Abstract
We present the case of a patient with depression who attempted suicide through self-dissection and severing of her permanent pacemaker leads. The case highlights the importance of screening for psychiatric disorders prior to device implantation and continued surveillance for self-harm behaviors. (Level of Difficulty: Beginner.)
Key Words: depression, pacemaker, self-harm, suicide
Abbreviations and Acronyms: AVRT, atrioventricular node re-entrant tachycardia
Graphical abstract
This paper presents the case of a patient with depression who attempted suicide through self-dissection and severing of her permanent pacemaker leads…
History of Presentation
A 61-year-old woman with subclinical depression presented to the authors’ hospital with exposed pacemaker wires from her dual-chamber pacemaker (Figure 1). Her depression featured several chronic social stressors and physical limitation due to back pain, ultimately leading her to formulate a plan to disconnect her permanent pacemaker to end her life. Her pacemaker had been implanted 4 years previously following an atrioventricular re-entrant tachycardia (AVRT) ablation procedure that was complicated by complete heart block. Her suicide plan involved disconnecting her pacemaker because she believed she was pacemaker-dependent. At her last device clinic appointment, 3 months preceding her attempt, she was 99% ventricular paced in DDDR (NBG code for pacing nomenclature, meaning dual-chamber pacing, dual-chamber sensing, dual-mode response, rate modulation mode).
Learning Objectives
-
•
To help patients understand the nature of their ailments and the therapies, including device therapies that we offer.
-
•
It is important to screen for depression or self-harm behaviors prior to offering treatments and while patients are taking treatments, including devices such as pacemakers.
Figure 1.
Exposed Pacemaker Leads
Self-extracted dual-chamber pacemaker leads that are exposed and cut.
On the night prior to admission, the patient froze the skin overlying her pacemaker with ice, made an incision with a knife, reached for a wire inside the pocket, and cut it. She then took her pulse, which was still 60 beats/min. She then pulled out the second wire, presumably the right ventricular lead, and cut it as well. She retook her pulse, noting that her pulse was now 40 beats/min. She thought that she was successful in disconnecting the pacemaker and went to sleep, not expecting to survive the night. Ultimately, she was unsuccessful in her suicide attempt as she presented to the emergency department the following morning.
On presentation, the patient had a narrow escape rhythm of 43 beats/min, blood pressure of 112/89 mm Hg, and was afebrile. Her jugular venous pressure demonstrated cannon A waves. Her cardiac examination revealed variable S1 with normal S2 heart sounds and no murmurs. Her respiratory examination was unremarkable.
Medical history
AVRT ablation procedure identified a posterior septal pathway. The triangle of Koch mapped near the coronary sinus ostium was ablated for 41 s. This led to complete heart block, which did not resolve after 24 h.
Dual-chamber permanent pacemaker was placed by a cephalic vein approach. Pre-implantation stable junctional rhythm was 50 beats/min. The pacemaker was an Ingenio DR with Guidant Flextend atrial and ventricular leads (Boston Scientific, Marlborough, Massachusetts). Episodes of symptomatic atrial tachycardia required pharmacological management during follow-up.
Other medical issues included chronic low back pain, osteoporosis, hypothyroidism, motor tic, chronic bilateral shoulder tendinosis, and gastroesophageal reflux disease.
Medications
The patient was taking flecainide, 50 mg orally twice daily; digoxin, 0.125 mg orally, daily; clonidine, 0.2 mg orally, 3 times daily; clonazepam, 2 mg orally 3 times daily; levothyroxine, 37.5 μg orally daily; cetirizine, 10 mg orally daily; and pantoprazole, 40 mg orally twice daily.
Social history
The patient took ethanol in the form of <1 glass of wine by mouth and had a 7-pack-year history as an ex-smoker.
Investigations
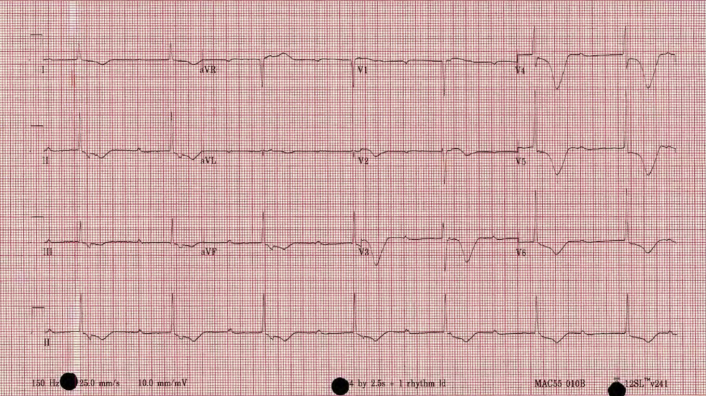
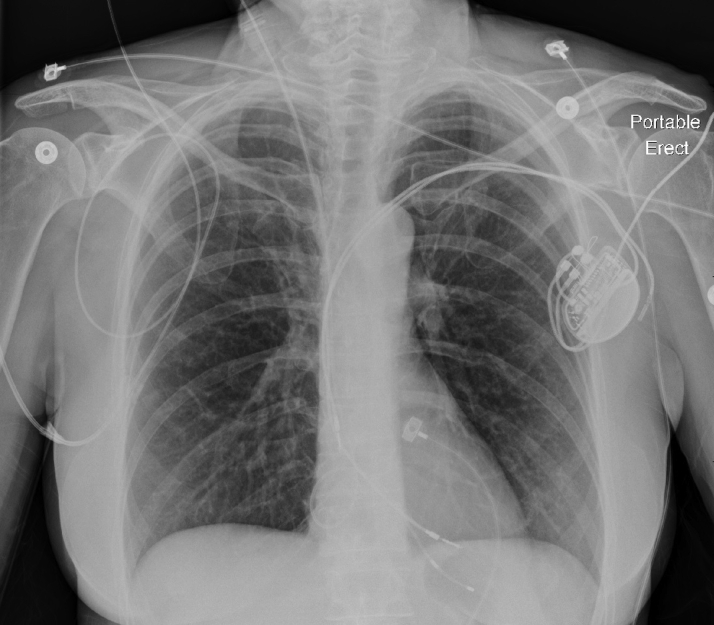
Her admission electrocardiography is shown in Figure 2. Admission bloodwork was normal (hemoglobin 140; white blood cell count 9.4; platelets 233; sodium 139; potassium 4.4; creatinine 94; alanine aminotransferase 21; aspartate aminotransferase 18), with normal toxicology screen (digoxin, salicylate, acetaminophen). Her chest radiograph demonstrated lead disconnection and a temporary pacemaker in place (Figure 3).
Figure 2.
Initial Electrocardiography
Electrocardiography demonstrating underlying rhythm (complete heart block with junctional escape) after disconnection of the dual-chamber pacemaker.
Figure 3.
Initial Chest Radiograph
Chest radiograph obtained upon admission shows the pacemaker lead disconnection from the generator and insertion of a transvenous pacemaker lead through the right internal jugular vein.
Management
Care for the patient was provided in consultation with various services, including arrhythmia, cardiac surgery, cardiology, and psychiatry. The patient was certified under the mental health act and admitted to the cardiac care unit for consideration of device removal and reimplantation. After extensive discussion with the patient and in consultation with psychiatry, the patient expressed remorse for her actions, so a new temporary pacemaker was inserted for symptomatic bradycardia.
Given the intentional breach of a sterile space, the patient was treated empirically with intravenous cefazolin during her admission, despite no clinical or microbiological evidence of infection. Ultimately, her permanent pacemaker was removed with laser-lead extraction without any complications. Implantation of a leadless pacemaker was considered but was not available at the authors’ institution at the time of this patient’s presentation, so a new dual-chamber pacemaker (Sensia L SEDRL1, Medtronic, Dublin, Ireland) was reimplanted (Figure 4). Psychiatry arranged for further outpatient follow-up with dialectical behavior therapy, and the patient was discharged home with a 10-day prescription of cephalexin along with pacemaker clinic follow-up.
Figure 4.
Post-Implantation Chest Radiography of a New Pacemaker
Post-operative chest radiography obtained after laser-lead device extraction and reimplantation of a new dual-chamber pacemaker device.
Discussion
This is the first known case of intentional self-harm in a patient who successfully deactivated her pacemaker by cutting its device leads at home. Other reported cases of self-harm include extraction of the pacemaker and its leads (1, 2, 3, 4), mutilation to the generator (5,6), and attempted lacerations over epicardial leads (7), which could be attributed to substance abuse, acute psychosis, or delirium. Our case illustrates the fact that patients with depression can, in a premeditated manner without the influence of psychosis or substances, use therapeutic devices to facilitate self-harm behavior. Manipulation of the pacemaker system, perhaps more commonly, is also done without the intent of self-harm as with the well described “twiddler’s syndrome” (8).
This case demonstrates the importance of recognizing (and treating) subclinical depression in patients who are being considered for cardiac device implantation. This responsibility falls upon device clinicians at the time of device implantation and also on primary care physicians during ongoing follow-up as the incidence of depression and suicide increases with age and number of comorbidities (9). Assessment tools such as the Medical Outcomes Study Short Form Survey (SF-36) and Hospital Anxiety and Depression Scale (HAD) are validated tools that have been used to assess the physical and psychosocial health of patients with implantable cardiac devices (10). Under certain clinical circumstances where there is ongoing concern for self-harm, it may therefore be reasonable to revisit the need for device implantation and, if so, consider other options less susceptible to self-manipulation such as implantation in less accessible anatomic locations or implantation of leadless devices.
The present case also highlights the lack of understanding some patients have of their treatments, which deprive patients of autonomy and can ultimately lead to unintended consequences. This patient was under the impression that severing her pacemaker wires would be fatal. However, this was not the case, and she inadvertently placed herself at risk for infection from the skin wound as well as complications related to generator and lead extraction and reimplantation. Informing the patient about the nature of pacemaker function as an augmentation rather than a sole provider of heart rhythm might have avoided exposing this patient to unintended risk.
Follow-up
The patient will follow up with the device clinic as well as the arrhythmia service at our hospital. She will also follow up with her family doctor to arrange for psychiatric as well as social support.
Conclusions
Psychosocial factors are important contributors to patients’ health and must be taken into consideration in all aspects of medicine, including implantable devices. This case underscores the importance of recognizing and treating underlying psychological conditions regardless of the medical setting.
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Informed consent was obtained for this case.
References
- 1.Harthorne J.W. Attempted suicide by self-removal of implanted pacemaker. Pacing Clin Electrophysiol. 1980;3:740–741. doi: 10.1111/j.1540-8159.1980.tb05581.x. [DOI] [PubMed] [Google Scholar]
- 2.Rosenthal R., Crisafi B.R., Coomaraswamy R.P. Manual extraction of a permanent pacemaker: an attempted suicide. Pacing Clin Electrophysiol. 1980;3:229–231. doi: 10.1111/j.1540-8159.1980.tb04334.x. [DOI] [PubMed] [Google Scholar]
- 3.Bordier P., Robert F. Suicide by self-removal of a pacemaker. Am J Forensic Med Pathol. 2004;25:78. doi: 10.1097/01.paf.0000113858.98640.d9. [DOI] [PubMed] [Google Scholar]
- 4.Norgaard M.L., Melchior T., Wagner T., Haugan K. Suicide attempt by complete self-removal of a 12-year-old permanent pacemaker system: case report. J Cardiovasc Electrophysiol. 2014;25:99–100. doi: 10.1111/jce.12295. [DOI] [PubMed] [Google Scholar]
- 5.Hochmeister M.N.M.D., Seifert D.M.D., Smetana R.M.D., Czernin J.M.D. Suicide attempted by aiming slaughtering gun at pacemaker. Letter. J Forensic Med. 1989;10:12. doi: 10.1097/00000433-198909000-00043. [DOI] [PubMed] [Google Scholar]
- 6.Corbisiero R., Muller D., Levy D.O.M., Armbuster D.O.R. Self-induced pacemaker mutilation three months post implant. J Cardiovasc Dis Res. 2014;2329:2. [Google Scholar]
- 7.Simon A.B., Kleinman P., Janz N. Suicide attempt by pacemaker system abuse: a case report with comments on the psychological adaptation of pacemaker patients. Pacing Clin Electrophysiol. 1980;3:224–227. doi: 10.1111/j.1540-8159.1980.tb04333.x. [DOI] [PubMed] [Google Scholar]
- 8.Bayliss C.E., Beanlands D.S., Baird R.J. The pacemaker-twiddler’s syndrome: a new complication of implantable transvenous pacemakers. Can Med Assoc J. 1968;99:371–373. [PMC free article] [PubMed] [Google Scholar]
- 9.Alexopoulos G.S. Depression in the elderly. Lancet. 2005;365:1961–1970. doi: 10.1016/S0140-6736(05)66665-2. [DOI] [PubMed] [Google Scholar]
- 10.Duru F., Büchi S., Klaghofer R. How different from pacemaker patients are recipients of implantable cardioverter-defibrillators with respect to psychosocial adaptation, affective disorders, and quality of life? Heart. 2001;85:375–379. doi: 10.1136/heart.85.4.375. [DOI] [PMC free article] [PubMed] [Google Scholar]