Central Message.
3D printing of complex anatomy may improve patient outcome by optimizing surgical planning when imaging, cardiology, and surgical inputs are combined.
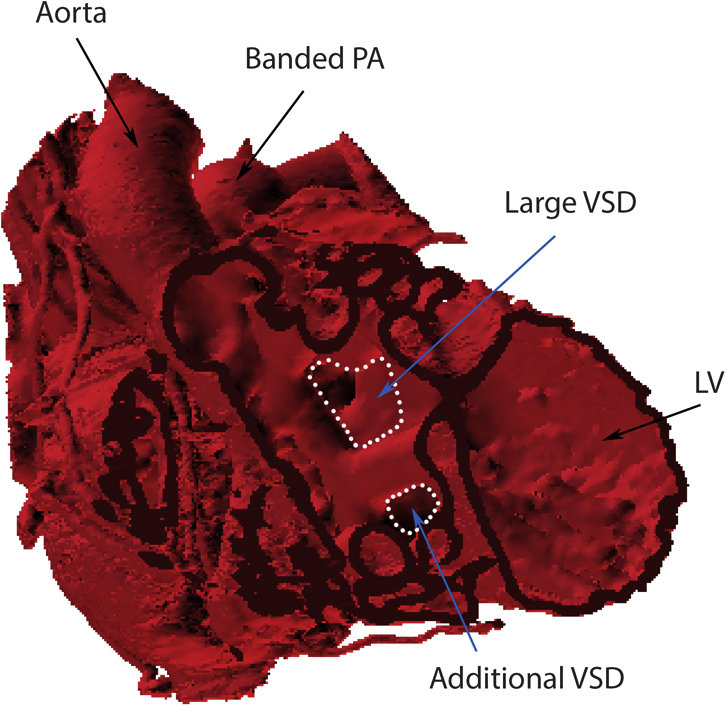
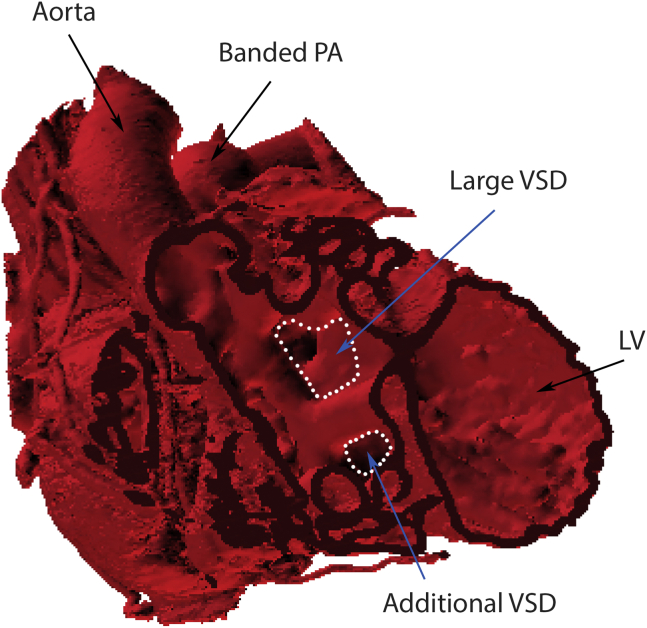
3D dataset of double-outlet right ventricle, demonstrating 2 important ventricular septal defects.
See Article page 135.
The often-stated benefits of 3-dimensional (3D)-printed reproductions of patient morphology in structural heart disease include (1) facilitation of surgical planning, (2) education of the broader team to better appreciate complex anatomy and its impact on physiology, and (3) enhancement of traditional teaching to correlate 3D structure with 2-dimensional echocardiographic images. The group responsible for this manuscript1 have pioneered much of this work, incorporating “softer” materials and development of operable models to allow rehearsal of common procedures.2
Pattern recognition is a major element of what accumulated experience affords a surgeon. This is the ability to correlate preoperative imaging with the intraoperative appearance seen in previous cases. For example, the anatomy of a ventricular septal defect (VSD) is understood and anticipated by surgeons as part of a morphologic constellation, such as the subpulmonary VSD in Taussig–Bing anatomy. In unusual anatomy, rare pathology, or early years of surgical practice, pattern recognition may not be sufficient or optimal preparation for complex surgery. Experienced cardiologists perform their own correlation between preoperative imaging and early clinical outcomes but sometimes don't have a good sense of what the surgeon will actually see. The most useful models then, will be those developed by a team of imaging, cardiology, and surgical experts collectively seeking to answer the main clinical question at hand.
In this study,1 the combination of left superior vena cava to the left atrium and a coronary sinus atrial septal defect is the clinical problem. For such patients with uncommon morphology, the strengths and weaknesses of available technical approaches need to be evaluated, since technical imperfection will have important long-term consequences likely to result in reintervention. The models were constructed to address the specific questions of intra-atrial baffling versus extracardiac approaches. Although experienced surgeons would likely default to enlargement of the atrial septal defect and intra-atrial baffling, with the extracardiac approaches as a backup plan, the model-based analytic approach nicely demonstrates the step-by-step evaluation of the various approaches that could be employed to address more complicated pathology.
Early application of 3D models in assessment of route-ability of the left ventricular outflow through a VSD to the aorta has been encouraging.3 This is of particular importance in identification of patients in whom a 2-ventricle circulation can be achieved, where it is not immediately obvious that this is possible. However, preoperative definition of multiple muscular VSDs and questions involving valve-related anatomy remain problematic.4 This occurs mostly as a result of technical limitations in the speed of acquisition and quality of the initial cross-sectional imaging rather than the process of segmentation that then describes the printed model. Evaluation of actual benefit to patient care is in its early stages5 and manipulation of the 3D dataset in PDF format may obviate the need for physical printing in some cases (see the Figure 1).
Figure 1.
3D dataset of double-outlet right ventricle, demonstrating 2 important ventricular septal defects. PA, Pulmonary artery; VSD, ventricular septal defect; LV, left ventricle.
What then is the future for 3D modeling in complex structural heart disease? Understanding the key question, high-quality image acquisition, and segmentation guided by clinical experts will enhance the yield of this promising approach. A good model cannot be “ordered,” it is evolved—collaboration inherent in this approach has many additional benefits in the creation and maintenance of a high-functioning team.
Footnotes
Disclosures: The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
References
- 1.Hussein N., Kasdi R., Coles J.G., Yoo S.-J. Use of 3-dimensionally printed heart models in the planning and simulation of surgery in patients with Raghib syndrome (coronary sinus defect with left superior vena cava) J Thorac Cardiovasc Surg Tech. 2020;2:135–138. doi: 10.1016/j.xjtc.2020.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yoo S.J., Thabit O., Kim E.K., Ide H., Yim D., Dragulescu A., et al. 3D printing in medicine of congenital heart diseases. 3D Print Med. 2015;2:3. doi: 10.1186/s41205-016-0004-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kappanayil M., Koneti N.R., Kannan R.R., Kottayil B.P., Kumar K. Three-dimensional-printed cardiac prototypes aid surgical decision-making and preoperative planning in selected cases of complex congenital heart diseases: early experience and proof of concept in a resource-limited environment. Ann Pediatr Cardiol. 2017;10:117–125. doi: 10.4103/apc.APC_149_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chepelev L., Wake N., Ryan J., Althobaity W., Gupta A., Arribas E., et al. Radiological Society of North America (RSNA) 3D printing special interest group (SIG): guidelines for medical 3D printing and appropriateness for clinical scenarios. 3D Print Med. 2018;4:11. doi: 10.1186/s41205-018-0030-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ryan J., Plasencia J., Richardson R., Velez D., Nigro J.J., Pophal S., et al. 3D printing for congenital heart disease: a single site's initial three-year experience. 3D Print Med. 2018;4:10. doi: 10.1186/s41205-018-0033-8. [DOI] [PMC free article] [PubMed] [Google Scholar]