, 2014; Han et al., 2009; Lee & Niederdeppe, 2011; Nagler, 2014; Portnoy et al., 2014) included only fatalism measures suspect of measuring information overload. This high reliance on potential information overload measures might have a tremendous impact on the conclusions that can be drawn about the research investigating cultivation effects of media exposure on fatalism. Media exposure might not lead to fatalism, rather to the distinct effect of information overload. To avoid potential mistakes in the future, studies should include measures capable of making a distinction between these constructs. The cancer information overload scale has been shown to reliably make this distinction between fatalism and information overload (Jensen et al., 2014).
The overload segment might explain the surprising finding in studies investigating fatalistic beliefs. Research has shown that contrary to conventional beliefs, ethnic minorities do not score worse on all three items commonly used when examining fatalistic beliefs (Niederdeppe & Levy, 2007; Ramírez, Freres, et al., 2013). Ethnic minorities scored worse compared to non-Hispanic whites on the non-controversial item ‘There’s not much people can do to lower their chances of getting cancer.’ However, ethnic minorities scored better on the two items that might be capturing the information overload segment. One explanation for these differences between ethnicities on items capturing the information overload segment might be the structural barriers, including information access. For instance, non-Hispanic Whites are more likely to have access to Internet compared to other ethnicities (Ramírez, Freres, et al., 2013). Similar differences between ethnicities have also been found for seeking health information (Viswanath & Ackerson, 2011). Inequalities in access to information might therefore explain differences in information overload levels and lack of information overload and might be a protective factor (Han et al., 2009; Ramírez, 2014; Ramírez, Freres, et al., 2013). Therefore, simply increasing the amount of information about a given health topic may ultimately be counterproductive to health communication (Ramírez, 2014).
Not all media are alike
Of the four studies measuring fatalism (i.e. Jensen & Hurley, 2012; McClure & Velluppillai, 2013; Miles et al., 2008; Niederdeppe et al., 2014), none investigated a specific medium, making it impossible to draw conclusions. However, other studies described in this review using either a combination of fatalism measures and measures suspect of measuring information overload, or only measures suspect of measuring information overload suggested that television exposure relates and possibly cultivates information overload (and potentially fatalism). Interestingly, a subset of the results suggest that a special type of media exposure - that is, from the Internet - may reduce these beliefs (Befort et al., 2013; Han et al., 2009; Lee et al., 2012). This conclusion might be surprising in light of all the inaccurate and incomplete information on the Internet that might suggest overwhelm or confusion aspects (Benigeri & Pluye, 2003). It is possible, however, that the nature of the information behavior may play a role in this. Internet exposure implies a passive process. The studies using a passive exposure measure generally found no relationship (Lee & Niederdeppe, 2011; Niederdeppe et al., 2010). However, Lee et al. (2012) used a seeking and scanning combination and Befort et al. (2013) asked about information seeking. These studies found that Internet did lower information overload (and potentially fatalism). Individuals seeking and scanning information pay more attention and are more motivated than people who are merely exposed to process information (Jensen et al., 2016), potentially explaining the different results.
Related to this more active process of dealing with information is that individuals have more control over their exposure to information on the Internet (Kim & Stout, 2010), thereby possibly muting the effects of the overwhelming contradicting information found on the Internet. Research has also shown that individuals turn to the Internet to seek health information when they do not understand the information they have access to from other sources, or when they need additional information to make informed decisions (Nagler et al., 2010). However, Internet use may reduce information overload (and potentially fatalism) only for individuals with lower levels of education and health knowledge, suggesting rather that the Internet can fulfill an information need for individuals with insufficient knowledge about a topic. In contrast, Internet use could lead to information overload in more educated individuals, negating the beneficial effects of Internet use.
Future directions
The current fatalism research is riddled with fatalism measures and needs more work identifying which concepts are actually measuring fatalism. Fatalism has been conceptually defined similarly (e.g. Chavez et al., 1996; Egede & Ellis, 2010; Powe & Finnie, 2003; Rippetoe & Rogers, 1987) for years but this has not prevented an abundance in measures. The little work that has been done on constructing fatalism scales based on the larger fatalism literature indicates that fatalism is a multidimensional construct (Esparza et al., 2015; Shen et al., 2009). Evidence needs to be collected - especially in the form of hierarchical and bi-factor analyses - to identify if the constructs we are currently using to measure fatalism actually have a shared underlying dimension and are not conflated with fatalism. This synthesis of the current state of the literature examining a relationship between fatalism and media exposure also shows that there needs to be a better distinction between fatalism and related constructs. Studies that use the HINTS fatalism measures should run separate analyses for the measures suspect of measuring information overload. In general, studies should include measures capable of making a distinction between fatalism, locus of control, and information overload. By using constructs related to fatalism, instead of fatalism itself, the relationship between media exposure and fatalism can be misrepresented.
The cross-sectional nature of many of the studies included in this review does not permit us to postulate much about the explanation for the relationship between media exposure and fatalism. The only experiment capable of giving insight (Niederdeppe et al., 2014) is compatible with the EPPM given that uncertainty about cancer cause and prevention is likely to create a high-threat and low efficacy situation. Additional research is necessary to examine how media exposure might cause fatalism.
The results of the current review suggest that the relationship between media exposure and information overload (and potentially fatalism) differ per medium (e.g. television exposure enhances these beliefs while Internet exposure decreases them) and point toward the possibility of actively seeking information on the Internet to reduce information overload. Given the deliberate transition to a healthcare environment where patients are active participants in their own medical decision-making (Kelly et al., 2010), it is important to understand these different media effects. However, as we described above, it might not be the medium that is responsible for fatalism but how individuals use the media. Future studies should focus on this difference. Of particular interest is social media - an environment that is known for its controversial information - as recent research has shown the majority of U.S. adults (62%) receive their news from social media (Barthel, Micthel, & Holcomb, 2016; Gottfried & Shearer, 2016). In addition, social media is Internet exposure that might more closely resemble television exposure, compared to information seeking on the Internet. Social media may therefore provide insight if cultivation effects are the result of the medium or media use.
Lastly, the majority of the work examining the relationship between media exposure and fatalism is limited to perceptions regarding cancer. The focus on cancer perceptions is understandable because cancer is one of the leading causes of death in the United States (Chung, 2014). Additionally, cancer receives a great deal of media attention (Adelman & Verbrugge, 2000; Viswanath et al., 2006). However, it seems likely that this relationship extends beyond cancer (and other illnesses). Future studies should extend this work beyond cancer and explore this relationship in other topics that receive media attention that may be similarly contradictory or overwhelming in nature (e.g. climate change).
Conclusion
Only a few studies used a non-conflated measure of fatalism to examine the relationship between fatalism and media exposure. Overall, the results of this literature review provide some evidence for a relationship between media exposure and the limited data suggest a direction in which fatalism is affected by media exposure. This is salient because the media are often important information sources. However, media exposure does not always lead to negative outcomes. Research showing positive effects of exposure on cancer prevention behaviors such as increases in breast cancer screening (Yanovitzky & Blitz, 2000), colorectal cancer screening (Brown & Potosky, 1990), and diet behaviors (Ramírez, Freres, et al., 2013). Finally, the effects of media exposure on fatalistic and information overload beliefs are often small. However, as these results are found in a society with both heavy and light consumers of media, effects might be stronger for individuals with higher exposure. Future work should further investigate the relationship between media exposure and fatalism using measures capable of distinguishing between fatalism and related constructs. Additionally, studies should extend this relationship beyond cancer, attempt more research to investigate causal directions using longitudinal designs, and investigate the content to understand why media exposure may increase fatalistic beliefs.
Acknowledgment
We take this opportunity to thank the four anonymous reviewers and Editor-in-Chief Dr. Ewoldsen for their extensive feedback on our manuscript.
Appendix
Table A1.
Overview of included studies.
| Author(s) (date) | Aim of the study | Study population | Definition of fatalism | Measurement of fatalism | Measurement of exposure | Methods | Controlled for | Direction of association between fatalism and media exposure (p < .05, unless otherwise noted) | Effect size |
|---|---|---|---|---|---|---|---|---|---|
| Surlin (1977) | Examine race, education and fatalism as predictors of involvement in radio programming | 321 57% White, 43% Black |
‘The perceived inability of an individual to control his own destiny’ | One item. ‘There is not much that you can do about most of the important problems that we face today.’ Agree/neutral/disagree | One item radio exposure. I.e. ‘On the average, how much time per day do you listen to the radio?’ 30 min or less; more than 30 min. to 2 h; more than 2 h | Survey, cross-sectional | Race Education |
n.s. | R = 0.10 |
| Miles, Voorwinden, Chapman, and Wardle (2008) | Examine the interrelationship between cancer fear, cancer fatalism, and cancer information avoidance among older adults | 901/1580
female M = 59 |
Powe’s cancer fatalism. ‘The belief that death is inevitable when cancer is present’ | The Powe Fatalism Inventory, a 15-item questionnaire. E.g. ‘I believe if someone gets cancer it was meant to be’ | Information avoidance, a five-item measure. E.g. ‘I avoid watching TV programs about cancer’ | Survey, cross-sectional | -Demographics -Cancer history -Fear -Cancer threat beliefs -Cancer efficacy beliefs |
+ | B = 0.137 |
| Han et al. (2009) | Examine the associations between various sociodemographic factors, mass media exposures, and perceived ambiguity regarding recommendations for preventing different cancers | 3657/5586 female, median age group 50–64, 73% non-Hispanic White | HINTS: fatalistic beliefs, characterized by pessimism, helplessness, and confusion | HINTS confusion: ‘There are so many different recommendations about preventing [colon/skin/lung] cancer, it ‘s hard to know which ones to follow’ | Tv (two items), radio (two items), Internet (two items), newspaper (one item). E.g. ‘On a typical weekday, about how many hours do you watch television?’ | Survey (HINTS, 2005), cross-sectional | -Demographics Cancer -Information seeking |
Television + Newspaper + Internet health − |
Skin cancer OR = 1.67 Colon cancer OR = 1.47 Colon cancer OR = 0.9 |
| Niederdeppe etal. (2010) | Test associations between local TV news viewing and fatalistic beliefs about cancer prevention | 50.3% female, n = 897, M = 46.7 SD = 16.7, 75.3% Caucasian | HINTS: fatalistic beliefs, characterized by pessimism, helplessness, and confusion | HINTS pessimism, helplessness, and confusion: e.g. ‘It seems like almost everything causes cancer’ | Local TV news viewing. E.g. ‘In the past seven days, on how many days did you watch the local news on TV?’ | Survey (ANHCS, 2005), cross-sectional | -Demographics -Marital status -Household size -Self-rated health -Body-mass index -Smoking -Binge drinking -National news watching -Newspaper reading -Radio news/talk show listening -Internet use |
+ | B = 0.08 |
| Jensen et al. (2011) | Examine whether hedging shapes the perceptions of news consumers | 569/1082 female M = 20, SD = 2 79.9% Caucasian, 12.4% Asian or Pacific Islander, 4% African American | Powe’s cancer fatalism. ‘The belief that death is inevitable when cancer is present’ | The Powe Fatalism Inventory, a 15-item questionnaire. E.g. ‘I believe if someone gets cancer it was meant to be’ | Exposed to a news article, manipulated to include hedged (i.e. describing limitations and uncertainties) or streamlined (i.e. not recognizing the ambiguity of the information) information | Experiment,
multiple message |
Randomized experiment | Hedged articles: – | Cohen’s d = 0.22 |
| Lee and Niederdeppe (2011) | Test lagged association between overall TV viewing, local TV news viewing, and fatalistic beliefs about cancer prevention | 53.2% female, n = 425–447, M = 47.7, SD = 17.5, 74.1% Caucasian | HINTS: fatalistic beliefs, characterized by pessimism, helplessness, and confusion | HINTS pessimism and confusion: E.g. ‘It seems like almost everything causes cancer’ | Overall TV (two items), local TV (one
item), other media use (control variable, four
items) E.g. ‘During a typical weekend, about how many total hours do you watch TV?’ |
Survey (ANHCS, 2005, two waves), longitudinal panel survey design | -Demographics -Marital status -Household size -Religious events attendance -Self-rated health -Body-mass index -Smoking -Binge drinking -Newspaper reading -Radio news listening -Internet news reading |
Media exposure predicting fatalism:
+ fatalism predicting overall TV viewing: n.s. fatalism predicting local TV news viewing: n.s. |
Overall TV viewing B
= 0.10 local TV news viewing B = 0.13 cancer fatalism B = 0.06 cancer fatalism B = −0.01 |
| Lee, Niederdeppe, and Freres (2012) | Examine the effect of Internet use for health information on changes in cancer fatalism | 843/1646 female M =
53 73–75% White, 11% African American, 10–9% Hispanic, 5% Other |
HINTS: Fatalistic beliefs, characterized by pessimism, helplessness, and confusion | HINTS pessimism, helplessness, and confusion. E.g. ‘It seems like almost everything causes cancer’ | Internet use for health information with two questions. E.g. ‘How often have you read health information on the Internet in the past 30 days?’ | Survey (two waves), longitudinal panel survey design | -Demographics -Marital status -Household size -Religious events attendance -Self-rated health -Body-mass index -Smoking -Personal cancer experience -Significant other cancer experience -Doctor visits -Health knowledge -Health information acquisition from other sources |
– | B = −0.07 |
| McClure and Velluppillai (2013) | Examine whether exposure to newspaper messages about a recent earthquake affects damage attributions, judgments of preventability, fatalism, and estimates of damage. | N = 75 | Fatalistic people think that nothing they do will influence their outcomes in an earthquake less likely to prepare for disasters. | Turner Nigg, and Paz (1986) four fatalism items. E.g. ‘There is nothing people can do about earthquakes, so there is no point trying to prepare for that emergency.’ | Two versions of news reports, fatalistic (i.e. describing widespread damage and anecdotal information) or informed (i.e. factual information about building performance and proportion of buildings damaged) on the Canterbury earthquake. | Experiment, multiple message |
Randomized experiment |
n.s. | 1) Cohen’s d =
−0.15 2) Cohen’s d = −0.07 3) Cohen’s d = −0.16 4) Cohen’s d = −0.43 |
| Befort, Nazir, Engelman, and Choi (2013) | Examine rural-urban differences in fatalistic beliefs about cancer prevention, cancer information sources, and trust in health information. | 3944/7674 female. Median age group 40–49. 83% White non-Hispanic, 7.9% Black non-Hispanic, 5.1% Hispanic. |
HINTS: Fatalistic beliefs, characterized by pessimism, helplessness, and confusion | HINTS pessimism, helplessness, and confusion E.g. ‘It seems like almost everything causes cancer.’ | Primary cancer information source: ‘The most recent time you looked for cancer information, where did you go first?’ Response options: books/-newspaper- /magazine/- newspaper, internet. | Survey (HINTS, 2008), cross-sectional | -Demographics -Marital status -Trust |
– | Internet: everything causes cancer OR = 0.71 so many recommendations OR = 0.76 |
| Northup (2014) | Examine how television use impacts nutritional views and knowledge | 403/591 female M = 22, SD = 5 29.8% Caucasian, 26.1% Hispanic, 19.3% African American, 19.1% Asian | HINTS: fatalistic beliefs, characterized by pessimism, helplessness, and confusion | Five statements about healthy eating, based on HINTS. E.g. ‘There are so many recommendations about eating a healthy diet, it’s hard to know which ones to follow’ | Overall Television and News Media Use. E.g. ‘During a typical weekend, about how many hours do you watch television (news) during the following time periods?’ | Survey, cross-sectional | -Demographics -Body-mass index -Food preference -interest in healthy eating |
+ | Total television use B = 0.032 |
| Nagler (2014) | Assess whether exposure to contradictory nutrition messages in the public information environment have negative effects on health | 353/631 female M = 51, SD = 16.5, >80% non-Hispanic White | Not explicitly stated | Nutrition confusion: E.g. ‘I find nutrition recommendations to be confusing’ | Media included television, radio, newspapers, magazines, and the Internet | Survey (ANHCS, 2010), cross-sectional | -Demographics -Mistrust |
+ | B = 0.13 |
| Niederdeppe et al. (2014) | Examine the extent to which both volume and content distinguish local TV news coverage of cancer from other sources, and the extent to which those differences matter in shaping fatalistic and overloaded beliefs | 290/558 female M = 29, SD = 14 57% White, 34% Asian, 10% Black, 9% Hispanic/Latino | The inevitability of getting cancer | The Powe Fatalism Inventory, a 15-item questionnaire. E.g. ‘If someone is meant to get cancer they will get it no matter what they do’ | 15 text only news story conditions | Experiment | Randomized experiment | Amount of stories: n.s. Story content: + |
B = 0.12 B = −0.25 |
| Portnoy et al. (2014) | Examine the relationship between two high-profile lung cancer events and fatalism | 3543/5392 female M = 52, SD = 17. 77% non-Hispanic White, 9% Hispanic, 9% non-Hispanic Black | HINTS: fatalistic beliefs, characterized by pessimism, helplessness, and confusion | HINTS pessimism. E.g. ‘It seems like almost everything causes [lung/colon/skin] cancer.’ Agree/disagree | Amount of newspaper reading and television news viewing in the previous week | Survey (HINTS, 2005), cross-sectional | -Demographics -Smoking -Insurance status -Cancer history |
Television: n.s. Newspaper: n.s. |
Television = 1.02 Newspaper: OR = 0.081 |
| Chung (2014) | Examine the cultivation effects medical dramas have on viewers’ beliefs in cancer fatalism | 6102/11555 female M = 48, SD = 16 White 72.7%, Hispanic 12.9%, Black 8.5% | HINTS: fatalistic beliefs, characterized by pessimism, helplessness, and confusion | Two items: ‘It seems like almost everything causes cancer’ and ‘There are so many recommendations about preventing cancer, it’s hard to know which ones to follow’ | Viewing of medical television dramas and other media. E.g. ‘In the past seven days, on how many days did you (read a newspaper, watch the national news on television, watch the local news on television, or listen to radio talk shows or news)?’ | Survey (ANHCS, 2011), cross-sectional | -Demographics -Health status |
Television: + Newspaper and radio: − |
Local TV B = 0.1
Newspaper B = −0.31 Radio B = −0.042 |
Note: +: a significant positive relationship between fatalism and media exposure; −: a significant negative relationship between fatalism and media exposure; n.s.: no significant relationship between fatalism and media exposure, M: mean, SD: standard deviation, B represents standardized coefficients.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Abraído-Lanza AF, Chao MT, & Flórez KR (2005). Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Social Science & Medicine, 61(6), 1243–1255. doi: 10.1016/j.socscimed.2005.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraído-Lanza AF, Viladrich A, Flórez KR, Céspedes A, Aguirre AN, & De La Cruz AA (2007). Commentary: Fatalismo reconsidered: A cautionary note for health-related research and practice with Latino populations. Ethnicity & Disease, 17(1), 153–158. [PMC free article] [PubMed] [Google Scholar]
- Adelman RC, & Verbrugge LM (2000). Death makes news: The social impact of disease on newspaper coverage. Journal of Health and Social Behavior, 41(3), 347–367. doi: 10.2307/2676325 [DOI] [PubMed] [Google Scholar]
- Arora NK, Hesse BW, Rimer BK, Viswanath K, Clayman ML, & Croyle RT (2008). Frustrated and confused: The American public rates its cancer-related information-seeking experiences. Journal of General Internal Medicine, 23(3), 223–228. doi: 10.1007/s11606-007-0406-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barthel M, Micthel A, & Holcomb J (2016). Many Americans believe fake news is sowing confusion. Retrieved from http://www.journalism.org/2016/12/15/many-americans-believe-fake-news-is-sowing-confusion.
- Basil M, & Witte K (2012). Health risk message design using the extended parallel process model. In Cho H (Ed.), Health communication message design: Theory and practice (pp. 41–58). Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Befort CA, Nazir N, Engelman K, & Choi W (2013). Fatalistic cancer beliefs and information sources among rural and urban adults in the USA. Journal of Cancer Education, 28(3), 521–526. doi: 10.1007/s13187-013-0496-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benigeri M, & Pluye P (2003). Shortcomings of health information on the Internet. Health Promotion International, 18(4), 381–386. doi: 10.1093/heapro/dag409 [DOI] [PubMed] [Google Scholar]
- Berman SH, & Wandersman A (1990). Fear of cancer and knowledge of cancer: A review and proposed relevance to hazardous waste sites. Social Science & Medicine, 31(1), 81–90. doi: 10.1016/0277-9536(90)90013-I [DOI] [PubMed] [Google Scholar]
- Bilandzic H, & Busselle RW (2008). Transportation and transportability in the cultivation of genre-consistent attitudes and estimates. Journal of Communication, 58(3), 508–529. doi: 10.1111/j.1460-2466.2008.00397.x [DOI] [Google Scholar]
- Boone C, De Brabander B, Gerits P, & Willeme P (1990). Relation of scores on Rotter’s i-e scale to short-term and long-term control expectancies and fatalism. Psychological Reports, 66(3c), 1107–1111. doi: 10.2466/pr0.1990.66.3c.1107 [DOI] [PubMed] [Google Scholar]
- Brodie M, Hamel EC, Altman DE, Blendon RJ, & Benson JM (2003). Health news and the American public, 1996–2002. Journal of Health Politics, Policy and Law, 28(5), 927–950. doi: 10.1215/03616878-28-5-927 [DOI] [PubMed] [Google Scholar]
- Brown ML, & Potosky AL (1990). The presidential effect: The public health response to media coverage about Ronald Reagan’s colon cancer episode. Public Opinion Quarterly, 54(3), 317–329. doi: 10.1086/269209 [DOI] [PubMed] [Google Scholar]
- Carlson M (2017). Facebook in the news. Digital Journalism, 1–17. doi: 10.1080/21670811.2017.1298044 [DOI] [Google Scholar]
- Chavez L, Hubbell F, Mishra S, & Valdez R (1996). The influence of fatalism on self-reported use of Papanicolaou smears. American Journal of Preventive Medicine, 13(6), 418–424. [PubMed] [Google Scholar]
- Chory-Assad RM, & Tamborini R (2003). Television exposure and the public’s perceptions of physicians. Journal of Broadcasting & Electronic Media, 47(2), 197–215. doi: 10.1207/s15506878jobem4702_3 [DOI] [Google Scholar]
- Chung JE (2014). Medical dramas and viewer perception of health: Testing cultivation effects. Human Communication Research, 40(3), 333–349. doi: 10.1111/hcre.12026 [DOI] [Google Scholar]
- Clarke JN, & Everest MM (2006). Cancer in the mass print media: Fear, uncertainty and the medical model. Social Science & Medicine, 62(10), 2591–2600. doi: 10.1016/j.socscimed.2005.11.021 [DOI] [PubMed] [Google Scholar]
- Cohen D, & Nisbett RE (1998). Are there differences in fatalism between rural southerners and midwesterners? Journal of Applied Social Psychology, 28(23), 2181–2195. doi: 10.1111/j.1559-1816.1998.tb01366.x [DOI] [Google Scholar]
- Cohen EL, Caburnay CA, Luke DA, Rodgers S, Cameron GT, & Kreuter MW (2008). Cancer coverage in general-audience and black newspapers. Health Communication, 23(5), 427–435. doi: 10.1080/10410230802342176 [DOI] [PubMed] [Google Scholar]
- Conrad ME, Brown P, & Conrad MG (1996). Fatalism and breast cancer in black women. Annals of Internal Medicine, 125(11), 941–942. [DOI] [PubMed] [Google Scholar]
- Cuéllar I, Arnold B, & González G (1995). Cognitive referents of acculturation: Assessment of cultural constructs in Mexican Americans. Journal of Community Psychology, 23(4), 339–356. doi: [DOI] [Google Scholar]
- Davison C, Frankel S, & Smith GD (1992). The limits of lifestyle: Re-assessing ‘fatalism’ in the popular culture of illness prevention. Social Science & Medicine, 34(6), 675–685. doi: 10.1016/0277-9536(92)90195-V [DOI] [PubMed] [Google Scholar]
- Dreier P, & Martin CR (2010). How ACORN was framed: Political controversy and media agenda setting. Perspectives on Politics, 8(3), 761–792. doi: 10.1017/S1537592710002069 [DOI] [Google Scholar]
- Dudo AD, Dahlstrom MF, & Brossard D (2007). Reporting a potential pandemic: A risk-related assessment of Avian influenza coverage in U.S. Newspapers. Science Communication, 28(4), 429–454. doi: 10.1177/1075547007302211 [DOI] [Google Scholar]
- Egede LE, & Bonadonna RJ (2003). Diabetes self-management in African Americans: An exploration of the role of fatalism. The Diabetes Educator, 29(1), 105–115. [DOI] [PubMed] [Google Scholar]
- Egede LE, & Ellis C (2010). Development and psychometric properties of the 12-item diabetes fatalism scale. Journal of General Internal Medicine, 25(1), 61–66. doi: 10.1007/s11606-009-1168-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esparza OA, Wiebe JS, & Quiñones J (2015). Simultaneous development of a multidimensional fatalism measure in English and Spanish. Current Psychology, 34(4), 597–612. doi: 10.1007/s12144-014-9272-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espinosa de los Monteros KE, & Gallo LC (2011). The relevance of fatalism in the study of Latinas’ cancer screening behavior: A systematic review of the literature. International Journal of Behavioral Medicine, 18(4), 310–318. doi: 10.1007/s12529-010-9119-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman L, Hart PS, & Milosevic T (2015). Polarizing news? Representations of threat and efficacy in leading US newspapers’ coverage of climate change. Public Understanding of Science. doi: 10.1177/0963662515595348 [DOI] [PubMed] [Google Scholar]
- Flórez KR, Aguirre AN, Viladrich A, Céspedes A, De La Cruz AA, & Abraído-Lanza AF (2009). Fatalism or destiny? A qualitative study and interpretative framework on Dominican women’s breast cancer beliefs. Journal of Immigrant and Minority Health, 11(4), 291–301. doi: 10.1007/s10903-008-9118-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floyd DL, Prentice-Dunn S, & Rogers RW (2000). A meta-analysis of research on protection motivation theory. Journal of Applied Social Psychology, 30(2), 407–429. doi: 10.1111/j.1559-1816.2000.tb02323.x [DOI] [Google Scholar]
- Foss KA (2011). ‘When we make mistakes, people die!’ Constructions of responsibility for medical errors in televised medical dramas, 1994–2007. Communication Quarterly, 59(4), 484–506. doi: 10.1080/01463373.2011.597350 [DOI] [Google Scholar]
- Freeman HP (1989). Cancer in the socioeconomically disadvantaged. CA: A Cancer Journal for Clinicians, 39(5), 266–288. doi: 10.3322/canjclin.39.5.266 [DOI] [PubMed] [Google Scholar]
- Gerbner G, Gross L, Morgan M, & Signorielli N (1980). The ‘mainstreaming’ of America: Violence profile no. 11. Journal of Communication, 30(3), 10–29. doi: 10.1111/j.1460-2466.1980.tb01987.x [DOI] [PubMed] [Google Scholar]
- Gill EA, & Babrow AS (2007). To hope or to know: Coping with uncertainty and ambivalence in women’s magazine breast cancer articles. Journal of Applied Communication Research, 35(2), 133–155. doi: 10.1080/00909880701263029 [DOI] [Google Scholar]
- Goldberg JP, & Sliwa SA (2011). Communicating actionable nutrition messages: Challenges and opportunities. Proceedings of the Nutrition Society, 70(1), 26–37. doi: 10.1017/S0029665110004714 [DOI] [PubMed] [Google Scholar]
- Goodall C, Sabo J, Cline R, & Egbert N (2012). Threat, efficacy, and uncertainty in the first 5 months of national print and electronic news coverage of the H1N1 virus. Journal of Health Communication, 17(3), 338–355. doi: 10.1080/10810730.2011.626499 [DOI] [PubMed] [Google Scholar]
- Gottfried J, & Shearer E (2016). News use across social media platforms 2016. Retrieved from http://www.journalism.org/2016/05/26/news-use-across-social-media-platforms-2016.
- Gross K, & Aday S (2003). The scary world in your living room and neighborhood: Using local broadcast news, neighborhood crime rates, and personal experience to test agenda setting and cultivation. Journal of Communication, 53(3), 411–426. doi: 10.1111/j.1460-2466.2003.tb02599.x [DOI] [Google Scholar]
- Hamilton JB, Best NC, Galbraith KV, Worthy VC, & Moore LAD (2014). Strategies African-American cancer survivors use to overcome fears and fatalistic attitudes. Journal of Cancer Education, 1–7. doi: 10.1007/s13187-014-0738-3 [DOI] [PubMed] [Google Scholar]
- Han PKJ, Moser RP, Klein WMP, Beckjord EB, Dunlavy AC, & Hesse BW (2009). Predictors of perceived ambiguity about cancer prevention recommendations: Sociodemographic factors and mass media exposures. Health Communication, 24(8), 764–772. doi: 10.1080/10410230903242242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart PS, & Feldman L (2014). Threat without efficacy? Climate change on U.S. Network News. Science Communication, 36(3), 325–351. doi: 10.1177/1075547013520239 [DOI] [Google Scholar]
- He S, Shen Q, Yin X, Xu L, & Lan X (2014). Newspaper coverage of tobacco issues: An analysis of print news in Chinese cities, 2008–2011. Tobacco Control, 23(4), 345–352. doi: 10.1136/tobaccocontrol-2012-050545 [DOI] [PubMed] [Google Scholar]
- Hetsroni A, & Tukachinsky RH (2006). Television-world estimates, real-world estimates, and television viewing: A new scheme for cultivation. Journal of Communication, 56(1), 133–156. doi: 10.1111/j.1460-2466.2006.00007.x [DOI] [Google Scholar]
- Hurley RJ, Kosenko KA, & Brashers D (2011). Uncertain terms: Message features of online cancer news. Communication Monographs, 78(3), 370–390. doi: 10.1080/03637751.2011.565061 [DOI] [Google Scholar]
- Jensen JD, Carcioppolo N, King AJ, Bernat JK, Davis L, Yale R, & Smith J (2011). Including limitations in news coverage of cancer research: Effects of news hedging on fatalism, medical skepticism, patient trust, and backlash. Journal of Health Communication, 16(5), 486–503. doi: 10.1080/10810730.2010.546491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen JD, Carcioppolo N, King AJ, Scherr CL, Jones CL, & Niederdeppe J (2014). The cancer information overload (CIO) scale: Establishing predictive and discriminant validity. Patient Education and Counseling, 94(1), 90–96. doi: 10.1016/j.pec.2013.09.016 [DOI] [PubMed] [Google Scholar]
- Jensen JD, & Hurley RJ (2012). Conflicting stories about public scientific controversies: Effects of news convergence and divergence on scientists’ credibility. Public Understanding of Science, 21(6), 689–704. doi: 10.1177/0963662510387759 [DOI] [PubMed] [Google Scholar]
- Jensen JD, Liu M, Carcioppolo N, John KK, Krakow M, & Sun Y (2016). Health information seeking and scanning among US adults aged 50–75 years: Testing a key postulate of the information overload model. Health Informatics Journal. doi: 10.1177/1460458215627290 [DOI] [PubMed] [Google Scholar]
- Jensen JD, Moriarty CM, Hurley RJ, & Stryker JE (2010). Making sense of cancer news coverage trends: A comparison of three comprehensive content analyses. Journal of Health Communication, 15(2), 136–151. doi: 10.1080/10810730903528025 [DOI] [PubMed] [Google Scholar]
- Jones GK, Brewer KL, & Garrison HG (2000). Public expectations of survival following cardiopulmonary resuscitation. Academic Emergency Medicine, 7(1), 48–53. doi: 10.1111/j.1553-2712.2000.tb01891.x [DOI] [PubMed] [Google Scholar]
- Kelly B, Hornik R, Romantan A, Schwartz JS, Armstrong K, DeMichele A, … Wong N (2010). Cancer information scanning and seeking in the general population. Journal of Health Communication, 15(7), 734–753. doi: 10.1080/10810730.2010.514029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H, & Stout PA (2010). The effects of interactivity on information processing and attitude change: Implications for mental health stigma. Health Communication, 25(2), 142–154. doi: 10.1080/10410230903544936 [DOI] [PubMed] [Google Scholar]
- Lee C-J, Long M, Slater MD, & Song W (2014). Comparing local TV news with national TV news in cancer coverage: An exploratory content analysis. Journal of Health Communication, 19(12), 1330–1342. doi: 10.1080/10810730.2014.894598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C-J, & Niederdeppe J (2011). Genre-specific cultivation effects lagged associations between overall TV viewing, local TV news viewing, and fatalistic beliefs about cancer prevention. Communication Research, 38(6), 731–753. doi: 10.1177/0093650210384990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C-J, Niederdeppe J, & Freres D (2012). Socioeconomic disparities in fatalistic beliefs about cancer prevention and the internet. Journal of Communication, 62(6), 972–990. doi: 10.1111/j.1460-2466.2012.01683.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowry DT, Nio TCJ, & Leitner DW (2003). Setting the public fear agenda: A longitudinal analysis of network TV crime reporting, public perceptions of crime, and FBI crime statistics. Journal of Communication, 53(1), 61–73. doi: 10.1111/j.1460-2466.2003.tb03005.x [DOI] [Google Scholar]
- Mayo RM, Ureda JR, & Parker VG (2001). Importance of fatalism in understanding mammography screening in rural elderly women. Journal of Women & Aging, 13(1), 57–72. doi: 10.1300/J074v13n01_05 [DOI] [PubMed] [Google Scholar]
- McClure J, & Velluppillai J (2013). The effects of news media reports on earthquake attributions and preventability judgments: Mixed messages about the Canterbury earthquake. Australasian Journal of Disaster and Trauma Studies, 2013 (1), 27–36. [Google Scholar]
- Michielutte R, Dignan MB, Sharp PC, Boxley J, & Wells HB (1996). Skin cancer prevention and early detection practices in a sample of rural women. Preventive Medicine, 25(6), 673–683. doi: 10.1006/pmed.1996.0106 [DOI] [PubMed] [Google Scholar]
- Miles A, Voorwinden S, Chapman S, & Wardle J (2008). Psychologic predictors of cancer information avoidance among older adults: The role of cancer fear and fatalism. Cancer Epidemiology Biomarkers & Prevention, 17(8), 1872–1879. doi: 10.1158/1055-9965.EPI-08-0074 [DOI] [PubMed] [Google Scholar]
- Morgan M, Shanahan J, & Signorielli N (2015). Yesterday’s new cultivation, tomorrow. Mass Communication and Society, 18(5), 674–699. doi: 10.1080/15205436.2015.1072725 [DOI] [Google Scholar]
- Nagler RH (2014). Adverse outcomes associated with media exposure to contradictory nutrition messages. Journal of Health Communication, 19(1), 24–40. doi: 10.1080/10810730.2013.798384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagler RH, & Hornik RC (2012). Measuring media exposure to contradictory health information: A comparative analysis of four potential measures. Communication Methods and Measures, 6(1), 56–75. doi: 10.1080/19312458.2011.651348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagler RH, Romantan A, Kelly BJ, Stevens RS, Gray SW, Hull SJ, … Hornik RC (2010). How do cancer patients navigate the public information environment? Understanding patterns and motivations for movement among information sources. Journal of Cancer Education, 25, 360–370. doi: 10.1007/s13187-010-0054-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neff JA, & Hoppe SK (1993). Race/ethnicity, acculturation, and psychological distress: Fatalism and religiosity as cultural resources. Journal of Community Psychology, 21(1), 3–20. doi: [DOI] [Google Scholar]
- Nelson D, Kreps G, Hesse B, Croyle R, Willis G, Arora N, … Alden S (2004). The health information national trends survey (HINTS): Development, design, and dissemination. Journal of Health Communication, 9(5), 443–460. doi: 10.1080/10810730490504233 [DOI] [PubMed] [Google Scholar]
- Niederdeppe J, Fowler EF, Goldstein K, & Pribble J (2010). Does local television news coverage cultivate fatalistic beliefs about cancer prevention? Journal of Communication, 60(2), 230–253. doi: 10.1111/j.1460-2466.2009.01474.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niederdeppe J, Lee T, Robbins R, Kim HK, Kresovich A, Kirshenblat D, … Fowler EF (2014). Content and effects of news stories about uncertain cancer causes and preventive behaviors. Health Communication, 29(4), 332–346. doi: 10.1080/10410236.2012.755603 [DOI] [PubMed] [Google Scholar]
- Niederdeppe J, & Levy AG (2007). Fatalistic beliefs about cancer prevention and three prevention behaviors. Cancer Epidemiology Biomarkers & Prevention, 16(5), 998–1003. doi: 10.1158/1055-9965.EPI-06-0608 [DOI] [PubMed] [Google Scholar]
- Northup T (2014). Understanding the relationship between television use and unhealthy eating: The mediating role of fatalistic views of eating well and nutritional knowledge. The International Journal of Communication and Health, 1(3), 10–15. [Google Scholar]
- Pérez-Stable E, Sabogal F, Otero-Sabogal R, Hiatt R, & McPhee S (1992). MIsconceptions about cancer among Latinos and Anglos. JAMA: The Journal of the American Medical Association, 268(22), 3219–3223. doi: 10.1001/jama.1992.03490220063029 [DOI] [PubMed] [Google Scholar]
- Pfau M, Mullen LJ, & Garrow K (1995). The influence of television viewing on public perceptions of physicians. Journal of Broadcasting & Electronic Media, 39(4), 441–458. doi: 10.1080/08838159509364318 [DOI] [Google Scholar]
- Portnoy DB, Leach CR, Kaufman AR, Moser RP, & Alfano CM (2014). Reduced fatalism and increased prevention behavior after two high-profile lung cancer events. Journal of Health Communication, 19(5), 577–592. doi: 10.1080/10810730.2013.821553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powe BD (1995). Fatalism among elderly African Americans: Effects on colorectal cancer screening. Cancer Nursing, 18(5), 385–392. [PubMed] [Google Scholar]
- Powe BD (2001). Cancer fatalism among elderly African American women. Journal of Psychosocial Oncology, 19(3–4), 85–95. doi: 10.1300/J077v19n03_07 [DOI] [PubMed] [Google Scholar]
- Powe BD, & Finnie R (2003). Cancer fatalism: The state of the science. Cancer Nursing, 26(6), 454–465; quiz 466–467. [DOI] [PubMed] [Google Scholar]
- Powe BD, & Weinrich S (1999). An intervention to decrease cancer fatalism among rural elders. Oncology Nursing Forum, 26(3), 583–588. [PubMed] [Google Scholar]
- Quick BL (2009). The effects of viewing grey’s anatomy on perceptions of doctors and patient satisfaction. Journal of Broadcasting & Electronic Media, 53(1), 38–55. doi: 10.1080/08838150802643563 [DOI] [Google Scholar]
- Ramírez AS (2014). Fatalism and cancer risk knowledge among a sample of highly acculturated Latinas. Journal of Cancer Education, 29(1), 50–55. doi: 10.1007/s13187-013-0541-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramírez AS, Finney Rutten LJ, Oh A, Leyva Vengoechea B, Moser RP, Vanderpool RC, & Hesse BW (2013). Perceptions of cancer controllability and cancer risk knowledge: The moderating role of race, ethnicity, and acculturation. Journal of Cancer Education, 28(2), 254–261. doi: 10.1007/s13187-013-0450-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramírez AS, Freres D, Martinez LS, Lewis N, Bourgoin A, Kelly BJ, … Hornik RC (2013). Information seeking from media and family/friends increases the likelihood of engaging in healthy lifestyle behaviors. Journal of Health Communication, 18(5), 527–542. doi: 10.1080/10810730.2012.743632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rippetoe PA, & Rogers RW (1987). Effects of components of protection-motivation theory on adaptive and maladaptive coping with a health threat. Journal of Personality and Social Psychology: Personality Processes and Individual Differences, 52(3), 596–604. doi: 10.1037/0022-3514.52.3.596 [DOI] [PubMed] [Google Scholar]
- Romer D, Jamieson KH, & Aday S (2003). Television news and the cultivation of fear of crime. Journal of Communication, 53(1), 88–104. doi: 10.1111/j.1460-2466.2003.tb03007.x [DOI] [Google Scholar]
- Rotter JB (1966). Generalized expectancies for internal versus external control of reinforcement. Psychological Monographs: General and Applied, 80(1), 1–28. [PubMed] [Google Scholar]
- Ruiu G (2012, July 16). Is fatalism a cultural belief? An empirical analysis on the origin of fatalistic tendencies (MPRA Paper). Retrieved May 20, 2015, from http://mpra.ub.uni-muenchen.de/41705/
- Rundmo T, & Hale AR (2003). Managers’ attitudes towards safety and accident prevention. Safety Science, 41(7), 557–574. doi: 10.1016/S0925-7535(01)00091-1 [DOI] [Google Scholar]
- Russell C (1999). Living can be hazardous to your health: How the news media cover cancer risks. JNCI Monographs, 1999(25), 167–170. [DOI] [PubMed] [Google Scholar]
- Scheier MF, & Bridges MWM (1995). Person variables and health: Personality predispositions and acute psychological states as shared determinants for disease. Psychosomatic Medicine, 57(3), 255–268. [DOI] [PubMed] [Google Scholar]
- Scheier MF, & Carver CS (1985). Optimism, coping, and health: Assessment and implications of generalized outcome expectancies. Health Psychology, 4(3), 219–247. doi: 10.1037/0278-6133.4.3.219 [DOI] [PubMed] [Google Scholar]
- Scheufele DA, Nisbet MC, & Brossard D (2003). Pathways to political participation? Religion, communication contexts, and mass media. International Journal of Public Opinion Research, 15(3), 300–324. doi: 10.1093/ijpor/15.3.300 [DOI] [Google Scholar]
- Schnoll RA, Malstrom M, James C, Rothman RL, Miller SM, Ridge JA, … Goldberg M (2002). Correlates of tobacco use among smokers and recent quitters diagnosed with cancer. Patient Education and Counseling, 46(2), 137–145. doi: 10.1016/S0738-3991(01)00157-4 [DOI] [PubMed] [Google Scholar]
- Schwartz LM, & Woloshin S (2002). News media coverage of screening mammography for women in their 40s and tamoxifen for primary prevention of breast cancer. JAMA, 287(23), 3136–3142. doi: 10.1001/jama.287.23.3136 [DOI] [PubMed] [Google Scholar]
- Shanahan J, & Morgan M (1999). Television and its viewers: Cultivation theory and research. Cambridge: Cambridge University Press. [Google Scholar]
- Shen L, & Condit CM (2012). Addressing fatalism with health messages. In Cho H (Ed.), Health communication message design: Theory and practice(pp. 191–208). Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Shen L, Condit CM, & Wright L (2009). The psychometric property and validation of a fatalism scale. Psychology & Health, 24(5), 597–613. doi: 10.1080/08870440801902535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shim M, Kim Y-C, Kye SY, & Park K (2016). News portrayal of cancer: Content analysis of threat and efficacy by cancer type and comparison with incidence and mortality in Korea. Journal of Korean Medical Science, 31(8), 1231–1238. doi: 10.3346/jkms.2016.31.8.1231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrum LJ, Burroughs JE, & Rindfleisch A (2003). A process model of consumer cultivation: The role of television is a function of the type of judgement. In Shrum LJ (Ed.), The psychology of entertainment media: Blurring the lines between entertainment and persuasion (pp. 177–191). Mahwah, NJ: Lawrence Erlbaum. [Google Scholar]
- Shrum LJ, & Lee J (2012). Television’s persuasive narratives: How television influences values, attitudes, and beliefs. In Shrum LJ (Ed.) The psychology of entertainment media: Blurring the lines between entertainment and persuasion (2nd ed., pp. 147–168). New York, NJ: Routledge. [Google Scholar]
- Shrum LJ, Lee J, Burroughs JE, & Rindfleisch A (2011). An online process model of second-order cultivation effects: How television cultivates materialism and its consequences for life satisfaction. Human Communication Research, 37(1), 34–57. doi: 10.1111/j.1468-2958.2010.01392.x [DOI] [Google Scholar]
- Spurlock W, & Cullins L (2005). Cancer fatalism and breast cancer screening in African American women. The ABNF Journal: Official Journal of the Association of Black Nursing Faculty in Higher Education, Inc, 17(1), 38–43. [PubMed] [Google Scholar]
- Squiers LB, Holden DJ, Dolina SE, Kim AE, Bann CM, & Renaud JM (2011). The public’s response to the U.S. preventive services task force’s 2009 recommendations on mammography screening. American Journal of Preventive Medicine, 40(5), 497–504. doi: 10.1016/j.amepre.2010.12.027 [DOI] [PubMed] [Google Scholar]
- Straughan PT, & Seow A (1998). Fatalism reconceptualized: A concept to predict health screening behavior. Journal of Gender, Culture, and Health, 3(2), 85–100. doi: 10.1023/A:1023278230797 [DOI] [Google Scholar]
- Surlin SH (1977). Race, education and fatalism: Predictors of involvement in radio programming. Journal of Broadcasting, 21(4), 413–426. doi: 10.1080/08838157709363851 [DOI] [Google Scholar]
- Taubes G (1995). Epidemiology faces its limits. Science, 269(5221), 164–169. doi: 10.1126/science.7618077 [DOI] [PubMed] [Google Scholar]
- Turner RH, Nigg JM, & Paz DH (1986). Waiting for disaster: Earthquake watch in California. Jackson, TN: University of California press. [Google Scholar]
- Unger JB, Ritt-Olson A, Teran L, Huang T, Hoffman BR, & Palmer P (2002). Cultural values and substance use in a multiethnic sample of California adolescents. Addiction Research & Theory, 10(3), 257–279. doi: 10.1080/16066350211869 [DOI] [Google Scholar]
- Urizar GG, & Sears SF (2006). Psychosocial and cultural influences on cardiovascular health and quality of life among Hispanic cardiac patients in south Florida. Journal of Behavioral Medicine, 29(3), 255–268. doi: 10.1007/s10865-006-9050-y [DOI] [PubMed] [Google Scholar]
- Van den Bulck JJM (2002). The impact of television fiction on public expectations of survival following inhospital cardiopulmonary resuscitation by medical professionals. Journal of Emergency Medicine, 9(4), 325–329. [DOI] [PubMed] [Google Scholar]
- Viswanath K, & Ackerson LK (2011). Race, ethnicity, language, social class, and health communication inequalities: A nationally-representative cross-sectional study. PLoS ONE, 6(1), e14550. doi: 10.1371/journal.pone.0014550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viswanath K, Breen N, Meissner H, Moser RP, Hesse BW, Steele WR, & Rakowski W (2006). Cancer knowledge and disparities in the information age. Journal of Health Communication, 11, 1–17. doi: 10.1080/10810730600637426 [DOI] [PubMed] [Google Scholar]
- Viswanath K, Nagler R, Bigman-Galimore C, McCauley M, Jung M, & Ramanadhan S (2012). The communications revolution and health inequalities in the 21st century: Implications for cancer control. Cancer Epidemiology, Biomarkers & Prevention : A Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology, 21(10), 1701–1708. doi: 10.1158/1055-9965.EPI-12-0852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weeks BE, Friedenberg LM, Southwell BG, & Slater JS (2012). Behavioral consequences of conflict-oriented health news coverage: The 2009 mammography guideline controversy and online information seeking. Health Communication, 27(2), 158–166. doi: 10.1080/10410236.2011.571757 [DOI] [PubMed] [Google Scholar]
- Witte K (1992). Putting the fear back into fear appeals: The extended parallel process model. Communication Monographs, 59(4), 329–349. doi: 10.1080/03637759209376276 [DOI] [Google Scholar]
- Witte K, & Allen M (2000). A meta-analysis of fear appeals: Implications for effective public health campaigns. Health Education & Behavior, 27(5), 591–615. doi: 10.1177/109019810002700506 [DOI] [PubMed] [Google Scholar]
- Woloshin S, Schwartz LM, Byram SJ, Sox HC, Fischhoff B, & Welch HG (2000). Women’s understanding of the mammography screening debate. Archives of Internal Medicine, 160(10), 1434–1440. doi: 10.1001/archinte.160.10.1434 [DOI] [PubMed] [Google Scholar]
- Yanovitzky I, & Blitz CL (2000). Effect of media coverage and physician advice on utilization of breast cancer screening by women 40 years and older. Journal of Health Communication, 5(2), 117–134. doi: 10.1080/108107300406857 [DOI] [PubMed] [Google Scholar]
- Yeh CJ, Inman AG, Kim AB, & Okubo Y (2006). Asian American families’ collectivistic coping strategies in response to 9/11. Cultural Diversity and Ethnic Minority Psychology, 12(1), 134–148. doi: 10.1037/1099-9809.12.1.134 [DOI] [PubMed] [Google Scholar]
- Zimrin H (1986). A profile of survival. Child Abuse & Neglect, 10(3), 339–349. doi: 10.1016/0145-2134(86)90009-8 [DOI] [PubMed] [Google Scholar]


