Abstract
Background/aims
A self-reported online survey was performed to investigate the immediate effect of COVID-19 lockdown restrictions in New Zealand on dietary intake, and lifestyle behaviours among pregnant women with diabetes.
Participants/methods
The survey was sent to 82 pregnant women who had Type 1, Type 2 Diabetes, or Gestational Diabetes and attended the Diabetes in Pregnancy Clinic in Wellington, New Zealand in May 2020, while the most restrictive COVID-19 lockdown measures were in place. All women received standard pregnancy nutrition advice provided by a dietitian, were monitoring blood glucose levels with nursing support, and seeing specialist endocrinologists and obstetricians for their pregnancy care.
Results
Fifty women (61%) responded to the survey. There was no evidence of differences in dietary intake during the restrictions, compared to before, for most food items. During the restriction's women consumed more bread (Odds Ratio (95% CI): 0.39 (0.18–0.83) p = 0.02); less battered fish: 3.11 (1.20–8.05) p = 0.02; and less hot chips/fries: 6.32 (2.67–14.93) p < 0.0001. During the restriction's women consumed more meals at home: 0.05 (0.14–0.15) p < 0.0001; less takeaways: 3.63 (1.54–7.34) p = 0.003; and less restaurant and café meals: 15.05 (6.03–37.59) p < 0.0001, when the services reopened.
Conclusions
The nutrition of pregnant women with diabetes was not compromised during a brief COVID-19 lockdown restriction. This finding is reassuring, with countries worldwide adopting brief intermittent lockdown periods to restrict the spread of the COVID-19 virus.
Keywords: COVID-19, Coronavirus, Diabetes, Pregnancy, Gestational Diabetes, Nutrition
1. Introduction
Coronavirus Disease 2019 (COVID-19) is a respiratory disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This novel coronavirus was declared a global pandemic by the World Health Organization in March 2020 [1]. Due to the high transmission rate and severity of this virus, the New Zealand (NZ) government committed to an elimination strategy in March 2020 [2]. On 25 March 2020, NZ was placed in Alert Level 4 Lockdown with restrictions for everyone to stay at home other than for essential personal movement. Working from home was encouraged for non-essential workers. Restrictions that impacted on access to food were the closure of all food outlets: fast food shops, takeaway outlets, cafes, and restaurants. Essential services remained open, such as supermarkets, convenience stores, and delivery businesses that provided meal ingredients which are prepared and consumed at home. The country remained in lockdown for five weeks before restrictions were lifted to Alert Level 3 on 27 April 2020 [3]. During Alert Level 3, restrictions were eased to allow businesses including food outlets to reopen if they could provide a service with no physical interaction with customers (see supplementary information). The country remained at Alert Level 3 with an easing of restrictions for two weeks until 13 May 2020.
In NZ, women with pre-existing diabetes and those diagnosed during pregnancy with gestational diabetes (GDM) are followed in a diabetes in pregnancy (DIP) clinic. The prevalence of GDM in NZ is higher among NZ Māori (7%), Pacific (11%), Asian (19%), and Indian (20%) compared with NZ European (5%) [4]. Dietary intervention is the primary treatment to meet the nutritional requirements of pregnancy and lessen adverse maternal and foetal outcomes known to occur with hyperglycaemia [5]. Many pregnant women do not meet nutritional guidelines for pregnancy in normal conditions [6,7], and we were concerned that during a time of social restriction, nutrition may have been further compromised. Potential factors included food choices, food availability, reduced physical activity, and financial implications, including food insecurity and uncertainty about long-term employment.
Understanding how these restrictions could affect dietary habits is essential for understanding the role of dietitians in a DIP clinic and what support can be offered to women during an epidemic-related quarantine in the future. Our study aimed to investigate the immediate effect that COVID-19 Alert Level 4 lockdown and Alert Level 3 restrictions in NZ had on dietary intake, types of meals consumed, lifestyle behaviours, and access to food, among pregnant women with diabetes.
2. Participants and methods
2.1. Study design and participants
This was a self-reported survey of pregnant women who attended the DIP Clinics at two hospital sites in Wellington, NZ. All pregnant women who had Type 1 diabetes (T1DM), Type 2 diabetes (T2DM) or GDM, were seen regularly throughout their pregnancy in the DIP clinic by a multidisciplinary team including obstetricians, endocrinologists, midwives, diabetes specialist nurses, and dietitians. Following the COVID-19 restrictions of social distancing, where clinically appropriate, consultations were held via telehealth, including standard pregnancy nutrition advice from the dietitian. Resources were provided that followed the NZ Food and Nutrition Guidelines for Healthy Pregnancy and Breastfeeding Women, including consume at least 2 portions of fruit per day, up to 4 serves of vegetables per day, at least 3 portions of dairy or dairy alternatives per day, choose mostly wholegrain bread and cereals, and limit consumption of high fat, high salt, and sugary foods/drinks [8]. Guidance of portion sizes of foods and even distribution of meals including, 3 meals and 2 to 3 snacks over the day was provided; women were encouraged to keep physically active and monitor their blood glucose levels.
The inclusion criteria were all pregnant women, aged 18 years and over, who were enrolled in the DIP clinic, between 13th and 27th May 2020. The exclusion criteria were pregnant women from the clinic who delivered before the 13th of May 2020.
All eligible women were sent an online survey via their smartphone on the 13th of May 2020, the last day of Alert Level 3. A reminder text message was sent one week and two weeks following the initial invite. The smartphone was chosen, as NZ has high ownership of smartphones, with 80% of the population having at least one smartphone [9]. If eligible women had limited access to a smartphone, mobile data, language barriers, or health literacy, then they were approached about the study in the clinic during Alert Level 2, when physical distancing was relaxed. Since GDM disproportionately affects NZ Māori and Pacific women and recruitment to studies of this population is typically low, all eligible women in the clinic, who identified as NZ Māori or Pacific were telephoned or approached about the study in the clinic by the researcher. The sample size was opportunistic based on attendees at the clinic during the pandemic.
The study was performed following the Declaration of Helsinki and ethical approvals were obtained from the NZ Health and Disability Ethics Committee (Ref 20/NTB/103), and the research ethics groups at the hospital sites. All participants were fully informed and gave consent to participate. There were no changes to their usual standard of care.
2.2. Survey methodology
The survey was completed anonymously on one occasion. Participants could choose to have a supermarket voucher posted to a specified address for their participation. The online survey was designed using REDCap (version 10.1.2 © 2020 Vanderbilt University) and was composed of 54 questions divided into five parts: (1) demographic information, (2) frequency of consumption of 18 selected food items, (3) frequency of types of meals consumed, (4) dietary and lifestyle behaviours; (5) access to food (see supplementary information). For demographic information, ethnicity was self-reported [10]. The New Zealand Index of Deprivation (NZDep) was used to measure the socioeconomic deprivation of women who took part in the study. The NZDep score is based on the geographical location of the individual and is calculated on nine variables from the 2018 census which reflect the eight dimensions of deprivation, with a score of 1 being least deprivation and 10 most deprivation [11]. Each participant's NZDep score was identified based on their domiciliary address.
2.3. Data analysis
Demographic characteristics were described with continuous variables expressed as mean and standard deviation (SD) and categorical variables expressed as number and proportions expressed as a percentage (%). Food item frequency was assessed with a Likert scale resembling an ordinal scale frequency of consumption. The data were paired and ordinal regression with a mixed linear model was used to assess the association between frequency of food consumption and relationship between before and during pandemic lock-down restrictions. With this method, the odds ratio reflected the odds (probability) of consuming the food more compared to less frequently, assuming a constant odds ratio between categories, and the paired data is accounted for by a random effect for participants allowing for correlated measurements for the same participants assessed twice. Continuous data were analysed by paired t-tests and strictly paired binary data by McNemar's test. For individual estimates of association 95% confidence intervals are shown with a nominal p-value for the significance of 0.05; however, there is no adjustment for multiplicity. SAS version 9.4 (SAS Institute, Cary, NC, USA) was used for all analyses.
3. Results
Of the 98 women enrolled in the DIP clinic between 13th and 27th May 2020, 82 women were eligible and invited to join the study and 50 (61%) responded to the anonymous survey. Forty-seven participants completed 100% of the survey and 3 participants completed 75% of the survey and were therefore included in the analysis. The characteristics of the respondents are summarised in Table 1 . Most women had GDM (72.9%), 12.5% T2DM and 14.6% T1DM, this was reflective of our cohort of women in the DIP clinic. The mean (range) age of the women was 32 (20–44) years. Most women were diagnosed with diabetes before the restrictions (72.9%). Self-reported ethnicity comprised of NZ Māori (12%), Pacific (20%), Indian/South Asian (22%), and European (28%). This reflected the ethnicity profile of the DIP clinic of NZ Māori (7.8%), Pacific (14.5%), Indian/South Asian (26.6%), and European (23.4%). In total 38% of women lived in households within the least deprived areas (score 1–2), and 15% of women lived in households within the most deprived areas (score 9–10). There were no cases of COVID-19 virus reported in this cohort of women, with 1500 confirmed cases in NZ, during the same period [12].
Table 1.
Characteristics of respondents.
| Variable | Mean (SD) [range] |
|---|---|
| Age (years) | 32.4 (5.4) [20 to 44] |
| Type of Diabetes | n/48d (%) |
| GDMa | 35 (72.9) |
| Type 2 DMb | 6 (12.5) |
| Type 1 DMc | 7 (14.6) |
| Diagnosed with diabetes | |
| Before restrictions | 35 (72.9) |
| Alert Level 4e | 7 (14.6) |
| Alert Level 3f | 6 (12.5) |
| Parity | |
| 0 | 18 (37.5) |
| 1 | 19 (39.6) |
| 2 | 8 (16.7) |
| 3 | 2 (4.2) |
| 4+ | 1 (2.1) |
| Ethnicity | n/50 (%) |
| NZ Māori | 6 (12) |
| Pacific Peoples | 10 (20) |
| Indian/South Asian | 11 (22) |
| Other Asian | 4 (8) |
| NZ European | 14 (28) |
| Other | 4 (10) |
| Social deprivation (NZDep)g | n/47 (%) |
| 1-2 | 18 (38) |
| 3-4 | 5 (11) |
| 5-6 | 6 (13) |
| 7-8 | 11 (23) |
| 9-10 | 7 (15) |
| No. of Dietitian consults during COVID-19 Alert Level 4 and 3h | Mean (SD) [range] |
| n/43 | |
| 2.3 (2.3) [0 to 8] | |
(GDM) Gestational Diabetes.
(T1DM) Type 1 Diabetes.
(T2DM) Type 2 Diabetes.
Two participants did not complete this question and the survey was completed anonymously.
Alert Level 4 lockdown, the most restrictive alert level with only essential shops open, see supplementary information.
Alert Level 3, fewer restrictions than Alert Level 4.
NZ Social deprivation score, decile 1 = household in the least deprived area to decile 10 = household in the most deprived areas, see methods section for further definition of deciles.
Dietitian consults between and including 25 March 2020 to 13 May 2020 (7 weeks).
3.1. Dietary intake
The frequency of 18 selected food items consumed before and during Alert Level 4 and Alert Level 3 restrictions is shown in Table 2 . The frequency of consumption of bread increased during Alert Level 4 compared to before the restrictions Odds Ratio (95% CI): 0.39 (0.18–0.83) p = 0.02. However, the type of bread consumed during the restrictions remained the same, with only a quarter of the women in the survey adhering to the guidelines of choosing wholegrain bread, before restrictions (24%) and during Alert Level 4 (26%) see supplementary information.
Table 2.
The frequency of food items consumed before and during alert level 4 and alert level 3 COVID-19 restrictions among pregnant women with diabetes.
| Food item | No. of servings per day n (%) |
OR (CI 95%) h | ||
|---|---|---|---|---|
| 0–1x day | 2–3x day | ≥4x day | ||
| Fruit | ||||
| Before | 9 (18) | 23 (66) | 8 (16) | |
| Level 4 | 7 (14) | 35 (70) | 8 (16) | 0.68 (0.32–1.46) p = 0.31 |
| level 3 | 7 (14) | 35 (70) | 8 (16) | |
| Vegetables | ||||
| Before | 4 (8) | 27 (54) | 19 (38) | |
| Level 4 | 2 (4) | 27 (56) | 21 (42) | 0.80 (0.36–1.79) p = 0.58 |
| level 3 | 3 (6) | 28 (56) | 19 (38) | |
| Dairy foods | ||||
| Before | 12 (24) | 34 (68) | 4 (8) | |
| Level 4 | 9 (18) | 34 (68) | 7 (14) | 0.49 (0.22–1.10) p = 0.08 |
| level 3 | 12 (24) | 31 (62) | 7 (14) | |
| Milk alternativesa | ||||
| Before | 42 (84) | 7 (14) | 1(2) | |
| Level 4 | 44 (88) | 5 (10) | 1(2) | 1.78 (0.65–4.87) p = 0.25 |
| level 3 | 44 (88) | 5 (10) | 1(2) | |
| Bread | ||||
| Before | 12 (24) | 25 (50) | 13 (26) | |
| Level 4 | 5 (10) | 29 (58) | 16 (32) | 0.39 (0.18–0.83) p = 0.02 |
| level 3 | 6 (12) | 33 (66) | 11 (22) | |
| Food item | No. of servings per week |
|||
|---|---|---|---|---|
| 0–1x week | 2–3x week | ≥4x week | ||
| Red Meat | ||||
| Before | 13 (26) | 29 (58) | 8 (16) | |
| Level 4 | 14 (28) | 31 (62) | 5 (10) | 1.30 (0.58–2.91) p = 0.52 |
| level 3 | 15 (30) | 30 (60) | 5 (10) | |
| Processed Meat | ||||
| Before | 29 (58) | 14 (28) | 7 (14) | |
| Level 4 | 27 (54) | 15 (30) | 8 (16) | 0.81 (0.36–1.82) p = 0.60 |
| level 3 | 30 (60) | 15 (30) | 5 (10) | |
| Fish fresh/frozenb | ||||
| Before | 36 (72) | 12 (24) | 2 (4) | |
| Level 4 | 41 (82) | 6 (12) | 3 (6) | 0.22 (0.002–25.29) p = 0.53 |
| level 3 | 42 (84) | 6 (12) | 2 (4) | |
| Fish battered | ||||
| Before | 42 (84) | 6 (12) | 2 (4) | |
| Level 4 | 45 (90) | 3 (6) | 2 (4) | 3.11 (1.20–8.05) p = 0.02 |
| level 3 | 40 (88) | 6 (12) | 0 (0) | |
| Legumes/pulses | ||||
| Before | 29 (58) | 15 (30) | 6 (12) | |
| Level 4 | 29 (58) | 12 (24) | 9 (18) | 0.82 (0.35–1.92) p = 0.63 |
| level 3 | 33 (66) | 9 (18) | 8 (16) | |
| Confectionaryc | ||||
| Before | 24 (48) | 15 (30) | 11 (22) | |
| Level 4 | 30 (60) | 8 (16) | 12 (24) | 1.47 (0.69–3.15) p = 0.31 |
| Level 3 | 33 (66) | 11 (22) | 6 (12) | |
| Cakes & biscuitsd | ||||
| Before | 23 (46) | 16 (32) | 11 (22) | |
| Level 4 | 27 (54) | 12 (24) | 11 (22) | 1.36 (0.65–2.81) p = 0.41 |
| Level 3 | 28 (56) | 18 (36) | 4 (8) | |
| Salty snackse | ||||
| Before | 20 (40) | 19 (38) | 11 (22) | |
| Level 4 | 22 (44) | 14 (28) | 14 (28) | 1.08 (0.51–2.28) p = 0.84 |
| Level 3 | 28 (56) | 12 (24) | 10 (20) | |
| Fruit juice | ||||
| Before | 31 (62) | 11 (22) | 8 (16) | |
| Level 4 | 36 (72) | 8 (16) | 6 (12) | 1.51 (0.67–3.38) p = 0.31 |
| Level 3 | 39 (78) | 8 (16) | 3 (6) | |
| Sugar Sweetened Beveragesf | ||||
| Before | 35 (70) | 8 (16) | 7 (14) | |
| Level 4 | 38 (76) | 8 (16) | 4 (8) | 2.02 (0.82–4.96) p = 0.12 |
| Level 3 | 40 (80) | 8 (16) | 2 (4) | |
| Hot chips/friesg | ||||
| Before | 30 (60) | 14 (28) | 6 (12) | |
| Level 3 | 42 (84) | 8 (16) | 0 (0) | 6.32 (2.67–14.93) p < 0.0001i |
n = 50.
Milk alternatives include soy, oat, coconut and rice milk.
Fish fresh/frozen includes shellfish.
Confectionary include sweets and chocolate.
Cakes & biscuits include muffins and sweet slices.
Salty snacks include nuts and crisps.
Sugar sweetened beverages, include sugar containing fizzy drinks and energy drinks.
Hot chips or fries from takeaway, fast food, café or restaurant only, includes French fries, wedges or sweet potato chips. No fast food, café or restaurants were open during Alert Level 4 restrictions.
Odds ratio (OR) of lower ordered values (lower frequency of servings) during Alert Level 4 compared to before the restrictions.
Odds ratio (OR) of lower ordered values (lower frequency of servings) during Alert Level 3 compared to before COVID-19 restrictions.
Women reported to consume less battered fish during Alert Level 4 compared to before the restrictions: 3.11 (1.20–8.05) p = 0.02, and consumed fewer servings of purchased hot chips/fries during Alert Level 3 when the shops reopened, compared to before the restrictions: 6.32 (2.67–14.93) p < 0.0001). There was no significant difference in reported dietary intake when comparing Alert Level 4 to before the restrictions for the remaining 15 food items (Table 2). Most women had a low consumption (zero to once per week) of confectionery, cakes & biscuits, salty snacks, fruit juice, sugar-sweetened beverages, processed meat, fried or battered fish, and hot chips/fries before and during both restriction levels (Table 2). This was per the pregnancy guidelines.
Most women met the guidelines of 2 or more servings of fruit per day before (82%) and during Alert Level 4 (86%), while only 42% of women met the guidelines for vegetables of 4 or more servings per day before and during Alert Level 4 (38%), see supplementary information. Similarly, 40% of women met the guidelines of 3 or more servings of dairy foods per day before and during Alert Level 4 (48%). There was no significant change in adherence to the guidelines during Alert Level 4 compared to before the restrictions, for fruit (−0.04 (−0.15 to 0.07) p = 0.48); vegetables (−0.04 (−0.12 to 0.04) p = 0.31); or dairy (−0.08 (−0.20 to 0.04) p = 0.20).
3.2. Types of meals consumed
The frequency of types of meals consumed before and during Alert Level 4 and Alert Level 3 restrictions is shown in Table 3 . Women were more likely to consume meals prepared at home during Alert Level 4 compared to before the restrictions: 0.05 (0.14–0.15) p < 0.0001. Women consumed fewer takeaways: 3.63 (1.54–7.34) p = 0.003 and were less likely to eat restaurant and café meals during Alert Level 3, when shops reopened, compared to before the restrictions: 15.05 (6.03–37.59) p < 0.0001.
Table 3.
The frequency of types of meals consumed before and during alert level 4 and alert level 3 COVID-19 restrictions among pregnant women with diabetes.
| Types of meals | Frequency of meals n (%) |
OR (CI 95%)c | |||
|---|---|---|---|---|---|
| 0–1x week | 2–3x week | 4–5x week | 6–7x week | ||
| Breakfast | |||||
| Before | 7 (14) | 7 (14) | 4 (8) | 32 (64) | |
| Level 4 | 5 (10) | 7 (14) | 2 (4) | 36 (72) | 0.59 (0.23–1.55) p = 0.28 |
| Level 3 | 6 (12) | 7 (14) | 1 (2) | 36 (72) | |
| Main meal prepared at home | |||||
| Before | 1 (2) | 5 (10) | 11 (22) | 33 (66) | |
| Level 4 | 0 (0) | 1 (2) | 2 (4) | 47 (94) | 0.05 (0.14–0.15) p < 0.0001 |
| Level 3 | 0 (0) | 1 (2) | 6 (12) | 43 (86) | |
| Main meal commercially provideda | |||||
| Before | 37 (75.5) | 6 (12.2) | 4 (8.2) | 2 (4.1) | |
| Level 4 | 36 (73.5) | 4 (8.1) | 7 (14.3) | 2 (4.1) | 0.97 (0.36–2.60) p = 0.95 |
| Level 3 | 38 (77.6) | 2 (4) | 7 (14.3) | 2 (4.1) | |
| Type of meals | Frequency of meals n(%) |
OR (CI 95%)d | ||||
|---|---|---|---|---|---|---|
| 0-<1x month | 1–2x month | 1x week | 2–3x week | ≥4x week | ||
| Takeawaysb | ||||||
| Before | 14 (28) | 15 (30) | 5 (10) | 15 (30) | 1 (2) | |
| Level 3 | 25 (50) | 10 (20) | 11 (22) | 4 (8) | 0 (0) | 3.63 (1.54–7.34) p = 0.003 |
| Restaurants & Cafes | ||||||
| Before | 10 (20) | 20 (40) | 9 (18) | 8 (16) | 3(6) | |
| Level 3 | 37 (74) | 9 (18) | 4 (8) | 0 (0) | 0 (0) | 15.05 (6.03–37.59) p < 0.0001 |
N = 50.
n = 49, Main meal commercially supplied or prepared (e.g. Hello Fresh, Woop, My Foodbag) and then consumed at home.
Takeaways include, fast food places like McDonalds, KFC.
Odds ratio (OR) of lower ordered values (lower frequency of meals) during Alert Level 4 compared to before the restrictions.
Odds ratio (OR) of lower ordered values (lower frequency of meals) during Alert Level 3 compared to before the restrictions.
3.3. Diet & lifestyle behaviours
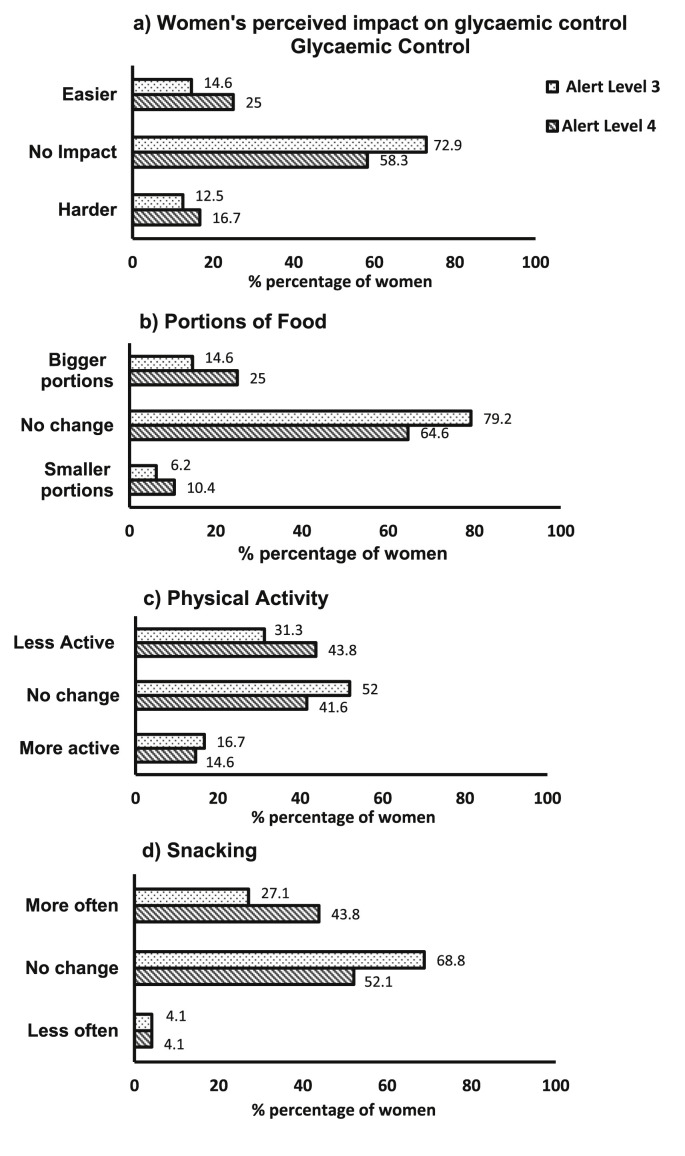
The impact of COVID-19 restrictions on lifestyle behaviours compared to before the restrictions are displayed in Fig. 1 . Compared to before the COVID-19 restrictions most women reported no change in how they perceived to manage their glycaemic control during the restrictions (Fig. 1). Compared to before the COVID-19 restrictions, 25% of women reported they perceived their glycaemic control was easier to manage during Alert Level 4 (lockdown). Women attributed this to not working and having more time to concentrate on glucose levels (n = 3), preparing meals at home (n = 3). Women reported that they could control the timing and preparation of food (n = 2), and were more physically active (n = 1).
Fig. 1.
The impact of COVID-19 Alert Level 4 and Alert Level 3 on Lifestyle Behaviours. a) Women's perceived management of glycaemic control during the restrictions compared to before. “Compared to before the restrictions how did Alert Level 4 impact your ability to stay within the recommended blood glucose range?” Options were easier, no impact or harder. b) The Impact of COVID-19 restrictions on portions of food consumed compared to before the restrictions. “Compared to your eating habits before the restrictions, how did Alert Level 4 change the amount you eat?”Options no change, smaller portions, bigger portions. c) The Impact of COVID-19 restrictions on snacking compared to before the restrictions, d) The Impact of COVID-19 restrictions on snacking compared to before the restrictions.
Compared to before the COVID-19 restrictions, 25% of women reported to consume bigger portions of food during Alert Level 4 (lockdown) (Fig. 1). Women attributed this to boredom (n = 3), and staying at home (n = 2).
Compared to before the COVID-19 restrictions 43.8% of women reported exercising less during Alert Level 4 (lockdown) (Fig. 1). Women attributed this to being less physically active than their usual routine (walking with friends, walking to work, the job was physically active, exercise classes) (n = 10), and feeling tired (n = 1).
Compared to before the COVID-19 restrictions, 43.8% of women reported snacking more during Alert Level 4 (Fig. 1). Women attributed this to boredom (n = 5), following dietary advice of 3 meals and 2 to 3 snacks per day (n = 3), change of environment at home (n = 3), managing nausea and hunger (n = 2), increased baking and cooking at home (n = 2).
3.4. Access to food
Compared to before the COVID-19 restrictions women reported they or someone in their household shopped less frequently at the supermarket in person and shopped more frequently using online supermarket shopping with home delivery or collection of items from the supermarket without entering the building (Table 4 ).
Table 4.
The frequency of different shopping methods before and during alert level 4 and alert level 3 COVID-19 restrictions among women with diabetes in pregnancy.
| Method of Shopping | Frequency of shopping n (%) |
OR (CI 95%)c | ||||
|---|---|---|---|---|---|---|
| 0-≤1x month | 1–2 x month | 1x week | 2–3x week | ≥4x week | ||
| Online supermarketa | ||||||
| Before | 38 (76) | 3 (6) | 6 (12) | 3 (6) | 0 (0) | |
| Level 4 | 28 (56) | 7 (14) | 11 (22) | 4 (8) | 0 (0) | 0.38 (0.15–0.95) p = 0.04 |
| Level 3 | 34 (68) | 4 (8) | 9 (18) | 3 (6) | 0 (0) | |
| Supermarketb | ||||||
| Before | 2 (4) | 8 (16) | 16 (32) | 17 (34) | 7 (14) | |
| Level 4 | 8 (16) | 13 (26) | 17 (34) | 12 (24) | 0 (0) | 5.96 (2.62–13.60) p < 0.0001 |
| Level 3 | 6 (12) | 13 (26) | 14 (28) | 17 (34) | 0 (0) | |
| Convenience storec | ||||||
| Before | 29 (58) | 9 (18) | 7 (14) | 5 (10) | 0 (0) | |
| Level 4 | 29 (58) | 6 (12) | 8 (16) | 5 (10) | 2 (4) | 0.81 (0.36–1.85) p = 0.61 |
| Level 3 | 28 (56) | 13 (26) | 4 (8) | 5 (10) | 0 (0) | |
N = 50.
Online supermarket shopping.
Supermarket shopping in person, by someone in the household.
Odds ratio (OR) lower ordered values (lower frequency of shopping) during Alert Level 4 compared to before the restrictions.
Most women 25 (52.1%) reported no change in household income while 23 (47.9%) reported a reduction in household income during the restrictions. Of the women who reported a reduced household income, 16 (69.6%) reported this did not affect their eating habits and 7 (30.4%) reported it did.
4. Discussion
The COVID-19 pandemic caused one of the most restrictive social environments in New Zealand, and many other parts of the world, in living memory. The findings from our study indicate that during a brief period of lockdown, there was minimal effect on dietary intake and lifestyle behaviours in pregnant women with diabetes. This finding is reassuring, with countries worldwide adopting brief intermittent lockdown periods to restrict the spread of the COVID-19 virus. There was a modest increase in bread consumption and a reduction in high-fat foods, including hot chips/fries, battered fish, and takeaway meals. Importantly, women met the nutritional guidelines in pregnancy before and during the restrictions for fruit, fried foods and sugary foods and beverages.
Overall, the COVID-19 Alert Level 4 lockdown in NZ had minimal effect on dietary intake. Similar to our findings, pregnant women without diabetes have reported no significant differences in dietary patterns [13], with increased intake of cereals and reduced intake of oils and fats observed [14] during COVID-19 restrictions. The minimal effect on dietary intake in our study may be due to negligible disruption to the food supply chain in NZ, with the relatively short duration of seven weeks of lockdown restrictions. NZ is a major producer of food and with a population of 5 million grows enough food to feed almost 40 million people [15]. With restrictions occurring during the summer months, local fruit and vegetables were abundant. Additionally, the NZ government implemented financial measures to buffer the loss of household income and provided emergency food assistance. The supermarkets and convenience stores remained open during the lockdown and online supermarket shopping with home delivery was also available. Restaurants and takeaway stores, however, did not operate during the lockdown restrictions and the positive impact of this on pregnant women was evident.
Importantly, most women met the nutritional guidelines for pregnancy before and during the restrictions, for servings of fruit (82–86%); minimal intake of hot chips/fries, battered fish, and sugary foods and beverages. This is in contrast to pregnant women, without diabetes and not living during a pandemic, who consumed fewer than the recommended servings of fruit per day (38%) [16]. Moreover, in non-pregnant women and men in NZ [17], and elsewhere [18] lower adherence to dietary guidelines for sugary foods and beverages during the COVID-19 restrictions has been demonstrated. The diligence of women in the study to limit intake of sugary foods and beverages and follow nutritional guidelines, where other populations have not succeeded, is noteworthy, and critical in the management of glycaemic control for women with diabetes. Moreover, the reduction in fried foods and takeaways could have positive maternal and foetal benefits with a potential reduction in energy intake. Slowing excess gestational weight gain (GWG), may reduce the rate of large for gestational age infants, macrosomia, and caesarean delivery [19].
In contrast, most women in this study consumed less than the recommended 4 servings of vegetables per day, before and during the restrictions. This was despite having dietitian input and with NZ being a net producer of vegetables. Further exploration of access to adequate vegetable intake to meet guidelines is warranted.
Pregnant women received ongoing nutrition advice and support from a dietitian as standard care, which may be the differentiating factor to other studies. It has been shown that dietary advice can lower the intake of refined sugars and fat intake with women with GDM [20]. Therefore, it would be worthwhile, to explore if the adherence to the pregnancy guidelines occurred before the women attended the clinic or because of the nutrition advice, they received from the dietitian. The women in our diabetes in pregnancy clinics are a unique group with high motivation to adhere to dietary advice. Generally, women reduce their intake of fried and fast food and increase fruit and vegetable consumption when they become pregnant [21]. Women report they prioritise the needs of the foetus first, which influences them to make healthy dietary choices for the benefit of their baby [22].
Wider societal influences may have affected the eating behaviour of the pregnant women, including concerns about household income leading to reduced consumption of meals from takeaways, cafes, and restaurants when they reopened, and the risk of being exposed to the COVID-19 virus when collecting food. Forty-eight percent of the general population reported fear of contracting the COVID-19 virus when supermarket shopping during the pandemic, particularly in women [23]. Changes to social connections have also been shown to have a detrimental impact on lifestyle behaviours among pregnant women during the COVID-19 pandemic [24].
In this study, 43.8% of women were less physically active during Alert Level 4 lockdown, similar to other studies that observed a significant reduction in physical activity levels of pregnant women without diabetes during the COVID-19 restrictions [13,24]. This was also reflected in the general population with 43–50% of people reducing their physical activity levels during the restrictions [25,26]. Physical activity, along with dietary intervention, can lower fasting and postprandial glucose levels in women with GDM [27]. This highlights the importance of additional support for pregnant women with diabetes during future pandemics to keep physically active. Similar to our findings, 23–60% of the general population reported increased between meals during the COVID-19 pandemic [28]. Boredom and stress contribute to increased snacking and subsequent less desirable food choices such as sugary and high-fat foods [29]. In our study ‘boredom’ was listed by some women as a reason for increased snacking. Interestingly, our findings showed although snacking increased, there was no significant increase in sugary or high-fat foods during the lockdown. Women in our clinic are advised to include two to three snacks per day to provide an even distribution of carbohydrates and optimise glycaemic control. Therefore, increased snacking could be considered a positive dietary change.
4.1. Limitations
One limitation of the study was that some of the confidence intervals for association were wide and so we were unable to rule out possibly large and important associations. Some statistical tests were performed without control of Type I error inflation, so associations may be spurious. However, the study was limited to a 2-week time frame in order to minimise the risk of recall bias of the women's experience during the restrictions. Self-reporting surveys have a bias with women wishing to appear to adhere to the guidelines. There may also have been selection bias, where women who were not following dietary advice, were less motivated to respond to the survey. This is somewhat offset by being an anonymous survey. It would be of interest in future studies to include food items such as cereals, nuts, and eggs which are important for healthy eating. We were unable to investigate the effect of food security in our group, but as food security is an essential part of following dietary guidelines, it would be important to incorporate this into future pandemic studies.
5. Conclusion
The nutrition of the pregnant women with diabetes in our NZ clinic was not compromised during a brief COVID-19 lockdown. This finding is reassuring with countries worldwide adopting rolling brief lockdown restrictions as a measure to restrict the spread of the COVID-19 virus. For future pandemics, support to keep women with diabetes in pregnancy physically active is important.
6. Statement of authorship
Tutangi Amataiti: Conceptualisation, Methodology, Investigation, Formal analysis, Writing – original draft. Fiona Hood: Conceptualisation, Methodology, Software, Writing - review & editing. Jeremy Krebs: Supervision, Conceptualisation, Methodology, Writing - review & editing: Mark Weatherall Formal analysis, Writing – review & editing. Rosemary Hall: Supervision, Conceptualisation, Methodology, Writing - review & editing. All authors have contributed and approved the manuscript.
Funding
This funding was supported by the Health Research Council of New Zealand and the Wellington Medical Research Foundation.
Declaration of competing interest
The authors declare they have no competing interests.
Acknowledgements
The authors would like to thank the participants who accepted to be part of the study and the multidisciplinary team from the Diabetes in Pregnancy clinic at Wellington Regional Hospital and Kenepuru Hospital, Capital & Coast District Health Board.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.clnesp.2021.07.011.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
A PDF document is attached that includes, key COVID-19 restrictions, the survey sent to participants, additional results of characteristics of respondents, frequency of food items, frequency of consumption of different types of bread, adequate intake of food items compared to pregnancy guidelines, frequency of types of meals consumed and frequency of different shopping methods
References
- 1.WHO announces COVID-19 outbreak a pandemic. 2020. http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic
- 2.Cousins S. New Zealand eliminates COVID-19. Lancet. 2020;395:1474. doi: 10.1016/S0140-6736(20)31097-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Health act (COVID-19 alert level 3) order 2020 (LI 2020/69) (as at 30 April 2020) contents – New Zealand legislation. http://www.legislation.govt.nz/regulation/public/2020/0069/latest/LMS339017.html?search=ts_act%40bill%40regulation%40deemedreg_alert_resel_25_a&p=1#LMS339020
- 4.NWH-Annual-Clinical-Report-2019.pdf. https://www.nationalwomenshealth.adhb.govt.nz/assets/Womens-health/Documents/ACR/NWH-Annual-Clinical-Report-2019.pdf
- 5.Metzger B.E., Lowe L.P., Dyer A.R., Trimble E.R., Chaovarindr U., Coustan D.R., HAPO Study Cooperative Research Group Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358:1991–2002. doi: 10.1056/NEJMoa0707943. [DOI] [PubMed] [Google Scholar]
- 6.Morton S.M.B., Grant C.C., Wall C.R., Atatoan Carr P.E., Bandara D.K., Schmidt J.M. Adherence to nutritional guidelines in pregnancy: evidence from the Growing up in New Zealand birth cohort study. Publ Health Nutr. 2014;17:1919–1929. doi: 10.1017/S1368980014000482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Caut C., Leach M., Steel A. Dietary guideline adherence during preconception and pregnancy: a systematic review. Matern Child Nutr. 2020;16:e12916. doi: 10.1111/mcn.12916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.New Zealand, Ministry of Health . Ministry of Health; Wellington, N.Z.: 2008. Food and nutrition guidelines for healthy pregnant and breastfeeding women: a background paper. [Google Scholar]
- 9.New Zealand - mobile social media penetration 2018. Statista. https://www.statista.com/statistics/680711/new-zealand-mobile-social-media-penetration/
- 10.Health Information Standards Organisation HISO inistry of Health . Ministry of Health; New Zealand: 2017. 10001:2017 ethnicity data protocols. [Google Scholar]
- 11.Atkinson J., Salmond C., Crampton P. University of Otago; Wellington: 2019. NZDep2018 Index of deprivation, user's manual. [Google Scholar]
- 12.COVID-19: current cases. Ministry of health NZ. https://www.health.govt.nz/our-work/diseases-and-conditions/covid-19-novel-coronavirus/covid-19-data-and-statistics/covid-19-current-cases
- 13.Biviá-Roig G., La Rosa V.L., Gómez-Tébar M., Serrano-Raya L., Amer-Cuenca J.J., Caruso S. Analysis of the impact of the confinement resulting from COVID-19 on the lifestyle and psychological wellbeing of Spanish pregnant women: an internet-based cross-sectional survey. Int J Environ Res Publ Health. 15 August 2020;17 doi: 10.3390/ijerph17165933. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang J., Zhang Y., Huo S., Ma Y., Ke Y., Wang P. Emotional eating in pregnant women during the COVID-19 pandemic and its association with dietary intake and gestational weight gain. Nutrients. 28 July 2020;12 doi: 10.3390/nu12082250. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Proudfoot I. KPMG; Auckland: 2020. Agribusiness agenda 2017: the recipe for action - KPMG New Zealand.https://home.kpmg/nz/en/home/insights/2017/06/agribusiness-agenda-2017-the-recipe-for-action.html [Google Scholar]
- 16.Slater K., Rollo M.E., Szewczyk Z., Ashton L., Schumacher T., Collins C. Do the dietary intakes of pregnant women attending public hospital antenatal clinics align with Australian guide to healthy eating recommendations? Nutrients. 13 August 2020;12 doi: 10.3390/nu12082438. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gerritsen S., Egli V., Roy R., Haszard J., De Backer C., Teunissen L. Seven weeks of home-cooked meals: changes to New Zealanders' grocery shopping, cooking and eating during the COVID-19 lockdown. J Roy Soc N Z. 2020:1–19. [Google Scholar]
- 18.Di Renzo L., Gualtieri P., Pivari F., Soldati L., Attina A., Cinelli G. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med. 8 June 2020;18 doi: 10.1186/s12967-020-02399-5. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldstein R.F., Abell S.K., Ranasinha S., Misso M., Boye J.A., Black M.H. Association of gestational weight gain with maternal and infant outcomes: a systematic review and meta-analysis. J Am Med Assoc. 2017;317:2207–2225. doi: 10.1001/jama.2017.3635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thomas B., Ghebremeskel K., Lowy C., Crawford M., Offley-Shore B. Nutrient intake of women with and without gestational diabetes with a specific focus on fatty acids. Nutrition. 2006;22:230–236. doi: 10.1016/j.nut.2005.07.017. [DOI] [PubMed] [Google Scholar]
- 21.Hillier S.E., Olander E.K. Women's dietary changes before and during pregnancy: a systematic review. Midwifery. 2017;49:19–31. doi: 10.1016/j.midw.2017.01.014. [DOI] [PubMed] [Google Scholar]
- 22.Baylis F., Ballantyne A., editors. Clinical research involving pregnant women. Springer International Publishing; 2016. Epub ahead of print. [DOI] [Google Scholar]
- 23.Sidor A., Rzymski P. Dietary choices and habits during COVID-19 lockdown: experience from Poland. Nutrients. 2020;12:1657. doi: 10.3390/nu12061657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Whitaker K.M., Hung P., Alberg A.J., Hair N.L., Liu J. Variations in health behaviors among pregnant women during the COVID-19 pandemic. Midwifery. 2021;95:102929. doi: 10.1016/j.midw.2021.102929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gallè F., Sabella E.A., Da Molin G., De Giglio O., Caggiano G., Di Onofrio V. Understanding knowledge and behaviors related to CoViD–19 epidemic in Italian undergraduate students: the EPICO study. Int J Environ Res Publ Health. 2020;17:3481. doi: 10.3390/ijerph17103481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Górnicka M., Drywień M.E., Zielinska M.A., Zielinska M., Hamulka J. Dietary and lifestyle changes during COVID-19 and the subsequent lockdowns among polish adults: a cross-sectional online survey PLifeCOVID-19 study. Nutrients. 3 August 2020;vol. 12 doi: 10.3390/nu12082324. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Allehdan S.S., Basha A.S., Asali F.F., Tayyem R. Dietary and exercise interventions and glycemic control and maternal and newborn outcomes in women diagnosed with gestational diabetes: systematic review. Diabetes Metab Syndr. 2019;13:2775–2784. doi: 10.1016/j.dsx.2019.07.040. [DOI] [PubMed] [Google Scholar]
- 28.Zupo R., Castellana F., Sardone R., Sila A., Giagulli V.A., Triggiani V. Preliminary trajectories in dietary behaviors during the COVID-19 pandemic: a public health call to action to face obesity. Int J Environ Res Publ Health. 27 September 2020;17 doi: 10.3390/ijerph17197073. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moynihan A.B., van Tilburg W.A.P., Igou E.R., Wisman A., Donnelly A.E., Mulcaire J.B. Eaten up by boredom: consuming food to escape awareness of the bored self. Front Psychol. 2015;6:369. doi: 10.3389/fpsyg.2015.00369. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A PDF document is attached that includes, key COVID-19 restrictions, the survey sent to participants, additional results of characteristics of respondents, frequency of food items, frequency of consumption of different types of bread, adequate intake of food items compared to pregnancy guidelines, frequency of types of meals consumed and frequency of different shopping methods