Abstract
Expansion of the Medicare Advantage program during 2009–18 saw greater enrollment among racial/ethnic minorities and other traditionally marginalized groups. Growth was more rapid among Black, Hispanic, and dually enrolled beneficiaries than among White and nondual beneficiaries. The implications of greater heterogeneity in the program for enrollee outcomes are uncertain.
Enrollment in Medicare Advantage (MA), the privately run and capitated segment of the Medicare program, increased from 23 percent of all beneficiaries in 2009 to 35 percent in 2018.1 It is vital to understand who is enrolling in Medicare Advantage and changes in enrollment patterns over time. We found that during this period, the percentage of all Black, Hispanic, and dually enrolled Medicare beneficiaries (those in Medicaid as well as Medicare) in Medicare Advantage increased from 23 percent to 38 percent, from 33 percent to 48 percent, and from 18 percent to 37 percent, respectively (exhibit 1). These rates of growth were larger than concurrent changes observed among White and nondual beneficiaries.
EXHIBIT 1. Enrollment in Medicare Advantage (MA), by race/ethnicity and dual enrollment status, 2009–18.
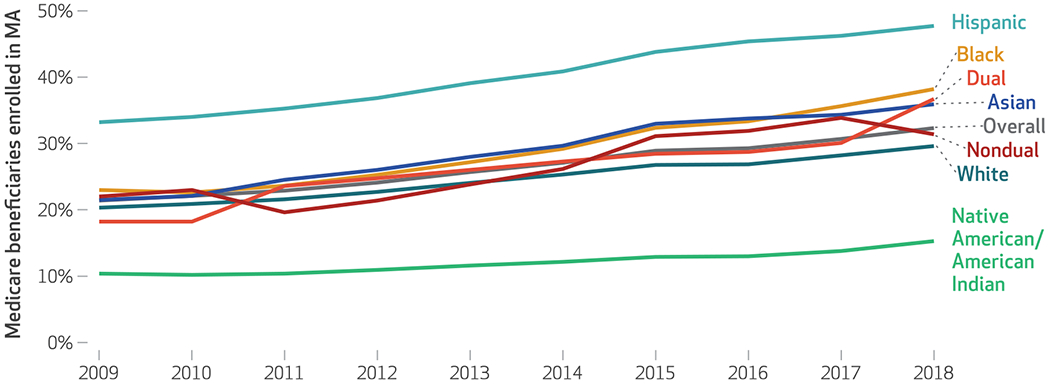
source Authors’ analysis of data from the Medicare Beneficiary Summary File, 2009–18. notes For each data point, the denominator is the number of all beneficiaries of that type in Medicare each year. The numerator is the number of those beneficiaries enrolled in an MA plan. Race/ethnicity variables are from the Research Triangle Institute race code. “Dual” indicates beneficiaries who are enrolled in both Medicaid and Medicare and includes those with both partial and full Medicaid coverage. “Nondual” indicates MA enrollees who are not enrolled in Medicaid. The average annual growth rate is 1.7 percent for Black, 1.6 percent for Hispanic, 1.0 percent for White, 1.6 percent for Asian, 0.5 percent for Native American/American Indian, 2.1 percent for dual, and 1.0 percent for nondual.
Recent developments may have fostered important shifts in the types of beneficiaries selecting MA plans. Expansion of plans with zero premiums, introduction of supplemental benefits to address social needs,2 and the formation of Special Needs Plans all may encourage a more heterogenous set of enrollees. The objective of this article is to present recent trends in MA enrollment among racial/ethnic minorities and other traditionally marginalized groups, to inform future work on the implications of those trends and the drivers behind them.
Study Data And Methods
We used the Medicare Master Beneficiary Summary File from the period 2009–18 as our primary source of enrollment and demographic information. We considered a beneficiary to be enrolled in Medicare Advantage during a given year if they were enrolled in an MA plan that January. Sensitivity analyses that defined MA enrollment based on plan participation for at least six months in a given year yielded similar findings. We considered a beneficiary to be not enrolled in Medicare Advantage if they were enrolled in traditional Medicare Parts A and B. From the Master Beneficiary Summary File, we used the Research Triangle Institute race code to classify enrollees by race/ethnicity; although not perfect, the code is an improvement over the base Master Beneficiary Summary File race/ethnicity variable.3 We also used the Master Beneficiary Summary File to determine whether beneficiaries were dually enrolled in Medicaid. In our primary analysis we considered both full and partial dual enrollees as dually enrolled; however, in sensitivity analyses we compared trends separately for both groups.
For information on MA plan characteristics, including Special Needs Plan type, premium, and star rating, we used publicly reported data from the Centers for Medicare and Medicaid Services (CMS). We linked these data to each enrollee using their contract and plan IDs from the Master Beneficiary Summary File. Using nine-digit ZIP codes available in that file, we also linked each beneficiary to the Social Deprivation Index.4 This is an index of neighborhood-level deprivation, calculated from nine variables in the American Community Survey and reported as a percentile for each ZIP code or county. Indices such as the Social Deprivation Index have been linked to adverse health outcomes.5,6 We assigned beneficiaries to Social Deprivation Index quintiles on the basis of their residential ZIP codes, with quintile 1 representing the least disadvantaged areas and quintile 5 the most.
To gain insight into MA enrollment trends, we first calculated the proportions of beneficiaries of a given race/ethnicity, with dual eligibility, or in a Social Deprivation Index group in the Medicare program who were in an MA plan each year. Next, among those enrolled in an MA plan, we compared enrollment in Special Needs Plans by race/ethnicity over time. In our primary analysis we did not conduct adjustments, as our goal was to provide information on overall trends for each type of enrollee. Finally, using data from 2018, the final year of our study period, we compared several contract characteristics across enrollee groups.We compared the percentages of MA enrollees in zero premium plans, in different types of Special Needs Plans, and in plans with various star ratings. For each enrollee type we also calculated Gini coefficients as a measure of how unequally distributed enrollees of a given type were across plans.We also compared differences using p90/p10 and p90/p50 ratios, which are often used to compare unequal distributions across groups. The p90/p10 is the ratio of the concentration of an enrollee type in plans at the ninetieth percentile of concentration to the tenth percentile, and the p90/p50 is the ratio of the ninetieth percentile to the fiftieth percentile, or median. To calculate these ratios, we first calculated, for each plan, the percentage of enrollees of a given type in that plan.We then measured the concentration at the ninetieth percentile and divided by the concentration at the tenth percentile and the fiftieth percentile.
We did not conduct any tests of statistical significance, to be able to present the universe of enrollment data.
Our study had several limitations. First, our analysis was cross-sectional and descriptive. We could not evaluate what might be driving the observed trends; however, gaining a sense of those trends is an important first step toward understanding the dynamics of program change over time. Second, the Research Triangle Institute race/ethnicity codes available in the Master Beneficiary Summary File might not perfectly capture an enrollee’s self-identified race/ethnicity; however, they are the only source of race/ethnicity information in the enrollment file, and the file has been used widely in prior research.3 Third, there is likely substantial overlap among enrollee race/ethnicity, dual enrollment, and neighborhood disadvantage. Our analysis did not account for this to avoid differentiating between factors based on possible importance in driving enrollment differences.
Study Results
Our study included 397,189,742 person-years from 82,626,490 Medicare beneficiaries during 2009–18.
In exhibit 1 we present trends in MA enrollment by race/ethnicity and dual enrollment status over time. In 2009, 23 percent of Black, 33 percent of Hispanic, and 18 percent of dual beneficiaries were in an MA plan compared with 38 percent, 48 percent, and 37 percent, respectively, in 2018. These amount to a 66 percent relative increase among Black beneficiaries, a 43 percent relative increase among Hispanic beneficiaries, and a 101 percent relative increase among dual enrollees compared with a 46 percent increase among White beneficiaries and a 43 percent increase among nondual enrollees.
In exhibit 2 we present trends in MA enrollment by beneficiary neighborhood disadvantage. We find that beneficiaries who live in neighborhoods in the higher quintiles of disadvantage were more likely to enroll in Medicare Advantage than those in lower quintiles of disadvantage. The largest growth in MA enrollment over time was among beneficiaries in the highest quintile of disadvantage, which saw enrollment increase from 25 percent to 40 percent—a 60 percent relative increase, compared with only a 42 percent relative increase among enrollees in neighborhoods in the lowest quintile.
EXHIBIT 2. Enrollment in Medicare Advantage (MA), by quintile of neighborhood disadvantage, 2009–18.
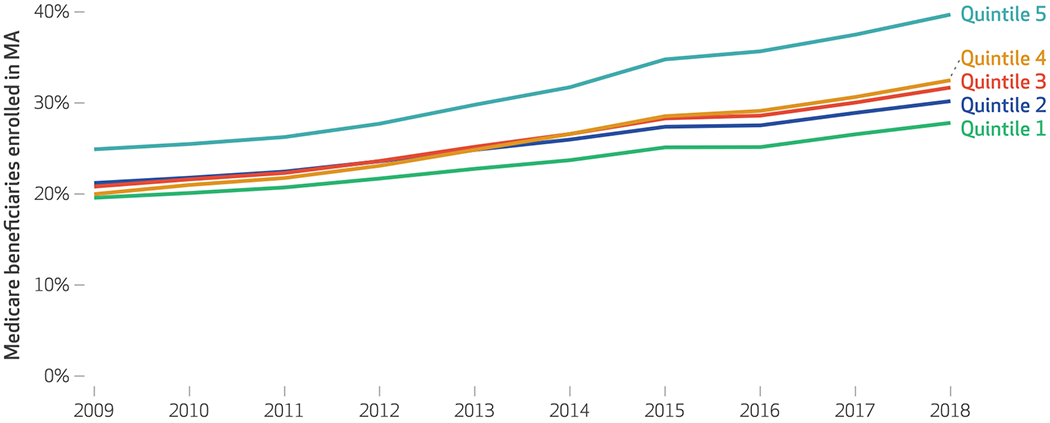
source Authors’ analysis of data from the Medicare Beneficiary Summary File, 2009–18. notes For each data point, the denominator is the number of all beneficiaries of that type in Medicare each year. The numerator is the number of those beneficiaries enrolled in an MA plan. Each beneficiary was assigned a Social Deprivation Index on the basis of their residence’s nine-digit ZIP code. The index was then classified into quintiles. Each line represents a quintile of social deprivation (quintile 1: Social Deprivation Index, 1–20; quintile 2: 21–40; quintile 3: 41–60; quintile 4: 61–80; quintile 5: 81–100). The average annual growth rate was 0.9 percent for the first quintile (representing the lowest level of deprivation) and 1.6 percent for the fifth quintile (representing the highest level of deprivation).
In exhibit 3 we present trends in Special Needs Plan enrollment among beneficiaries who were enrolled in an MA plan. Although enrollment in Special Needs Plans fluctuated across groups from 2009 to 2018, 43 percent and 55 percent of Hispanic and dual enrollees, respectively, enrolled in Special Needs Plans in 2018 compared with 10 percent of White enrollees.
EXHIBIT 3. Enrollment in Medicare Advantage (MA) Special Needs Plans (SNPs), by race/ethnicity and dual enrollment status, 2011–18.
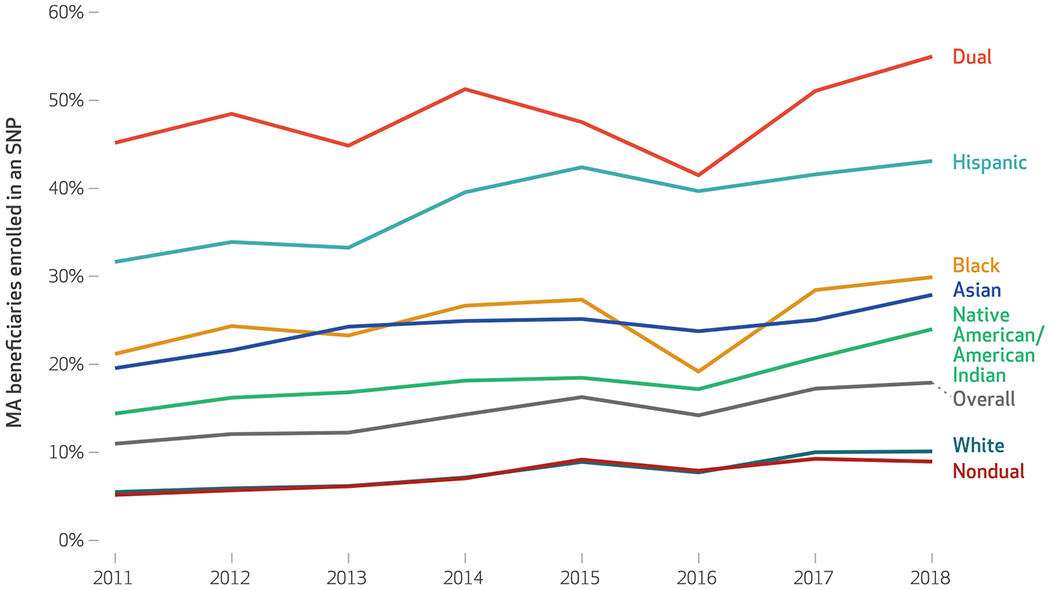
source Authors’ analysis of data from the Medicare Beneficiary Summary File and the Centers for Medicare and Medicaid Services Plan Characteristics Files, 2011–18. notes For each data point, the denominator is the number of all beneficiaries of that type in Medicare Advantage each year. The numerator is the number of those beneficiaries enrolled in any type of SNP “Dual” and “nondual” are defined in the notes to exhibit 1.
In exhibit 4, we compare differences in plan characteristics across groups in 2018. In a comparison of Gini coefficients, a coefficient of 0 would indicate that a group was equally distributed across plans, whereas a coefficient of 1 would indicate that all individuals of that type were concentrated in a single plan.We found that White enrollees were generally equally distributed across plans, with a Gini coefficient of 0.25, compared with more unequal distributions for Black (0.53) Hispanic (0.66), Asian (0.69), and Native American/American Indian (0.71) enrollees.
EXHIBIT 4.
Gini coefficients, inequality ratios, and Medicare Advantage (MA) plan characteristics, by enrollee type, 2018
| Race/ethnicity |
Dual enrollment statusa |
Level of disadvantageb |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Overall | Black | Hispanic | White | Asian | NA/AI | Dual | Nondual | High | Low | |
| Gini coefficientc | —d | 0.53 | 0.66 | 0.25 | 0.69 | 0.71 | 0.46 | 0.4 | 0.43 | 0.45 |
| Inequality ratiose | ||||||||||
| p90/p10 ratio | —d | 4.2 | 50.6 | 4.8 | 25.8 | 28 | 24.6 | 113.5 | 12.4 | 13.4 |
| p90/p50 ratio | —d | 0.5 | 9.6 | 1.4 | 6.6 | 5.4 | 3.0 | 1.3 | 2.7 | 2.8 |
| Type of SNP, % | ||||||||||
| Chronic disease | 2.7 | 3.8 | 6.2 | 1.8 | 1.8 | 2.0 | 2.8 | 2.6 | 3.2 | 1.0 |
| Dual | 14 | 25.1 | 36.0 | 6.9 | 24.7 | 21.0 | 50.1 | 5.3 | 25.2 | 4.7 |
| Institutional | 1.3 | 0.9 | 0.9 | 1.4 | 1.4 | 1.0 | 2.2 | 1.1 | 1.1 | 1.4 |
| Plan premium | ||||||||||
| Zero premium, % | 38.0 | 34.7 | 53.3 | 35.1 | 37.9 | 30.8 | 19.9 | 42.9 | 38.5 | 35.3 |
| Median monthly premium, $ | 25 | 20 | 0 | 29 | 25 | 25 | 25 | 20 | 20 | 30 |
| MA star rating,f % | ||||||||||
| Unrated | 9.4 | 9.8 | 12.5 | 7.8 | 21.0 | 9.6 | 15.2 | 7.8 | 12.9 | 6.7 |
| 2 or 2.5 | 0.5 | 1.4 | 0.5 | 0.3 | 0.8 | 0.3 | 1.1 | 1.1 | 0.8 | 0.4 |
| 3 or 3.5 | 25.0 | 33.5 | 27.2 | 22.1 | 36.0 | 36.6 | 38.7 | 38.7 | 34.6 | 19. |
| 4 or 4.5 | 62.2 | 54. 2 | 57.5 | 66.4 | 38.8 | 52.0 | 43.3 | 43.3 | 49.7 | 69.8 |
| 5 | 2.3 | 1.1 | 2.4 | 3.4 | 3.4 | 1.7 | 1.8 | 1.8 | 2.1 | 4.1 |
source Authors’ analysis of data from the Medicare Beneficiary Summary File and Centers for Medicare and Medicaid Services (CMS) Plan Characteristics File for 2018. notes Percentages are column percentages representing, for example, the percentage of all White MA beneficiaries included in a chronic disease Special Needs Plan (SNP). NA/AI is Native American/American Indian.
“Dual” and “nondual” are defined in the exhibit 1 notes.
High disadvantage refers to enrollees whose nine-digit ZIP code is in the highest quintile of deprivation, based on the Social Deprivation Index. Low disadvantage represents those in the lowest quintile.
Measure of inequality ranging from 0 (lowest inequality) to 1 (highest inequality). A coefficient of 0 would indicate that there is a completely equal distribution of a given group across plans, whereas a coefficient of 1 would indicate that all enrollees of a given group are enrolled in only a single plan.
Not applicable.
p90/p10 is the ratio of the concentration at the 90th percentile to the 10th percentile. p90/p50 is the ratio of the concentration at the 90th percentile to the 50th percentile (median).
Star ratings are reported by CMS in 0.5-star increments.
When we compared inequality ratios, we found that for Hispanic enrollees the p90/p10 was 50.6 and the p90/p50 was 9.6—that is, the concentration of Hispanic enrollees in plans at the ninetieth percentile of Hispanic concentration was 50.6 times the concentration at the tenth percentile, and the concentration at the ninetieth percentile was 9.6 times the concentration at the fiftieth percentile (median). We also found that the percentage of nondual enrollees in a plan at the ninetieth percentile was 113.5 times the concentration at the tenth percentile, indicating that dual and nondual enrollees may concentrate heavily in different plans. We found similarly large differences in the distribution of enrollees across other enrollee categories: The ratios were 4.2 and 0.5 for Black enrollees, 25.8 and 6.6 for Asian enrollees, 24.6 and 3.0 for dual enrollees, and 12.4 and 2.7 for the least disadvantaged enrollees.
Racial/ethnic minority enrollees had substantially higher rates of Special Needs Plan enrollment: Only 6.9 percent of White enrollees were in a dual Special Needs Plan compared with 25.1 percent of Black enrollees and 36.0 percent of Hispanic enrollees. Hispanic enrollees were most often enrolled in a zero-premium plan (53.3 percent of the time), and 69.8 percent of White beneficiaries were in plans rated with four or five stars compared with 55.3 percent of Black, 59.9 percent of Hispanic, 42.2 percent of Asian, and 53.7 percent of Native American/American Indian enrollees. Enrollees in the most disadvantaged areas were enrolled in four- or five-star plans 51.8 percent of the time, compared with 73.9 percent of enrollees in the least disadvantaged areas.
Discussion
Our analysis of trends in MA enrollment over time yielded four key findings. First, from 2009 to 2018 the largest increases in MA enrollment were concentrated among enrollees who were Black, were dual enrollees, and resided in areas with the highest level (that is, in the highest quintile) of neighborhood disadvantage. Second, enrollees from racial/ethnic minority groups appear to have been heavily concentrated in specific plans, whereas White enrollees were more broadly distributed. Third, Hispanic enrollees tended to select plans with lower premiums. Finally, enrollees from racial/ethnic minority groups, overall, tended to enroll in lower-quality plans.
Although prior work has studied MA enrollment trends using publicly reported data, our study built on this literature by including detailed person-level data during a longer period. This is also the first study to our knowledge to compare MA enrollment by enrollees’ neighborhood Social Deprivation Index.
Our findings describing high and growing enrollment of Black and Hispanic enrollees in Medicare Advantage have important implications for the future contours of the program. If current trends continue, the majority of Black, Hispanic, and dual enrollees will be in Medicare Advantage within the next five years (the majority of all beneficiaries are expected to be in Medicare Advantage within ten years).7 There is a growing body of literature indicating that marginalized MA enrollees may face substantial disparities in outcomes.8–11 Thus, MA plans may need to become a key partner in finding effective ways to address those disparities. Specifically, the fact that Black and Hispanic beneficiaries tended to be enrolled in lower-quality plans may need greater attention from policy makers. Although these trends may be in part a result of differences in the geographic availability of high-quality plans, that does not make them less concerning.
Although the present analysis avoided trying to identify causal relationships, it should be acknowledged that growing rates of MA enrollment among dual enrollees are likely multifactorial. In 2017 CMS increased the bonus to risk-adjusted payments that it paid to plans for taking care of dual enrollees.12 These payment incentives may continue to spur the development of dual Special Needs Plans and MA enrollment among dual enrollees moving forward. As beneficiaries from racial/ethnic minority groups are more often dually enrolled compared with White enrollees, this may contribute to their high enrollment in Special Needs Plans.
In the research and policy discourse, Medicare Advantage is often considered monolithic. Our findings suggest that a more nuanced interpretation is needed to understand the current program and its likely future state. The demographics of its service population changed substantially during the period 2009–18. As plan offerings have diversified, enrollees from racial/ethnic minority groups have become concentrated in a narrower set of plans, and it is unclear to what extent these plans may currently be addressing those enrollees’ needs and how these plans may differ from others offered in the program.
Acknowledgments
This work was funded by the National Institute on Aging. David Meyers was paid as an independent consultant by NORC. Vincent Mor is the chair of the Independent Quality Committee at HCR Manor Care and the chair of the Scientific Advisory Board and consultant for NaviHealth Inc., as well as a former director of PointRight Inc., where he holds less than 1 percent equity. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the National Institute on Aging, the Department of Veterans Affairs, or the US government.
Contributor Information
David J. Meyers, Department of Health Services, Policy, and Practice at the Brown University School of Public Health, in Providence, Rhode Island.
Vincent Mor, Florence Pirce Grant University Professor in the Department of Health Services, Policy, and Practice and the Center for Gerontology and Healthcare Research, Brown University School of Public Health, and a research health scientist at the Providence Veterans Affairs Medical Center, in Providence, Rhode Island.
Momotazur Rahman, Department of Health Services, Policy, and Practice at the Brown University School of Public Health.
Amal N. Trivedi, Department of Health Services, Policy, and Practice at the Brown University School of Public Health and a research health scientist at the Providence Veterans Affairs Medical Center.
NOTES
- 1.Neuman P, Jacobson GA. Medicare Advantage checkup. N Engl J Med. 2018;379(22):2163–72. [DOI] [PubMed] [Google Scholar]
- 2.Meyers DJ, Durfey SNM, Gadbois EA, Thomas KS. Early adoption of new supplemental benefits by Medicare Advantage plans. JAMA. 2019;321(22):2238–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eicheldinger C, Bonito A. More accurate racial and ethnic codes for Medicare administrative data. Health Care Financ Rev. 2008; 29(3):27–42. [PMC free article] [PubMed] [Google Scholar]
- 4.Robert Graham Center. Social Deprivation Index (SDI) [Internet]. Washington (DC): The Center; [cited 2021 Apr 14]. Available from: https://www.graham-center.org/rgc/maps-data-tools/sdi/social-deprivation-index.html [Google Scholar]
- 5.Butler DC, Petterson S, Phillips RL, Bazemore AW. Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health Serv Res. 2013;48(2 Pt 1):539–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kind AJH, Jencks S, Brock J, Yu M, Bartels C, Ehlenbach W, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med. 2014;161(11):765–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Congressional Budget Office. Medicare—CBO’s baseline as of March 6, 2020 [Internet]. Washington (DC): CBO; 2020. March 6 [cited 2021 Apr 21]. Available from: https://www.cbo.gov/system/files/2020-03/51302-2020-03-medicare.pdf [Google Scholar]
- 8.Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. Relationship between quality of care and racial disparities in Medicare health plans. JAMA. 2006;296(16):1998–2004. [DOI] [PubMed] [Google Scholar]
- 9.Weech-Maldonado R, Elliott MN, Adams JL, Haviland AM, Klein DJ, Hambarsoomian K, et al. Do racial/ethnic disparities in quality and patient experience within Medicare plans generalize across measures and racial/ethnic groups? Health Serv Res. 2015;50(6):1829–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li Y, Cen X, Cai X, Thirukumaran CP, Zhou J, Glance LG. Medicare Advantage associated with more racial disparity than traditional Medicare for hospital readmissions. Health Aff (Millwood). 2017;36(7):1328–35. [DOI] [PubMed] [Google Scholar]
- 11.Rivera-Hernandez M, Leyva B, Keohane LM, Trivedi AN. Quality of care for White and Hispanic Medicare Advantage enrollees in the United States and Puerto Rico. JAMA Intern Med. 2016;176(6):787–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Keohane LM, Stevenson DG, Stewart L, Thapa S, Freed S, Buntin MB. Risk adjusting for Medicaid participation in Medicare Advantage. Am J Manag Care. 2020;26(8):e258–63. [DOI] [PMC free article] [PubMed] [Google Scholar]


