Abstract
Background
Substitutive hospital-level care in a patient’s home (“home hospital”) has been shown to lower cost, utilization, and readmission compared to traditional hospital care. However, patients’ perspectives to help explain how and why interventions like home hospital accomplish many of these results are lacking.
Objective
Elucidate and explain patient perceptions of home hospital versus traditional hospital care to better describe the different perceptions of care in both settings.
Design
Qualitative evaluation of a randomized controlled trial.
Participants
36 hospitalized patients (19 home; 17 control).
Intervention
Traditional hospital (“control”) versus home hospital (“home”), including nurse and physician home visits, intravenous medications, remote monitoring, video communication, and point-of-care testing.
Approach
We conducted a thematic content analysis of semi-structured interviews. Team members developed a coding structure through a multiphase approach, utilizing a constant comparative method.
Key results
Themes clustered around 3 domains: clinician factors, factors promoting healing, and systems factors. Clinician factors were similar in both groups; both described beneficial interactions with clinical staff; however, home patients identified greater continuity of care. For factors promoting healing, home patients described a locus of control surrounding their sleep, activity, and environmental comfort that control patients lacked. For systems factors, home patients experienced more efficient processes and logistics, particularly around admission and technology use, while both noted difficulty with discharge planning.
Conclusions
Compared to control patients, home patients had better experiences with their care team, had more experiences promoting healing such as better sleep and physical activity, and had better experiences with systems factors such as the admission processes. Potential explanations include continuity of care, the power and familiarity of the home, and streamlined logistics. Future improvements include enhanced care transitions and ensuring digital interfaces are usable.
Trial Registration
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-020-06416-7.
KEY WORDS: home hospital, hospital at home, hospital alternative, hospital experience, qualitative, home-based care
INTRODUCTION
Hospitals are the standard of care for acute illness in the USA, but hospital care is expensive and potentially unsafe and uncomfortable, particularly for older individuals.1,2 “Home hospital” care delivers acute hospital-level care in a patient’s home as a substitute for the traditional hospital.3 Prior quantitative work suggests home hospital can reduce cost, maintain quality and safety, and improve patient experience for select acutely ill adults who require traditional hospital-level care.4–13 However, robust evidence to explain how and why home hospital accomplishes many of these results is lacking.
Though prior studies have noted cost and other benefits to home hospital, those that studied patient experience have been mixed and were limited by reports of acceptability,14 quantitative evaluations,15 or lack of a randomized comparator.16,17 A global experience measure and patient experience scale used for inpatients did not demonstrate a difference between home hospital and traditional hospital in a recent randomized controlled trial.18 This quantitative evaluation leaves an incomplete view with significant gaps in our understanding of the complex lived realities of patients who receive acute home hospital care. A robust qualitative study of patient experience is necessary to explore and potentially explain the mechanisms by which home hospital improves outcomes, but also to provide lessons for future efforts to improve and disseminate such programs. To best elucidate the inner workings of home hospital, we report a qualitative evaluation of home hospital compared to usual hospital care.
METHODS
Study Design
We previously reported quantitative findings from the first pilot randomized controlled trial (RCT) in the USA of home hospital19 and subsequent replication in a larger population.18 During both RCTs, we prospectively performed a qualitative evaluation of patient experience in both the home hospital (“home”) and traditional hospital (“control”) arms.
We conducted our pilot RCT between September 12, 2016, and November 13, 2016, and followed this with replication in a larger RCT between June 12, 2017, and January 16, 2018, at Brigham and Women’s Hospital (an academic medical center) and Brigham and Women’s Faulkner Hospital (affiliated community hospital). This investigator-initiated study was approved by the Partners HealthCare IRB and registered at clinicaltrials.gov (NCT03203759). All participants provided written informed consent.
Participants and Randomization
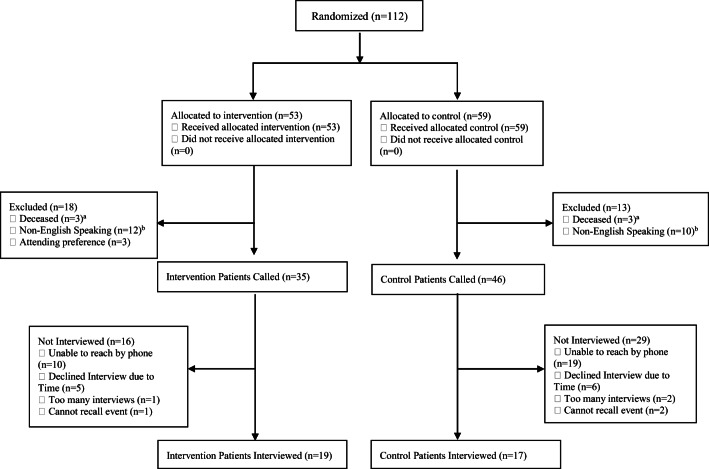
We previously described selection criteria in detail.18 Briefly, adult participants were recruited in the emergency department (ED) and were eligible for inclusion based on their home’s geographic location, their illness type (general medical condition such as infection and heart failure exacerbation), and their functional status (able to ambulate to a bedside commode). Participants could live alone. Participants were only approached for enrollment following determination by the ED that admission was necessary. After meeting the criteria and providing written informed consent, participants were randomized to home or control (Fig. 1). All patients who enrolled prospectively consented to a qualitative interview that would be conducted after discharge by telephone. We attempted to contact all living patients without dementia or a disorder that would prevent them from speaking on the phone (e.g., cognitive delay or vocal cord paralysis) irrespective of thematic saturation (Fig. 1).
Figure 1.
Participant flow. aSome patients passed away following discharge prior to their interview being performed. bSome Spanish-speaking patients were excluded due to the intermittent availability of a Spanish-speaking interviewer.
Home Hospital Intervention
We previously described the home hospital intervention in detail.18 Briefly, all patients received at least one daily visit from an attending general internist and two daily visits from a registered nurse (Partners HealthCare at Home), with additional visits performed as needed. Also tailored to patient need, participants could receive medical meals and the services of a home health aide, social worker, physical therapist, and/or occupational therapist.
Home hospital could provide most of the acute-care services expected of a traditional hospital, including respiratory therapies (e.g., oxygen), intravenous medications (Smiths Medical, St. Paul, MN), imaging studies, and continuous monitoring (VitalConnect, San Jose, CA). We mandated no treatment pathways or algorithms. Urgent responses could occur in less than 20 min and a return to hospital could occur on a case-by-case basis.
Participants randomized to the control group received usual care in the hospital from an attending general internist (usually a hospitalist) or cardiologist.
Qualitative Procedures
Interview Guide Development
We developed a semi-structured interview guide informed by prior clinical experience delivering home hospital and traditional hospital care, gaps in understanding left by quantitative experience evaluations of home hospital care, and discussions with patients and clinicians.14–17 The interview guide focused on the patient’s perspectives and experiences with her/his own wellness and the clinicians and caregivers supporting that wellness. By design, it asked broad, open-ended questions that could be further probed as needed, focusing on interactions with clinicians; fears, surprises, and difficulties during hospitalization; burden placed on caregivers; and improvements that ought to be made. It was also written such that it applied to both home and control patients without major adaptation. The final interview guide was constructed after pilot testing with 5 standardized patients (DML) resulting in vocabulary simplification for goal interview length of 15 min to limit participant burden (eAppendix).
Data Collection
All interviews were audio-recorded and then transcribed in a HIPAA-compliant manner. Patients’ caregivers could be present via speakerphone if applicable and desired by the patient. Patients were told the interview was to examine their experience with the care they received during their admission. They did not have a prior relationship with the interviewer and were not told interviewer characteristics. Interviews were conducted by phone from October 30, 2016, to March 6, 2018, by trained qualitative interviewers (AP: MSW, research assistant, female; AS: MD, attending physician, female; JP: medical student, female). Due to the intermittent availability of trained Spanish-speaking interviewers (AP and AS), English-speaking patients were interviewed more frequently.
Qualitative Analysis
We performed a thematic content analysis. Our analytic approach borrowed from grounded theory, which involves open coding (comparing and conceptualizing the data), followed by axial coding (forming groupings based on relationships in the data), and then finally selective coding (describing central themes). Because our participants were divided into intervention and control groups, we analyzed responses via the constant comparative method.20,21 A codebook was developed based on the first 5 interviews and subsequently refined throughout the coding process to create domains and subdomains. For subdomains noted in small frequencies, we only note representative quotes in tabular form. Two investigators coded each interview (JP and KM) with oversight (DL) using qualitative analysis software (NVivo 12, version 12.2.0). Any discrepancies in coding were discussed and finalized by consensus. We followed the EQUATOR network’s consolidated criteria for reporting qualitative research.
RESULTS
Patient Characteristics
Of 112 randomized patients, 81 patients were eligible. We were able to contact 36 for an interview (duration range: 3.4 to 22.5 min), including 19 home and 17 control patients (Fig. 1). Twenty-nine (36%) participants were unable to be reached by phone and 14 (17%) patients reached for an interview declined. No statistically significant sociodemographic differences existed between those who were and were not interviewed, although those interviewed trended toward having less education but similar health literacy (Table 1).
Table 1.
Patient Characteristics
| Interviewed | Not interviewed | |||
|---|---|---|---|---|
| Home (n = 19) | Control (n = 17) | All (n = 36) | All (n = 45) | |
| Age, years, median (IQR) | 77 (24) | 75 (21) | 76 (23) | 67 (29) |
| Female, n (%) | 10 (53) | 10 (59) | 20 (56) | 29 (64) |
| Race/ethnicity, n (%) | ||||
| White | 9 (47) | 11 (65) | 20 (56) | 29 (64) |
| Black | 6 (32) | 3 (18) | 9 (25) | 9 (20) |
| Latino | 2 (11) | 2 (12) | 4 (11) | 6 (13) |
| Asian | 2 (11) | 1 (5.9) | 3 (8.3) | 0 (0) |
| Other | 0 (0) | 0 (0) | 0 (0) | 1 (2.2) |
| Partner status, n (%) | ||||
| Partnered | 9 (47) | 7 (41) | 16 (44) | 18 (41) |
| Divorced | 5 (26) | 1 (5.9) | 6 (17) | 5 (11) |
| Widowed | 1 (5.2) | 3 (18) | 4 (11) | 7 (16) |
| Single, never partnered | 4 (21) | 5 (29) | 9 (25) | 13 (29) |
| Other | 0 (0) | 0 (0) | 0 (0) | 2 (4.4) |
| Primary language, n (%) | ||||
| English | 17 (89) | 16 (94) | 33 (92) | 42 (93) |
| Spanish | 2 (11) | 1 (6) | 3 (8) | 3 (7) |
| Insurance, n (%) | ||||
| Private | 9 (47) | 7 (41) | 16 (44) | 17 (38) |
| Medicare | 6 (32) | 9 (53) | 15 (42) | 18 (40) |
| Medicaid | 1 (5) | 0 (0) | 1 (3) | 5 (11) |
| Medicare + Medicaid | 0 (0) | 2 (12) | 2 (5) | 6 (13) |
| None | 4 (21) | 0 (0) | 4 (11) | 0 (0) |
| Education, n (%) | ||||
| < High school | 4 (21) | 3 (18) | 7 (19) | 8 (18) |
| High school | 2 (11) | 7 (42) | 9 (25) | 16 (35) |
| < 4-year college | 6 (32) | 0 (0) | 6 (17) | 8 (18) |
| 4-year college | 2 (11) | 3 (18) | 5 (14) | 8 (18) |
| > 4-year college | 5 (26) | 4 (24) | 9 (25) | 4 (9) |
| Employment, n (%) | ||||
| Employed | 8 (42) | 5 (29) | 13 (36) | 12 (27) |
| Unemployed | 1 (5.2) | 3 (18) | 4 (11) | 6 (13) |
| Retired | 10 (53) | 9 (53) | 19 (53) | 26 (58) |
| Cigarette smoking, n (%) | ||||
| Never | 10 (53) | 11 (65) | 21(58) | 19 (42) |
| Current | 2 (11) | 2 (12) | 4 (11) | 6 (13) |
| Prior | 8 (42) | 4 (21) | 12 (33) | 20 (44) |
| PRISMA (0–7), median (IQR) | 4 (3) | 3.5 (2.3) | 3.5 (3) | 3 (3.3) |
| Ascertain dementia-8 (0–8), median (IQR) | 0 (3) | 2 (2.5) | 1 (3) | 0.5 (3) |
| Health literacy (4–20), median (IQR)a | 16.5 (12) | 17 (8) | 18.5 (8) | 15 (7) |
| Comorbidity count, median (IQR)b | 7 (10) | 7.5 (5) | 7 (7.5) | 7 (8) |
| Code status: full code, n (%) | 14 (74) | 15 (88) | 29 (81) | 35 (78) |
| Yes, surprised if died in 1 year, n (%) | 11 (58) | 12 (71) | 23 (64) | 32 (71) |
| EuroQol VAS (0–100), mean (95% CI) | 64 (55,74) | 59 (48,71) | 62 (54,69) | 62 (57,68) |
| ADLs on admission (0–6), median (IQR) | 6 (5) | 6 (5) | 6 (5) | 4 (5) |
| IADLs on admission (0–8), median (IQR) | 4 (6.5) | 5 (7) | 4.5 (7) | 4.5 (7) |
| PHQ-2 (0–6), median (IQR) | 0 | 0 | 0 | 0 |
| PROMIS emotional support (4–20), median (IQR) | 20 (12) | 20 (8) | 20 (8) | 18 (7) |
| Hospital admission in last 6 months, n (%) | 5 (26) | 8 (47) | 13 (36) | 30 (67) |
| Emergency department visit in last 6 months, n (%) | 13 (68) | 12 (71) | 25 (69) | 27 (60) |
| Number outpatient medications, mean (95% CI) | 10.47 (4.35) | 11.23 (3.77) | 10.83 (2.72) | 11.33 (3.01) |
| Diagnosis, n (%)c | ||||
| Infection | ||||
| Pneumonia | 3 (16) | 5 (29) | 8 (22) | 20 (35) |
| Skin/soft tissue infection | 5 (26) | 1 (6) | 6 (17) | 7 (16) |
| Complicated UTI/pyelonephritis | 1 (5) | 2 (12) | 3 (8) | 4 (9) |
| Diverticulitis | 0 (0) | 4 (24) | 4 (11) | 8 (18) |
| Heart failure | 4 (21) | 2 (12) | 6 (17) | 14 (31) |
| Airway disease | ||||
| Asthma | 1 (5) | 0 (0) | 1 (3) | 3 (7) |
| COPD | 4 (21) | 0 (0) | 4 (11) | 7 (16) |
| Other | 1 (5) | 3 (18) | 4 (11) | 16 (36) |
aBrief health literacy screener, 4–12: limited; 13–16: marginal; 17–20: adequate23
bCount of patient’s chronic comorbidities
cDiagnoses were block randomized at the level of infection, heart failure, airway disease, and others. Diagnoses made by the home or control physician. Other diagnoses included complications of diabetes, anticoagulation needs, gout exacerbation, and others
No statistically significant differences (p < 0.05) existed between those who were and were not interviewed nor between interviewed home and control patients
Abbreviations: ADLs, activities of daily living; CI, confidence interval; COPD, chronic obstructive pulmonary disease; IADLs, instrumental activities of daily living; IQR, interquartile range; PHQ-2, Patient Health Questionnaire-2 (measure of depression); PRISMA, Program of Research to Integrate Services for the Maintenance of Autonomy (measure of frailty); PROMIS, Patient-Reported Outcomes Measurement Information System; UTI, urinary tract infection; VAS, Visual Analog Scale
Interviewed home patients had a median age of 77 (interquartile range, 24) and were 53% female, 47% White, and 32% Medicare recipients, and 26% had been hospitalized in the past 6 months (Table 1). Interviewed control patients were not statistically different but trended toward a higher percentage of White patients (65%), higher percentage of Medicare (53%), and a higher percentage of hospitalization in the last 6 months (47%).
Qualitative Domains
Three predominant qualitative domains emerged in which patients expressed varying views on their perceived experience: (1) clinician factors, (2) factors promoting healing, and (3) systems factors (Table 2). Clinician factors encompassed participant perceptions of the availability, continuity, and expertise of the care team as well as their interpersonal and communication skills. Perspectives pertaining to social support, comfort, safety, physical activity, and sleep—all factors patients described as crucial to their healing—were included in factors promoting healing. Systems factors included logistics associated with admission, transfer, discharge, and access to care. Across all domains, home patients, compared to control patients, described more unified communication, continuity of care, a locus of control, and simplified logistics. We noted large differences for factors promoting healing, with benefits at home associated with a general locus of control surrounding one’s sleep, activity, nutrition, stress, and environmental comfort. Each domain is further explored below.
Table 2.
Domains, Subdomains, and Illustrative Quotes
| Domain | Subdomain | Description | Example |
|---|---|---|---|
| Clinician factors promoting quality patient care | Experience with physicians | Content related to experiences with physicians that impact the quality of patient care (e.g., response time, patient education, perception of MD) | “Oh, Dr. X seems to be a great doctor and he was very caring, very understanding, he helped us and totally helped make sure that the patient was comfortable. He was very polite and very, very delicate for his work. I recommend him also. In the future I would deal with him as well, you know, and the program available to my mom so he can be part of my mom’s care.” (home, participant 16) |
| Experience with nurses | Content related to experiences with nurses that impact the quality of patient care (e.g., response time, patient education, perception of RN) | “The nurses were real good. The nurses and the aides. You know, they answered all of our questions or if we wanted something for our mother, they would get it for her. And they were very helpful and knowledgeable.” (home, participant 16) | |
| Experience with other patient care team members | Content related to experiences with support staff that impact the quality of patient care | “They were very informative about every step of the process of what I could expect, who was coming to get me, what was happening, what I could expect when we got to the house” (home, participant 9) | |
| Patient experience factors to promote healing | Sleep | Content related to quality of sleep | “You know I was sleeping in my own bet. So you can’t pop back. I got one of those tempur-pedic mattresses. You don’t have those at the hospital?” (home, participant 8) |
| Burden | Content related to burden to patient family/friend or other caregivers | “The only thing is that because my dedication is like 24 hours, and I have to be here with my mom on a 24-hour basis, and the reason for it is that she knows me well, she trusts me and I did everything for her.So it affect me in some way by, um, I have to be here at all times.” (home, participant 16) | |
| Nutrition | Content related to patient’s nutrition intake, nutrition education, etc. | “Well, ah, well it’s difficult cooking. You know, if I have to get up and cook, it’s difficult for me to stand because of my back problem. That is a difficult thing.” (home, participant 20) | |
| Activity | Content related to patient’s level of activity. | “Umm, I was able to move around the house. It was just before Thanksgiving, so my husband and I, we fixed Thanksgiving dinner, not a big one, a small one, so I was able to do a lot.” (home, participant 19) | |
| Stress | Content related to patient’s level of stress. | “You get a little bit more relaxed and you’re a little bit more able to deal with what’s going on when you’re at home, so I would definitely suggest to anybody that if they have the opportunity to take it.” (control, participant 25) | |
| Pain | Content related to pain and discomfort (+ is absence of pain/discomfort and − is pain/discomfort) | “Well, during my visit there and my stay, it was okay. They gave me medicine on a schedule so I didn’t get pain.” (control, participant 36) | |
| Social Support | Content related to social support (e.g., patient family’s ease of access to patient) | “I really have no difficulties at all and my families is close by. I don’t want to have to lift anything heavy… Uh, my son and his wife and granddaughter are close by. My wife was close by and we have our tenants, um, because we give him a little reduced in the rent. He takes care of all the snow shoveling and gardening so we don’t worry about that.” (home, participant 8) | |
| Safety | Content related to patient’s perception of safety/receiving effective medical care | “First of all because it saves us from getting, you know, any kind of disease from other people being in the hospital is not the best idea.” (home, participant 14) | |
| Environment comfort | Content related to patient’s perception of the comfort of the environment in which they are receiving care | “And uh, you feel more comfortable. It’s just a remarkable feeling to be in your own home.” (home, participant 14) | |
| Systems factors | Admission factors | Content related to factors that promoted a smooth admission | “So I am sitting in the emergency room absolutely, you know, with convolutions and they are looking at me, well, we’ll get to you, you know, it’s like okay.” (control, participant 30) |
| Cultural considerations | Content related to culturally relevant care | “I was mostly worry about the house—being clean and you know like welcoming people. Physicians and nurses in my house and they have stuff organized and neat. That was my primary concern you know worry.” (home, participant 3) | |
| General attitudes | Content related to the attitude around care in the hospital/hospital admission | “I mean, it’s a great program and my experience, I understand better, I understand how everything works. I recommend the program to many, many, many elderly people who are entrusted to have this kind of program available better.” (home, participant 16) | |
| Experience with technology | Content related to experiences with technology that impact the quality of patient care | “ow quickly the information that they found when I explained, when the doctors were here I had a like an anxiety attack. And he said that, umm, you know, that he could see how long it took for my hot flash to be calmed down, he was monitoring me the whole time. So that was really fascinating.” (home, participant 19) | |
| Experience with facility | Experience with facility factors | “The pillows, you know, the pillows are hard and not the kind of pillows she likes to sleep with and she’s got neck problems and it is always hard to get her neck comfortable.” (control, participant 32) | |
| Discharge planning | Content related to patient’s perception of discharge planning and post-admission care | “[Y]eah, you could um have a list of places where I could obtain um medications and other supplies.” (home, participant 5) | |
| Logistical ease | Content related to patient’s perception of the logistical ease of receiving effective medical care | “[I]t’s very convenient to me, and I don’t have to spend the time to travel back and forth to the hospital and it’s really good for me. You know, if I have to go to the hospital, they release me, but then they will tell me what time would come back, tomorrow, day after tomorrow, then I will travel everyday to the hospital, sometime you get into traffic and all the time you waste a lot of time you know.” (home, participant 6) |
Clinician Factors
Overall, clinician factors were similar in both groups, except home patients identified greater continuity of care. Both groups noted generally positive experiences with their clinicians, but they were more often positive in the home group, including their experiences with physicians, nurses, and other staff. Conversely, the home group had fewer negative comments regarding their physicians, nurses, and other staff (Table 2).
Numerous home patients praised the physicians’ ability to adapt to both the patient and environment’s unique requirements: “The doctors were able to kind of think on their feet for me and kind of make sure that the services were a little bit tailored to my needs” (home, participant 1). In addition, patients appreciated the physicians’ availability: “I was happy with him, you know, he was available any time that I called him and you know if he needs to come in for anything, he was more than happy. And [I was happy] that I have that kind of relationships with a physician to the point that you know I could reach out any time in the moment” (home, participant 3).
The reaction to physicians among control patients was weighted toward the positive: “wonderful, they were very responsive and helpful” (control, participant 24), with some patients impressed with the frequency with which they interfaced with the physicians: “literally, checking on me like 3 times a day. I mean, that’s crazy” (control, participant 31). However, a few hospital patients felt that the doctors could have communicated better and facilitated more efficient care: “[they say] we’re gonna send you down for this test and that test … this whole thing about ‘they’ll be right here’ was sort of funny because right here in hospital speak means you’re lucky if someone comes in an hour” (control, participant 30).
Results were similar for experiences with nurses. Home patients noted a preference for the consistency of nursing: “…[I] didn’t have the issue of different nurses on different shifts and on different days, so there was a continuity of care that was comforting” (home, participant 2). Overall, many home patients found: “both the doctor and the nurse were very informative, very patient, very caring, and quick with their visits; but they were also very available for answers to any of my questions” (home, participant 9).
The reaction to nurses among control patients was mostly positive, with patients especially noting the convenience of having constant proximity: “I had nurses around. Anything I needed, I got” (control, participant 21) and: “They were very, very attentive” (control, participant 22). On the other hand, some control patients wished for greater attentiveness: “I have noticed that nurses are very chatty, even when people need them…[there is] an air of informality and the air of almost holding up social relationships with one another above their patients” (control, participant 27).
Factors Promoting Healing
Home patients described more factors promoting healing compared to control patients in each subdomain. Home patients had more positive comments about sleep. They emphasized the value of being in their own environment: “You know, I was sleeping in my own bed. You can’t top that” (control, participant 20). Control patients repeatedly commented on interrupted sleep: “It’s busy; they wake you up every hour on the hour at night. It’s not conducive to relaxation” (home, participant 1), the physical discomforts of a hospital bed: “the pillows are hard and not the kind of pillows I like to sleep with” (control, participant 32), and how ultimately the environment was just not the same as home: “I don’t like being away from home…I’m not a good sleeper. I barely slept when I was in the hospital” (control, participant 21).
Most references to physical activity were positive from home patients and negative from control patients. Home patients described their ability to do their daily activities: “I was able to do everything at home, you know like I tried to relax a little bit, but I was able to wash the dishes, do some laundry” (home, participant 3) and their ability to roam around their usual environment: “At least, I was here. I was not, you know, confined while I was at home, [I could] do what I wanted to do” (home, participant 15). Control patients described activity that was confined to stationary pursuits: “Well, I read, it was okay” (control, participant 34), if at all: “Oh, I didn’t have any activity” (control, participant 28).
Home patients cited improved social support from family compared to control patients. For example, home patients stated that their family and friends “were able to visit me much easier,” (home, participant 1) but a few noted that some of their family members were “a little bit more burdened” (home, participant 8) by the home hospitalization. Control patients, however, also cited increased burden on their family members, both financially: “it’s very expensive when they come for the day” (control, participant 20) and physically: “challenging for loved ones to sleep in a cot all night and to sit in that chair all night, destroyed my neck” (control, participant 31).
Environmental comfort was nearly entirely positive for home patients and often negative for control patients. Home patients repeatedly mentioned the positive effects of familiarity: “I could watch my own television and you know holler at the garbage man for throwing my lid—you know all the stuff you like to have at home” (home, participant 1) and the generally calmer environment of home: “just the general ambiance of being at home as opposed to being in a hospital that tends to be noisy, busy, and with a lot of activity going on” (home, participant 2). Control patients repeatedly expressed the notion that the hospital was different: “it just wasn’t home” (control, participant 20) citing in particular the disruptive noises and lack of privacy: “I got everyone coming in and buzzing and everything” (control, participant 23).
Patients reported similarly positive perceptions of safety. Home patients cited the continuous vitals monitoring, physical distancing from other infectious patients: “it saves us from getting…any kind of disease from other people” (home, participant 14), and feeling as if they: “could call [the care team] anytime” (home, participant 10) as reasons for feeling safe. However, some home patients expressed doubts about the program’s safety in the case of more serious illness or in the case of a patient with less social support (Table 2). Control patients noted the proximity to care they were guaranteed by staying in the hospital: “The nurses were there, the doctors were there, so if anything happened, you know, it would be quick” (control, participant 35).
Systems Factors
For systems factors, home patients noted more efficient processes and logistics, particularly around admission and with technology use, although all patients noted difficulty with discharge. Admission (i.e., physical transfer from the ED) for home patients had a positive perception compared to control patients. Home patients noted a seamless process: “Their approach and their explanation of the program was smooth… It was nice too that they gave me a ride home in an ambulance” (home, participant 1). Control patients were mostly negative about the amount of time that it took to be transferred from the ED to the floor: “The ED was the worst part of my stay. You know laying around there for 10 hours was not easy” (control, participant 21). A small group of home patients noted embarrassment that their home was: “too messy” (home, participant 3).
Home patients expressed more positivity about their experience with technology, compared to control patients. Home patients were generally enthusiastic about the use of the wireless skin patch for vitals monitoring: “I really like that they had me on the monitor so if anything was going on I had the capacity to call them and… they knew what my heart rate was, my respirations so they always had a pretty good check on my health. So I thought that was really comforting” (home, participant 1). The ease of communication with advanced technological tools was also viewed positively by home patients: “The problem came up; I was immediately able to directly communicate with the doctor” (home, participant 2).
Logistical efficiency was cited more by home patients than control patients. For instance, home patients often expressed surprise at how quickly care providers appeared at their home: “The doctor said ‘I’ll see you soon.’ I thought [since the doctor was] at the hospital it would be at least an hour, but he was there” (home, participant 1). Control patients cited lack of general efficiency in the hospital, due to long wait times and many administrative processes: “hospitals, as far as I’m concerned, are not efficient” (control, participant 30).
Both home and control patients noted difficulties with the discharge process, citing difficulty carrying out the proposed plan after discharge. One home patient had trouble obtaining medication and another wished that they had medical care for a day longer. Control patients faced similar problems with the added issue of adjusting to a new environment and health care routine: “you had to learn stuff, how to do this and that, and medications and when to give them to her, the right dosage and so on” (control, participant 35).
DISCUSSION
In this qualitative analysis of patients enrolled in a randomized controlled trial comparing a home hospital program with standard inpatient care, we found that home patients had better experiences with their care team, had more experiences promoting healing such as better sleep and physical activity, and had better experiences with systems factors such as the admission processes. Our work builds on others who have examined the inner workings of home hospital care.14 Prior quantitative studies found home patients reported improved communication and valued the home as treatment location.15,16 Qualitative interviews of home patients in Switzerland also corroborate our findings surrounding safety concerns based on the severity of illness, although these interviews occurred in a time when remote patient monitoring and video technology were not available.22 Our analysis identified clear subdomains where home patients had improved experience, yielding insights into how home hospital may achieve its positive quantitative outcomes.
Both groups described excellent interaction with their care team, although home patients noted more meaningful connections. Several possibilities may explain this. First, interacting with a patient in the home affords the clinician an opportunity to tailor care to a patient’s lived experience more easily than in the hospital. Second, home hospital clinicians were more available whether by video, telephone, or in the home. Patients had direct access to their home hospital clinicians at all hours of the day, compared with a call button and an unclear wait for assistance. Third, there was generally more continuity of nursing care with home hospital, leading to less loss of information and perhaps greater trust.
Home patients experienced more factors promoting healing, revolving around their improved locus of control while home. Patients at home appeared more satisfied with their sleep, physical activity, stress levels, social support, and environmental comfort. Many of these benefits likely stemmed from being in one’s home. Home hospital design principles augmented this: low-profile technology, visits scheduled around the patient not the clinical team, and tailored supports such as a home health aide. In contrast, some home patients were concerned about safety. A small number of patients who were satisfied with their home experience questioned whether, had they been sicker, home hospital would have been safe. They noted that social support, whether in the form of family or an aide provided by home hospital, was important to ensuring safety.
Home patients noted improved experience with systems factors. Home patients had better experiences with their admission, as they were often quickly transferred home from the ED, compared to a long wait for a hospital bed. When care was delivered at home, patients noted that logistics worked better, likely because all care by default had to revolve around their home, as opposed to around teams in the hospital. Although mostly positive, some negative comments existed regarding patients’ experience with technology. The home hospital’s technology had been specifically designed for use with older adults of low health literacy, but some patients still struggled. Discharge planning and the days following discharge were in general negative experiences for both groups. This reflects that care plan changes may be challenging for patients and families and that anticipated services following hospitalization may not come to fruition as planned.
These findings allow for clear recommendations for future home hospital efforts. In the domain of clinician factors, home hospital programs should work to preserve the home-based touch, continuity, and constant availability afforded to patients. Balancing these principles with desire for scale-up may be challenging. Regarding factors promoting healing, home hospital programs should carefully select patients for acuity and social support and be able to supplement support when necessary. Attention to caregiver burden should be a key aspect to assessing appropriate social support. For system factors, our findings suggest that additional user experience testing is necessary and recommended for all home-based technologies. Finally, efforts should focus on improving care transitions back to the community, taking full advantage of the home to customize the discharge plan. Key elements include additional training in supplies, medications, and warm handoffs with a visiting nurse or caregiver. Optimizing the home hospital’s role in the physical, social, and economic structures at home is crucial, as the home hospital team can bring a multidisciplinary approach that gives voice to the patient’s issues often hidden for control patients. Some home hospital programs have chosen to improve transitions by continuing to follow patients for 30 days after discharge in a less acute manner.13 All of these interventions require further investigation.
Our study has limitations.18 First, we enrolled patients at 2 sites in Boston, limiting generalizability. We were not able to interview as many patients who preferred Spanish or other languages due to limited Spanish-speaking interviewers. Although our patients were from diverse racial/ethnic backgrounds, our sample may not reflect the experiences of other patient cohorts. Second, we did not interview clinicians or family members (we recorded family member input when offered). These individuals may offer insights on mechanisms of better care complementary to those noted by patients (and/or conversely, caregiver burden). Third, many patients declined to enroll in home hospital. This biased our findings toward patients who were comfortable with the idea but accurately reflects the perspective of patients willing to engage in home hospital. Fourth, it was not possible to blind coders to the study arm, potentially introducing bias. Fifth, our study was not designed to address the optimal severity of illness that would benefit from home hospital.
CONCLUSIONS
In this qualitative analysis of patients enrolled in a randomized controlled trial comparing acute hospital-level care at home with standard inpatient care, we found that patients treated at home had better experiences with their care team, more experiences promoting healing due to their surroundings, and better interaction with the logistics of the health care system from admission to discharge. Beneficial mechanisms included continuity of care, the power and familiarity of the home, and streamlined logistics. Future improvements include care transitions after discharge, managing caregiver burden, and ensuring usability of digital interfaces for older and low-literacy adults.
Supplementary Information
(DOCX 16 kb)
Acknowledgments
The authors would like to acknowledge the clinicians who cared for all of the patients in this study during their time of need.
The authors also graciously acknowledge the various departments at Brigham Health who were instrumental to the success of the home hospital program: Cardiology, Emergency Medicine, General Internal Medicine and Primary Care, Hospital Medicine Unit, Pharmacy, Laboratory, and Population Health.
Funding
The study was supported by Brigham and Women’s Hospital President’s Fund.
Compliance with Ethical Standards
Conflict of Interest
Dr. Levine is a recipient of funding from Biofourmis for an investigator-initiated study of machine learning warning scores for acutely ill patients, both traditionally and home hospitalized.
Dr. Schnipper is a recipient of funding from Mallinckrodt Pharmaceuticals for an investigator-initiated study of opioid-related adverse drug events in post-operative hospitalized patients.
All other authors declare that they do not have a conflict of interest.
Disclaimer
None of the study’s commercial vendors participated in design, analysis, interpretation, preparation, review, or approval.
Footnotes
Prior Presentations
Society of General Internal Medicine—National conference; Washington, DC, 2019
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.FastStats - Health Expenditures. Accessed December 3, 2018. https://www.cdc.gov/nchs/fastats/health-expenditures.htm
- 2.Hung WW, Ross JS, Farber J, Siu AL. Evaluation of the Mobile Acute Care of the Elderly (MACE) service. JAMA Intern Med. 2013;173(11):990–996. doi: 10.1001/jamainternmed.2013.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leff B. Defining and disseminating the hospital-at-home model. CMAJ. 2009;180(2):156–157. doi: 10.1503/cmaj.081891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leff B, Burton L, Mader SL, et al. Hospital at home: feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005;143(11):798–808. doi: 10.7326/0003-4819-143-11-200512060-00008. [DOI] [PubMed] [Google Scholar]
- 5.Cryer L, Shannon SB, Van Amsterdam M, Leff B. Costs for “hospital at home” patients were 19 percent lower, with equal or better outcomes compared to similar inpatients. Health Aff (Millwood). 2012;31(6):1237–1243. doi: 10.1377/hlthaff.2011.1132. [DOI] [PubMed] [Google Scholar]
- 6.Tibaldi V, Isaia G, Scarafiotti C, et al. Hospital at Home for Elderly Patients With Acute Decompensation of Chronic Heart Failure. Arch Intern Med. 2009;169(17):1569–1575. doi: 10.1001/archinternmed.2009.267. [DOI] [PubMed] [Google Scholar]
- 7.Caplan GA, Sulaiman NS, Mangin DA, Aimonino Ricauda N, Wilson AD, Barclay L. A meta-analysis of “hospital in the home”. Med J Aust. 2012;197(9):512–519. doi: 10.5694/mja12.10480. [DOI] [PubMed] [Google Scholar]
- 8.Shepperd S, Doll H, Angus RM, et al. Avoiding hospital admission through provision of hospital care at home: a systematic review and meta-analysis of individual patient data. Can Med Assoc J. 2009;180(2):175–182. doi: 10.1503/cmaj.081491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shepperd S, Iliffe S, Doll HA, et al. Admission avoidance hospital at home. In: Shepperd S, ed. Cochrane Database of Systematic Reviews. Vol 9. John Wiley & Sons, Ltd; 2016:CD007491. 10.1002/14651858.CD007491.pub2
- 10.Board N, Brennan N, Caplan GA. A randomised controlled trial of the costs of hospital as compared with hospital in the home for acute medical patients. Aust N Z J Public Health. 2000;24(3):305–311. doi: 10.1111/j.1467-842X.2000.tb01573.x. [DOI] [PubMed] [Google Scholar]
- 11.Caplan GA, Coconis J, Board N, Sayers A, Woods J. Does home treatment affect delirium? A randomised controlled trial of rehabilitation of elderly and care at home or usual treatment (The REACH-OUT trial) Age Ageing. 2006;35(1):53–60. doi: 10.1093/ageing/afi206. [DOI] [PubMed] [Google Scholar]
- 12.Caplan GA, Coconis J, Woods J. Effect of hospital in the home treatment on physical and cognitive function: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2005;60(8):1035–1038. doi: 10.1093/gerona/60.8.1035. [DOI] [PubMed] [Google Scholar]
- 13.Federman AD, Soones T, DeCherrie LV, Leff B, Siu AL. Association of a Bundled Hospital-at-Home and 30-Day Postacute Transitional Care Program With Clinical Outcomes and Patient Experiences. JAMA Intern Med. 2018;178(8):1033. doi: 10.1001/jamainternmed.2018.2562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ojoo JC, Moon T, McGlone S, et al. Patients’ and carers’ preferences in two models of care for acute exacerbations of COPD: results of a randomised controlled trial. Thorax. 2002;57(2):167–169. doi: 10.1136/thorax.57.2.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilson A, Wynn A, Parker H. Patient and carer satisfaction with “hospital at home”: quantitative and qualitative results from a randomised controlled trial. Br J Gen Pract. 2002;52(474):9–13. [PMC free article] [PubMed] [Google Scholar]
- 16.Leff B, Burton L, Mader S, et al. Satisfaction with Hospital at Home Care. J Am Geriatr Soc. 2006;54(9):1355–1363. doi: 10.1111/j.1532-5415.2006.00855.x. [DOI] [PubMed] [Google Scholar]
- 17.Montalto M. Patients’ and Carers’ Satisfaction with Hospital-in-the-Home Care. Int J Qual Heal Care. 1996;8(3):243–251. doi: 10.1093/intqhc/8.3.243. [DOI] [PubMed] [Google Scholar]
- 18.Levine DM, Ouchi K, Blanchfield B, et al. Hospital-Level Care at Home for Acutely Ill Adults: A Randomized Controlled Trial. Ann Intern Med. 2020;172(2):77–85. doi: 10.7326/M19-0600. [DOI] [PubMed] [Google Scholar]
- 19.Levine DM, Ouchi K, Blanchfield B, et al. Hospital-Level Care at Home for Acutely Ill Adults: a Pilot Randomized Controlled Trial. J Gen Intern Med. Published online February 6, 2018. 10.1007/s11606-018-4307-z. [DOI] [PMC free article] [PubMed]
- 20.Curry L, Nunez-Smith M. Mixed Methods in Health Science Research: A Practical Primer. SAGE Publications; 2015.
- 21.Creswell J. Qualitative Inquiry & Research Design: Choosing among Five Approaches. 3rd ed. SAGE Publications; 2013.
- 22.Dubois A, Santos-Eggimann B. Evaluation of Patients’ Satisfaction with Hospital-At-Home Care. Eval Health Prof. 2001;24(1):84–98. doi: 10.1177/01632780122034812. [DOI] [PubMed] [Google Scholar]
- 23.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–594. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 16 kb)