INTRODUCTION
More than 20 million people in the USA have a substance use disorder (SUD).1 Rising substance-related morbidity and mortality has resulted in increasing emergency department (ED) visits and hospitalizations for substance-related causes.2–4 Prior research has demonstrated the feasibility of utilizing specialized addiction consult teams during hospitalization.5, 6 However, implementation remains uncommon and whether addiction consultation reduces the likelihood of hospital readmission is not known. We sought to evaluate the impact of being seen by an inpatient addiction consult team on 30-day hospital readmission.
METHODS
In 2014, Massachusetts General Hospital (MGH) started an inpatient addiction consult team (ACT) consisting of a rotating group of addiction medicine and psychiatry physicians, advanced practice nurses, social workers, recovery coaches, and trainees. The team focuses on initiating pharmacotherapy, providing brief counseling, aftercare planning, and linking patients directly to SUD treatment following discharge.
For patients ever seen by ACT during a 5-year period (October 2014–2019), we calculated the frequencies of consults, diagnosis codes, and 30-day readmission rates. We separated SUD diagnosis codes for active SUD from those with modifiers noting the patient was in remission. A generalized estimating equation (GEE) analysis was used to compare readmission rates accounting for repeated measures. We determined that the 99th percentile for number of admissions for all patients admitted during the study period was 10. Given the risk that the high number of admissions in this small group could distort the results and that this group may have significant medical comorbidity that would not be modifiable by addiction consultation, we subsequently excluded patients with 10 or more admissions from some analyses.
This study was approved by the Partners Healthcare IRB.
RESULTS
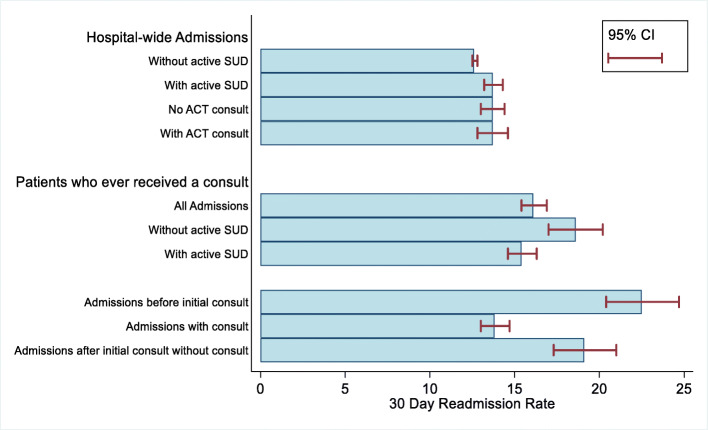
Since 2014, ACT completed consults on 4719 unique patients (Table 1). There were 7489 identifiable hospital admissions which included one or more ACT consults. Of these, 2405 patients were admitted 2 or more times and 217 were admitted 10 or more times. Alcohol and opioid use disorder were the most frequently seen diagnoses. The 30-day readmission rates among patients with active SUD were 22.5% for admissions with active SUD before the first ACT consult, 13.8% for admissions with an ACT consult, and 19.1% for admissions after first ACT consult that did not involve a consult during that current admission (Fig. 1). Among patients who ever received a consult, excluding those with 10 or more admissions, compared with admissions before the first ACT consult, readmission within 30 days was less likely for admissions with an ACT consult (OR 0.57, 95% CI 0.49–0.67) and for readmissions after the first ACT consult that did not include a current ACT consult (OR 0.55, 95% CI 0.46, 0.67). There were no differences in the likelihood of readmission by age, gender, or race/ethnicity.
Table 1.
Patient Characteristics
| All admissions | Admissions with ACT consult | |||
|---|---|---|---|---|
| N | Percent | N | Percent | |
| Admissions | 233,567 | 7489 | ||
| Patients | ||||
| Total | 139,061 | 4719 | ||
| Patients admitted ≥ 2 times | 39,631 | 28.5 | 2405 | 51.0 |
| Patients admitted ≥ 10 times | 943 | 0.7 | 217 | 4.6 |
| Demographics (patient-level) | ||||
| Age (Mean (SD)) | 57.0 (19.2) | 46.7 (13.4) | ||
| Male | 65,469 | 47.1 | 3313 | 70.2 |
| Race | ||||
| White | 107,979 | 77.6 | 3702 | 78.4 |
| Black or African American | 7889 | 5.7 | 339 | 7.2 |
| Hispanic or Latino | 7457 | 5.4 | 326 | 6.9 |
| Asian | 5913 | 4.3 | 43 | 0.9 |
| Other | 3335 | 2.4 | 114 | 2.4 |
| Unknown | 6488 | 4.7 | 195 | 4.1 |
| Discharge disposition | ||||
| Home | 179,374 | 76.8 | 5160 | 68.9 |
| Transferred | 44,691 | 19.1 | 1613 | 21.5 |
| Left AMA | 2209 | 0.9 | 642 | 8.6 |
| Deceased | 7174 | 3.1 | 70 | 0.9 |
| Other | 119 | 0.1 | 4 | 0.1 |
| Active SUD diagnosis | ||||
| Alcohol | 12,688 | 5.4 | 4432 | 59.2 |
| Opioid | 5812 | 2.5 | 2316 | 30.9 |
| Cocaine | 2574 | 1.1 | 1027 | 13.7 |
| Stimulant | 295 | 0.1 | 123 | 1.6 |
| Sedative | 520 | 0.2 | 207 | 2.8 |
| Other/Poly | 1758 | 0.8 | 668 | 8.9 |
| Any SUD diagnosis | 18,618 | 8.0 | 6441 | 86.0 |
| Number of SUD diagnoses (median (IQR)) | 1 (1–1) | 1 (1–2) | ||
| Overdose | ||||
| Opioid | 390 | 0.2 | 153 | 2.0 |
| Other | 129 | 0.1 | 64 | 0.9 |
| 30-day readmission* (rate (95% CI) | ||||
| All admissions | 14.7 (14.6–14.9) | 22.1 (21.4–22.8) | ||
| Patients admitted < 10 times | 12.7 (12.6–12.8) | 16.1 (15.4–16.9) | ||
*Excludes deceased patients
Fig. 1.
30-day readmission rates.
DISCUSSION
In this evaluation of patients seen by an addiction consult team during hospitalization, we found a lower 30-day readmission rate associated with consultation. Compared with admissions before being seen by ACT, receiving an addiction consultation was associated with a reduced 30-day readmission rate. This impact on readmission persisted for subsequent admissions that did not involve ACT. This suggests that the benefits of engagement with ACT may persist; however, ongoing ACT involvement for patients who frequently touch the healthcare system may be beneficial. Reduced readmission may be due to ACT’s facilitation of pharmacotherapy initiation, discharge planning, and linkage to ongoing addiction care which is often integrated with primary care. This is consistent with prior research showing patients with SUD who receive primary care in practices with embedded addiction treatment have lower ED utilization and inpatient hospital bed days than patients in practices without these resources.7
Implementing addiction consult teams does require new resources and funding. The association between consultation and reduced readmission may allow institutions to make a case for the value of this care model in addition to the clinical benefit to individual patients in reducing addiction severity, as shown in previous research.5
There are limitations to this study. The absence of a control group limits comparison to patients who did not receive a consult. Also, our readmission data included only readmissions to our hospital. It is possible patients were readmitted to other hospitals during the study period.
Funding Information
The work represented in the manuscript was funded by Massachusetts General Hospital. In addition, Dr. Wakeman received research support from the National Institutes of Health (1R01DA044526-01A1), the National Institute on Drug Abuse (3UG1DA015831-17S2), the Substance Abuse and Mental Health Services Administration (1H79TI081442-01), the Laura and John Arnold Foundation, and received salary support from OptumLabs as a co-investigator on a research project during the study period.
Compliance with Ethical Standards
Conflict of Interest
Dr. Wakeman received salary support from Optum Labs during the study period.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.: Substance Abuse and Mental Health Services Administration. (2019). Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health (HHS Publication No. PEP19-5068, NSDUH Series H-54). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from https://www.samhsa.gov/data/ on February 3, 2020
- 2.Weiss AJ, Elixhauser A, Barrett ML, Steiner CA, Bailey MK, O’Malley L. Opioid-Related Inpatient Stays and Emergency Department Visits by State, 2009-2014. HCUP Statistical Brief #219. December 2016. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb219-Opioid-Hospital-Stays-ED-Visits-by-State.pdf. [PubMed]
- 3.Centers for Disease Control and Prevention. Annual Surveillance Report of Drug-Related Risks and Outcomes — United States, 2017. Surveillance Special Report 1. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. Published August 31, 2017. Accessed November 20, 2017 from https://www.cdc.gov/drugoverdose/pdf/pubs/2017 cdc-drug-surveillance-report.pdf
- 4.Kariisa M, Scholl L, Wilson N, Seth P, Hoots B. Drug Overdose Deaths involving Cocaine and Psychostimulants with Abuse Potential – United States, 2003-2017. Morb Mortal Wkly Rep. ePub. 3 May 2019. [DOI] [PMC free article] [PubMed]
- 5.Wakeman SE, Metlay JP, Chang Y, Herman GE, Rigotti NA. Inpatient Addiction Consultation for Hospitalized Patients Increases Post-Discharge Abstinence and Reduces Addiction Severity. J Gen Intern Med. 2017;32(8):909–916. doi: 10.1007/s11606-017-4077-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Englander H, Dobbertin K, Lind BK, et al. Inpatient Addiction Medicine Consultation and Post-Hospital Substance Use Disorder Treatment Engagement: a Propensity-Matched Analysis. J Gen Intern Med. 2019;34(12):2796–2803. doi: 10.1007/s11606-019-05251-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wakeman SE, Rigotti NA, Chang Y, et al. Effect of Integrating Substance Use Disorder Treatment into Primary Care on Inpatient and Emergency Department Utilization. J Gen Intern Med. 2019;34(6):871–877. doi: 10.1007/s11606-018-4807-x. [DOI] [PMC free article] [PubMed] [Google Scholar]