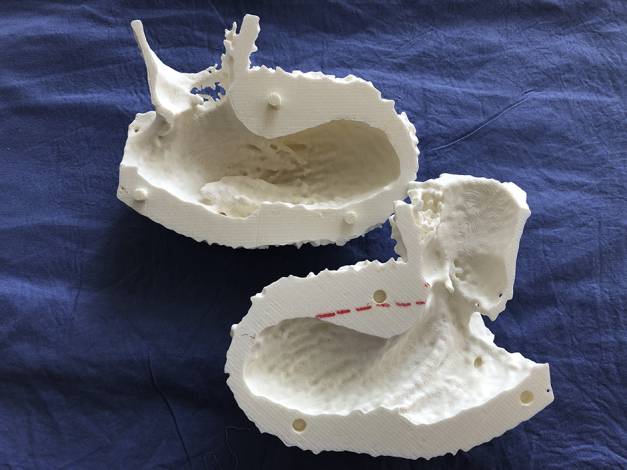
A preoperative 3D cardiac print of a patient with hypertrophic obstructive cardiomyopathy.
Central Message.
The introduction of imaging technologies into the operating room offers a potential aid to shorten the learning curve for septal myectomy.
See Article page 60.
I took a mechanical drawing class in junior high school. I come from a family of architects and engineers, and I fondly remember looking at my father's drawings and how proud he was of his printing. His block letters had a particular style. If you look at any old architectural plans or mechanical drawings you can see that each author added individual style to otherwise proudly uniform and consistent lettering. Just enough personal character to make those drawings almost artistic. We have evolved since then and now use computer-aided design software to create plans, superseding the skills I spent hours cheerfully mastering. No one would deny that computer-aided design drawings represent a major advance, even if at a bit of cost to the art.
Which brings us to septal myectomy for hypertrophic obstructive cardiomyopathy. If ever there was a condition with a gap between imaging science and intraoperative technique, it is this one. On the imaging side, we have echocardiography, computed tomography, and magnetic resonance imaging, from which we can create precise 3-dimensional prints. On the technical surgical side, however, it feels much more like art. There are a handful of undisputed masters at the major clinics—Hartzell Schaff at Mayo and Nick Smedira at Cleveland—each with literally thousands of myectomies to their names. Precise, consistent, and seemingly effortless, they are artists. At the other extreme are pedestrians like me, who find the learning curve steep and intimidating. How deep? Deep enough? Too deep? Yikes! Far enough to the left or the right? Avoid the conduction system! Plicating leaflets, mobilizing papillary muscles, and excising abnormal ones. As far as I can tell I am not alone; it remains a technique hard to learn and, from what I see, hard to teach as well.
The answer of course is experience. Deliberate practice and 10,000 hours to climb that learning curve. But how much of the learning curve can we tolerate, and by how many surgeons? Should myectomies be done by handful of “reference surgeons,” or will that effectively deny access to patients? Hypertrophic obstructive cardiomyopathy is a remarkably common condition, and we know that the surgical procedure is more effective than catheter-based ones. But if surgical expertise is not locally available, will patients get the less satisfactory procedure?
All this goes to argue in favor of efforts to abbreviate the learning curve. In their study in this issue of the Journal, Williams and colleagues1 suggest a means of closing the gap between art and science by bringing imaging into the operating room and into the heart itself. Although the series is small, and the results are preliminary, I applaud their effort. It is certainly something that I will pursue as I climb my own learning curve in this procedure. And I do not think we will lose the art altogether—just as the artistry of the engineers' underlying design remains in computer-aided design drawings, even if the flair of their individual penmanship is lost. In the end, it is progress, and we all benefit.
Footnotes
Disclosures: The author reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Reference
- 1.Williams D.M., Nampi R.G., Saric M., Grossi E.A., Sherrid M.V., Swistel D.G. On-pump intracardiac echocardiography during septal myectomy for hypertrophic cardiomyopathy. J Thorac Cardiovasc Surg Tech. 2020;2:60–66. doi: 10.1016/j.xjtc.2020.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]


