Abstract
Background
Previously treated (ie, recurrent) tuberculosis (TB) cases account for approximately 7%–8% of incident TB globally and in Singapore. Molecular fingerprinting has enabled the differentiation of these patients into relapsed or reinfection cases.
Methods
Patient demographics, disease characteristics, and treatment information were obtained from the national TB notification registry and TB Control Unit. We performed a retrospective, case-control study to evaluate factors associated with recurrent TB disease in Singapore citizens and permanent residents with culture-positive TB from 2006 to 2013 and who developed a second episode of culture-positive TB up to 2016 using multivariable logistic regression analyses.
Results
Ninety-one cases with culture-positive first and recurrent TB disease episodes were identified. Recurrent TB was associated with age ≥60 years (adjusted odds ratio [aOR], 1.98 [95% confidence interval {CI}, 1.09–3.61), male sex (aOR, 2.29 [95% CI, 1.22–4.51]), having concomitant pulmonary and extrapulmonary TB (aOR, 3.10 [95% CI, 1.59–6.10]) and extrapulmonary TB alone (aOR, 3.82 [95% CI, 1.12–13.31]), and was less likely in non-Malays (aOR, 0.52 [95% CI, .27–.99]). DNA fingerprinting results for both episodes in 49 cases differentiated these into 28 relapsed and 21 reinfection cases. Relapse was associated with having concomitant pulmonary and extrapulmonary TB (aOR, 9.24 [95% CI, 2.50–42.42]) and positive sputum acid-fast bacilli smear (aOR, 3.95 [95% CI, 1.36–13.10]).
Conclusions
Relapse and reinfection contributed to 57% and 43%, respectively, of recurrent TB in Singapore. Our study highlights the underappreciated association of concomitant pulmonary and extrapulmonary TB as a significant risk factor for disease relapse.
Keywords: exogenous reinfection, extrapulmonary, tuberculosis, relapse
Relapse and reinfection contributed to 57% and 43%, respectively, of recurrent tuberculosis (TB) cases in Singapore, a densely populated country with intermediate TB incidence. Positive sputum smear and concomitant pulmonary and extrapulmonary TB disease were significantly associated with risk of relapse.
Persons with previously treated tuberculosis (TB) account for approximately 7% of incident TB cases globally [1]. Recurrence of TB disease after clinical cure/treatment completion of a previous episode may be due to endogenous reactivation of residual tuberculous bacilli from the original episode (referred to as relapse) or exogenous reinfection. Over the past 2 decades, molecular genotyping techniques have enabled the study of the diversity of Mycobacterium tuberculosis strains and have demonstrated that exogenous reinfection plays a more important role in causing recurrent disease than previously thought [2]. It is likely that reinfection drives the TB epidemic in areas with high TB and human immunodeficiency virus (HIV) prevalence. Nonetheless, there does not appear to be a consistent correlation in the literature between the predominant cause of recurrent TB (ie. relapse vs reinfection) and geographical TB prevalence [3–8].
Singapore is a densely populated island city-state with an intermediate TB incidence of 35–40 cases per 100 000 population and a very low HIV/AIDS notification rate of 7.9 per 100 000 population in 2018 [9]. There are approximately 3000 notified TB cases in the country annually, of whom approximately 50% are Singapore citizens or permanent residents. Among these, persons with a history of previously treated TB account for approximately 8% of notified TB episodes [9]. We undertook a retrospective case-control study to investigate the characteristics of Singapore citizens and permanent residents with recurrent culture-positive TB (“recurrent TB”). The availability of DNA fingerprinting results provided the opportunity to examine factors associated with recurrent disease due to relapse or exogenous reinfection.
METHODS
Tuberculosis disease is notifiable by law in Singapore. The national TB notification registry is also electronically linked to the 2 mycobacterial culture laboratories in Singapore, enabling complete capture of all positive Mycobacterium tuberculosis complex (MTC) culture results. Singapore citizens and permanent residents 16 years and older with a first episode of culture-positive TB notified between 1 January 2006 and 31 December 2013 and who developed a second episode of culture-positive TB in the period up to 31 December 2016 were identified from the national TB notification registry. For this study, “recurrent TB” was defined as a second episode of culture-positive TB disease occurring in persons who had completed treatment of a first episode of culture-positive TB.
Data analyzed in this study pertained to the first disease episode and included age, sex, ethnic group, and presence of diabetes mellitus (DM) and HIV coinfection, sputum acid-fast bacilli (AFB) smear status, site(s) of disease (pulmonary TB [PTB] with or without concomitant extrapulmonary disease), presence of cavitation on baseline chest radiograph (CXR), treatment regimen, mode of treatment delivery (whether directly observed therapy [DOT] or self-administered therapy), AFB culture results at 2 months of treatment, and whether the duration of short-course TB therapy was extended beyond the conventional 6 months. This information was obtained from clinical case records for patients who were treated at the TB Control Unit (70% of patients in this study) during the first episode of TB; otherwise, the information was extracted from the TB registry for patients treated in other institutions.
For the case-control study, cases were defined as patients with recurrent TB. Controls were culture-positive patients who were not notified with recurrent TB within the period of the study. Two controls were randomly selected for each study case, matched by date of notification (± 5 days). For subgroup analyses, cases with available 24-loci mycobacterial interspersed repetitive unit variable number tandem repeat (MIRU-VNTR) and spacer oligonucleotide (spoligotyping) results for both TB episodes were classified into those with identical/near-identical DNA fingerprinting results (“relapse cases”) or different results (“reinfection cases”) for both episodes.
Statistical Analysis
The χ 2 test or Fisher exact test, where appropriate, was used to compare baseline characteristics between individuals with and without recurrent TB. No imputation was carried out for missing data. We inserted an “unknown” category for variables with missing data. The main outcome was whether an individual had recurrent TB. Crude and adjusted odds ratios (ORs) were calculated using Firth logistic regression analyses. Variables for the multivariable logistic regression model were selected through stepwise use of Akaike information criterion. All P values reported were 2-sided and statistical significance was taken as P < .05. Statistical analyses were performed using SPSS version 24 (IBM Corporation, Armonk, New York) and R version 3.6.2 (R Foundation for Statistical Computing, Vienna, Austria).
Ethics Approval
Ethics approval was obtained from the National Healthcare Group Domain Specific Review Board (study reference number 2015/01122). Personal identifiers were removed prior to data analysis.
RESULTS
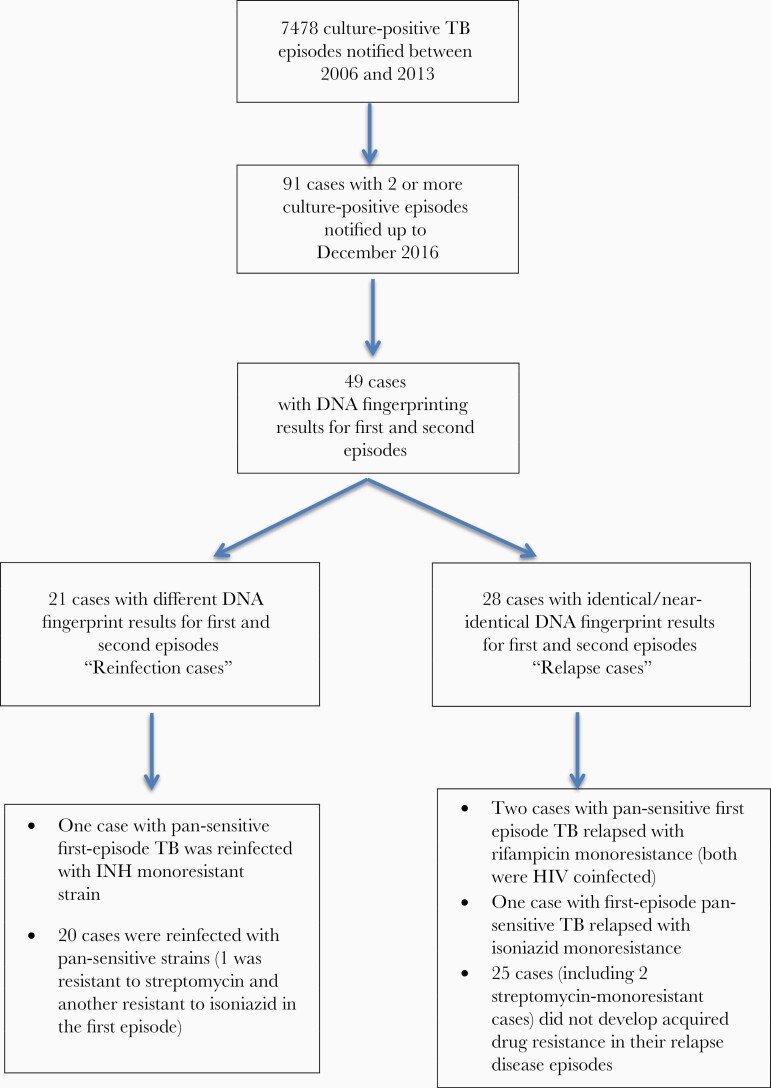
There were 7478 culture-positive TB case episodes notified between 1 January 2006 and 31 December 2013. Of these, 91 (1.2%) cases had 2 or more culture-positive TB episodes as of 31 December 2016 (Figure 1).
Figure 1.
There were 7478 culture-positive tuberculosis (TB) cases notified from 1 January 2006 to 31 December 2013. Of these, 91 had 2 or more culture-positive TB episodes as of 31 December 2016. Mycobacterial interspersed repetitive unit variable number tandem repeat and spoligotyping results were available for both TB disease episodes in 49 of the 91 (53.8%) cases. Twenty-four cases had identical results and 4 had results that differed by 1 or 2 loci (relapse cases). Twenty-one cases had different DNA fingerprint results for the first and recurrent episodes (reinfection cases). Abbreviations: HIV, human immunodeficiency virus; INH, isoniazid; TB, tuberculosis.
The median time to disease recurrence was 24 months (1.5–110 months). Among the 91 cases with recurrent TB, the median age was 53.02 years, 74 (81.3%) were male, 23 (25.3%) were of Malay ethnicity, 32 (35.2%) had DM, and 7 (7.7%) had HIV coinfection at the time of their first disease episode. Eighty-five (93.4%) had PTB in their first TB episode; among these, 24 (26.4%) had concomitant extrapulmonary site disease. Six (6.6%) had extrapulmonary disease only (2 pleura, 3 lymphatic, 1 gastrointestinal). Forty-one (45.1%) patients had cavitary disease, and 60 (65.9%) were sputum AFB smear positive. Fifty-five (60.4%) were treated under DOT. At 2 months (end of intensive phase) of treatment, 52 (57%) cases were sputum culture negative, 4 (4.4%) were sputum culture positive, and 35 (38.5%) had unknown sputum culture status. Eleven (12.1%) had extension of their continuation phase of treatment.
Recurrent TB was significantly associated with age ≥60 years (adjusted OR [aOR], 1.98 [95% confidence interval {CI}, 1.09–3.61]), male sex (aOR, 2.29 [95% CI, 1.22–4.51]), having concomitant pulmonary and extrapulmonary TB (aOR, 3.10 [95% CI, 1.59–6.10]), and extrapulmonary TB alone (aOR, 3.82 [95% CI, 1.12–13.31]) and was less likely to occur in persons of non-Malay ethnicity (aOR, 0.52 [95% CI, .27–.99]) (Table 1).
Table 1.
Odds Ratios of Candidate Predictors for Recurrent Tuberculosis
| Univariable Model | Multivariable Modela | |||||
|---|---|---|---|---|---|---|
| Characteristic | Cases (n = 91), No. (%) |
Controls (n = 182), No. (%) |
OR (95% CI) | P Value | aOR (95% CI) | P Value |
| Age group | ||||||
| <60 y | 61 (67.0) | 145 (79.7) | 1.00 (reference) | 1.00 (reference) | ||
| ≥60 y | 30 (33.0) | 37 (20.3) | 1.92 (1.09–3.38) | .024 | 1.98 (1.09–3.61) | .026 |
| Sex | ||||||
| Female | 17 (18.7) | 61 (33.5) | 1.00 (reference) | 1.00 (reference) | ||
| Male | 74 (81.3) | 121 (66.5) | 2.15 (1.20–4.03) | .010 | 2.29 (1.22–4.51) | .009 |
| Ethnic group | ||||||
| Malay | 23 (25.3) | 33 (18.1) | 1.00 (reference) | 1.00 (reference) | ||
| Non-Malay | 68 (74.7) | 149 (81.9) | 0.65 (.36–1.20) | .167 | 0.52 (.27–.99) | .047 |
| Diabetes mellitus | ||||||
| No | 59 (64.8) | 131 (72.0) | 1.00 (reference) | … | ||
| Yes | 32 (35.2) | 51 (28.0) | 1.39 (.81–2.38) | .225 | … | |
| HIV infection | ||||||
| No | 84 (92.3) | 171 (94.0) | 1.00 (reference) | 1 | ||
| Yes | 7 (7.7) | 11 (6.0) | 1.32 (.49–3.40) | .569 | … | |
| TB site | ||||||
| PTB | 61 (67.0) | 154 (84.6) | 1.00 (reference) | 1.00 (reference) | ||
| PTB with extrapulmonary TB | 24 (26.4) | 22 (12.1) | 2.74 (1.44–5.24) | .002 | 3.10 (1.59–6.10) | .001 |
| Extrapulmonary TB | 6 (6.6) | 6 (3.3) | 2.51 (.79–7.95) | .011 | 3.82 (1.12–13.31) | .033 |
| Cavitation present in baseline CXR | ||||||
| No | 50 (54.9) | 120 (65.9) | 1.00 (reference) | 1.00 (reference) | ||
| Yes | 41 (45.1) | 62 (34.1) | 1.58 (.95–2.65) | .078 | 1.63 (.94–2.84) | .081 |
| Sputum AFB smear | ||||||
| Negative | 31 (34.1) | 82 (45.1) | 1.00 (reference) | … | ||
| Positive | 60 (65.9) | 98 (53.8) | 1.61 (.96–2.73) | .07 | … | |
| Not done | 0 (0.0) | 2 (1.1) | 0.52 (.004–6.67) | .66 | … | |
| Sputum culture conversion at 2 mo of treatment | ||||||
| No | 4 (4.4) | 7 (3.8) | 1.00 (reference) | … | ||
| Yes | 52 (57.1) | 120 (65.9) | 0.73 (.22–2.66) | .610 | … | |
| Unknown | 35 (38.5) | 55 (30.2) | 1.07 (.31–4.01) | .919 | … | |
| Treatment delivery mode | ||||||
| SAT | 36 (39.6) | 64 (35.2) | 1.00 (reference) | … | ||
| DOT | 55 (60.4) | 118 (64.8) | 0.83 (.49–1.39) | .473 | … | |
| Extension of continuation phase of treatment | ||||||
| No | 71 (78.0) | 140 (76.9) | 1.00 (reference) | … | ||
| Yes | 11 (12.1) | 26 (14.3) | 0.85 (.39–1.77) | .674 | … | |
| Unknown | 9 (9.9) | 16 (8.8) | 1.13 (.47–2.60) | .776 | … | |
Abbreviations: AFB, acid-fast bacilli; aOR, adjusted odds ratio; CI, confidence interval; CXR, chest radiograph; DOT, directly observed therapy; HIV, human immunodeficiency virus; OR, odds ratio; PTB, pulmonary tuberculosis; SAT, self-administered therapy; TB, tuberculosis.
aAdjusted for age group, gender, ethnic group, TB site, and whether cavitation was present in baseline CXR.
Subgroup Analysis According to Relapse or Reinfection
MIRU-VNTR and spoligotyping results were available for both TB disease episodes in 49 of the 91 (53.8%) cases with recurrent TB. There was no significant difference in age, sex, ethnicity, presence of DM or HIV, sputum AFB smear, presence of cavity, disease site (PTB with or without concomitant extrapulmonary disease), sputum AFB culture status at 2 months of treatment, treatment delivery mode, or duration of treatment between the cases with and without available DNA fingerprinting results for both TB episodes (Supplementary Table 1). Of the 49 cases with available genotyping, 24 had identical results and 4 had results that differed by 1 or 2 loci for the first and recurrent disease episodes—these 28 cases were classified as “relapse cases.” Twenty-one cases with different MIRU-VNTR results for the first and recurrent episodes were classified as “reinfection” cases (Figure 1).
There was no significant difference in age, sex, ethnicity, and proportion infected with the Beijing strain between the relapse and reinfection groups. The median time to disease recurrence was significantly shorter in those who relapsed (22 months [range, 2–68]) compared with those who were reinfected (49 months [range, 4–110]) (P = .003; Table 2).
Table 2.
Comparison Between Characteristics of Relapse and Reinfection Cases
| Variable | Relapse Cases (n = 28) | Reinfection Cases (n = 21) | P Valuea |
|---|---|---|---|
| Age group, No. (%) | |||
| 60 y | 20 (71.4) | 15 (71.4) | 1.000 |
| ≥60 y | 8 (28.6) | 6 (28.6) | |
| Sex, No. (%) | |||
| Female | 7 (25) | 5 (23.8) | 1.000 |
| Male | 21 (75) | 16 (76.2) | |
| Ethnic group, No. (%) | |||
| Malay | 11 (39.3) | 5 (23.8) | .359 |
| Non-Malay | 17 (60.7) | 16 (76.2) | |
| Median time to disease recurrence, mo | 22.0 | 49.00 | .003 |
| Infecting strain, No. (%) | |||
| Beijing | 18 (64.3) | 13 (61.9) | 1.000 |
| Non-Beijing | 10 (35.7) | 8 (38.1) |
a P values comparing relapse and reinfection cases are from Fisher exact test for categorical variables and Mann-Whitney U test for the continuous variable.
Relapse Cases
Relapse cases were more likely to have PTB and concomitant extrapulmonary disease (aOR, 9.24 [95% CI, 2.50–42.42]) and to be sputum AFB smear positive (aOR, 3.59 [95% CI, 1.36–13.10]) (Table 3). Relapse was not associated with age, sex, ethnicity, DM, HIV coinfection, having extrapulmonary TB alone, cavitation on baseline CXR, sputum AFB culture status at 2 months of treatment, mode of treatment delivery, or duration of TB treatment.
Table 3.
Odds Ratios of Candidate Predictors for Relapsed Cases
| Univariable Model | Multivariable Modela | |||||
|---|---|---|---|---|---|---|
| Characteristic | Cases (n = 28), No. (%) | Controls (n = 56), No. (%) | OR (95% CI) | P Value | aOR (95% CI) | P Value |
| Age group | ||||||
| <60 y | 20 (71.4) | 45 (80.4) | 1.00 (reference) | … | ||
| ≥60 y | 8 (28.6) | 11 (19.6) | 1.64 (.57–4.59) | .349 | … | |
| Sex | ||||||
| Female | 7 (25.0) | 16 (28.6) | 1.00 (reference) | … | ||
| Male | 21 (75.0) | 40 (71.4) | 1.17 (.43–3.34) | .762 | … | |
| Ethnic group | ||||||
| Malay | 11 (39.3) | 14 (25.0) | 1.00 (reference) | 1.00 (reference) | ||
| Non-Malay | 17 (60.7) | 42 (75.0) | 0.52 (.20–1.36) | .179 | 0.38 (.12–1.18) | .094 |
| Diabetes mellitus | ||||||
| No | 22 (78.6) | 40 (71.4) | 1.00 (reference) | 1.00 (reference) | ||
| Yes | 6 (21.4) | 16 (28.6) | 0.71 (.24–1.95) | .513 | 0.34 (.09–1.16) | .086 |
| HIV infection | ||||||
| No | 25 (89.3) | 52 (92.9) | 1.00 (reference) | … | ||
| Yes | 3 (10.7) | 4 (7.1) | 1.60 (.34–7.09) | .536 | … | |
| TB site | ||||||
| PTB | 16 (57.1) | 49 (87.5) | 1.00 (reference) | 1.00 (reference) | ||
| PTB with extrapulmonary TB | 10 (35.7) | 5 (8.9) | 5.73 (1.83–19.79) | .003 | 9.24 (2.50–42.42) | .001 |
| Extrapulmonary TB | 2 (7.1) | 2 (3.6) | 3.00 (.43–20.92) | .250 | 3.93 (.50–32.76) | .183 |
| Cavitation present in baseline CXR | ||||||
| No | 15 (53.6) | 41 (73.2) | 1.00 (reference) | … | ||
| Yes | 13 (46.4) | 15 (26.8) | 2.33 (.92–6.01) | .075 | … | |
| Sputum AFB smear | ||||||
| Negative | 9 (32.1) | 31 (55.4) | 1.00 (reference) | 1.00 (reference) | ||
| Positive | 19 (67.9) | 24 (42.9) | 2.64 (1.05–6.97) | .038 | 3.95 (1.36–13.10) | .011 |
| Not done | 0 (0.0) | 1 (1.8) | 1.11 (.01–22.57) | .953 | 0.90 (.01–21.61) | .953 |
| Sputum culture conversion at 2 mo of treatment | ||||||
| No | 2 (7.1) | 1 (1.8) | 1.00 (reference) | … | ||
| Yes | 16 (57.1) | 37 (66.1) | 0.26 (.02–2.14) | .206 | … | |
| Unknown | 10 (35.7) | 18 (32.1) | 0.34 (.03–2.91) | .319 | … | |
| Treatment delivery mode | ||||||
| SAT | 11 (39.3) | 20 (35.7) | 1.00 (reference) | … | ||
| DOT | 17 (60.7) | 36 (64.3) | 0.85 (.34–2.17) | .738 | … | |
| Extension of continuation phase of treatment | ||||||
| No | 23 (82.1) | 42 (75.0) | 1.00 (reference) | … | ||
| Yes | 2 (7.1) | 6 (10.7) | 0.70 (.12–2.99) | .638 | … | |
| Unknown | 3 (10.7) | 8 (14.3) | 0.74 (.17–2.69) | .663 | … | |
Abbreviations: AFB, acid-fast bacilli; aOR, adjusted odds ratio; CI, confidence interval; CXR, chest radiograph; DOT, directly observed therapy; HIV, human immunodeficiency virus; OR, odds ratio; PTB, pulmonary tuberculosis; SAT, self-administered therapy; TB, tuberculosis.
aAdjusted for ethnic group, diabetes, TB site, and smear result.
Reinfection Cases
There was no statistically significant difference between reinfection cases and controls in terms of age, sex, ethnicity, presence of DM or HIV, concomitant PTB and extrapulmonary disease, extrapulmonary disease alone, bacteriological burden (smear and cavitary status), sputum AFB culture status at 2 months of treatment, mode of treatment delivery, or duration of TB treatment (Table 4).
Table 4.
Odds Ratios of Candidate Predictors for Reinfection Cases
| Univariable Model | Multivariable Modela | |||||
|---|---|---|---|---|---|---|
| Characteristic | Cases (n = 21), No. (%) |
Controls (n = 42), No. (%) | OR (95% CI) | P Value | aOR (95% CI) | P Value |
| Age group | ||||||
| <60 y | 15 (71.4) | 35 (83.3) | 1.00 (reference) | … | ||
| ≥60 y | 6 (28.6) | 7 (16.7) | 1.98 (.58–6.72) | .269 | … | |
| Sex | ||||||
| Female | 5 (23.8) | 19 (45.2) | 1.00 (reference) | 1.00 (reference) | ||
| Male | 16 (76.2) | 23 (54.8) | 2.49 (.83–8.34) | .105 | 2.48 (.82–8.39) | .109 |
| Ethnic group | ||||||
| Malay | 5 (23.8) | 7 (16.7) | 1.00 (reference) | … | ||
| Non-Malay | 16 (76.2) | 35 (83.3) | 0.63 (.18–2.30) | .477 | … | |
| Diabetes mellitus | ||||||
| No | 11 (52.4) | 30 (71.4) | 1.00 (reference) | 1.00 (reference) | ||
| Yes | 10 (47.6) | 12 (28.6) | 2.23 (.77–6.56) | .140 | 2.22 (.76–6.68) | .146 |
| HIV infection | ||||||
| No | 18 (85.7) | 37 (88.1) | 1.00 (reference) | … | ||
| Yes | 3 (14.3) | 5 (11.9) | 1.29 (.27–5.42) | .733 | … | |
| TB site | ||||||
| PTB | 15 (71.4) | 36 (85.7) | 1.00 (reference) | … | ||
| PTB with extrapulmonary TB | 5 (23.8) | 4 (9.5) | 2.88 (.72–12.12) | .133 | … | |
| Extrapulmonary TB | 1 (4.8) | 2 (4.8) | 1.41 (.12–11.53) | .751 | … | |
| Cavitation present in baseline CXR | ||||||
| No | 15 (71.4) | 26 (61.9) | 1.00 (reference) | … | ||
| Yes | 6 (28.6) | 16 (38.1) | 0.67 (.21–1.98) | .478 | … | |
| Sputum AFB smear | ||||||
| Negative | 9 (42.9) | 16 (38.1) | 1.00 (reference) | … | ||
| Positive | 12 (57.1) | 25 (59.5) | 0.85 (.30–2.46) | .763 | … | |
| Not done | 0 (0.0) | 1 (2.4) | 0.58 (.00–12.02) | .736 | … | |
| Sputum culture conversion at 2 mo of treatment | ||||||
| No | 1 (4.8) | 1 (2.4) | 1.00 (reference) | … | ||
| Yes | 12 (57.1) | 25 (59.5) | 0.49 (.04–6.50) | .557 | … | |
| Unknown | 8 (38.1) | 16 (38.1) | 0.52 (.04–7.08) | .592 | … | |
| Treatment delivery mode | ||||||
| SAT | 7 (33.3) | 19 (45.2) | 1.00 (reference) | … | ||
| DOT | 14 (66.7) | 23 (54.8) | 1.60 (.56–4.84) | .381 | … | |
| Extension of continuation phase of treatment | ||||||
| No | 16 (76.2) | 32 (76.2) | 1.00 (reference) | … | ||
| Yes | 4 (19.0) | 6 (14.3) | 1.36 (.34–5.18) | .652 | … | |
| Unknown | 1 (4.8) | 4 (9.5) | 0.66 (.06–3.94) | .663 | … | |
Abbreviations: AFB, acid-fast bacilli; aOR, adjusted odds ratio; CI, confidence interval; CXR, chest radiograph; DOT, directly observed therapy; HIV, human immunodeficiency virus; OR, odds ratio; PTB, pulmonary tuberculosis; SAT, self-administered therapy; TB, tuberculosis.
aAdjusted for gender and diabetes.
Cases With PTB and Concomitant Extrapulmonary TB Disease in the First Episode
Twenty-four patients with recurrent TB disease had PTB and concomitant extrapulmonary TB disease in their first disease episode. A variety of extrapulmonary sites were involved, the most common being the pleura (n = 14), followed by lymph node (n = 4), skeletal (n = 3), gastrointestinal (n = 2), larynx (n = 2), genitourinary (n = 2), and central nervous system (CNS) (n = 1). Four patients had 2 sites of extrapulmonary disease (Table 5). All but 1 of the 24 cases were sputum culture-positive in their first disease episode. Of these, all but 1 had pan-sensitive MTC grown in their sputum. Those with CNS or skeletal TB received treatment of appropriate duration. The majority (67%) had recurrent disease confined to the lungs. Fifteen cases had available DNA fingerprinting results for both episodes; of these, 10 were relapse cases (3 were HIV coinfected, 1 of whom relapsed with rifampicin-resistant disease); 5 were reinfection cases (1 was HIV coinfected, who had isoniazid resistance in the first disease episode and was reinfected with a pan-sensitive strain).
Table 5.
Sites of Disease in 24 Cases With Pulmonary Tuberculosis (TB) and Concomitant Extrapulmonary TB in Their First TB Episode
| Sites of Disease (First Episode) |
Duration of Treatment of First Episode, mo/Mode of Treatment Delivery | Sites of Disease (Recurrent Episode) |
Remarks | |
|---|---|---|---|---|
| Relapsed cases (ie, matching DNA fingerprints for both disease episodes), n = 10 | ||||
| 1 | PTB + pleura | 9/DOT | PTB | |
| 2 | PTB + pleura | 15/SAT with non-rifampicin-containing regimen | PTB | |
| 3 | PTB + larynx | 6/DOT | PTB | |
| 4 | PTB + pleura | 6/DOT | PTB + GI | |
| 5 | PTB + larynx | 6/DOT | PTB | |
| 6 | PTB + GI | 8.5/SAT | PTB | |
| 7 | PTB + pleura + LN | 6/DOT | PTB | |
| 8 | PTB + skeletal | 16/SAT | PTB + LN (rifampicin-resistant) | HIV-infected |
| 9 | PTB + LN + GU | 6/DOT | CNS | HIV-infected |
| 10 | PTB + CNS | 12/SAT | PTB + LN + CNS | HIV-infected |
| Reinfection cases (ie, different DNA fingerprints for both disease episodes), n = 5 | ||||
| 1 | PTB + pleura | 12/SAT | PTB | |
| 2 | PTB + pleura + LN | 6/DOT | PTB | |
| 3 | PTB + pleura | 6/DOT | PTB | |
| 4 | PTB + pleura | 6/DOT | PTB | |
| 5 | PTB + pleura + LN (isoniazid-resistant) | 9/DOT | PTB (pan-sensitive) | HIV-infected |
| Cases without DNA fingerprint results for both disease episodes, n = 9 | ||||
| 1 | PTB + pleura | 6/DOT | PTB | |
| 2 | PTB + GU | 10/DOT | PTB | |
| 3 | PTB + pleura | 18/DOT with non-rifampicin-containing regimen | PTB + eye | |
| 4 | PTB + skeletal | 9/DOT in institutional setting | PTB + GI | |
| 5 | PTB + skeletal | 10/SAT | Skeletal | |
| 6 | PTB + GI | 12/SAT | PTB | |
| 7 | PTB + pleura | 6/DOT | PTB | |
| 8 | PTB + pleura | 7/DOT | PTB | |
| 9 | PTB + pleura | 9/SAT | Pleura |
Abbreviations: CNS, central nervous system; DOT, directly observed therapy; GI, gastrointestinal; GU, genitourinary; LN, lymph node; PTB, pulmonary tuberculosis; SAT, self-administered therapy.
Acquisition of Drug Resistance
None of the 91 patients with recurrent TB had multidrug-resistant TB (ie, strains resistant to at least rifampicin and isoniazid) in their first or recurrent disease episodes. Six cases had new drug-resistant recurrent episodes, of whom 4 had available MIRU and spoligotyping results for both disease episodes (Figure 1). All 6 cases had pan-sensitive TB in their first episode: 2 HIV-coinfected patients relapsed with rifampicin-monoresistant TB, 1 patient relapsed with isoniazid-resistant TB, and 1 patient was reinfected with an isoniazid-resistant strain, whereas the remaining 2 patients with isoniazid-monoresistant recurrent TB disease (1 of whom was HIV coinfected) did not have available DNA fingerprinting results for both episodes. Three cases had streptomycin-monoresistant TB for both first and recurrent episodes—2 were relapse cases, while the third case had no available DNA fingerprinting result.
All 3 patients who relapsed with acquired drug resistance did not receive DOT and were not treated under the national TB program for their first TB episode.
DISCUSSION
Our case-control analysis showed age ≥60 years, male sex, Malay ethnicity, PTB with concomitant extrapulmonary TB, and extrapulmonary TB alone in the first disease episode to be significantly associated with recurrent TB disease. This information is useful to raise awareness as to the local epidemiological risk groups for TB disease recurrence (whether due to relapse or reinfection). Consistent with the TB literature, recurrent disease due to relapse occurred significantly earlier than that from exogenous reinfection. The odds of disease relapse were significantly higher in persons with PTB and concomitant extrapulmonary disease, and with sputum AFB smear positivity in the first episode. Our study did not identify any factors associated with exogenous reinfection.
A key objective of TB treatment is to eradicate populations of persisting bacilli to achieve durable cure (ie. to prevent relapse). The risk of relapse arises when there is suboptimal bacteriologic response to treatment of the first episode—this may be due to high bacteriological burden, or treatment factors such as inappropriate regimens, poor adherence, or drug pharmacokinetic/pharmacodynamic factors affecting therapeutic drug levels in individual patients. Indicators of disease burden such as cavitation/extensive disease on CXR and slower response to treatment as indicated by lack of sputum culture conversion at 2 months of treatment, presence of cavity on end-of-treatment chest radiograph, and lack of weight gain during the intensive phase of treatment have been well shown to be associated with risk of relapse [10–15]. Our finding that baseline sputum AFB smear positivity was significantly associated with relapse is not unexpected as this is an indicator of high initial disease burden. The association of concomitant extrapulmonary TB and PTB with risk of relapse was reported by a study in Hong Kong in 2004 (Chang et al [16]). Their study, however, did not have the benefit of genotyping to distinguish between true relapse and exogenous reinfection cases. The predominant extrapulmonary site in their patients was the lymph node (mainly cervical), followed by the pleura. All 12 of their patients with coexisting lymph node TB relapsed with lymph node disease (2 with concomitant PTB in their relapse episode). Only 9 of their 22 cases with concomitant extrapulmonary and PTB had positive sputum cultures. Our finding of a significant association of concomitant extrapulmonary TB and PTB with relapse highlights this previously underappreciated risk group for relapse. Of note, the extrapulmonary disease sites in our patients were wide-ranging. As persons with multisite TB disease presumably have higher bacterial burden, this association is biologically plausible. Interestingly, unlike the experience of Chang et al, the majority (67%) of our patients relapsed with pulmonary TB only.
Current international guidelines recommend extending the continuation phase of the standard 6-month short-course therapy by 3 months (ie, a total of 9 months of treatment) in persons with cavitation on their baseline CXR who have positive cultures at 2 months of treatment [17]. Other factors to consider in the decision to prolong treatment in patients with either baseline CXR cavitation or positive culture at 2 months (but not both) are being >10% below ideal body weight, being an active smoker, having DM, HIV coinfection or any other immunosuppressing condition, or having extensive disease on CXR [17]. Pertaining to extrapulmonary disease, these guidelines recommend extension of treatment duration only for CNS and skeletal TB. That our study found no association of relapse risk with cavitation on baseline CXR or sputum AFB culture at 2 months of treatment may have been influenced by the practice in the TB Control Unit of routinely extending the treatment continuation phase for persons with these factors. Our finding that persons with concomitant PTB and extrapulmonary disease involving a variety of extrapulmonary sites are at risk of relapse may suggest the need for extending treatment in these patients, regardless of the site of extrapulmonary disease.
DNA fingerprinting has shed light on the relative contribution of relapse (57%) vs reinfection (43%) to the burden of recurrent TB in Singapore. The risk of exogenous reinfection is influenced by the prevalence and transmission of TB in the community and host immunological factors. That exogenous reinfection accounted for almost half of the recurrent TB cases may not be surprising as Singapore is a densely populated, intermediate-TB-incidence (albeit low-HIV-incidence) country. The rate of relapsed culture-positive TB in Singapore was reassuringly low during the study period. We believe that this is testimony to the effectiveness of the Singapore TB Elimination Programme (STEP), which has, since 1998, utilized in-person DOT (daily during the intensive phase and thrice weekly in the continuation phase) at the patients’ nearest public health care clinic for the majority of the country’s TB cases [18, 19]. The STEP Treatment Surveillance Module, which actively tracks all TB cases in Singapore until their final outcome, has also served to ensure high treatment completion rates nationally [20].
It is noteworthy that all 3 patients who relapsed with acquired drug-resistant disease were not treated under the national TB program and did not receive DOT during their first TB episode. Two were HIV coinfected at the time of their first TB episode. This observation is consistent with the established fact that HIV-coinfected TB patients are at high risk for acquisition of drug (particularly rifampicin) resistance and underscores the vital role of DOT in these persons to achieve best treatment outcomes [21]. Also noteworthy was that, contrary to World Health Organization 2017 recommendations, the use of intermittent dosing (ie, thrice-weekly DOT) in the treatment continuation phase by our national TB program did not diminish its effectiveness as evidenced by our low relapse rate [22]. This attests to the quality of in-person DOT administered by our program through the years.
A strength of our study was the complete capture of all MTC culture-positive cases in Singapore. A study limitation was the lack of MIRU-VNTR and spoligotyping results for both disease episodes in 46% of the cohort, resulting in a small sample size for analysis. However, we believe that these cases were representative of the cohort as there was no difference in characteristics between those with and without available DNA fingerprinting results for both disease episodes. The unavailability of whole genome sequencing to more definitively exclude reinfection for our cases with the same DNA fingerprints for both disease episodes was another study limitation. Although MIRU-VNTR and spoligotyping have been used successfully in Northern European countries to distinguish reinfection and relapse [23, 24], it has been shown that these methods lack discriminatory power for strains of non–Euro-American lineage [25, 26]. The Beijing family strain and the East African–Indian strain account for 47% and 24%, respectively, of the strains in the country [27]. Another study limitation was the lack of data on pharmacodynamic factors such as therapeutic rifampicin levels and N-acetyltransferase type 2 status (which are not performed in routine clinical practice) of our study population, which could potentially influence treatment outcomes [28, 29]. Socioeconomic and lifestyle factors, which may be important determinants of risk for exogenous reinfection, were also not captured and analyzed in this study.
In conclusion, our study provides insights into recurrent TB disease in Singapore and its associated risk factors. We believe our finding of a significant association of concomitant PTB and extrapulmonary TB with relapse has identified a risk group for which measures to mitigate this outcome may be considered.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Potential conflicts of interest. All authors: No reported conflicts of interest.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. World Health Organization. Global tuberculosis report 2020. Geneva, Switzerland: WHO; 2020.
- 2. McIvor A, Koornhof H, Kana BD. Relapse, re-infection and mixed infections in tuberculosis disease. Pathog Dis 2017;75. doi: 10.1093/femspd/ftx020. [DOI] [PubMed] [Google Scholar]
- 3. Naidoo K, Dookie N. Insights into recurrent tuberculosis: relapse versus reinfection and related risk factors. IntechOpen 2018. doi:10.5772/intechopen.73601. [Google Scholar]
- 4. Lambert ML, Hasker E, Van Deun A, et al. . Recurrence in tuberculosis: relapse or reinfection? Lancet Infect Dis 2003; 3:282–7. [DOI] [PubMed] [Google Scholar]
- 5. Verver S, Warren RM, Beyers N, et al. . Rate of reinfection tuberculosis after successful treatment is higher than rate of new tuberculosis. Am J Respir Crit Care Med 2005; 171:1430–5. [DOI] [PubMed] [Google Scholar]
- 6. Mirsaeidi M, Sadikot RT. Patients at high risk of tuberculosis recurrence. Int J Mycobacteriol 2018; 7:1–6. [DOI] [PubMed] [Google Scholar]
- 7. Panjabi R, Comstock GW, Golub JE. Recurrent tuberculosis and its risk factors: adequately treated patients are still at high risk. Int J Tuberc Lung Dis 2007; 11:828–37. [PubMed] [Google Scholar]
- 8. Hermans SM, Zinyakatira N, Caldwell J, Cobelens FGJ, Boulle A, Wood R. High rates of recurrent tuberculosis disease: a population-level cohort study. Clin Infect Dis 2020; 72:1919–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ministry of Health, Singapore. Communicable diseases surveillance in Singapore 2018. Singapore: Ministry of Health; 2019. [Google Scholar]
- 10. Aber VR, Nunn AJ. Factors affecting relapse following short-course chemotherapy. Bull Int Union Tuberc 1978; 53:276–80. [PubMed] [Google Scholar]
- 11. Benator D, Bhattacharya M, Bozeman L, et al. ; Tuberculosis Trials Consortium. Rifapentine and isoniazid once a week versus rifampicin and isoniazid twice a week for treatment of drug-susceptible pulmonary tuberculosis in HIV-negative patients: a randomised clinical trial. Lancet 2002; 360:528–34. [DOI] [PubMed] [Google Scholar]
- 12. Jo KW, Yoo JW, Hong Y, et al. . Risk factors for 1-year relapse of pulmonary tuberculosis treated with a 6-month daily regimen. Respir Med 2014; 108:654–9. [DOI] [PubMed] [Google Scholar]
- 13. Khan A, Sterling TR, Reves R, et al. . Lack of weight gain and relapse risk in a large tuberculosis treatment trial. Am J Respir Crit Care Med 2006; 174:344–8. [DOI] [PubMed] [Google Scholar]
- 14. Hamilton CD, Stout JE, Goodman PC, et al. ; Tuberculosis Trials Consortium. The value of end-of-treatment chest radiograph in predicting pulmonary tuberculosis relapse. Int J Tuberc Lung Dis 2008; 12:1059–64. [PMC free article] [PubMed] [Google Scholar]
- 15. Zierski M, Bek E, Long MW, Snider DE Jr. Short-course (6 month) cooperative tuberculosis study in Poland: results 18 months after completion of treatment. Am Rev Respir Dis 1980; 122:879–89. [DOI] [PubMed] [Google Scholar]
- 16. Chang KC, Leung CC, Yew WW, et al. . A nested case-control study on treatment-related risk factors for early relapse of tuberculosis. Am J Respir Crit Care Med 2004; 170:1124–30. [DOI] [PubMed] [Google Scholar]
- 17. Nahid P, Dorman SE, Alipanah Net al. . Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America Clinical Practice Guidelines: treatment of drug-susceptible tuberculosis. Clin Infect Dis 2016; 63:853–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chee CB, Emmanuel SC, Wang YT. A brave STEP forward—the Singapore Tuberculosis Elimination Programme. Singapore Med J 1997; 38:359–60. [PubMed] [Google Scholar]
- 19. Chee CB, James L. The Singapore Tuberculosis Elimination Programme: the first five years. Bull World Health Organ 2003; 81:217–21. [PMC free article] [PubMed] [Google Scholar]
- 20. Chee CB, Lim LK, KhinMar KW, et al. . Surveillance of tuberculosis treatment outcomes of Singapore citizens and permanent residents, 2002–2011. Int J Tuberc Lung Dis 2014; 18:141–6. [DOI] [PubMed] [Google Scholar]
- 21. Sharling L, Marks SM, Goodman M, Chorba T, Mase S. Rifampicin-resistant tuberculosis in the United States, 1998–2014. Clin Infect Dis 2020;70:1596–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. World Health Organization. Guidelines for treatment of drug-susceptible tuberculosis and patient care, 2017 update. Geneva, Switzerland: WHO; 2017. [Google Scholar]
- 23. Korhonen V, Soini H, Vasankari T, Ollgren J, Smit PW, Ruutu P. Recurrent tuberculosis in Finland 1995–2013: a clinical and epidemiological cohort study. BMC Infect Dis 2017: 17:721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bang D, Andersen AB, Thomsen VO, Lillebaek T. Recurrent tuberculosis in Denmark: relapse vs. re-infection. Int J Tuberc Lung Dis 2010; 14: 447–53. [PubMed] [Google Scholar]
- 25. Jamieson FB, Teatero S, Guthrie JL, et al. . Whole-genome sequencing of the Mycobacterium tuberculosis Manila sublineage results in less clustering and better resolution than mycobacterial interspersed repetitive-unit-variable-number tandem-repeat (MIRU-VNTR) typing and spoligotyping. J Clin Microbiol 2014; 52:3795–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chee CBE, Lim LKY, Ong RTH, Sng LH, Hsu LY, Lee VJM, Wang YT. Whole genome sequencing analysis of multidrug-resistant tuberculosis in Singapore, 2006–2018. Eur J Clin Microbiol Infect Dis 2020; 40: 1079–83. [DOI] [PubMed] [Google Scholar]
- 27. Wang YT, Lim LKY, Hsu LY, Sng LH, Lee VJM, Chee CBE. Universal genotyping of Mycobacterium tuberculosis in Singapore, 2011–2017. Eur Respir J 2018; 52(Suppl 62):PA3884. [Google Scholar]
- 28. Magis-Escurra C, Anthony R, van der Zanden AGM, van Soolingen D, Alffenaar J-W. Pound foolish and penny wise—when will dosing of rifampicin be optimized? Lancet Respir Med 2018; 6:e11–12. [DOI] [PubMed] [Google Scholar]
- 29. Kinzig-Schippers M, Tomalik-Scharte D, Jetter A, et al. . Should we use N-acetyltransferase type 2 genotyping to personalize isoniazid doses? Antimicrob Agents Chemother 2005; 49:1733–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.