Abstract
Patients pursuing solid organ transplantation are encouraged to receive many vaccines on an accelerated timeline. Vaccination prior to transplantation offers the best chance of developing immunity and may expand the pool of donor organs that candidates can accept without needing post-transplant therapy. Furthermore, transplant recipients are at greater risk for acquiring vaccine-preventable illnesses or succumbing to severe sequelae of such illnesses. However, a rising rate of vaccine refusal has challenged transplant centers to address the phenomenon of vaccine hesitancy. Transplant centers may need to consider adopting a policy of denial of solid organ transplantation on the basis of vaccine refusal for non-medical reasons (i.e., philosophical or religious objections or personal beliefs that vaccines are unnecessary or unsafe). Arguments supporting such a policy are motivated by utility, stewardship, and beneficence. Arguments opposing such a policy emphasize justice and respect for persons, and seek to avoid worsening inequities or medical coercion. This paper examines these arguments and situates them within the special cases of pediatric transplantation, emergent transplantation, and living donation. Ultimately, a uniform national policy addressing vaccine refusal among transplant candidates is needed to resolve this ethical dilemma and establish a consistent, fair, and standard approach to vaccine refusal in transplantation.
1. Background
Ethicists generally frame medical and public health ethical dilemmas around the principles of beneficence (benefit to the patient and/or the community), non-maleficence (avoidance of unnecessary harms), justice (fair and equal treatment), and respect for persons (autonomy and dignity).1 Solid organ transplant allocation by the Organ Procurement and Transplantation Network (OPTN) is informed by utility, or maximizing benefit for the greatest number of people, and justice, or fair distribution of resources.2 Transplant providers and centers serve as gatekeepers to transplant waiting lists. Regarding non-medical candidate criteria, the OPTN recommends that centers adopt policies that are broad, and universal, while also being attentive to unique individual circumstances. Lifestyle choices such as tobacco, alcohol, or illicit drug use are considered relative contraindications to transplantation, with individual centers specifying how these factors must be addressed prior to listing. The OPTN has recommended that adherence to treatment recommendations may be an appropriate non-medical consideration, specifically in cases of “serious, consistent, and documented non-compliance.”3
The number of people in the United States who refuse routine vaccination has increased. Despite Centers for Disease Control and Prevention (CDC) recommendations for universal influenza vaccination, influenza vaccine coverage among adults is only 44.8%. Pneumococcal vaccine coverage among adults with an indication to be vaccinated is only 23%.4 In 2019, the CDC estimated that, for kindergarteners, nationwide measles vaccine coverage was 94.7%, and as low as 87.4% in Colorado. The number of kindergarteners with a registered exemption from at least one required vaccination had risen to 2.5% from 2.1% in 2017, and the majority of exemptions were nonmedical, including philosophical objections (2.2% of children nationwide and up to 7.5% in Oregon).5 Pediatricians report dismissing children of vaccine-refusing parents from their practices at an increasing rate, up to 11.7% in 2013, citing lack of trust between parents and the healthcare team and concern for other patients.6
Vaccine hesitancy has been linked to ideas about bodily autonomy and parental authority, as well as mistrust of science, medicine, and government.7 A vocal anti-vaccination movement promotes these beliefs and advocates for vaccine refusal. While many patients expressing hesitancy may be persuaded by counseling and education, some patients persist in outright refusal. As a consequence of under-vaccination, outbreaks of vaccine-preventable illnesses are occurring at an increasing rate.5,8
Transplant providers recommend that candidates receive vaccines on an accelerated timeline.9 Despite this regimen, a 2019 study found that less than 90% of pediatric liver transplant recipients were up to date on live vaccinations before their transplant, and only 55% were up to date on all age-appropriate vaccinations, although reasons for under-vaccination were not specified.10 In a 2011 survey of pediatric organ transplant programs, 39% of programs had experienced cases involving caregiver refusal of vaccination for non-medical reasons (i.e., philosophical or religious objections or beliefs that vaccines are unnecessary or unsafe). When presented with a hypothetical scenario of a patient whose guardian had refused all vaccinations, 47% of respondents reported that their program would list the patient for transplantation, 22% said they would not, and 30% were unsure; only 4% of pediatric transplant programs reported having a written policy regarding vaccine refusal.11 Adult transplant practices have never been studied in the same way. Currently, no national policy addresses this issue, although guidelines universally recommend routine vaccination for transplant candidates.9,12
2. Objectives
The authors are comprised of transplant infectious diseases professionals and bioethicists with experience in transplantation and vaccination from both adult and pediatric transplant centers throughout the United States. We collaborated on this manuscript to advocate for further discussion with a broader group of experts and stakeholders prior to issuing any “consensus” policy. This paper reviews existing data on the relationship of vaccination and non-vaccination with transplant outcomes, and presents ethical arguments to the question: “Is it ethically permissible to institute a policy of denying solid organ transplantation on the basis of refusal of medically-indicated vaccinations?” (Table 1). We also assess these arguments within the special cases of pediatric transplantation, emergent transplantation, and living donation, with the intent of stimulating discussion toward a uniform guideline.
Table 1: Summary of ethical arguments.
Table 1 briefly summarizes the arguments in support of denying solid organ transplantation on the basis of vaccine refusal, and the arguments in opposition.
| Is it Appropriate to Deny Solid Organ Transplantation on the Basis of Vaccine Refusal? | |
|---|---|
| Arguments in Support | Arguments in Opposition |
| Beneficence: Benefits the patient by protecting the patient and their graft from complications of vaccine-preventable illness. | Non-maleficence: Inability to access a transplant causes immediate, severe, and irreversible harm to patients who refuse vaccination. |
| Beneficence: Maximally protects others in the clinical environment, including transplant patients, other patients, and healthcare staff. Avoids negative impact on performance metrics and transplant center liability. | Autonomy: Achieving vaccination through coercion risks damaging the provider-patient relationship, the family unit and the public perception of vaccination. |
| Stewardship: Maximizes the benefits of organ transplantation, a scarce resource. | Justice: Creates additional barriers to transplantation for patients from marginalized groups. |
| Justice: Is consistent with OPTN recommendations that “serious, consistent, and documented non-compliance” be considered in listing decisions. | Respect: Relies on unproven assumptions about adherence to other recommendations apart from vaccination, and fails to respect patients’ reporting of their intentions. |
Abbreviations: OPTN, Organ Procurement and Transplantation Network.
3. Arguments in Support of Denying Solid Organ Transplantation on the Basis of Vaccine Refusal
Proponents argue that denying organ transplantation to patients who refuse vaccines is justified based on the medical benefits of vaccination for transplant recipients, stewardship of the scarce resource of donated organs, and improvement in the general utility of transplantation (Table 2). At the individual level, patients who are under-vaccinated face greater risk of poor outcomes for themselves and for their grafts.13 For example, while some vaccine-preventable illnesses are rare, others such as pneumococcal pneumonia and influenza are common and result in significant morbidity and mortality among solid organ transplant recipients.14 Transplant recipients who have an impaired immune response from anti-rejection medications may suffer even more severe presentations of vaccine-preventable illness, including accelerated progression of human papillomavirus-associated cervical and anal carcinomas.15 Liver transplant candidates who are vaccinated against Hepatitis B can be considered for transplants from hepatitis B core antibody-positive donors, while candidates who are not vaccinated either cannot be considered or require post-transplant treatment.16 Diagnosing vaccine-preventable illness may be more challenging in transplant recipients because of atypical presentations and the broad differential diagnosis for common symptoms like fever and rash. Complications of vaccine-preventable illnesses may include allograft rejection.17,18
Table 2: Levels of risk associated with vaccine refusal in solid organ transplantation.
Table 2 categorizes the risks considered in the utilitarian justification of denial of solid organ transplantation on the basis of vaccine refusal. The graft is placed at the broader community end of the spectrum because the placement of the organ and subsequent fate of the graft represent the summative impact of listing and allocation decisions and holds significance for all patients awaiting transplantation, not just one hypothetical recipient.
 |
Recipient |
|
| Other patients |
|
|
| Institutional environment |
|
|
| Transplant center |
|
|
| Graft |
|
These risks may extend to other recipients and candidates at the transplant center, patients who are immunosuppressed because of other medical conditions treated at a large medical center, and to the general population. Other patients may be put at undue risk regardless of their own desire to get vaccinated. Documented instances of measles transmission from unvaccinated infected patients in the clinic setting have occurred, including to vaccinated patients.19,20 At the community level, a high proportion of non-medical exemptions for required vaccines has been associated with heightened risk for both unvaccinated and vaccinated community members.21 Thus, from a public health ethics perspective, non-maleficence to the community must also be considered.
Difficulty diagnosing vaccine-preventable illnesses in the transplant recipient population also poses challenges for infection prevention and control. Delayed detection, high viral loads, and prolonged viral shedding in the context of immunosuppression increase the risk of transmissions from these patients.22 Costs can be considerable even for one exposure, as crucial prevention strategies like intravenous immune globulin are expensive, and in short supply.23 Transplant programs may face legal or regulatory questions about the level of protection provided to patients who develop vaccine-preventable illness, or to patients affected by subsequent infections or exposures.24 An outbreak can shut a transplant center down completely, with adverse effects for all patients served by that center.
Many proponents of vaccination requirements also argue that patients who refuse vaccination may hesitate when presented with the more intensive and invasive demands of transplantation including multi-agent immunosuppression, routine procedural testing (i.e., biopsies), dietary restrictions, etc. Although data supporting this conjecture are sparse, pediatric patients whose guardians refuse vaccination present less frequently for routine care, as documented in one study.25 This argument is clearly weighed very highly by transplant clinicians; in the aforementioned survey of pediatric transplant centers, 70% of respondents cited possible non-adherence to post-transplantation care as the leading rationale for considering vaccine-refusal in listing decisions.11 If validated, this concern would align with recommendations from the OPTN that “serious, consistent, and documented non-compliance” be considered in listing decisions.3
Arguments in support of denying solid organ transplantation on the basis of vaccine refusal must also address concerns about fairness and autonomy. Proponents argue that not listing such patients would be fair because access to transplantation would be restricted based on a factor that is within the patient’s control. Some patients opposed to vaccination might object that restricting access to transplantation represents a violation of autonomy. However, proponents may argue that this small encroachment on autonomy is justified by the substantial benefits of vaccination to the patient and the community. Perhaps most importantly, because organs represent a scarce resource, some limits to freedom of choice (autonomy) may be justified to optimize the utility of transplantation. This example is similar to many socially accepted public health situations in which infringement of personal autonomy is ethically permissible and legally mandated in order to protect the wellbeing of the population (i.e., tobacco policy).26
4. Arguments in Opposition to Denying Solid Organ Transplantation on the Basis of Vaccine Refusal
Opponents of denying transplantation to patients who refuse vaccination may recognize the safety, cost-effectiveness, and individual and public health benefits of vaccination, but still feel that denying transplantation on the basis of vaccine refusal crosses a moral boundary. Their arguments challenge claims that vaccination substantially increases overall utility, and raise concerns about justice and autonomy. Because vaccine refusal is, so far, uncommon, the difference in transplant outcomes between vaccinated and non-vaccinated recipients would have to be substantial to justify excluding vaccine-refusing patients on the basis of overall utility. While case reports describe severe outcomes from vaccine-preventable illness, many presentations, at least in immunocompetent hosts, are associated with low mortality and manageable morbidity. Some outcomes may be more favorable today than when vaccine-preventable illnesses were last widespread, owing to improvements in treatment and supportive care.27 All of these considerations would attenuate the benefits of mandatory vaccination. From the perspective of the individual patient, even under-vaccinated, receiving a transplant clearly remains in that patient’s best interest. When considering the principles of beneficence and non-maleficence, opponents of vaccination requirements weigh the immediate, certain, and severe harms of denial of organ transplantation much more heavily than the possibility of downstream complications due to vaccine-preventable illness. Claims about community risk can also be challenged, particularly outside of larger community outbreaks or clusters. Studies of community risk deal with geographic areas where there is extensive, long-term commingling in schools, workplaces, and public spaces, and are not representative of healthcare environments.
If non-vaccination decreases patient and graft survival (utility), then patients who are unable to be vaccinated for a medical contraindication and patients who fail to mount a protective immune response after vaccination would also need to be considered less than ideal transplant candidates, but this is not being proposed. The claim that vaccine-refusing patients will also be non-adherent to other recommended treatments remains untested.7 While OPTN ethics guidelines advise transplant programs to consider documented non-adherence in waitlisting decisions, the OPTN emphasizes that some pre-transplant behaviors like dietary indiscretion or missing dialysis may not be indicators of post-transplant behaviors, and the same may be true for vaccine refusal.28 In the absence of evidence linking vaccine refusal to post-transplant behavior, taking patients at their word about their beliefs and intentions toward other treatments beside vaccination may be more respectful.
Injustices resulting from vaccine requirements are nuanced in the context of existing social structures. Vaccine refusal differs by racial, ethnic, socioeconomic, or religious groups. A large proportion of vaccine refusers are white and well-educated, a group that is not typically marginalized or structurally oppressed. However, vaccine hesitancy is also more common among African Americans than the general population, with community members in one study citing past instances of medical abuse against African Americans as sources of ongoing fear and mistrust of the medical system.29 Denial of organ transplantation to patients who have refused vaccination because of mistrust earned from historic mistreatment of marginalized communities may increase inequities in transplantation and exacerbate transgenerational traumas. Clusters of vaccine-preventable illness related to societal or religious vaccine refusals have also occurred amongst Orthodox Jewish communities in New York, Somali-Americans in Minnesota, and on the United States-affiliated island of Samoa.30 Opponents of mandatory vaccination emphasize the risk of magnifying existing disparities in transplantation by disproportionately affecting people of color, immigrants, non-English language speakers, or minority religious groups.31
Finally, opponents of vaccination requirements argue that such policies may be coercive, by tying access to a life-saving medical intervention to preventive care that the patient has historically refused. Medical coercion occurs when a patient is compelled to accept a proposal (such as vaccination) that they otherwise may reject because of an imposed threat of an unacceptably worse outcome.32 Importantly, based on this definition of coercion, such an outcome (not receiving an organ transplant) must be below a standard that patient is normally entitled to.33 When coercion occurs, it is a serious violation of respect for persons and may damage the provider-patient relationship.34 Even if we conclude that the patient is not normally entitled to receiving an organ transplant, the perception of coercion alone may be damaging.35 Vaccine requirements shift clinical practice away from education and shared decision-making. Rather than promoting vaccine acceptance, these policies may validate accusations of single-mindedness and lack of respect, further alienating those expressing vaccine hesitancy and further damaging, rather than improving, population health (beneficence, utility).
5. Special Considerations
5.1. Which Vaccines should be required?:
All recommended vaccines have substantial individual and public health importance and a proven safety record, and vaccination is prioritized prior to transplantation to maximize safety and efficacy. Any proposed vaccine requirements should be consistent across institutions and rooted in established evidence. This could be achieved by basing requirements on existing guidelines from national organizations such as the Advisory Committee on Immunization Practices (ACIP).36 Most insurance plans and many state-sponsored programs cover ACIP-recommended vaccinations or provide them for free, and the National Vaccine Injury Compensation Program offers a mechanism for redress of vaccine injury petitions related to covered vaccines.37 Some transplant programs may encourage additional off-schedule vaccination or vaccines not yet approved for this population, but individualized recommendations above and beyond a standard group of vaccines should not be included in a policy of vaccine requirements. For new vaccines, such as those currently in development for SARS-CoV-2, a demonstrated track record of safety and efficacy must be established before these vaccines will be included in ACIP recommendations. In addition, as with other new agents, safety and efficacy should be demonstrated for patients with end-stage organ dysfunction or organ transplants, and any theoretical risk for immunostimulation must be considered prior to updating vaccine requirements specific to transplant candidates.
5.2. Children of vaccine-refusing guardians:
Requiring vaccination prior to transplantation may result in some children being vaccinated, but may also lead to rare scenarios where a child faces the loss of a life-saving opportunity because of their guardians’ unwavering convictions. Some state courts have established a legal precedent that parental vaccine refusal may be viewed as medical neglect, but generally focus on engaging parents over time rather than more intrusive measures.38 While education should be emphasized, the accelerated vaccination timeline prior to transplantation or some cases of persistent vaccine refusal may lead to situations where agreement cannot be reached. In these situations, transplant programs would need to carefully consider whether to involve state actors (child protection agencies, courts) to accomplish vaccination of children over parental objection prior to transplantation. There is precedent for treatment over parental objection when children face serious, immediate harm from parental decisions, as with blood transfusion for children of Jehovah’s witnesses.39 While there is no comparable precedent for state agencies or courts to require routine vaccination of children over parental objection, it could be argued that if transplantation is essential to the welfare of the child and it cannot be performed unless the child is vaccinated, the threshold for state intervention has been met.
5.3. Emergent transplantation:
Fulminant organ failure requiring emergent transplantation may not afford an opportunity for in-depth counseling about vaccines, and even when counseling can occur, these patients are vulnerable by virtue of the lack of time to consider their options. Even if a patient receives counseling and agrees to be vaccinated, any vaccines given shortly before or shortly after transplantation are less likely to be effective because of intensive immunosuppression, and live virus vaccines would be contraindicated. This situation shares commonalities with transplantation in the setting of acute alcoholic hepatitis. Programs will transplant selected patients with fulminant liver failure from alcohol use with the understanding that these patients have no opportunity to demonstrate commitment to sobriety.40 This “benefit of the doubt” approach should be considered in cases of fulminant organ failure and vaccine refusal, even if other patients are expected to comply with vaccine requirements.
5.4. Living Donation:
Living donors who offer an organ by directed donation do so outside of the usual framework of organ allocation, and already are not held to the same standards for general utility (i.e., the greatest benefit for all candidates awaiting transplantation). However, transplant centers have an obligation to proceed with living donation only when there is a good chance of safety and benefit for both the donor and recipient, and the importance of vaccination for recipients remains a reasonable consideration.41 Whether or not a policy requiring vaccination for deceased donor transplantation is enacted, potential living donors should be informed that recipients who refuse vaccination may be at increased risk for adverse outcomes, consistent with OPTN policy regarding informed consent for living donation.42 Recipients who refuse vaccination despite education and counseling should be instructed to take every possible action to protect themselves from infection, and transplant centers should also take actions to protect other patients, for example by requiring that unvaccinated patients wear a mask in the waiting room.
6. Conclusion:
Vaccine refusal has contributed to the increasing incidence of vaccine-preventable illnesses. Patients pursuing solid organ transplantation may be among those who are unvaccinated or under-vaccinated due to vaccine refusal or hesitancy. Transplant centers screening patients for their appropriateness for listing may desire to include vaccination status as a part of this evaluation. The ethical frameworks of beneficence and utility provide the justification for denying solid organ transplantation on the basis of vaccine refusal. Risks to the graft, the patient, other patients in the clinical environment, the transplant program, and society, should all be considered. Opponents of such policies voice concerns with regard to justice, autonomy, and medical coercion. These issues require special consideration in situations of pediatric transplantation, emergent transplantation, and living donation. A uniform national policy developed with input from a diverse group of stakeholders is urgently needed to standardize the approach to this challenge. We have proposed a policy development process beginning with baseline needs assessment and coalition-building, followed by detailed review, and ratification by national transplant organizations. (Figure 1) Bringing together a diverse group of experts to address key parallel considerations such as vaccine access, cost, education for candidates, families, and clinicians, and contingency planning for adverse events will establish a safe, equitable, and trustworthy context for deploying any new policy. Finally, we propose ongoing assessment of vaccination practices, outcomes after transplantation, impact on equity in transplantation, and public opinion after implementation.
Figure 1: Proposed Framework for National Guideline Development.
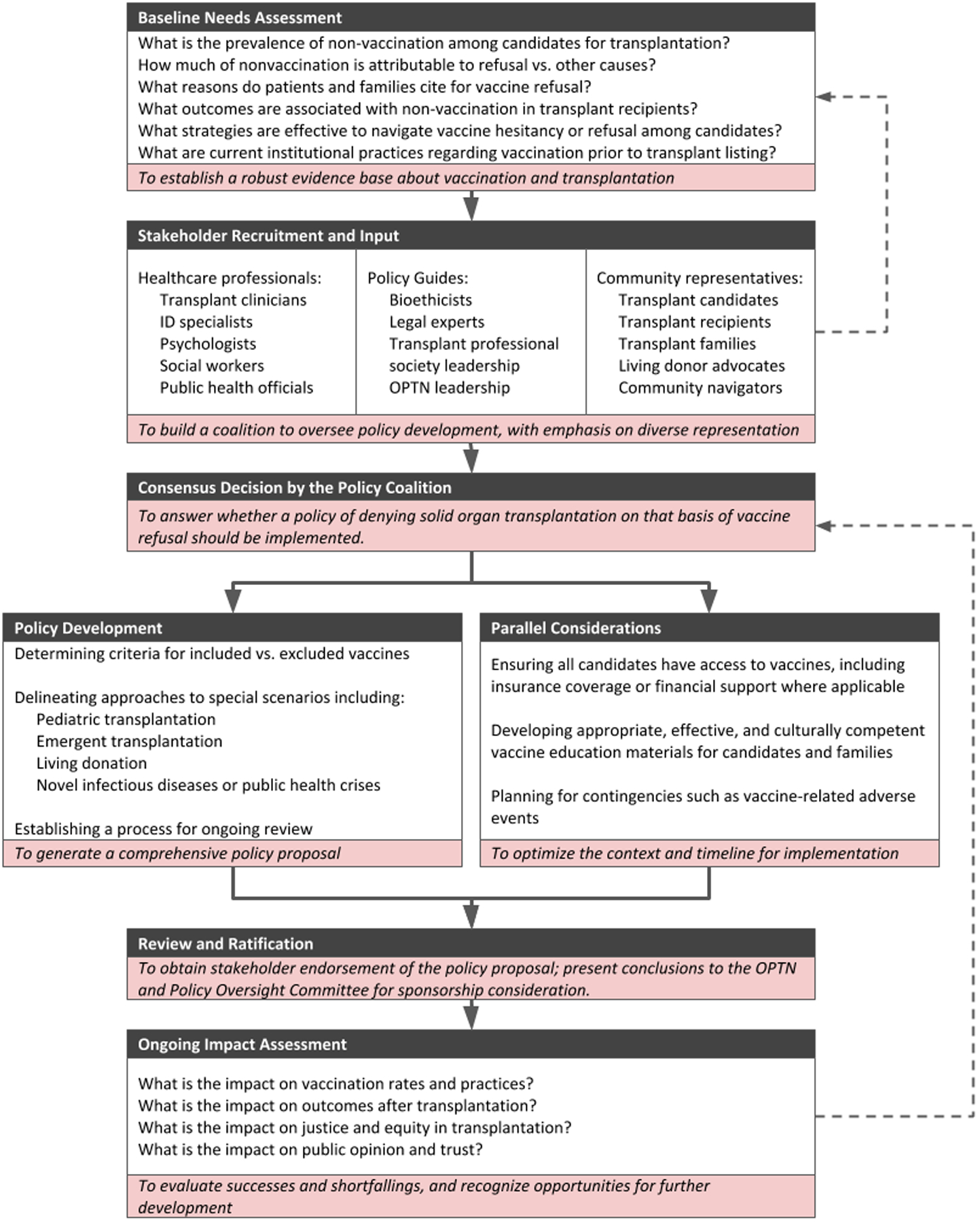
Figure 1 outlines detailed process steps toward the implementation of a uniform policy to address vaccine refusal in solid organ transplant candidates.
Ultimately, a clearly articulated policy could reinforce the importance of vaccination prior to transplantation, guide discussions between transplant teams and candidates, and lead to consistent treatment of all candidates nationally. Given rising rates of vaccine hesitancy and refusal, increasing outbreaks of vaccine-preventable illness, and the recent emergence of a novel infectious threat with SARS-CoV-2, a standardized approach to vaccination for transplant candidates is more important now than ever.43 We call for transplant organizations to consider these ethical arguments and to support and coordinate a policy development process. Preliminary best practices should be implemented immediately while awaiting a consensus policy (Table 3).
Table 3: Preliminary best practices for transplantation when working with non-vaccinated patients.
Table 3 recommends best practices that can be implemented in all centers regardless of institutional policy while awaiting a consensus statement regarding transplant listing for candidates who refuse recommended vaccines.
| Before Transplant |
|
| After Transplant |
|
Recommendations for basic precautions to protect patients from vaccine-preventable illnesses may not be sufficient in the context of widespread disease activity or a novel contagion. These practices do not replace specific recommendations from public health organizations which may include universal masking, physical distancing, or stay at home orders.
Disclosure
The authors of this manuscript have conlficts of interest to disclose as described by the American Journal of Transplantation. Dr. Pergam receives research support from Global Life Technologies, Inc., and participates in research trials with Chimerix, Inc and Merck & Co. He also currently participates in a clinical trial sponsored by the National Institute of Allergy and Infectious Diseases (U01-AI132004); vaccines for this trial are provided by Sanofi-Aventis. Dr. Wolfe reports being a paid member of DSMB for Merk and Jansesen Pharmaceticals, Biogen, and payments to Duke University for clinical research trials by Gilead, Ansum Bio Pharma. Dr. Danziger-Isakov reports being a paid member of DSMB for Merck; personal consulting fees from GSK; payments to Cincinnati Children’s Hopsital Medical Center for clinical research trials by Ansun BioPharma, Astellas, Merck, Takeda, and Viracor. Dr. Ison reports being a paid member of DSMB for NIH, Janssen, Merck, SAB Biotherapeutics, Sequiris, Takeda and Vitaeris; personal consulting fees from AlloVir, Celltrion, Genentech/Roche, Janssen, Shionogi and Viracor Eurofin; payments to Northwestern University by AiCuris, Janssen and Shire for research. The other authors have no conflicts of interest to disclose.
Abbreviations
- ACIP
Advisory Committee on Immunization Practices
- CDC
Centers for Disease Control and Prevention
- OPTN
Organ Procurement and Transplantation Network
Footnotes
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analyzed.
References
- 1.Gillon R Defending the four principles approach as a good basis for good medical practice and therefore for good medical ethics. J Med Ethics. 2015;41(1):111–116. [DOI] [PubMed] [Google Scholar]
- 2.Ethical Principles in the Allocation of Human Organs. Organ Procurement and Transplantation Network. https://optn.transplant.hrsa.gov/resources/ethics/ethical-principles-in-the-allocation-of-human-organs. Updated June, 2014. Accessed October 18, 2019. [Google Scholar]
- 3.General Considerations in Assessment for Transplant Candidacy. Organ Procurement and Transplantation Network. https://optn.transplant.hrsa.gov/resources/ethics/general-considerations-in-assessment-for-transplant-candidacy. Updated January, 2014. Accessed October 18, 2020. [Google Scholar]
- 4.Williams WW, Lu PJ, O’Halloran A, et al. Surveillance of Vaccination Coverage among Adult Populations - United States, 2015. MMWR Surveill Summ. 2017;66(11):1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seither R, Loretan C, Driver K, Mellerson JL, Knighton CL, Black CL. Vaccination Coverage with Selected Vaccines and Exemption Rates Among Children in Kindergarten - United States, 2018–19 School Year. MMWR Morb Mortal Wkly Rep. 2019;68(41):905–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hough-Telford C, Kimberlin DW, Aban I, et al. Vaccine Delays, Refusals, and Patient Dismissals: A Survey of Pediatricians. Pediatrics. 2016;138(3). [DOI] [PubMed] [Google Scholar]
- 7.Benecke O, DeYoung SE. Anti-Vaccine Decision-Making and Measles Resurgence in the United States. Glob Pediatr Health. 2019;6:2333794×19862949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Omer SB, Salmon DA, Orenstein WA, deHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N Engl J Med. 2009;360(19):1981–1988. [DOI] [PubMed] [Google Scholar]
- 9.Danziger-Isakov L, Kumar D. Vaccination of solid organ transplant candidates and recipients: Guidelines from the American society of transplantation infectious diseases community of practice. Clin Transplant. 2019;33(9):e13563. [DOI] [PubMed] [Google Scholar]
- 10.Feldman AG, Sundaram SS, Beaty BL, Torres R, Curtis DJ, Kempe A. Immunization Status at the Time of Liver Transplant in Children and Adolescents. Jama. 2019;322(18):1822–1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ladd JM, Karkazis K, Magnus D. Parental refusal of vaccination and transplantation listing decisions: a nationwide survey. Pediatr Transplant. 2013;17(3):244–250. [DOI] [PubMed] [Google Scholar]
- 12.Chong PP, Avery RK. A Comprehensive Review of Immunization Practices in Solid Organ Transplant and Hematopoietic Stem Cell Transplant Recipients. Clin Ther. 2017;39(8):1581–1598. [DOI] [PubMed] [Google Scholar]
- 13.Rafat C, Klouche K, Ricard JD, et al. Severe Measles Infection: The Spectrum of Disease in 36 Critically Ill Adult Patients. Medicine (Baltimore). 2013;92(5):257–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Aalst M, Lötsch F, Spijker R, et al. Incidence of invasive pneumococcal disease in immunocompromised patients: A systematic review and meta-analysis. Travel Med Infect Dis. 2018;24:89–100. [DOI] [PubMed] [Google Scholar]
- 15.Chin-Hong PV, Reid GE. Human papillomavirus infection in solid organ transplant recipients: Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019;33(9):e13590. [DOI] [PubMed] [Google Scholar]
- 16.Jones JM, Kracalik I, Levi ME, et al. Assessing Solid Organ Donors and Monitoring Transplant Recipients for Human Immunodeficiency Virus, Hepatitis B Virus, and Hepatitis C Virus Infection - U.S. Public Health Service Guideline, 2020. MMWR Recomm Rep. 2020;69(4):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Feldman AG, Sundaram SS, Beaty BL, Kempe A. Hospitalizations for Respiratory Syncytial Virus and Vaccine-Preventable Infections in the First 2 Years After Pediatric Liver Transplant. J Pediatr. 2017;182:232–238.e231. [DOI] [PubMed] [Google Scholar]
- 18.Sternfeld T, Spöri-Byrtus V, Riediger C, et al. Acute measles infection triggering an episode of liver transplant rejection. Int J Infect Dis. 2010;14(6):e528–530. [DOI] [PubMed] [Google Scholar]
- 19.Hope K, Boyd R, Conaty S, Maywood P. Measles transmission in health care waiting rooms: implications for public health response. Western Pac Surveill Response J. 2012;3(4):33–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Istre GR, McKee PA, West GR, et al. Measles spread in medical settings: an important focus of disease transmission? Pediatrics. 1987;79(3):356–358. [PubMed] [Google Scholar]
- 21.Phadke VK, Bednarczyk RA, Salmon DA, Omer SB. Association Between Vaccine Refusal and Vaccine-Preventable Diseases in the United States: A Review of Measles and Pertussis. Jama. 2016;315(11):1149–1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van der Vries E, Stittelaar KJ, van Amerongen G, et al. Prolonged influenza virus shedding and emergence of antiviral resistance in immunocompromised patients and ferrets. PLoS Pathog. 2013;9(5):e1003343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Information About Immune Globulin (Human) Product Shortage. United States Food and Drug Administration. Safety & Availability: Biologics Web site. https://www.fda.gov/vaccines-blood-biologics/safety-availability-biologics/information-about-immune-globulin-human-product-shortage. Updated August 16, 2019. Accessed February 25, 2020. [Google Scholar]
- 24.Gagnon L Infection prevention measures may limit liability. Cmaj. 2008;178(12):1536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jones MU, Carter CG, Cameron KL, Smith TK. The Impact of Vaccine Refusal on Physician Office Visits During the Subsequent 12 Months. Mil Med. 2017;182(9):e1810–e1815. [DOI] [PubMed] [Google Scholar]
- 26.Shickle D The ethics of public health practice: balancing private and public interest within tobacco policy. Br Med Bull. 2009;91:7–22. [DOI] [PubMed] [Google Scholar]
- 27.Notes from the field: measles outbreak among members of a religious community - Brooklyn, New York, March-June 2013. MMWR Morb Mortal Wkly Rep. 2013;62(36):752–753. [PMC free article] [PubMed] [Google Scholar]
- 28.Educational Guidance on Patient Referral to Kidney Transplantation. Organ Procurement and Transplantation Network. https://optn.transplant.hrsa.gov/resources/guidance/educational-guidance-on-patient-referral-to-kidney-transplantation. Updated September, 2015. Accessed July 30, 2020. [Google Scholar]
- 29.Quinn S, Jamison A, Musa D, Hilyard K, Freimuth V. Exploring the Continuum of Vaccine Hesitancy Between African American and White Adults: Results of a Qualitative Study. PLoS Curr. 2016;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Measles Cases and Outbreaks. Centers for Disease Control and Prevention. Measles (Rubeola) Web site. https://www.cdc.gov/measles/cases-outbreaks.html. Updated February 3, 2020. Accessed February 25, 2020. [Google Scholar]
- 31.Gilkey MB, Calo WA, Marciniak MW, Brewer NT. Parents who refuse or delay HPV vaccine: Differences in vaccination behavior, beliefs, and clinical communication preferences. Hum Vaccin Immunother. 2017;13(3):680–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Emanuel EJ. Undue inducement: nonsense on stilts? Am J Bioeth. 2005;5(5):9–13; discussion W18–11, W17. [DOI] [PubMed] [Google Scholar]
- 33.Szmukler G. Compulsion and “coercion” in mental health care. World Psychiatry. 2015;14(3):259–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Caspar EA, Christensen JF, Cleeremans A, Haggard P. Coercion Changes the Sense of Agency in the Human Brain. Curr Biol. 2016;26(5):585–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pridham KM, Berntson A, Simpson AI, Law SF, Stergiopoulos V, Nakhost A. Perception of Coercion Among Patients With a Psychiatric Community Treatment Order: A Literature Review. Psychiatr Serv. 2016;67(1):16–28. [DOI] [PubMed] [Google Scholar]
- 36.General recommendations on immunization --- recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2011;60(2):1–64. [PubMed] [Google Scholar]
- 37.National Vaccine Injury Compensation Program. Health Resources & Services Administration. https://www.hrsa.gov/vaccine-compensation/index.html. Updated November 2020. Accessed November 11, 2020. [Google Scholar]
- 38.Parasidis E, Opel DJ. Parental Refusal of Childhood Vaccines and Medical Neglect Laws. Am J Public Health. 2017;107(1):68–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Woolley S Children of Jehovah’s Witnesses and adolescent Jehovah’s Witnesses: what are their rights? Arch Dis Child. 2005;90(7):715–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schneekloth TD, Niazi SK, Simonetto DA. Alcoholic hepatitis: appropriate indication for liver transplantation? Curr Opin Organ Transplant. 2017;22(6):578–583. [DOI] [PubMed] [Google Scholar]
- 41.Network OPaT. Policy 14: Living Donation. OPTN Policies. 2020;February 2020:276–295. [Google Scholar]
- 42.Network OPaT. Requirements for Living Donor Informed Consent. In. Policies: Health Resources and Services Administration:281–282. [Google Scholar]
- 43.Kates OS, Haydel BM, Florman SS, et al. COVID-19 in solid organ transplant: A multi-center cohort study. Clin Infect Dis. 2020. [Google Scholar]
- 44.Pineda EMZ, Spinner ML, Pallotta A, Koval C, Bollinger J. Infectious diseases pre-transplant evaluation improves vaccination rates for liver transplant candidates. Transpl Infect Dis. 2019;21(5):e13160. doi: 10.1111/tid.13160 [DOI] [PubMed] [Google Scholar]
- 45.Medical Advisory Committee of the Immune Deficiency Foundation, Shearer WT, Fleisher TA, et al. Recommendations for live viral and bacterial vaccines in immunodeficient patients and their close contacts. J Allergy Clin Immunol. 2014;133(4):961–966. doi: 10.1016/j.jaci.2013.11.043 [DOI] [PMC free article] [PubMed] [Google Scholar]


