Abstract
This report describes a case of embolic myocardial infarction secondary to a pulmonary arteriovenous malformation. Pulmonary arteriovenous malformations are rare and mostly congenital and are inherited as an autosomal dominant disorder known as hereditary hemorrhagic telangiectasia. Myocardial infarction is an uncommon complication in patients with untreated pulmonary arteriovenous malformations. (Level of Difficulty: Advanced.)
Key Words: bubble echocardiography, cardiac magnetic resonance, computed tomography, genetic disorders, myocardial infarction, occluder, pulmonary circulation
Abbreviations and Acronyms: AVM, arteriovenous malformation; CT, computed tomography; HHT, hereditary hemorrhagic telangiectasia; MI, myocardial infarction; PAVM, pulmonary arteriovenous malformation
Graphical abstract
This report describes a case of embolic myocardial infarction secondary to a pulmonary arteriovenous malformation.…
Case
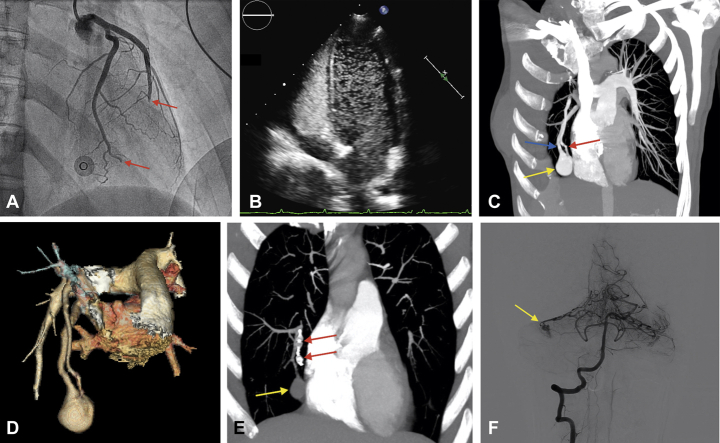
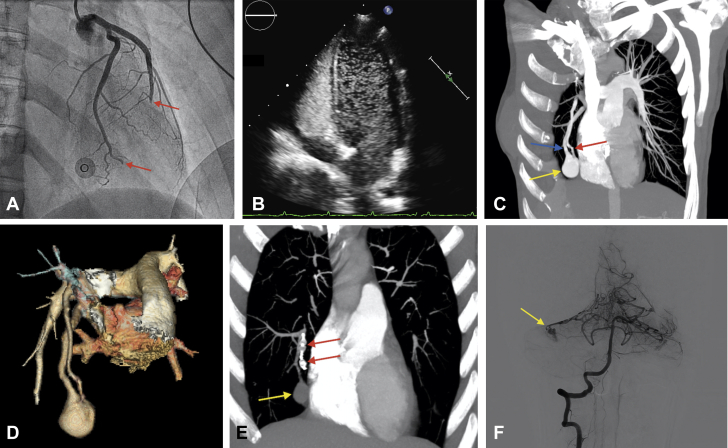
A 42-year-old woman with no relevant medical history presented to the emergency department with acute onset chest tightness. Physical examination and chest radiography results were normal. An electrocardiogram showed ST-segment elevation in the anterior and inferior leads, so an emergent cardiac catheterization was performed. Simultaneous embolic occlusion of the mid left anterior descending and the first obtuse marginal branch arteries were observed (Figure 1A, Video 1). Intracoronary thrombectomy and balloon angioplasty were successfully performed in both arteries with no evidence of coronary atherosclerosis.
Figure 1.
Coronary Angiography Results
(A) Coronary angiography shows embolic occlusion of mid LAD and OM1 (red arrows). (B) Saline-contrast echocardiogram shows bubbles in left cardiac cavities. (C) Thoracic CT shows PAVM (yellow arrow). The afferent artery (red arrow) and efferent vein (blue arrow) are observed. (D) 3-dimensional reconstruction. (E) Follow-up CT shows PAVM (yellow arrow) and occluder devices (red arrows). (F) Dural AVM appears in the right cerebellar hemisphere (yellow arrow). LAD = left anterior descending; OM1 = first obtuse marginal branch; PAVM = pulmonary arteriovenous malformation.
Online Video 1.
Coronary angiography showing simultaneously embolic occlusion of mid LAD and OM1.
At admission in the unit, the patient presented with an uncomplicated episode of epistaxis, which was managed conservatively. Laboratory findings were normal apart from a peak serum high-sensitivity troponin T concentration of 6,668 ng/l (normal range: 0 to 13 ng/l) and iron deficiency anemia. A thrombophilia study showed no significant abnormalities. Baseline echocardiography results were normal, except for an apical akinesia. During a saline-contrast echocardiogram that showed a massive right-to-left shunt (Figure 1B, Video 2) the patient presented with oppressive chest pain and transient ST-segment elevation. A transesophageal echocardiogram ruled out the presence of a patent foramen ovale. Suspecting an extracardiac shunt, her attending physician performed a contrast-enhanced thoracic computed tomography (CT) that demonstrated the presence of a 30-mm × 25-mm pulmonary arteriovenous malformation (PAVM) (Figures 1C and 1D), which was successfully embolized with 2 Amplatzer™ Vascular Plug IV devices (St. Jude Medical, Plymouth, Minnesota) (Video 3).
Online Video 2.
Saline-contrast echocardiogram demonstrating right to left shunt.
Online Video 3.
Transcatheter embolization of the PAVM.
A follow-up thoracic CT showed a decrease in the PAVM’s size and an absence of contrast enhancement (Figure 1E). The patient reported a long-term history of migraines, so a brain magnetic resonance scan was performed and showed a cerebellar arteriovenous malformation, which was confirmed by angiography and managed conservatively (Figure 1F). A genetic study demonstrated a p.Leu306Pro heterozygosis mutation in the endoglin (ENG) gene, associated with hereditary hemorrhagic telangiectasia (HHT).
HHT is an autosomal dominant disorder caused by mutations in the ENG, ACVRL1, or SMAD4 genes (1). Characteristic findings include systemic arteriovenous malformations, mucocutaneous telangiectasias, epistaxis, iron deficiency anemia, or paradoxical embolism. Despite the fact that low rates of myocardial infarction (MI) have been reported in these patients, prior cases of embolic MI have been described (2). Current HHT guidelines recommend that PAVMs should be embolized as long as it is technically feasible, even in asymptomatic patients, and a follow-up CT should be performed within 6 to 12 months after embolization (1).
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Informed consent was obtained for this case.
Appendix
For supplemental videos, please see the online version of this paper.
References
- 1.Faughnan M.E., Palda V.A., Garcia-Tsao G. HHT Foundation International---Guidelines Working Group. International guidelines for the diagnosis and management of hereditary haemorrhagic telangiectasia. J Med Genet. 2011;48:73–87. doi: 10.1136/jmg.2009.069013. [DOI] [PubMed] [Google Scholar]
- 2.Wu W., Lu C., Shen J., Zhang X., Zhang S. Paradoxical coronary embolisms as a presentation of hereditary hemorrhagic telangiectasia. J Am Coll Cardiol. 2014;63:e5. doi: 10.1016/j.jacc.2013.07.114. [DOI] [PubMed] [Google Scholar]