Abstract
Intra-aortic balloon pump via the axillary approach has been increasingly utilized to facilitate physical rehabilitation prior to definitive heart failure therapy. There is a high risk of device fracture with loss of arterial accessibility. Three cases are presented that demonstrate innovative arteriotomy hemostasis techniques for malfunctioning axillary intra-aortic balloon pumps. (Level of Difficulty: Intermediate.)
Key Words: acute heart failure, hemostasis, tamponade
Abbreviations and Acronyms: IABP, intra-aortic balloon pump; PCI, percutaneous coronary intervention
Graphical abstract
Intra-aortic balloon pump via the axillary approach has been increasingly utilized to facilitate physical rehabilitation prior to definitive…
An intra-aortic balloon pump (IABP) is often used in management for cardiogenic shock for mechanical circulatory support. IABP are designed for transfemoral placement; however, using this approach may introduce complications related to immobility in heart failure patients who may require many days of support. An attractive alternative is axillary arterial access for IABP placement. The IABP access site comes with unique complications and troubleshooting, mostly related to inflexibility of these devices. In their report of 50 axillary IABP patients, Estep et al. (1) reported a 44% rate of device migration requiring repositioning and 20% rate of device fracture requiring replacement. The standard practice at many institutions for IABP removal is to regain arterial wire access and use a Perclose (Abbott Vascular, Santa Clara, California) closure device (2). However, when the device fractures, rewiring is not possible, and manual compression is ineffective because the axillary artery is not opposed to a bony structure. There are reports of subclavian and axillary artery injuries due to penetrating and blunt trauma being treated with endovascular balloon tamponade for temporary hemostasis and endoluminal stents for definitive repair (3). Using prolonged intravascular balloon tamponade, with and without endoluminal stenting, has not been described previously. We present 3 cases of IABP fracture with loss of arterial access showing different innovative hemostasis techniques.
Learning Objectives
-
•
Recognize that axillary IABP can have complications such as migration and device fracture.
-
•
Describe contemporary endovascular techniques of achieving hemostasis of axillary IABP arteriotomy site.
-
•
Review risk and management of arterial dissection as a complication of endovascular balloon tamponade.
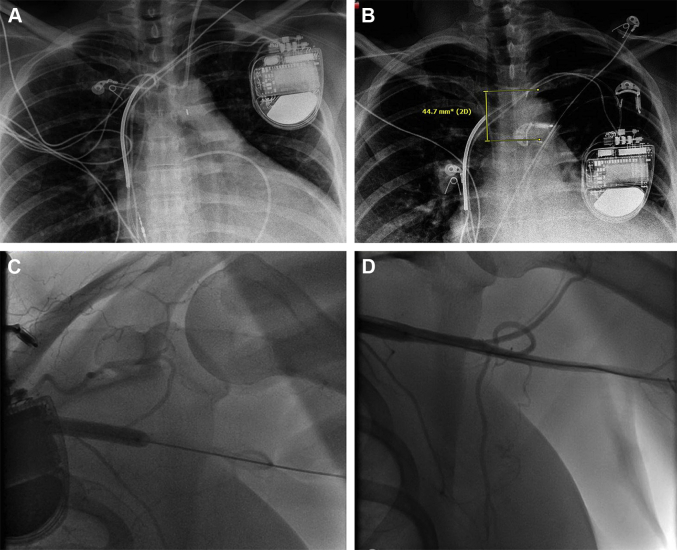
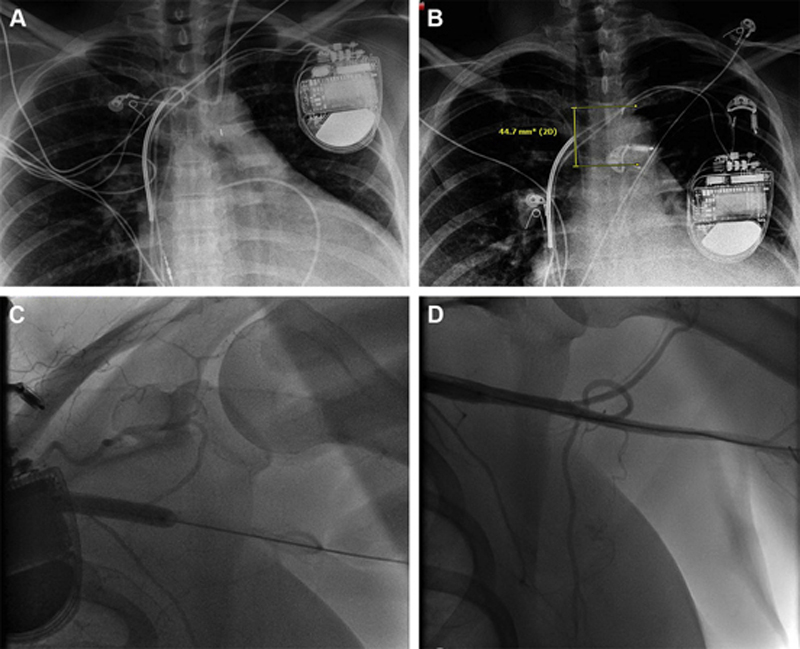
Patient #1 is a 41-year-old woman with stage D nonischemic cardiomyopathy who presented with cardiogenic shock requiring inotropes, aggressive diuresis, and ultimately a left axillary IABP for mechanical support as a bridge to durable left ventricular assist device. Axillary arterial access was obtained percutaneously under ultrasound guidance without difficulty, and an 8-F sheath was utilized. Approximately 6 days after axillary IABP placement, IABP alerted of pressure loss and blood was found in the helium tube, indicating rupture of the IABP. Replacement of the IABP was then emergently planned. She was hemodynamically stable with a palpable left radial artery pulse. Chest x-ray showed 4-cm proximal migration of the IABP device (Figures 1A and 1B).
Figure 1.
Case 1
(A) The initial chest x-ray. (B) The chest x-ray shows a 4-cm proximal migration of the intra-aortic balloon pump. (C) The chest x-ray shows a 6.0 × 40 mm Armada peripheral balloon, which was inflated for 20 min. (D) The post-inflation angiogram shows no extravasation.
We unsuccessfully attempted to rewire the IABP device. A 0.014 × 300 cm MiracleBros 12 guidewire (Asahi Intecc, Tustin, California) was advanced through the axillary arteriotomy insertion sheath past the IABP, and the IABP was externalized. A new IABP sheath could not be advanced due to the lack of wire support. Thus, the attempt to reinsert an axillary device was aborted. Manual pressure was applied without sufficient hemostasis. The right common femoral artery was accessed, and a 7-F 90-cm Destination sheath (Terumo Medical Corp., Somerset, New Jersey) was inserted; left subclavian angiography was performed using a Judkins Right 4 catheter. A 6.0 × 40 mm Armada peripheral balloon (Abbott, Chicago, Illinois) was inflated for 20 min at nominal pressure to obtain hemostasis in the axillary artery (Figure 1C). External manual compression was then discontinued, and repeat angiography showed no evidence of contrast extravasation or dissection (Figure 1D). Left radial and ulnar pulses remained intact. A femoral IABP was then inserted via the right common femoral artery. Heparin infusion had been held for 2 h during the procedure, and protamine was not utilized.
Patient #2 is a 48-year-old man with stage D nonischemic cardiomyopathy on home inotropes as a bridge to heart transplant that was admitted with cardiogenic shock. The patient was not a candidate for durable left ventricular assist device due to right ventricular dysfunction. An axillary IABP was inserted as a bridge to biventricular assist device placement in a similar fashion to case 1. Clinical course was stable, other than right knee hemarthrosis and left ventricular thrombus requiring heparin infusion. On day 10, harsh noises were noted by the patient, and 20 min later, there was loss of pressure and blood in the helium tube. The proximal IABP marker was displaced 6 cm above the carina on chest x-ray, compared with 2 cm at the time of insertion. The patient remained hemodynamically stable; however, the left radial pulse was decreased compared with the right side, which was concerning for acute vascular complication.
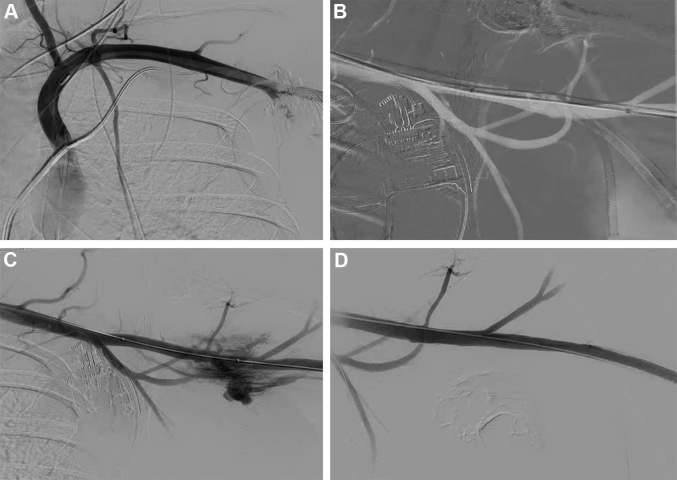
Fluoroscopy confirmed migration and “accordioning” of IABP (Figure 2A). Using common femoral arterial access, a 7-F 90-cm Destination sheath was inserted, and selective angiography of the left subclavian artery was performed without evidence of subclavian arterial injury. Keeping the angiogram as a roadmap, a 7 × 59 mm Armada balloon was advanced across the left axillary artery access site to use as an internal tamponade (Figure 2B). We failed to advance a 0.025-inch wire through the axillary IABP, and the accordioned IABP with the sheath were removed en block. The backup balloon was immediately inflated for 5 min at nominal pressure for internal tamponade. The balloon was then deflated, and selective left subclavian angiography revealed active contrast extravasation (Figure 2C). The balloon was then reinflated for 10 min twice, and 20 mg of protamine were given. After the protamine administration and the third balloon inflation, manual pressure was released and angiography revealed resolution of contrast extravasation from the left axillary arteriotomy (Figure 2D). A femoral IABP was inserted, and heparin infusion was restarted after 6 h without complications.
Figure 2.
Case 2
(A) Initial angiogram showing migration and accordioning of the intra-aortic balloon pump. (B) With the angiogram as the roadmap, a 7 × 59 mm Armada balloon was advanced across the left axillary artery access site. (C) Angiogram showing active contrast extravasation after a single balloon inflation. (D) No further extravasation is shown after repeated inflations and Protamine administration.
Patient #3 is a 61-year-old man with cardiogenic shock due to acute coronary syndrome. Diagnostic coronary angiography showed severe multivessel disease. He had an IABP placed as a bridge to surgical revascularization. Axillary arterial access was achieved per the standardized approach used in cases 1 and 2. However, this patient was later deemed not a surgical candidate and underwent high-risk percutaneous coronary intervention (PCI) with planned mechanical support.
An Impella CP (Abiomed, Danvers, Massachusetts) was initially placed via the left common femoral artery. He then had complex PCI of the left anterior descending chronic total occlusion and the severe left circumflex lesion. After the PCI, the left axillary IABP was removed, and external compression was applied. Planned balloon tamponade of the left subclavian artery was performed with an 8.0 × 40 mm Armada balloon. Balloon tamponade was successful in obtaining hemostasis of the left axillary IABP insertion site. However, final angiogram showed an extensive dissection of left subclavian artery originating at the IABP access site (Video 1). As such, further balloon inflations were performed at nominal pressure with follow-up angiogram showing a large residual flap. Due to a significant left axillary dissection, an Absolute PRO 8.0 × 100 mm stent (Abbott) was placed with satisfactory angiographic result. Importantly, dorsal scapular, thoraco-acromial, and circumflex humeral branches were all patent (Video 2).
Online Video 1.
Case 3: Dissection of Left Subclavian Artery
Extensive dissection of left subclavian artery starting at the access site for the intra-aortic balloon pump.
Online Video 2.
Case 3: Angiogram Post-Subclavian Artery Stenting
Angiogram of post-subclavian artery stenting showing patent vessel with no contrast extravasation.
These cases demonstrate the utility of prolonged intravascular balloon tamponade for the closure of transaxillary IABP. We have noted in our center that the IABP tends to migrate proximally, and malfunction and/or rupture occurred when the proximal radiopaque marker was >5 cm above the carina on chest x-ray. As such, we have anecdotally been serially following chest x-rays to reposition the device and in those cases, no complications were noted.
Typically, hemostasis of the axillary arteriotomy is achieved using Perclose with manual compression. Prolonged intravascular balloon tamponade has been used in trauma and hemorrhagic cases; however, this method has not been previously reported for closure of transaxillary arterial devices (4). Prolonged intravascular balloon tamponade, with or without protamine, is an effective technique for closure of transaxillary arterial devices. Per our experience, there was no upper extremity ischemia. Nevertheless, in the third case, prolonged balloon tamponade resulted in angiographically significant left axillary dissection requiring stenting. Of note, if stenting is needed, care must be taken to avoid jailing any of the many vital branches of the subclavian artery, mainly the vertebral and the humeral arteries. All of the interventions described herein were performed in the cardiac catheterization laboratory by interventional cardiologists with vascular surgery backup. We look forward to the release of dedicated IABP devices for axillary access.
Footnotes
Dr. Wayangankar has served as a proctor of valve therapies for Medtronic and Edwards Lifesciences; and as a consultant for Abiomed. Dr. Aranda has served as a consultant to ZOLL Medical Corp. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Informed consent was obtained for this case.
Appendix
For supplemental videos, please see the online version of this paper.
References
- 1.Estep J.D., Cordero-Reyes A.M., Bhimaraj A. Percutaneous placement of an intra-aortic balloon pump in the left axillary/subclavian position provides safe, ambulatory long-term support as bridge to heart transplantation. J Am Coll Cardiol HF. 2013;1:382–388. doi: 10.1016/j.jchf.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 2.Tayal R., Hirst C.S., Garg A., Kapur N.K. Deployment of acute mechanical circulatory support devices via the axillary artery. Expert Rev Cardiovasc Ther. 2019;17:353–360. doi: 10.1080/14779072.2019.1606712. [DOI] [PubMed] [Google Scholar]
- 3.Waller C.J., Cogbill T.H., Kallies K.J. Contemporary management of subclavian and axillary artery injuries—a Western Trauma Association multicenter review. J Trauma Acute Care Surg. 2017;83:1023–1031. doi: 10.1097/TA.0000000000001645. [DOI] [PubMed] [Google Scholar]
- 4.Wolf R.K., Berry R.E. Transaxillary intra-aortic balloon tamponade in trauma. J Vasc Surg. 1986;4:95–97. doi: 10.1067/mva.1986.avs0040095. [DOI] [PubMed] [Google Scholar]